Abstract
Particle beam therapy (PBT), including proton and carbon ion therapy, is an emerging innovative treatment for cancer patients. Due to the high cost of and limited access to treatment, meticulous selection of patients who would benefit most from PBT, when compared with standard X-ray therapy (XRT), is necessary. Due to the cost and labor involved in randomized controlled trials, the model-based approach (MBA) is used as an alternative means of establishing scientific evidence in medicine, and it can be improved continuously. Good databases and reasonable models are crucial for the reliability of this approach. The tumor control probability and normal tissue complication probability models are good illustrations of the advantages of PBT, but pre-existing NTCP models have been derived from historical patient treatments from the XRT era. This highlights the necessity of prospectively analyzing specific treatment-related toxicities in order to develop PBT-compatible models. An international consensus has been reached at the Global Institution for Collaborative Research and Education (GI-CoRE) joint symposium, concluding that a systematically developed model is required for model accuracy and performance. Six important steps that need to be observed in these considerations include patient selection, treatment planning, beam delivery, dose verification, response assessment, and data analysis. Advanced technologies in radiotherapy and computer science can be integrated to improve the efficacy of a treatment. Model validation and appropriately defined thresholds in a cost-effectiveness centered manner, together with quality assurance in the treatment planning, have to be achieved prior to clinical implementation.
Keywords: particle beam therapy, normal tissue complication probability, model-based approach, GI-CoRE
INTRODUCTION
Thanks to support from the Japanese Government and Hokkaido University, a joint symposium has emerged for collaboration between the Global Institution for Collaborative Research and Education, the Global station for quantum medical science and engineering (GI-CoRE GSQ), the Global Station for Big data and Cybersecurity (GSB), and the Institute for Genetic Medicine (IGM), Hokkaido University. The scope of the symposium focused on a model-based approach (MBA) to tumor control probability (TCP) and normal tissue complication probability (NTCP) for particle beam therapy (PBT) as a step toward an international consensus. Highly respected speakers from 10 institutions (the University Medical Center Groningen; the Stanford Cancer Institute and Stanford University Medical Center; the Mayo Clinic; the University of Texas MD Anderson Cancer Center, the Johns Hopkins University School of Medicine; the University of Technology Sidney; the National Institute of Radiological Science in Chiba; Osaka University; Kobe Pharmaceutical University; and Hokkaido University) were invited to present their scientific knowledge related to the establishment of a global consensus on how to assess treatment efficacy and toxicity with PBT. The principles of MBA, big data analysis, fundamental radiation biology, radiation treatment planning systems, cancer care coordination, and medical economics on particle beam therapy were comprehensively discussed.
The goal of this symposium was to collaboratively develop an internationally accepted model for identifying patients and tumors that will derive the most benefit from PBT, in consideration of the high cost of developing and implementing this therapy.
MODEL-BASED APPROACH
A number of retrospective studies have demonstrated the dosimetric and clinical benefits of PBT for several tumor sites, but a randomized controlled trial (RCT) of PBT versus standard X-ray therapy (XRT) is still expected to be needed in order to obtain Level I evidence in medical practice. However, there are a number of obstacles to conducting an RCT in terms of ethical and pragmatic issues [1, 2]. An MBA is an alternative option for aiding in clinical decision-making for the Radiation Oncology Society, where evolving technologies are rapidly being developed. Without randomization, patient selection biases can be eliminated by stratification based on specified characteristics when applying the model; for example, the NTCP model for radiation-induced liver disease will be different from that for patients with Child–Pugh A versus Child–Pugh B–C. In the multivariable model, the clinical and non-clinical (including dosimetric) features of individual patients will be included and analyzed to produce the model predicting specific treatment-related toxicities. Using an appropriate statistical method, the effect of each variable is weighted by a coefficient value and integrated with other variables for the same patient, leading to a personalized predictive score. In order to achieve appropriate patient selection for PBT, a model with tailor-made criteria is eagerly anticipated to help decide the details of the RCT. Minimal requirements for rigorous models include prospective data collection, sufficient numbers of patients and events, multivariable analysis, available clinical decision rules, internal validation, and model performance testing [3]. The concept of MBA patient selection for PBT was first introduced by the University of Groningen, the Netherlands [4, 5] and successfully approved by the Dutch Health Council and the Dutch Health Care Insurance Board. Practically, patients will be eligible for proton therapy if individually applied validated NTCP models predict low levels of toxicity.
