Abstract
INTRODUCTION:
Hot flashes are considered to be a common experience for menopausal women and they can compromise the quality of life. The objective of this study is to assess the efficacy of Cimicifuga racemosa in comparison with evening primrose oil (EPO) in postmenopausal women with menopause-related symptoms.
MATERIALS AND METHODS:
This study was performed on 80 postmenopausal women with hot flashes. The participants were randomly divided into two groups by blocked randomization. The participants of one group received black cohosh and the other group received EPO for 8 weeks. The severity and number of hot flashes and quality of life were measured by four-point scale, and the Menopause-Specific Quality of Life (MENQOL) questionnaire at pre-intervention, 1st, 4th, and 8th weeks after treatment. Data were analyzed in SPSS Version 16 using independent t-test, Chi-square, and Fisher's exact test.
RESULTS:
Average severity of hot flashes in both groups and number of hot flashes in black cohosh group in 8th week were significantly lower than 1st week (P < 0.001), but number of hot flashes in primrose oil group in 8th week showed no significant differences (P = 0.32). The number of hot flashes and quality of life score in black cohosh arm compared to EPO showed a significant decrease in the 8th week (P < 0.05). All MENQOL scores were significantly improved in two groups (P < 0.05), but the percentage of improvement in black cohosh arm was significantly superior to EPO group.
CONCLUSION:
Both herbs were effective in reduction of severity of hot flashes and improvement of the quality of life, but it seems that black cohosh is more effective than primrose oil because it was able to reduce the number of hot flashes too.
Keywords: Cimicifuga, evening primrose oil, herbal therapy, hot flashes, menopause
Introduction
Menopause is clinically diagnosed when a previously menstruating woman is amenorrheic for at least 12 months and usually occurs at the age between 45 and 54 years when the ovarian function begins to decrease.[1,2] The health consequences of menopause are associated with vasomotor symptoms such as hot flashes, psychic and somatic disorders, depressed mood, sleeping disorders, physical and emotional distress, skeletal and cardiovascular effects, and urogenital complaints.[1,3] Hot flashes are described as a rapid feeling of exaggerated internal warmth that begins in the chest and rises to the neck and face along with sweating, flushing, and chills. Palpitations and anxiety are not uncommon. Hot flashes frequency is variable, and they may occur several times daily. Hot flashes can have deleterious effects on a woman's work, recreation, sleep, and general quality of life. Estrogen withdrawal appears to trigger hot flashes although the precise neuroendocrine mechanisms have yet to be elucidated.[1,4] Hormone replacement therapy (HRT) is a form of widely used treatment for menopause associated symptoms. However, HRT has been associated with an increased risk of breast cancer and negative cardiovascular consequences.[5,6] Recent clinical studies have demonstrated higher risks for long-term HRT use, particularly for combined estrogen-progestogen therapy started in the late postmenopausal period.[3] Progressive interest in non-hormonal therapies for relief of climacteric symptoms has increased since the publication of adverse effects of estrogen replacement therapy.[7] Many women are turning to herbal medicines and refrain from using HRT because of fear of side effect of hormone therapy.[8] Besides the safety concerns with HRT, about 18% of postmenopausal women do not benefit from HRT in terms of hot flash reduction and about 29% discontinue HRT within 5 months usually due to recurrent menses.[5] Complementary and alternative medicines (CAM) including herb-based therapies are commonly used for treatments of menopausal symptoms. These therapies include herbal remedies such as Cimicifuga racemosa (CR) or black cohosh and evening primrose oil (EPO) (Oenothera biennis L.).[7,9] Racemosa rhizome contains triterpene glycosides, ectoine, 27deoxyactein, cimicifugoside, cytisine, N-methyl cytisine, phenolic acids, flavonoids, volatile oils, tannins and a resinoid material called cimicifugin, which contain 25%–50% of the rhizome substances and other pharmacologically active components. The pharmacological effects of black cohosh may be described as selective estrogen receptor modulator augmented by central nervous effects.[10,11] Furthermore, dopaminergic, serotonergic, and progestogenic effects are proposed.[3] Comprehensive studies have reported the efficacy of CR in the reduction of hot flashes and controlling of vasomotor symptoms with mild side effects and good tolerability and safety.[6,12] EPO is a rich source of gamolenic acid (a precursor of prostaglandin E), popularly believed to suppress menopausal flushing.[13] EPO is obtained from the seeds of Oenothera biennis, a biennial plant. Moreover, EPO may decrease the severity of menopausal hot flashes.[7] It is recognized as a potential source of unsaturated fatty acids.[14]
The objective of this study is to assess the efficacy of CR in comparison with EPO in postmenopausal women with menopause-related symptoms.
