Abstract
Background and Aim:
A community-based rehabilitation programme, Sri Ramachandra University-Transforming Faces project, was initiated to provide comprehensive management of communication disorders in individuals with CLP in two districts in Tamil Nadu, India. This community-based programme aims to integrate hospital-based services with the community-based initiatives and to enable long-term care. The programme was initiated in Thiruvannamalai (2005) district and extended to Cuddalore (2011). The aim of this study was to identify needs related to speech among children with CLP, enroled in the above community-based programme in two districts in Tamil Nadu, India.
Design:
This was a cross–sectional study.
Participants and Setting:
Ten camps were conducted specifically for speech assessments in two districts over a 12-month period. Two hundred and seventeen individuals (116 males and 101 females) >3 years of age reported to the camps.
Methods:
Investigator (SLP) collected data using the speech protocol of the cleft and craniofacial centre. Descriptive analysis and profiling of speech samples were carried out and reported using universal protocol for reporting speech outcomes. Fleiss' Kappa test was used to estimate inter-rater reliability.
Results:
In this study, inter-rater reliability between three evaluators revealed good agreement for the parameters: resonance, articulatory errors and voice disorder. About 83.8% (n = 151/180) of the participants demonstrated errors in articulation and 69% (n = 124/180) exhibited abnormal resonance. Velopharyngeal port functioning assessment was completed for 55/124 participants.
Conclusion:
This study allows us to capture a “snapshot” of children with CLP, living in a specific geographical location, and assist in planning intervention programmes.
KEY WORDS: Cleft lip and palate, cleft speech, community-based rehabilitation
INTRODUCTION
In India, as in several developing countries, the challenge in providing services for individuals with CLP is impacted by social, cultural and economic characteristics of the population seeking services; most of them are from rural areas, belong to lower socioeconomic strata and have limited access to medical care.[1] Failure to follow-up is compounded by non-availability of trained professionals to deal with such cases. Cleft teams are by far few in developing countries. Thus, speech disorders are ignored or not addressed.[2,3]
In India, community-based programme has been implemented in rural areas as model of service delivery for differently abled children.[4] In UNICEF funded project, grass root level workers from a community were involved in the detection and management of speech and hearing-related issues.[5] A community-based rehabilitation programme Sri Ramachandra University (SRU) Transforming Faces project) was initiated in Tamil Nadu, India, to provide comprehensive management for communication disorders in individuals with CLP. The objective of this community-based programme was to integrate hospital-based services with community-based initiatives and to enable long-term care. This program was initiated in Thiruvannamalai in 2005 and extended to Cuddalore in 2011. Individuals with CLP were enroled by local Community-Based Rehabilitation Workers (CBRWs). The programme was structured to provide surgical repair of CLP, assessment of velopharyngeal port functioning for speech and advanced orthognathic services at the tertiary care hospital. In the community, CBRWs are trained to identify/refer, counsel, screen for speech disorders; support dental services and speech correction services were provided through camps. Periodic review is undertaken to identify the needs at the level of the community. To enable systematic evaluation and for documentation of evaluation of programmes, the protocols for data collection should be standardised and uniform. This is essential to ensure that the data are useful and available for planning and scientific reporting.[6]
Needs assessment was first conducted in 2007, in the 2nd year of the community-based programme, to identify the requirements for implementation of a speech correction programme to be delivered by the CBRW in the community.[7] Results of this study suggested that individuals who might benefit from speech services faced several barriers such as, poor economic status, poor local transport facility to travel to the nearest centre for treatment and the lack of awareness that speech could be addressed or improved. This initial data provided valuable information of the type of challenges faced at the level of the community. In this group, 37/160 were individuals with repaired isolated cleft of lip only, who exhibited clinically normal development in all aspects of communication. Sixteen individuals with repaired UCLP demonstrated normal articulation and resonance. Seventy-six individuals exhibited errors in articulation and resonance. Twenty-four individuals exhibited errors in articulation only. One individual exhibited error in resonance only. Fifty-one individuals exhibited impairments in articulation and resonance. The assessment could not be completed for 31 individuals at the campsite who were <3 years of age. This study had significant limitations in the manner in which speech information was collected. The information was collected by four SLPs and evaluated in real time. Inter-rater reliability was not reported and the data did not provide information on velopharyngeal port function. Subsequent to the study, the number of individuals enroled in the programme has gone up and children who were enroled at an earlier age are older and in need for dental or surgical correction for speech-related issues.