There are several types of TCP and NTCP models. The historical Webb TCP model [6] and Lyman–Kutcher–Burman NTCP model [7, 8] are useful for a comparison between radiation modalities, but differences in biological and absorbed doses are still a concern, especially when charged particle or non-conventional fractionation is used [9, 10]. Recently, researchers from Hokkaido University have systematically reviewed NTCP models for liver tumors in the literature and found heterogeneous results among the models, although the same patient data were applied (unpublished results); thus, an international consensus on NTCP models is needed. Explanations for the variation of results generated by the different models may lie in the diversity of patients, diseases, and treatment regimens. The limitation of the approach is a result of the XRT-derived NTCP models being assumed to be valid for proton-based treatments. Despite validity assertions for head and neck cancers[11], it is recommended that specific treatment-related toxicities should be prospectively analyzed and the models refined in order to validate PBT-compatible NTCP models.
PROPOSED SYSTEMATIC DEVELOPMENT OF TCP/NTCP MODELS
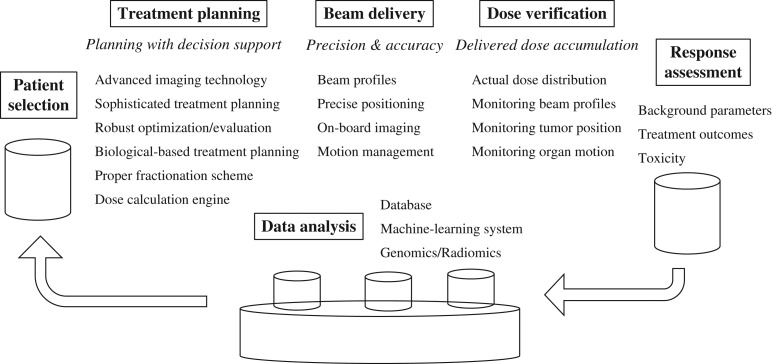
The consensus that has been drawn from this international symposium is that a systematically developed model is required. Six important steps should be scrutinized to ensure model accuracy and performance, as illustrated in Fig. 1.
Fig. 1.
Six critical steps in developing an accurate, highly effective and useful model in radiotherapy.
Patient selection
The rationale for patient selection is of paramount importance, and is a good starting point for a mutually agreed study design. Inclusion and exclusion criteria, as well as study endpoints, must be clear and clinically meaningful, and they will significantly impact the clinical outcomes.
Treatment planning
Advanced technologies have emerged for improving the efficacy of radiation treatments. First, for target delineation, computed tomography (CT), magnetic-resonance imaging (MRI), and positron-emitting tomography (PET)/CT all provide good image quality with high spatial resolution. Four-dimensional CT (4DCT) accounting for respiratory-dependent organ motion further improves the temporal resolution for moving tumors. In addition, molecular imaging–based radiation treatment planning and monitoring are currently evolving: for example, hypoxia imaging using 18Fluorine-labeled fluoromisonidazole (18F-FMISO) [12] and Caspase-3-sensitive nanoaggregation MRI (C-SNAM) [13]. Second, sophisticated treatments such as intensity-modulated proton therapy need to be subject to robust optimization and evaluation, since small errors could jeopardize the TCP or worsen the NTCP, so establishing the therapeutic window while considering the predicted TCP/NTCP is critically helpful in the treatment planning step. Third, a biological-based treatment planning using Monte Carlo simulation increases plan accuracy by comprehensively considering PBT uncertainties together with biological doses from relatively high linear energy transfer (LET), as well as from the physics of particle interactions and tissue inhomogeneity and its scattering effects [14, 15]. Finally, appropriate fractionation schemes must be carefully selected by optimization of both physical and biological profiles [16]. These innovations will provide treatment plans with reliably supported decision-making.