Materials and Methods
Study design and subjects
In this randomized, double-blind clinical trial, 80 postmenopausal women with hot flashes who refer to Gynecology Clinic of Fatemieh Hospital (which has the highest number of client), Hamadan, Iran, were randomly assigned into two interventional Groups A and B by simple block randomization.
Intervention
Women gave written informed consent before entry to the study. Participants who had the eligibility criteria were randomized to either the black cohosh, Group A (n = 40) or the EPO group, Group B (n = 40). Drugs were placed in the similar exclusive packets, encoding with A and B. Packets were given to the gynecologist and she opened the packets and read the code of each group. Then, Group A was given 40 mg of black cohosh twice a day and Group B received 500 mg EPO twice a day for 8 continuous weeks.
Study medication
Coated tablets of dried extract of black cohosh root (Cimifugol™) which is produced by Goldaru Pharmaceutical Company contain 20 mg dried extract of cohosh (equal to 0.17–0.18 mg of 27deoxyactein) and EPO capsule manufactured by Barij Essence pharmaceutical company, Iran, with the name of Barij EPO™ as soft capsule containing 1000 mg EPO that is equal to 70–140 mg gamolenic acid (gamma-linolenic acid).
Assessment of menopausal symptoms
The severity and number of hot flashes (day and night) was measured by four-point Likert scale diary of daily hot flashes characteristics (score 1 represents the lowest and 4 the highest severity of hot flashes) for the whole treatment period. The scores for hot flashes and night sweat severity scores were 1: No problem, 2: Mild, sensation of heat without sweating, and no daily task dysfunction, 3: Average, sensation of heat with sweating and low daily task dysfunction, and 4: Severe, extra intense sensation of heat, and sweating with daytime dysfunction. Furthermore, the effect of hot flashes on quality of life was measured by the Menopause-Specific Quality of Life (MENQOL) questionnaire, which is a 29-item validated self-administered instrument comprising four symptom domains: vasomotor (3 items), physical (16 items), psychological (7 items), and sexual (3 items. (The score by domain is the mean of the converted item scores forming that domain and ranges from 1–8. Data from the MENQOL instrument were scored by converting item scores, which range on an ordinal scale of 1–8, score 1 for no symptoms, and 2–8 for the range from least to most bothersome.[15] Obviously, the decline in the total numbers reflects the improvement in women's quality of life. Furthermore, assessment tools included demographic questionnaire and a form for recording any adverse effects such as dizziness, headache, nausea, diarrhea, and vomiting.
The improvement in hot flashes and quality of life was compared between two groups at the pre-intervention phase and weeks 1, 4, and 8 after treatment.
Thus, women were selected who had the following inclusion criteria: 45–60 year-old women, no menstruation during the last year, normal blood pressure, normal kidney and liver function, no abnormal vaginal bleeding, no use of estrogen replacement therapy or herbal drugs for treatment of menopausal symptoms, no use of psychiatric drugs, no use of anticoagulants, no sensitivity to herbal substances, no smoking and alcohol drinking.
Exclusion criteria were history or existence of breast, cervical, or endometrium carcinoma and other serious diseases such as hepatic disease, depression, or hyperthyroidism or other conditions interfering with the study objectives, lack of appropriate use of herbal medicines. Validity of the questionnaire was confirmed by ten faculty members, and test-retest was used for their reliability (r = 0.96).
Ethical considerations
The objectives of the study were explained to the patients, and informed consent was obtained from all participants. Participants could leave the study at any time during the study. The study was approved by the Ethical Committee of Hamadan University of Medical Sciences (approval number: IR. UMSHA. REC.1395.17). Furthermore, the trial was registered with the Iranian registry of clinical trials (IRCT2016041827452N1).