In 2013, a study was undertaken in four Taluks of Thiruvannamalai. This study focussed on the needs of all individuals with CLP above 2 years of age.[8] This study served the important purpose of documenting and analysing the current profile and communication status of 88 individuals from a specified geographical area using internationally accepted guidelines. Among the 88 individuals who attended camp, 55% (48 individuals) had immediate need for speech services, 26% (23 individuals) would need speech services in the near future and 19% (17 individuals) would not require any speech services in future.
Over the past 10 years, the programme has expanded in Thiruvannamalai district and extended to Cuddalore district. Types of services provided at the community have steadily increased, and surgical repair has been provided. Inputs from speech pathologist have also enhanced the awareness of speech and communication disorders. CBRW have been trained repeatedly and appropriate networking, down to the individual's home, has been established. Children with CLP who were enroled in the earlier years of the programme have grown older and new enrolments have been made in the programme since the last needs assessment conducted in 2013. It is evident that some type of community-based activity has to be provided through CBRW for facilitating improvements in speech. For the design of such a speech intervention programme, it was necessary to obtain a profile of the communication status as a group, and at the individual level, for all children with CLP enroled in the programme. The aim of this study was to identify the needs related to speech in children with CLP enroled in the community-based programme in Thiruvannamalai and Cuddalore districts in Tamil Nadu, India.
METHOD
This study was carried out after obtaining approval from the Institutional Ethics Committee. The reference number is IEC-N1/10/DEC/20/42.
Participants
Four hundred individuals with CLP, enroled in the community-based programme implemented in Cuddalore and Thiruvannamalai districts of Tamil Nadu, were identified from the database maintained by the programme office at the tertiary care hospital. They were contacted either through post/telephone/home visit by 08 CBRWs working for the programme in Cuddalore (04CBRW) and Thiruvannamalai (04 CBRW) district. They informed the families of individuals with CLP about the date, time and venue for the monthly speech assessment camps. Table 1 shows the distribution of participants for whom speech assessment was completed/not completed.
Table 1.
Distribution of participants from Cuddalore and Thiruvannamalai who completed/did not complete assessments
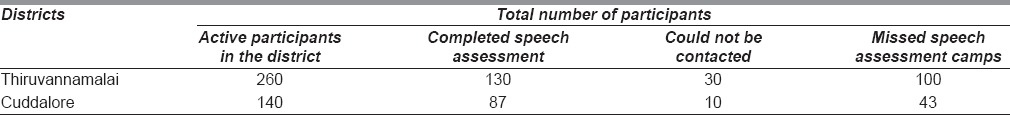
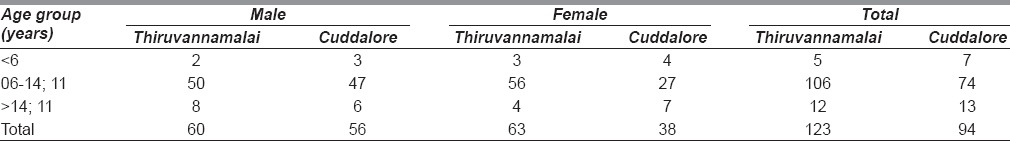
A total of 217 individuals (116 males and 101 females) with a repaired cleft of lip and palate reported to the 10 camps (05 each in Cuddalore and Thiruvannamalai districts) conducted over 12 months. All of them received surgical correction at or before 36 months of age by a surgeon experienced in the repair of cleft lip and palate. Table 2 depicts age and gender breakup of the participants.
Table 2.
