Abstract
There is growing recognition of the importance of understanding the nature of the associations between anxiety and cardiovascular disease (CVD), although limited research has examined mechanisms that may explain the anxiety-CVD link. Anxiety sensitivity (fear of anxiety-relevant somatic sensations) is a cognitive-affective risk factor implicated in the development of anxiety psychopathology and various behavioral risk factors for CVD, although has not been examined among individuals with CVD. Adult daily smokers (n = 619; 50.9% female; Mage = 44.0, SD = 13.67) completed an online survey that included the Anxiety Sensitivity Index-3 (ASI-3) and the Patient Health Questionnaire (PHQ). The presence of CVD was assessed via the presence of ≥ 1 of the following: heart attack, heart murmur, positive stress test, heart valve abnormality, angina, and heart failure. Smokers with CVD indicators (n = 66, 10.7%) had significantly higher scores on the ASI-3 (M = 33.5, SD = 22.15), relative to smokers without CVD (M = 22.0, SD = 17.92; Cohen’s d = .57). Those with CVD were significantly more likely to have moderate or high anxiety sensitivity (66.7%) relative to those without CVD (49.4%). Physical and social concerns about the meaning of somatic sensations were common among smokers with CVD.
Keywords: anxiety, nicotine dependence, cardiac, anxiety sensitivity
Introduction
Cardiovascular disease (CVD) is the leading cause of death in the United States (CDCP, 2014; Go et al., 2013). Anxiety disorders in patients with CVD increase the risk of mortality and recurrence of cardiac events by approximately two-fold (Edmondson et al., 2012; Tully, Cosh, & Baumeister, 2014). The associations between anxiety, CVD, and the perpetuation of these disease processes are likely (a) transactional and (b) occur directly and indirectly via shared bio-psychological vulnerability processes. One potential underlying psychological risk factor is anxiety sensitivity, defined as the extent to which individuals believe anxiety and anxiety-related sensations have harmful consequences (Reiss, Peterson, Gursky, & McNally, 1986). Anxiety sensitivity is a risk factor for the acquisition and maintenance of anxiety psychopathology (Olatunji & Wolitzky-Taylor, 2009), and while it is conceptualized as a relatively stable dispositional factor, anxiety sensitivity is malleable and serves as an explanatory mechanism in the treatment of anxiety (Smits, Berry, Rosenfield, et al., 2008; Smits, Berry, Tart, & Powers, 2008).
Theoretically, anxiety sensitivity may be elevated among individuals with CVD due to increased presence of physiological and autonomic disturbance (Kemp et al., 2012; Tully, Cosh, & Baune, 2013), which may serve as a prominent cue for perceived danger and risk (Jeejeebhoy, Dorian, & Newman, 2000; Korczak, Goldstein, & Levitt, 2007). Indeed, among non-cardiac patients, anxiety sensitivity is associated with greater cardiopulmonary fears (e.g., Aikens, Zvolensky, & Eifert, 2001). It is possible that anxiety sensitivity may contribute to risk for CVD through engagement in various health risk behaviors, like cigarette smoking (Leventhal & Zvolensky, 2015), emotional and binge eating (Anestis, Holm-Denoma, Gordon, Schmidt, & Joiner, 2008; Hearon, Utschig, Smits, Moshier, & Otto, 2013), and physical inactivity (Moshier, Szuhany, Hearon, Smits, & Otto, 2016). In addition, anxiety sensitivity may have a direct effect on CVD. For example, higher anxiety sensitivity is associated with increased likelihood carotid plaques and arterial stiffness among individuals without CVD (Seldenrijk et al., 2013). To our knowledge, no published studies to date have assessed anxiety sensitivity among individuals with CVD. Thus, the current study aimed to characterize the nature of anxiety sensitivity among smokers with self-reported indicators of CVD.
Prior data indicate that smokers report greater fear about cardiac sensations than non-smokers, and the combination of smoking and coronary artery disease (compared to ether alone) is associated with increased cognitive bias to cardiac sensations, even after adjusting for cardiac pain severity (Zvolensky, Eifert, Feldner, & Leen-Feldner, 2003). Therefore, we hypothesized that community-recruited smokers with CVD would have higher levels of anxiety sensitivity relative to smokers without CVD.
Method
Participants and Procedure
Participants (n=619; 50.9% female) were daily smokers who recruited through Qualtrics Online Sample for an anonymous study on smoking and health. Participants were included on the following criteria: (a) ≥18 years of age, (b) daily smoking for ≥1 year, (c) smoking ≥5 cigarettes/day, and (d) cigarettes as primary tobacco product. Participants were excluded if they reported reduced smoking rate by more than half in the past 6 months. The survey was approximately 40 minutes in length. Cases were retained on the basis of accurately answering four imbedded validity ‘check’ questions. The study protocol was approved by the Institutional Review Board where the study was conducted.