Statistical analysis
Data were analyzed in SPSS Version 16 (SPSS Inc. Released 2007. Chicago) using independent t-test, Chi-square test, and Fisher's exact test. The level of significance was considered lower than 0.05.
Results
This study was conducted on 80 postmenopausal women in two interventional groups. Data collection lasted for 8 weeks without sample loss. Average age of patients in the Group A was 53.72 ± 4.80 years, and average age of Group B was 49.64 ± 10.00 years (P = 0.07). Data analysis reflects the homogeneity of the number of hot flashes (P > 0.05) and severity of them (P = 0.07), and menopause-specific quality of life (P = 0.48) between the two groups before the intervention.
Based on Kruskal-Wallis test result, in the 8th week of treatment, the severity of hot flashes in women treated with black cohosh and EPO significantly decreased in comparison with pre intervention (P < 0.001).
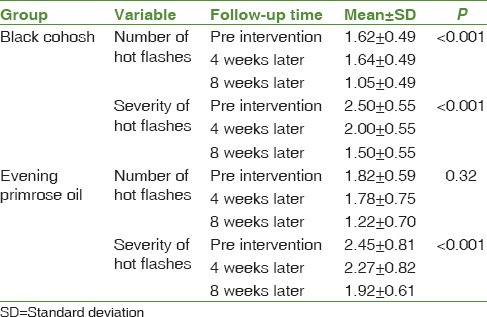
Average severity of hot flashes in both groups and number of hot flashes in black cohosh group in 8th week were significantly lower than 1st week (P < 0.001), but number of hot flashes in EPO group in 8th week showed no significant differences (P = 0.32) [Table 1].
Table 1.
Mean severity and number of hot flashes in terms of follow-up time
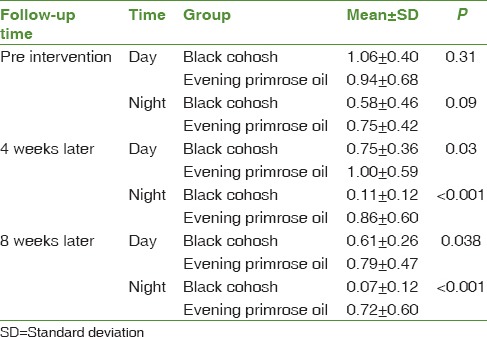
At the beginning of the study, there was no significant difference between the two groups regarding the frequency of hot flashes in the night and day time flushes (P > 0.05). The number of hot flashes score in black cohosh arm compared to EPO showed a significant decrease between the two groups in weeks 4 and 8 (P < 0.05) This indicate the significant superiority of black cohosh to EPO in decreasing the number of hot flashes in the 4th and 8th week of treatment [Table 2].
Table 2.
Mean frequency of hot flashes during the night and day time in terms of follow-up time
All MENQOL scores were significantly improved in two groups after 4 and 8 weeks of treatment (P < 0.001), but the percentage of improvement in black cohosh arm was significantly superior to EPO group [Table 3]. No side effects noted during the study.
Table 3.
Mean Menopause-Specific Quality of Life in terms of follow-up

Discussion
The main objective of this study was determining the effectiveness of black cohosh and EPO on hot flashes and quality of life in postmenopausal women. The results indicate that both black cohosh and primrose oil were effective in reduction of severity of hot flashes and improvement of quality of life, but it seems that black cohosh is more effective than primrose oil because it was able to reduce the number of hot flashes too. The efficacy of black cohosh as a treatment for menopausal symptoms is uncertain; some clinical trials have shown the effectiveness of black cohosh, and some others have not. Treatment by CR in the present study caused a significant reduction in severity and number of hot flashes. The mechanism of black cohosh in alleviating the menopausal symptoms is unclear, several hypotheses have been proposed such as acting as a selective estrogen receptor modulator, acting through serotonergic system as an antioxidant, and inflammatory mechanism.[16]
Many previous studies[11,17,18] reported efficacy of black cohosh especially in the reduction of the number of hot flashes which is consistent with the findings of the present study.