Distribution of age and gender of participants who attended recruitment camps
Profiling of speech and language skills
The investigator, an SLP with more than 10 years of experience in the clinical assessment of speech and language in individuals with CLP, completed the assessments in the Tamil language for each participant. The database and records of each participant were perused to identify whether the individual with CLP required detailed the assessment of language. Language assessments were recommended for participants whose two successive assessments indicated language delay. Speech tasks for evaluation of articulation and resonance included general conversation, word repetition, sentence repetition, syllable repetition ([pa: ], [pi: ], [ta: ], [ti: ], [ka: ], [ki: ], [sa: ], [si: ]) and number counting (1–10 and 60–70 in English). For word repetition task, controlled speech stimuli consisting of 44 words were used. This material was developed as part of Sri Ramachandra University Speech training initiative.[9] For sentence repetition task, ten sentences loaded with pressure consonants, used in cleft and craniofacial speech clinic, were used. Any participant exhibiting hypernasal resonance, nasal air emission, weak pressure consonants, nasalisation oral pressure consonants were recommended the assessment of velopharyngeal port function. Caregivers who accompanied the participants were explained about the need for assessment and were referred to the tertiary care centre after obtaining their consent.
Recording of speech sample
Audio video recording was obtained in the quietest environment available at the campsite. Sony DCR-DVD 905 handy cam camcorder and portable digital voice recorder (Sony ICD-UX 70) were used.
Nasoendoscopy assessment
The nasoendoscopy procedure was carried out by a plastic surgeon and speech pathologist at the tertiary care hospital. Local nasal anaesthetic spray lidocaine (10% lidocaine topical solution) was administered. This procedure was performed using Olympus GLK-4 model instrument to view the velopharyngeal port. The impression of velopharyngeal dysfunction was established by the presence of hypernasal resonance at the sentence level and a gap in the velopharyngeal valve observed during nasoendoscopy. The speech samples included: syllable repetition, number counting and sentence repetition. The nasoendoscopy analysis focused on assessing the movement of the velum and the walls of the pharyngeal cavity (lateral pharyngeal walls and posterior pharyngeal wall). The presence of the velopharyngeal gap if any was rated on a 3 point rating scale (1-Mild, 2-Moderate, 3-Large). The rating of overall gap size was determined by agreement between plastic surgeon and speech pathologist using the protocol used for nasoendosocpy assessment at the tertiary care centre.
Analysis
Perceptual evaluation of recorded speech sample
Speech samples of 180/217 participants were subjected for perceptual evaluation. Twelve participants below 6 years of age did not cooperate for speech sample recording. Twenty-five participants had requested to be relieved from services related to speech.
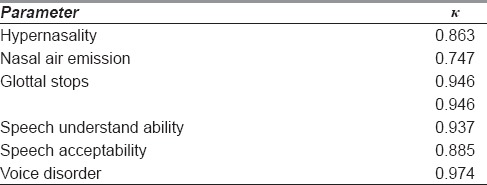
All 180 speech samples were coded after editing demographics/personal information of participants. Three SLPs with more than 3 years' experience in assessing cleft palate speech independently evaluated the blinded speech samples using the standard protocol. They transcribed the speech sample and coded the pattern of error using universal parameters of reporting cleft speech.[10] Inter-rater reliability measures were established using Fleiss Kappa. Inter-rater reliability between the three SLPs revealed adequate agreement across all the parameters. The values obtained are tabulated in Table 3.
Table 3.
Interrater reliability across parameters
RESULTS
The speech and language profile of 12 participants (<6 years of age) who did not cooperate for speech sample recording were evaluated at the campsite. None of them met the criteria stated above for language evaluation. Informal assessment of speech sound production in this group revealed the presence of developmental errors (patterns of sound errors that typically developing children use to simplify speech during the early stages of speech sound acquisition) and backing to glottal for pressure consonants [t], [k], [s].
The perceptual evaluation of speech samples of 180 participants could be classified into four categories: (i) normal speech, (ii) a combination of errors in articulation and resonance, (iii) abnormal articulation and normal resonance, (iv) abnormal resonance and normal articulation. The distribution is represented in Figure 1. Voice was rated to be within normal limits in all participants.
Figure 1.