Measures
Items from the Smoking History Questionnaire (SHQ; Brown, Lejuez, Kahler, & Strong, 2002) were used to describe the sample in terms of smoking. Cardiovascular disease and risk factors were assessed via a medical checklist of 34 different health conditions (yes/no). Six items were used to index presence of CVD: heart attack, heart murmur, positive stress test, heart valve abnormality, angina, and heart failure. The presence of ≥1 of these conditions was used to indicate CVD. Several health risk factors for CVD were also assessed including presence of high blood pressure, high cholesterol, and diabetes (yes/no). Body Mass Index (BMI) was calculated based on self-reported weight and height as an index of body weight ([weight(lbs)/[height (in)]2 x 703]; WHO, 2002). The International Physical Activity Questionnaire (IPAQ; Craig et al., 2003) was used to denote average weekly number of moderate-to-vigorous physical activity minutes and sedentary time. The Patient Health Questionnaire (PHQ; Spitzer, Kroenke, & Williams, 1999) is a self-report assessment that was used to assess the presence/absence of common DSM-IV Axis I disorders (Spitzer et al., 1999). The Anxiety Sensitivity Index-3 (ASI-3; Taylor et al., 2007) is an 18-item psychometrically-sound self-report measure of anxiety sensitivity. Responses are rated on a five-point Likert scale ranging from 0 (very little) to 4 (very much) and summed to create a total score (possible range 0–72) and three subscale scores (possible range 0–24) reflecting physical, cognitive, and social consequences of anxiety sensations. The ASI-3 is validated in smokers (Farris et al., 2015) and clinical cut-scores ≥17 indicate at least moderate anxiety sensitivty (Allan et al., 2014). Cronbach’s alphas ranged from .87–.96 for total and subscale items.
Data Analytic Procedures
Inferential statistics were used to examine differences between smokers with and without CVD. Welch-Satterthwaite degrees of freedom were used in analyses where non-homogeneous variances were observed. Cohen’s d and odds ratios were computed to index standardized effect sizes.
Results
The presence of CVD was 10.7% (n = 66). The majority of participants with CVD had only one indictor (74.2%), with an average of 1.3 (range 1–4). Differences in demographic, smoking, and health factors by CVD group is presented in Table 1. Smokers with CVD (relative to those without) had significantly higher levels of tobacco dependence, smoked longer, and were more likely to have high cholesterol, high triglycerides and diabetes.
Table 1.
Demographic, health, and psychiatric characteristics among smokers with and without a history of CVD
| Variable | Total (n = 619) | CVD (n = 66) | Non-CVD (n = 553) | t(df) or x2 |
|---|---|---|---|---|
| Demographics | ||||
| Gender (female) | 315 (50.9%) | 35 (53.0%) | 280 (50.6%) | .14 |
| Age | 44.0 (13.66) | 47.2 (13.48) | 43.6 (13.65) | −2.01(617)* |
| Race (non-white) | 68 (11.0%) | 4 (6.1%) | 64 (11.6%) | 1.83 |
| Ethnicity (Hispanic) | 46 (7.4%) | 7 (10.6%) | 39 (7.1%) | 1.08 |
| Marital Status (married) | 319 (51.5%) | 36 (54.5%) | 283 (51.2%) | .27 |
| Education (≥ part college) | 446 (72.1%) | 46 (69.7%) | 400 (72.3%) | .20 |
| Employment (full time) | 318 (51.4%) | 24 (36.4%) | 294 (53.2%) | 6.66** |
| Income (≥ $50,000) | 215 (40.1%) | 19 (33.9%) | 196 (40.8%) | .99 |