A clinical trial reported that using Black cohosh (6.5 mg of dried extract each day) for 8 weeks can reduce the menopausal symptoms compared with placebo. The treatment efficacy increased with longer use. Black cohosh decreased the Greene climacteric scale's total score and all vasomotor symptoms score during 4 and 8 weeks of treatment.[18] Two other studies that combined black cohosh with other therapies also reported a decrease in symptoms associated with menopause.[19,20] The results of a randomized clinical trial demonstrate that the CR extract can improve the moderate to severe menopausal complaints and it is similar to tibolone in improving the Kupperman Menopausal Index (KMI, measuring mainly neurovegetative symptoms) and even is better than tibolone.[12] In another study, black cohosh was significantly effective in reduction of vasomotor symptoms, especially in reducing the frequency and severity of hot flashes after 12 months treatment.[6] Schellenberg et al. reported a dose-dependent improvement of climacteric symptom severity and quality of life by using extract of Black cohosh.[21] Nevertheless, the results of some studies failed to show efficacy of black cohosh in reducing the frequency of hot flashes which is not in accordance with the results of the present study.[2,3,22,23] However, methodological limitation and variations in product and dosage limit ultimate conclusions. Wuttke and colleagues failed to detect any reduction in hot flash frequency among women taking black cohosh compared with placebo, but they found a statistically significant reduction in the Menopause Rating Scale.[24] Furthermore, a systematic review by Borrelli failed to demonstrate efficacy of black cohosh in the improvement of menopausal symptoms, but a beneficial effect of black cohosh in early menopause was likely.[9] Results of another meta-analysis of clinical trials suggest that there was no significant association between black cohosh treatment and vasomotor symptoms.[25]
According to our finding, application of 8 weeks oral EPO (500 mg twice a day) is effective in reduction of severity of hot flashes and improvement of the quality of life, but it seems that it is not effective in reducing the number of hot flashes. The evening primrose is rich source of omega-6 essential fatty acids such as linoleic acid and gamma-linolenic acid. The therapeutic effects of this herb are attributed to the direct action of its fatty acid ingredients on immune cells, as well as their indirect effect on the synthesis of eicosanoids including prostaglandins, cytokines, and cytokine mediators.[26]
Farzaneh et al. studied the oral intake of EPO (500 mg) during 6 weeks compared with placebo for controlling the symptoms of hot flashes and declared that frequency, severity, and duration of hot flashes improved in evening primrose group, but only severity of hot flashes was significantly better in this arm compared with placebo, which is in line with the findings of our study.[7] The randomized, placebo-controlled study by Chenoy et al. with 35 menopausal women reported that EPO (2000 mg/day) offers no significant benefit over placebo in improving the menopausal hot flashes, sweating, other vasomotor symptoms, and Kupperman menopausal index which is inconsistent with our results. However, the trial was suffered from low sample size.[13] Results of another study confirmed our results and noted that phytoestrogens such as EPO and black cohosh could be the most effective herbs in reducing the menopausal symptoms.[27]
No side effects noted during this study by participants; also, in other studies the CR is considered as a safe drug.[11,18,22] However, the most probable side effects are mild gastric symptoms, which tend to disappear after a while. Headaches, vomiting, and dizziness may occur by using high doses.[6] Slight side effects of the EPO such as nausea was reported by Chenoy et al.[13], but in another study, it was mentioned that using this herb in patients with epilepsy may increase the risk of seizure.[28]
The research presented in this article has some limitations including the small sample size of the study, lack of a placebo group, and short study period. Further studies in larger sample sizes and longer study duration are needed to confirm these results. We ignored to do so because of budget constraints.
Conclusion
According to the results of this study, both black cohosh and primrose oil can be used as an effective alternative treatment in relieving of severity of hot flashes and improvement of quality of life in menopausal period, but it seems that black cohosh is more effective than primrose oil because it was able to reduce the number of hot flashes too.
