The most recent guidelines for the management of Barrett's oesophagus published in 2014 recommended endoscopic surveillance for patient with histological evidence of low-grade dysplasia (LGD) on random biopsies.1 In the last 2 years, new evidence on the natural history of LGD in Barrett's oesophagus and on the safety and efficacy of endoscopic treatment in this subgroup of patients has been published.
Duits et al have conducted a retrospective analysis of 293 patients with LGD diagnosed in community hospitals.2 Following consensus review, the original LGD diagnosis was confirmed in 27% of cases, while the remaining of the cases were downgraded to non-dysplastic Barrett's oesophagus or indefinite for dysplasia (IND). Patients with a LGD consensus diagnosis had a progression rate to high-grade dysplasia (HGD) or cancer of 9.1%/year over a median follow-up of 39 months. By contrast, patients whose diagnosis was down-staged to either non-dysplastic Barrett's oesophagus or IND had a conversion rate of 0.6% and 0.9%/year, respectively (evidence grade: low). This study reiterates the difficulty in making a pathological diagnosis of LGD, but also shows that confirmation by an expert pathologist from a different institution associates with a substantially higher risk of progression. In keeping with this study, a recent meta-analysis found that studies on cohorts with a low LGD/non-dysplastic Barrett's oesophagus ratios (<0.15), indicative of a more stringent and robust dysplasia diagnosis, reported a significantly higher annual incidence of cancer (0.76%, 95% CI 0.45% to 1.07%) compared with studies with a ratio >0.15, where many LGD cases were likely overdiagnosed (0.32%; 95% CI 0.07% to 0.58%) (evidence grade: low).3
With regard to endoscopic treatment, a recent multicentre randomized controlled trial compared the outcome of 68 patients with LGD treated with radiofrequency ablation (RFA) with an equal number of patients undergoing annual endoscopic surveillance.4 The main inclusion criterion was a diagnosis of LGD confirmed by a central pathologist with extensive experience in Barrett's oesophagus. Over a 3-year follow-up period, 1% of patients in the treatment arm progressed to HGD or cancer, compared with 26.5% in the control arm (p<0.001) (evidence grade: high). Complete eradication of dysplasia and intestinal metaplasia by RFA was achieved in 98% and 90%, respectively. The most common complication was stricture, which occurred in 12% of patients, but this was successfully managed in all patients with endoscopic dilatation.
Taken together, the new published data suggest that a consensus diagnosis of LGD by independent pathologists correlates with a significant risk of progression to HGD/cancer and that RFA significantly reduces this risk. This strongly indicates that endoscopic ablation, preferably with RFA, is an appropriate treatment for Barrett's oesophagus with LGD (figure 1). Due to the considerable diagnostic difficulties, LGD should be diagnosed and confirmed by an expert GI pathologist in at least two endoscopes. Treatment options should be discussed by an upper GI multidisciplinary team (MDT) to ensure pathology review and assess patient fitness and endoscopic therapy should be restricted to high volume centres as per main 2014 guidelines. As noted in the current guidelines, p53 immunohistochemistry can be a useful diagnostic adjunct.
Figure 1.