Beam delivery
Due to the effect of dose uncertainties on the accuracy of model-based patient selection [17], the treatment plan robustness and differences between planned and delivered dose distributions need to be investigated. The accuracy of the beam delivery requires reliable beam profiles and minimal uncertainties in beam range and set-up errors. Precise tumor positioning can be achieved, mainly by appropriate patient immobilization, on-board imaging (OBI), and effective motion mitigation of interplay effects. Orthogonal X-ray and cone-beam computed tomography (CBCT) are the commonly used OBI methods. They facilitate beam delivery and tumor margin restrictions, as well as correction for interfraction motion and volumetric changes during the treatment, leading to a significant decrease in NTCP without compromising TCP [18–20]. Several motion management strategies have been proposed. Real-time tumor-tracking radiotherapy (RTRT) is the most promising technology and can be integrated with a proton spot-scanning system, a so called real-time tumor-tracking scanning proton therapy system [21].
Dose verification
Actual dose distribution verification involves monitoring of beam profiles, tumor position and organ motion. Acquirement of the delivered dose accumulation in the patient is necessary when incorporated with clinical outcomes in order to generate accurate TCP/NTCP models. Related to this issue, it is a challenge to acquire the 3D delivered dose distribution during the treatment scans rapidly enough to be able to make real-time treatment decisions.
Response assessment
During and after treatment, regular follow-up of treatment outcomes and toxicity is needed. Data collection and organization are critical parts of the research in order to maintain the study integrity. Given that the validity of the study improves with the number of study subjects, multi-institutional data aggregation will be useful. For instance, the Mayo clinic has an outcomes warehouse for data-sharing among their three regional sites. The warehouse data consists of (i) hospital registration (demographic data and death status); (ii) Electronic Medical Record or EMR (diagnosis, treatment and physician-reported toxicity); (iii) patient-reported outcomes (PROs) survey (patient-reported toxicity and quality of life); and (iv) dose–volume histogram (DVH) data. Such a database, including treatment outcomes and toxicity, can be comprehensively analyzed in order to develop reliable TCP/NTCP models.
Data analysis
Good collaboration among clinicians, statisticians and informaticists is necessary for clinical and dosimetric data analysis. The evolving machine-learning methods are performed to convert the knowledge into clinical prediction using data science models. For example, the Johns Hopkins ‘Oncospace’ software collects clinical information and DVH data of prior patients [22].The results of specific clinical aspects can be drawn from the analysis of a large database and incorporated into the treatment plans of new patients to improve safety and quality of life. This is termed a knowledge-based planning approach. In the future, genomics and radiomics can be integrated and used to further develop the model.
After model development, the next mandatory step is model validation in order to determine the performance, accuracy and generalization of the model. The quality of TCP/NTCP models is assessed by internal and external validation of the model in different groups of patients using data from the same and different institutions, respectively. In addition, thanks to advances in computer science, large database analyses using a model-based machine-learning approach can be used to intermittently validate the model by integration of current patient data in the validation step. This will maintain the good quality of the models. Eventually, the fully developed complete model would be able to confidently determine tumors and patients who will potentially benefit from PBT.