| Smoking Characteristics | ||||
| Years smoking | 25.4 (14.25) | 29.1 (15.09) | 25.0 (14.09) | −2.25(617)* |
| Cigarettes/day (past week) | 17.0 (8.31) | 18.3 (9.45) | 16.8 (8.16) | −1.44 |
| Tobacco Dependence (FTND) | 5.4 (1.97) | 6.1 (1.75) | 5.3 (1.98) | −3.72(86.1)*** |
| Health Risk Indicators | ||||
| Body Mass Index | 27.9 (7.34) | 27.8 (7.24) | 27.9 (7.36) | .13(587) |
| High Cholesterol (Yes) | 113 (18.3%) | 21 (31.8%) | 92 (16.6%) | 9.11** |
| High Triglycerides (Yes) | 108 (17.4%) | 21 (31.8%) | 87 (15.7%) | 10.59** |
| Diabetes (Yes) | 57 (9.2%) | 13 (19.7%) | 44 (8.0%) | 9.72** |
| MVPA (minutes/wk) | 251.3 (448.56) | 215.5 (345.20) | 255.5 (459.41) | 0.69 |
| Sedentary time (hours) | 7.9 (4.31) | 8.2 (4.64) | 7.9 (4.37) | −0.62 |
| PHQ Diagnosis n(%) | ||||
| Major Depression | 79 (12.8%) | 22 (33.3%) | 57 (10.3%) | 28.08*** |
| Panic Attack | 87 (14.1%) | 16 (24.2%) | 71 (12.8%) | 6.35* |
| Other Anxiety | 69 (11.1%) | 17 (25.8%) | 52 (9.4%) | 15.92*** |
| Eating Disorder | 29 (4.7%) | 5 (7.6%) | 24 (4.3%) | 1.38 |
| Alcohol Abuse | 107 (17.3%) | 21 (31.8%) | 86 (15.6%) | 10.91** |
p < .05,
p<.01,
p<.001; df in parenthesis;
CVD = Cardiovascular disease; MVPA = Moderate-to-vigorous physical activity
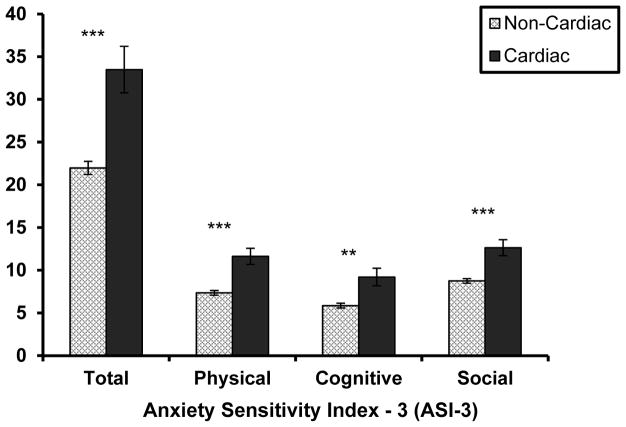
The percentage of those that screened positive for a psychiatric disorder is presented in Table 2. Smokers with CVD, relative to those without, were significantly more likely to have major depression, panic attacks, other (generalized) anxiety, and alcohol abuse, but were not significantly more likely to have an eating disorder. See Table 2 and Figure 1 for ASI-3 results. The shared variance between ASI-3 and having any PHQ diagnoses was 18.5%. Scores on the ASI-3 were significantly higher among smokers with CVD, compared to smokers without. Smokers with CVD were significantly more likely to have moderate or high anxiety sensitivity (66.7%) relative to those without CVD (49.4%). The ASI-3 Physical and Social concerns subscales had the largest sized effects. An examination of item-level data (see Table 3) indicated that three items from the Physical concerns subscale (#3, 8, 12) had the largest differences by CVD status. These items reflect specific concern about cardiac related symptoms. Additionally, three items from the Cognitive concerns subscale (#6, 9, 13) demonstrated the largest differences by CVD status. These items reflect fear/worry that others will notice anxiety sensations.
Table 2.
ASI-3 and Psychiatric Disorders by CVD status
| Dimensional M(SD) | Total (n = 619) | CVD (n = 66) | Non-CVD (n = 553) | t(df) | d |
|---|---|---|---|---|---|
| ASI-3 Total | 23.2 (18.73) | 33.5 (22.15) | 22.0 (17.92) | −4.07(75.5)*** | 0.57 |
| ASI-3 Physical | 7.8 (6.82) | 11.6 (7.69) | 7.4 (6.57) | −4.34(76.8)*** | 0.59 |
| ASI-3 Cognitive | 6.2 (6.91) | 9.2 (8.34) | 5.9 (6.64) | −3.15(75.2)** | 0.44 |
| ASI-3 Social | 9.2 (6.55) | 12.7 (7.62) | 8.8 (6.29) | −3.99(76.0)*** | 0.56 |
|
| |||||
| Categorical n(%) | ASI-3 M (SD) | Total (n = 619) | CVD (n = 66) | Non-CVD (n = 553) | x2 |
|
| |||||
| Moderate-High AS (≥17) | 38.1 (14.46) | 317 (51.2%) | 44 (66.7%) | 273 (49.4%) | 7.06** |
| ’Normative’ AS (<17) | 7.6 (4.70) | 302 (48.8%) | 22 (33.3%) | 280 (50.6%) | |
p<.05,
p<.01,
p<.001
Figure 1.