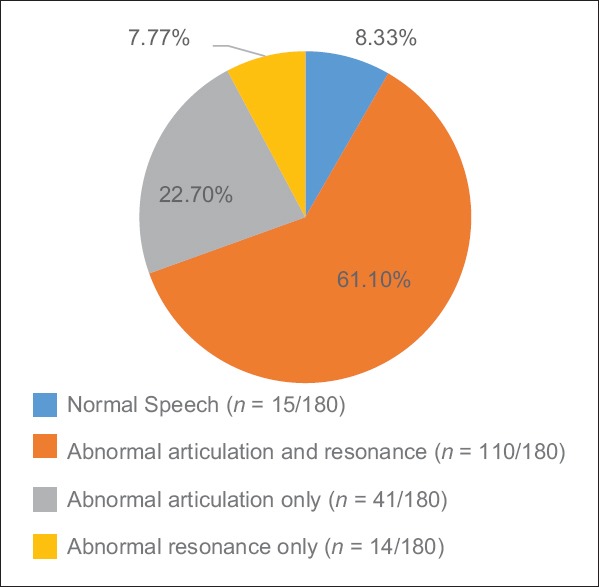
Distribution of speech profile of participants
Specific errors in articulation
Errors in articulation were calculated both at word and sentences levels, and are represented in percentage. The types of error pattern were similar across word and sentence levels. Errors in articulation were exhibited by 83.8% (n = 151/180) of the participants. Distribution of the type of errors in articulation is tabulated in Table 4.
Table 4.
Distribution of errors in articulation among those with articulation deficits
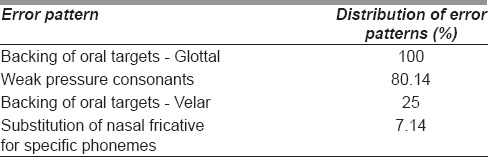
The most common error exhibited was backing of oral targets to glottal. The presence of glottal stops was observed predominantly in consonants [k] and [t]. In this group of 180 participants' developmental articulation/phonological error were rated as “none” by the evaluators in the universal parameters of reporting cleft speech.[10]
Abnormal resonance and nasal air emission
The result of perceptual analysis of 124/180 participants with varying degrees of abnormal resonance is as profiled. Hypernasality was rated to be mild, 60.04% (n = 75/124), moderate, 25% (n = 31/124) and severe, 14.51% (n = 18/124). Hyponasal resonance was not reported in this group of participants. Nasal air emission was rated to be present in (n = 77/180) participants. The presence of nasal air emission was rated to be intermittent in 33.88% (n = 61/180) and frequent in 8.88% (n = 16/180) of the participants.
Speech understandability and speech acceptability
Speech understandability and speech acceptability parameters were normal in 8.33% (n = 15/180) of participants. Speech understandability was rated as mildly impaired in 61.11% (n = 110/180) participants, moderate in 24.44% (n = 44/180) and severe in 6.11% (n = 11/180). Similarly, in speech acceptability, speech was rated to be deviated from normal aspects, as mild in 69.44% (n = 125/180) participants, moderate in 12.22% (n = 22/180), and severe in 18% (n = 18/180).
Nasoendoscopy assessment
During assessment in the camps, 124/180 participants, perceived to have hypernasality, were recommended for further assessment of velopharyngeal port functioning for speech. Only 55/124 followed up at the tertiary care centre. Nasoendoscopy assessment results revealed full or near complete closure for 16/55 participants. They were recommended for speech therapy for correction of errors in articulation. 39/55 participants were identified to have velopharyngeal dysfunction defects ranging from minimal to large defects. They were recommended for surgical intervention followed by speech therapy. In the group of participants recommended for surgical intervention, 25/39 participants were recommended superior-based pharyngeal flap, 12/39 participants for intravelar veloplasty and 02/39 participants for Hynes pharyngoplasty.
DISCUSSION
The objective of this study was to identify the needs relating to the speech of beneficiaries of this community-based programme in two districts. The aspects explored included: (1) perceived need and motivation of parents/beneficiaries as measured by attendance to camps/tertiary care centre, (2) estimation of beneficiaries requiring specific services relating to speech as measured by the perceptual evaluation and (3) potential challenges and barriers relating to delivery of speech services at the community. This profiling would serve as a framework for developing a speech intervention programme to be delivered by CBRW under the supervision of SLP.