OPINIONS IDENTIFYING THE SHORTCOMINGS OF A MODEL-BASED APPROACH
The limitations of a model-based patient selection for PBT include the deductions made from XRT-derived models, unknown thresholds of risk/benefit for determining the use of PBT, and the quality of treatment planning. Even with the existing models derived from XRT data, the model validation for PBT treatment has to be confirmed, for example, in the Blanchard study on head and neck cancers [11]. However, some statistical issues remain unresolved: for example, studies on NTCP models did not consider model uncertainties. This could lead to random errors and misinterpretations of the results [17]. Additionally, appropriate thresholds must be defined at specific endpoints for each particular tumor on a cost–effectiveness basis. Due to the diversity of opinion about the cost effectiveness of PBT, it is difficult to generate a general rule of reimbursement among institutions and countries. The cost depends on the treatment cost and the cost of care after treatment, which is negotiable at the level of the institution. The incremental cost–effectiveness ratio (ICER), considering increase in treatment costs versus improvements in quality-adjusted life years (QALYs), can be performed in a model-based cost–effectiveness analysis [23]. If the ICER of PBT exceeds the willingness-to-pay threshold, a PBT is not a cost-effective treatment compared with standard XRT. With this method, appropriate ∆NTCP thresholds can be identified. Further, the treatment planning for IMRT can intentionally be made suboptimal in order to make a PBT look better in calculating the ∆NTCP, even when the TCP is the same. This shows the need for quality assurance in treatment planning.
CONSENSUS FROM THE GI-CORE JOINT SYMPOSIUM
The MBA is helpful from the view point of the costs and work load involved in an RCT, although the RCT is still the gold standard at present. The MBA can be seen as an alternative measure of evidence-based medicine that needs to be improved continuously. Good databases and reasonable TCP and NTCP models are crucial for the reliability of this approach. The optimal solution may lie in between the RCT and MBA; specifically, using the RCT as the gold standard and the MBA as a useful measure for selecting patients for the RCT. This could allow the number of patients who are required for an RCT to be smaller if an MBA is used. Practically, the government and other stakeholders in health insurance must agree to an MBA, despite the consensus among clinicians. Hopefully, Japanese Proton Beam Therapy Institutions will be interested in analyzing their large data volumes for an establishment of the MBA.
ACKNOWLEDGEMENTS
Some of the results of this study were presented at the 5th Global station for Quantum Medical Science and Engineering (GSQ) & the 1st Global Station for Big data and Cybersecurity (GSB) symposium.
CONFLICT OF INTEREST
The authors declare that there are no conflicts of interest.
References
- 1. Hellman S, Hellman DS. Of mice but not men. Problems of the randomized clinical trial. N Engl J Med 1991;324:1585–9. [DOI] [PubMed] [Google Scholar]
- 2. Goitein M, Cox JD. Should randomized clinical trials be required for proton radiotherapy? J Clin Oncol 2008;26:175–6. [DOI] [PubMed] [Google Scholar]
- 3. Collins GS, Reitsma JB, Altman DG et al. . Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): the TRIPOD statement. Ann Intern Med 2015;162:55–63. [DOI] [PubMed] [Google Scholar]
- 4. Langendijk JA, Lambin P, De Ruysscher D et al. . Selection of patients for radiotherapy with protons aiming at reduction of side effects: the model-based approach. Radiother Oncol 2013;107:267–73. [DOI] [PubMed] [Google Scholar]
- 5. Jakobi A, Bandurska-Luque A, Stutzer K et al. . Identification of patient benefit from proton therapy for advanced head and neck cancer patients based on individual and subgroup normal tissue complication probability analysis. Int J Radiat Oncol Biol Phys 2015;92:1165–74. [DOI] [PubMed] [Google Scholar]