Financial support and sponsorship
Financial support of this study (No.9504221994) was provided by vice-chancellor for research and technology, Hamadan University of Medical Sciences, Hamadan, Iran.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This paper is part of the thesis of Mr. Fallahian for the degree of doctor of pharmacy. The authors sincerely acknowledge the Hamadan University of Medical Sciences in Iran for their valuable support and participation. Hereby, the authors would like to gratefully thank the patients participating in the study.
References
- 1.Bordeleau L, Pritchard K, Goodwin P, Loprinzi C. Therapeutic options for the management of hot flashes in breast cancer survivors: An evidence-based review. Clin Ther. 2007;29:230–41. doi: 10.1016/j.clinthera.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 2.Borrelli F, Ernst E. Black cohosh (Cimicifuga racemosa) for menopausal symptoms: A systematic review of its efficacy. Pharmacol Res. 2008;58:8–14. doi: 10.1016/j.phrs.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 3.Frei-Kleiner S, Schaffner W, Rahlfs VW, Bodmer CH, Birkhäuser M. Cimicifuga racemosa dried ethanolic extract in menopausal disorders: A double-blind placebo-controlled clinical trial. Maturitas. 2005;51:397–404. doi: 10.1016/j.maturitas.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 4.Freedman RR. Menopausal hot flashes: Mechanisms, endocrinology, treatment. J Steroid Biochem Mol Biol. 2014;142:115–20. doi: 10.1016/j.jsbmb.2013.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guttuso T Jr. Effective and clinically meaningful non-hormonal hot flash therapies. Maturitas. 2012;72:6–12. doi: 10.1016/j.maturitas.2012.01.023. [DOI] [PubMed] [Google Scholar]
- 6.Nasr A, Nafeh H. Influence of black cohosh (Cimicifuga racemosa) use by postmenopausal women on total hepatic perfusion and liver functions. Fertil Steril. 2009;92:1780–2. doi: 10.1016/j.fertnstert.2009.05.038. [DOI] [PubMed] [Google Scholar]
- 7.Farzaneh F, Fatehi S, Sohrabi MR, Alizadeh K. The effect of oral evening primrose oil on menopausal hot flashes: A randomized clinical trial. Arch Gynecol Obstet. 2013;288:1075–9. doi: 10.1007/s00404-013-2852-6. [DOI] [PubMed] [Google Scholar]
- 8.Yousefi Z, Abdollahpour N, Ghazanfarpour M, Sadeghi R, Pourmoghadam N. Impacts of herbal medicines on hot flash: A systematic review. J Med Plants. 2016;3:40–6. [Google Scholar]
- 9.Borrelli F, Ernst E. Alternative and complementary therapies for the menopause. Maturitas. 2010;66:333–43. doi: 10.1016/j.maturitas.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 10.Borrelli F, Ernst E. Black cohosh (Cimicifuga racemosa): A systematic review of adverse events. Am J Obstet Gynecol. 2008;199:455–66. doi: 10.1016/j.ajog.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 11.Shahnazi M, Nahaee J, Mohammad-Alizadeh-Charandabi S, Bayatipayan S. Effect of black cohosh (Cimicifuga racemosa) on vasomotor symptoms in postmenopausal women: A randomized clinical trial. J Caring Sci. 2013;2:105–13. doi: 10.5681/jcs.2013.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bai W, Henneicke-von Zepelin HH, Wang S, Zheng S, Liu J, Zhang Z, et al. Efficacy and tolerability of a medicinal product containing an isopropanolic black cohosh extract in chinese women with menopausal symptoms: A randomized, double blind, parallel-controlled study versus tibolone. Maturitas. 2007;58:31–41. doi: 10.1016/j.maturitas.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 13.Chenoy R, Hussain S, Tayob Y, O'Brien PM, Moss MY, Morse PF, et al. Effect of oral gamolenic acid from evening primrose oil on menopausal flushing. BMJ. 1994;308:501–3. doi: 10.1136/bmj.308.6927.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Granica S, Czerwińska ME, Piwowarski JP, Ziaja M, Kiss AK. Chemical composition, antioxidative and anti-inflammatory activity of extracts prepared from aerial parts of Oenothera biennis L.and Oenothera paradoxa Hudziok obtained after seeds cultivation. J Agric Food Chem. 2013;61:801–10. doi: 10.1021/jf304002h. [DOI] [PubMed] [Google Scholar]