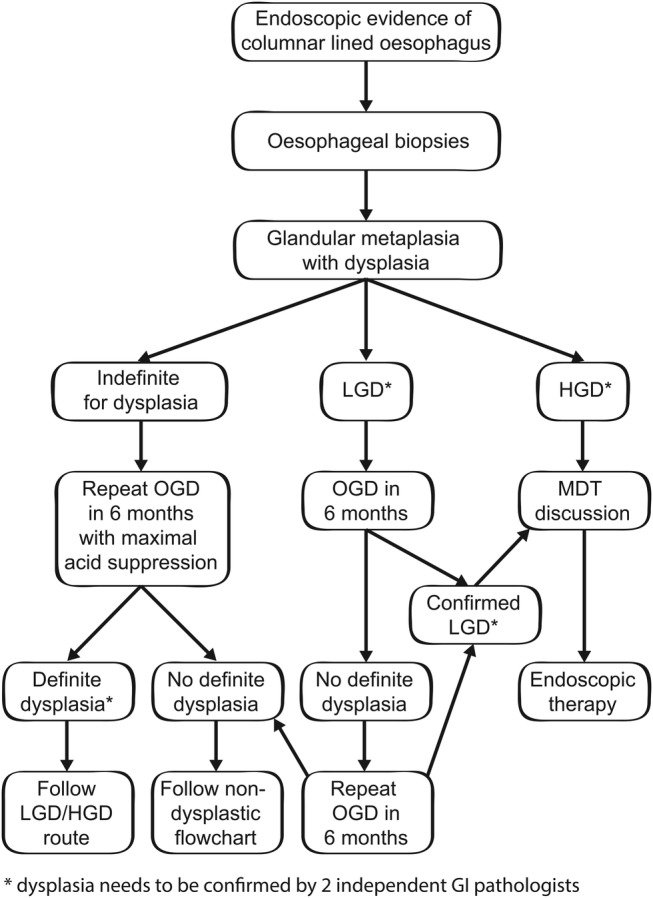
Updated flow chart for the management of dysplastic Barrett's oesophagus. A pathological finding of indefinite for dysplasia does not exclude the presence of dysplasia; therefore, a 6-month follow-up is warranted. Endoscopic follow-up in 6 months is recommended for LGD. If LGD is also found at follow-up endoscopy, even if not consecutive, provided that the diagnosis of dysplasia on two occasions is confirmed by two independent GI pathologists (ideally from a different institution), endoscopic ablation should be considered. A diagnosis of high-grade dysplasia (HGD) also needs to be confirmed by a second GI pathologist. Patients with dysplasia should be offered endoscopic therapy following discussion within MDT setting. LGD, low-grade dysplasia; HGD, high-grade dysplasia; MDT, multidisciplinary team; OGD, oesophagogastroduodenoscopy.
Therefore, the new recommendation on the management of LGD in Barrett's oesophagus is:
Patients with LGD should have a repeat endoscopy in 6 months' time. If LGD is found in any of the follow-up oesophagogastroduodenoscopy and is confirmed by an expert GI pathologist in at least two sets of biopsies, the patient should be offered endoscopic ablation therapy, preferably with RFA, after review by the specialist MDT. If ablation is not undertaken, 6-monthly surveillance is recommended (recommendation grade A for endoscopic therapy and C for surveillance). Agreement: A+ 56%, A 33%, U 0%, D 11%, D+ 0%.
Footnotes
Twitter: Follow Massimiliano Di Pietro @massi_dipietro
Contributors: MdP has led on the Delphi process, written the manuscript and produced the figure. RCF has written the manuscript.
Competing interests: RCF developed the Cytosponge technology, which has been licensed by MRC-Technology to Medtronic. MdP received educational grants from Medtronic.
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1. Fitzgerald RC, Di Pietro M, Ragunath K, et al. . British Society of Gastroenterology guidelines on the diagnosis and management of Barrett's oesophagus. Gut 2014;63:7–42. 10.1136/gutjnl-2013-305372 [DOI] [PubMed] [Google Scholar]
- 2. Duits LC, Phoa KN, Curvers WL, et al. . Barrett's oesophagus patients with low-grade dysplasia can be accurately risk-stratified after histological review by an expert pathology panel. Gut 2015;64:700–6. 10.1136/gutjnl-2014-307278 [DOI] [PubMed] [Google Scholar]
- 3. Singh S, Manickam P, Amin AV, et al. . Incidence of esophageal adenocarcinoma in Barrett's esophagus with low-grade dysplasia: a systematic review and meta-analysis. Gastrointest Endosc 2014;79:897–909.e4; quiz 983.e1, 983.e3 e4 10.1016/j.gie.2014.01.009 [DOI] [PubMed] [Google Scholar]
- 4. Phoa KN, Van Vilsteren FGI, Weusten BLAM, et al. . Radiofrequency ablation vs endoscopic surveillance for patients with Barrett esophagus and low-grade dysplasia: a randomized clinical trial. JAMA 2014;311:1209–17. 10.1001/jama.2014.2511 [DOI] [PubMed] [Google Scholar]