- 6. Webb S, Nahum AE. A model for calculating tumour control probability in radiotherapy including the effects of inhomogeneous distributions of dose and clonogenic cell density. Phys Med Biol 1993;38:653–66. [DOI] [PubMed] [Google Scholar]
- 7. Lyman JT. Complication probability as assessed from dose–volume histograms. Radiat Res 1985;8:S13–9. [PubMed] [Google Scholar]
- 8. Burman C, Kutcher GJ, Emami B et al. . Fitting of normal tissue tolerance data to an analytic function. Int J Radiat Oncol Biol Phys 1991;21:123–35. [DOI] [PubMed] [Google Scholar]
- 9. Niemierko A. Reporting and analyzing dose distributions: a concept of equivalent uniform dose. Med Phys 1997;24:103–10. [DOI] [PubMed] [Google Scholar]
- 10. Toesca DA, Osmundson EC, Eyben RV et al. . Central liver toxicity after SBRT: an expanded analysis and predictive nomogram. Radiother Oncol 2017;122:130–6. [DOI] [PubMed] [Google Scholar]
- 11. Blanchard P, Wong AJ, Gunn GB et al. . Toward a model-based patient selection strategy for proton therapy: external validation of photon-derived normal tissue complication probability models in a head and neck proton therapy cohort. Radiother Oncol 2016;121:381–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lee NY, Mechalakos JG, Nehmeh S et al. . Fluorine-18-labeled fluoromisonidazole positron emission and computed tomography-guided intensity-modulated radiotherapy for head and neck cancer: a feasibility study. Int J Radiat Oncol Biol Phys 2008;70:2–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shuhendler AJ, Ye D, Brewer KD et al. . Molecular magnetic resonance imaging of tumor response to therapy. Sci Rep 2015;5:14759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Paganetti H. Nuclear interactions in proton therapy: dose and relative biological effect distributions originating from primary and secondary particles. Phys Med Biol 2002;47:747–64. [DOI] [PubMed] [Google Scholar]
- 15. Wan Chan Tseung HS, Ma J, Kreofsky CR et al. . Clinically applicable Monte Carlo–based biological dose optimization for the treatment of head and neck cancers with spot-scanning proton therapy. Int J Radiat Oncol Biol Phys 2016;95:1535–43. [DOI] [PubMed] [Google Scholar]
- 16. Mizuta M, Takao S, Date H et al. . A mathematical study to select fractionation regimen based on physical dose distribution and the linear–quadratic model. Int J Radiat Oncol Biol Phys 2012;84:829–33. [DOI] [PubMed] [Google Scholar]
- 17. Bijman RG, Breedveld S, Arts T et al. . Impact of model and dose uncertainty on model-based selection of oropharyngeal cancer patients for proton therapy. Acta Oncol 2017;56:1444–50. [DOI] [PubMed] [Google Scholar]
- 18. Maund IF, Benson RJ, Fairfoul J et al. . Image-guided radiotherapy of the prostate using daily CBCT: the feasibility and likely benefit of implementing a margin reduction. Br J Radiol 2014;87:20140459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rothe Arnesen M, Eilertsen K, Malinen E. Optimal treatment margins for radiotherapy of prostate cancer based on interfraction imaging. Acta Oncol 2008;47:1373–81. [DOI] [PubMed] [Google Scholar]
- 20. Ho KF, Marchant T, Moore C et al. . Monitoring dosimetric impact of weight loss with kilovoltage (kV) cone beam CT (CBCT) during parotid-sparing IMRT and concurrent chemotherapy. Int J Radiat Oncol Biol Phys 2012;82:e375–82. [DOI] [PubMed] [Google Scholar]
- 21. Shimizu S, Miyamoto N, Matsuura T et al. . A proton beam therapy system dedicated to spot-scanning increases accuracy with moving tumors by real-time imaging and gating and reduces equipment size. PLoS One 2014;9:e94971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McNutt T, Evans K, Moore J et al. . WE-G-108–02: Oncospace: a database designed for personalized medicine in radiation oncology. Med Phys 2013;40:501. [Google Scholar]
- 23. Ramaekers BLT, Grutters JPC, Pijls-Johannesma M et al. . Protons in head-and-neck cancer: bridging the gap of evidence. Int J Radiat Oncol Biol Phys 2013;85:1282–8. [DOI] [PubMed] [Google Scholar]