All 400 beneficiaries enroled in the programme in both Thiruvannamalai and Cuddalore districts were informed about the camps specifically focussing on the evaluation of speech and need for speech services. This information was provided to the beneficiaries through the network of 08 CBRW involved in the programme. The camps were held in locations accessible to public transport and within 3 h of travel distance from the site of the camp. Participants who missed the initial camp had the opportunity to attend later camps. In spite of these efforts, a little more than 50% (217/400) of the participants reported to the camps. It is also possible that only parents or participants who had concerns about speech attended the camps. There was a group of 25 participants predominantly above 15 years of age who categorically stated that they did not wish to receive speech services. All of them were either employed or enroled for higher education that did not permit them to avail any form periodic services related to speech. This would suggest that speech intervention programme does not have to be anticipated for every beneficiary enroled in the community-based programme. This has important implications for allocation of financial/human resources in the execution of the programme.
Speech profile was obtained for 192 participants. This included a group of 12 participants <6 years of age. These participants clearly demonstrated a need for early intervention to learn correct placement of articulation. The remaining 180 participants in the age group of 6–14; 11 years were enroled in school. Speech intervention was indicated in 165/180 participants. The most common error pattern observed was backing to glottal (Glottal stops) in pressure consonants [k], [t], [T] was observed in 151 participants who exhibited errors in articulation. Specifically, 124 participants were referred for evaluation of velopharyngeal port functioning. Only 55 followed up despite frequent calls and multiple rescheduling. Of these 55 participants, 10 were recommended speech therapy and surgical correction followed by speech therapy for 45 participants.
The speech profile is similar to that reported in two earlier studies reported by George and Nagarajan,[7] Sampath and Nagarajan[8] restricted to Thiruvannamalai district. These studies completed in 2007 and 2013 related to the development of services such as identification, triage and referrals of individuals with CLP. The inferences of these studies helped to expand the services and develop human resources to provide services related to speech. Since then, the community-based programme has expanded in Thiruvannamalai district, and the programme was extended in a new district (Cuddalore).
The present study provides a valuable framework for developing a speech intervention programme to be delivered in the community. There emerged the need for different types of services, one of it being the implementation of intervention module that could be delivered by parents to provide a model for learning appropriate articulatory patterns for children below 6 years of age. Community-based workers could be trained as facilitators for such a programme. In Thailand, a networking model of speech correction was evaluated.[11] Parents implemented activities recommended by the SLP which were overseen by speech assistants (Hospital nurse) in their region. Authors reported improvement in the percentage of correct consonant production in 3/6 children and recommended this as a model in regions where services of SLP are limited.
Another type of service would focus on a speech correction programme for those individuals with CLP who could comply with a more structured speech correction programme. Such a programme when delivered in the community would focus on correction of errors relating to the production of consonants by a CBRW under the supervision of SLP.
Any community-based programme would have to take into account barriers and challenges that beneficiaries may have even if the services are provided close to their community. Parents attributed their inability to attend camps to one or more of the following reasons: (a) Could not take leave from work due to the loss of income; (b) no permission from school; (c) family/social obligations function; (d) father was not available to accompany the participant to the camp. Challenges reported for poor follow-up at camps, and tertiary care hospital are similar to the findings reported.[1,12] The challenges in providing timely speech intervention in this study are similar to the problem reported to be observed in South Asian countries.[13,14] It is important to determine the factors that encourage investment of parent in the ongoing programme.
About 50% of the participants/parents of children with CLP were concerned enough to report to camps relating to speech. Analysis revealed that a major group of participants in this study exhibited some form of speech disorder requiring speech intervention. Needs of a child with CLP may change as he/she grows, especially in the management of CLP, which is long-term with intervention following a timeline. Hence, it is important to conduct a needs assessment at different time points in such community-based programmes which requires intensive administrative and financial planning. This study provides a breakup and profile of the number of participants who are ready for direct speech intervention and surgical intervention before speech correction. These participants can be mapped their residences in both districts for planning logistics. This information is important in linking CBRW to the participants especially to deliver services that are efficient with reference to cost and time taken for travel.
This speech profile obtained would be helpful in planning/designing of training programmes for the CBRW to listen and identify abnormal patterns, strategies to correct, provide reinforcement and documentation. The findings of this study also suggest the need to understand parent's perception of their child's speech and to involve them in the design of speech intervention programme.