- 15.Wathen CN. Alternatives to hormone replacement therapy: A multi-method study of women's experiences. Complement Ther Med. 2006;14:185–92. doi: 10.1016/j.ctim.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 16.Ruhlen RL, Sun GY, Sauter ER. Black cohosh: Insights into its mechanism(s) of action. Integr Med Insights. 2008;3:21–32. [PMC free article] [PubMed] [Google Scholar]
- 17.Dog TL. Menopause: A review of botanical dietary supplements. Am J Med. 2005;118:98–108. doi: 10.1016/j.amjmed.2005.09.044. [DOI] [PubMed] [Google Scholar]
- 18.Mohammad-Alizadeh-Charandabi S, Shahnazi M, Nahaee J, Bayatipayan S. Efficacy of black cohosh (Cimicifuga racemosa L.) in treating early symptoms of menopause: A randomized clinical trial. Chin Med. 2013;8:20. doi: 10.1186/1749-8546-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chung DJ, Kim HY, Park KH, Jeong KA, Lee SK, Lee YI, et al. Black cohosh and st. John's wort (GYNO-Plus®) for climacteric symptoms. Yonsei Med J. 2007;48:289–94. doi: 10.3349/ymj.2007.48.2.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rotem C, Kaplan B. Phyto-female complex for the relief of hot flushes, night sweats and quality of sleep: Randomized, controlled, double-blind pilot study. Gynecol Endocrinol. 2007;23:117–22. doi: 10.1080/09513590701200900. [DOI] [PubMed] [Google Scholar]
- 21.Schellenberg R, Saller R, Hess L, Melzer J, Zimmermann C, Drewe J, et al. Dose-dependent effects of the Cimicifuga racemosa extract ze 450 in the treatment of climacteric complaints: A Randomized, placebo-controlled study. Evid Based Complement Alternat Med. 2012;2012:260301. doi: 10.1155/2012/260301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Geller SE, Shulman LP, van Breemen RB, Banuvar S, Zhou Y, Epstein G, et al. Safety and efficacy of black cohosh and red clover for the management of vasomotor symptoms: A randomized controlled trial. Menopause. 2009;16:1156–66. doi: 10.1097/gme.0b013e3181ace49b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leach MJ, Moore V. Black cohosh (Cimicifuga spp.) for menopausal symptoms. The Cochrane database of systematic reviews. 2012;9 doi: 10.1002/14651858.CD007244.pub2. Cd007244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wuttke W, Seidlová-Wuttke D, Gorkow C. The cimicifuga preparation BNO 1055 vs. conjugated estrogens in a double-blind placebo-controlled study: Effects on menopause symptoms and bone markers. Maturitas. 2003;44(Suppl 1):S67–77. doi: 10.1016/s0378-5122(02)00350-x. [DOI] [PubMed] [Google Scholar]
- 25.Franco OH, Chowdhury R, Troup J, Voortman T, Kunutsor S, Kavousi M, et al. Use of plant-based therapies and menopausal symptoms: A Systematic review and meta-analysis. JAMA. 2016;315:2554–63. doi: 10.1001/jama.2016.8012. [DOI] [PubMed] [Google Scholar]
- 26.Bayles B, Usatine R. Evening primrose oil. Am Fam Physician. 2009;80:1405–8. [PubMed] [Google Scholar]
- 27.van der Sluijs CP, Bensoussan A, Liyanage L, Shah S. Women's health during mid-life survey: The use of complementary and alternative medicine by symptomatic women transitioning through menopause in sydney. Menopause. 2007;14:397–403. doi: 10.1097/01.gme.0000236937.36078.f4. [DOI] [PubMed] [Google Scholar]
- 28.Rouhi-Boroujeni H, Rouhi-Boroujeni H, Gharipour M, Mohammadizadeh F, Ahmadi S, Rafieian-Kopaei M, et al. Systematic review on safety and drug interaction of herbal therapy in hyperlipidemia: A guide for internist. Acta Biomed. 2015;86:130–6. [PubMed] [Google Scholar]