CONCLUSION
The fundamental aim of community-based programmes is to provide services at venues as close to the individuals requiring services as possible. This could be homes, or schools or other centres close to the child. While penetration of technology facilitates better networking, it is yet to translate into delivery of services such as speech. Such a service requires trained CBRW, careful selection of individuals, appropriate techniques, intensity and reinforcement to ensure application of behaviour modification strategies for correction of speech. Therefore, obtaining a speech profile “snapshot” is vital to design resource material and in the training of CBRW who would deliver the speech correction programme to selected children under the close supervision of SLP. The strategy is to obtain as detailed an assessment as possible for planning and executing individualised speech intervention plans for children with CLP living in rural communities, keeping in mind, the challenges and availability of local resources.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We would like to acknowledge Transforming Faces, a non-profit Canadian organisation for their support for the ongoing community-based programme and this study.
REFERENCES
- 1.Raju SR. An Unpublished Study by, Unit for Urban Studies, Tata Institute of Social Sciences. Mumbai, India: 2000. In Search of a Smile: Study of Children Born With Cleft Lips and Palates in India. [Google Scholar]
- 2.D'Antonio LL, Nagarajan R. Use of a consensus building approach to plan speech services for children with cleft palate in India. Folia Phoniatr Logop. 2003;55:306–13. doi: 10.1159/000073254. [DOI] [PubMed] [Google Scholar]
- 3.Prathaneel B, Makarabhirom K, Jaiyong P, Pradubwong S. Khon Kaen: A community-based speech therapy model for an area lacking in speech services for clefts. Southeast Asian J Trop Med Public Health. 2014;45:1182–95. [PubMed] [Google Scholar]
- 4.WHO-SEARO. Compilation of Community-Based Rehabilitation Practices in the WHO South-East Asia Region. Who-Searo. 2013 [Google Scholar]
- 5.Rao EM, Mukundan G, Kant A. Mobilizing rural workers in rehabilitation of the speech and hearing handicapped. Indian J Disabil Rehabil. 1990;4:45–53. [Google Scholar]
- 6.Sell D, Grunwell P, Mars M. A methodology for the evaluation of severely disordered cleft palate speech. Clin Linguist Phonetics. 1994;8:219–33. [Google Scholar]
- 7.George SA, Nagarajan R. Unpublished Manuscript. Sri Ramachandra University; 2007. Speech services for individuals with cleft lip and palate in a rural community: An assessment of neeeds. [Google Scholar]
- 8.Sampath P, Nagarajan R. Unpublished Manuscript. Sri Ramachandra University; 2013. Communication Profile of Individuals with Cleft Lip and Palate From Four Taluks of Thiruvannamalai. [Google Scholar]
- 9.Nagarajan R, Savitha VH, Navitha U. Development of Controlled Speech Stimuli Across Indian Languages. Chennai: Sri Ramachandra University- Smile Train Speech Training Initiative (SRUSTI); 2012. [Google Scholar]
- 10.Henningsson G, Kuehn DP, Sell D, Sweeney T, Trost-Cardamone JE, Whitehill TL, et al. Universal parameters for reporting speech outcomes in individuals with cleft palate. Cleft Palate Craniofac J. 2008;45:1–7. doi: 10.1597/06-086.1. [DOI] [PubMed] [Google Scholar]
- 11.Pumnum T, Kum-ud W, Prathanee B. A networking of community-based speech therapy: Borabue district, Maha Sarakham. J Med Assoc Thai. 2015;98(Suppl 7):S120–7. [PubMed] [Google Scholar]
- 12.Raman S, Jacob M, Jacob MS, Nagarajan R. Providing intervention services for communication deficits associated with cleft lip and/or palate – A retrospective analysis. Asia Pacific Disabil Rehabil J. 2004;15:78–85. [Google Scholar]
- 13.Prathanee B, Lorwatanapongsa P, Makarabhirom K, Suphawatjariyakul R, Thinnaithorn R, Thanwiratananich P, et al. Community-based model for speech therapy in Thailand: Implementation. J Med Assoc Thai. 2010;93(Suppl 4):S1–6. [PubMed] [Google Scholar]
- 14.Prathanee B, Dechongkit S, Manochiopinig S. Development of community-based speech therapy model: For children with cleft lip/palate in Northeast Thailand. J Med Assoc Thai. 2006;89:500–8. [PubMed] [Google Scholar]