Anxiety Sensitivity Index-3 (ASI-3) by smokers with and without CVD indicators
Table 3.
Anxiety Sensitivity Index-3 (ASI-3) item averages by CVD status
|
|
|||||
|---|---|---|---|---|---|
| CVD | Non-CVD | Cohen’s d | |||
|
| |||||
| Anxiety Sensitivity Index-3 (ASI-3) | M | SD | M | SD | |
| Physical Subscale | |||||
| 3. It scares me when my heart beats rapidly. | 2.5 | 1.43 | 1.7 | 1.32 | 0.58 |
| 4. When my stomach is upset, I worry that I might be seriously ill. | 1.4 | 1.45 | 0.9 | 1.21 | 0.37 |
| 7. When my chest feels tight, I get scared that I won’t be able to breathe properly. | 2.1 | 1.59 | 1.5 | 1.40 | 0.40 |
| 8. When I feel pain in my chest, I worry that I’m going to have a heart attack. | 2.4 | 1.47 | 1.4 | 1.39 | 0.70 |
| 12. When I notice my heart skipping a beat, I worry that there is something seriously wrong with me. | 1.8 | 1.38 | 1.1 | 1.36 | 0.51 |
| 15. When my throat feels tight, I worry that I could choke to death. | 1.4 | 1.68 | 0.7 | 1.17 | 0.48 |
| Cognitive Subscale | |||||
| 2. When I cannot keep my mind on a task, I worry that I might be going crazy. | 1.5 | 1.53 | 1.0 | 1.32 | 0.35 |
| 5. It scares me when I am unable to keep my mind on a task. | 1.8 | 1.51 | 1.2 | 1.30 | 0.43 |
| 10. When I feel “spacey” or spaced out I worry that I may be mentally ill. | 1.3 | 1.53 | 0.8 | 1.24 | 0.36 |
| 14. When my thoughts seem to speed up, I worry that I might be going crazy. | 1.4 | 1.57 | 0.9 | 1.28 | 0.35 |
| 16. When I have trouble thinking clearly, I worry that there is something wrong with me. | 1.6 | 1.47 | 1.0 | 1.25 | 0.44 |
| 18. When my mind goes blank, I worry there is something terribly wrong with me. | 1.5 | 1.50 | 0.9 | 1.25 | 0.43 |
| Social Subscale | |||||
| 1. It is important for me not to appear nervous. | 2.7 | 1.25 | 2.3 | 1.26 | 0.32 |
| 6. When I tremble in the presence of others, I fear what people will think of me | 2.0 | 1.46 | 1.2 | 1.38 | 0.56 |
| 9. I worry that other people will notice my anxiety. | 2.1 | 1.70 | 1.3 | 1.42 | 0.51 |
| 11. It scares me when I blush in front of people. | 1.4 | 1.55 | 0.8 | 1.20 | 0.43 |
| 13. When I begin to sweat in a social situation, I fear people will think negatively of me. | 2.0 | 1.56 | 1.2 | 1.37 | 0.54 |
| 17. I think it would be horrible for me to faint in public. | 2.6 | 1.53 | 1.9 | 1.53 | 0.46 |
Note: All means are statistically significant. Effect sizes ≥.5 reflecting medium size effects are in bold.
Discussion
Anxiety sensitivity was significantly higher among smokers with CVD relative to those without (medium-sized differences): 66.7% of those with CVD had high anxiety sensitivity relative to 49.4% in those without CVD. Items on the ASI-3 reflecting concern about physical consequences of cardiac-related anxiety sensations may be uniquely prominent among individuals with CVD. Individuals with CVD, relative to those without, also had higher average scores on items reflecting concerns about the social consequences of experiencing somatic sensations. Such concerns may drive avoidance of certain health behaviors due to embarrassment (e.g., exercising in public; Clark et al., 2013).
Generalized anxiety/worry is linked to adaptive health behaviors (Meyer, Hussein, Lange, & Herrmann-Lingen, 2015; Parker, Hyett, Hadzi-Pavlovic, Brotchie, & Walsh, 2011), potentially due to increase vigilance to health which may prompt individuals to seek medical care. However, excessive worry and fear of bodily sensations (including cardiac sensations) and the formulation of inaccurate assumptions about the meaning of such sensations may increase subjective cardiac pain/symptoms (Zvolensky et al., 2003) which may lead to maladaptive responses (e.g., non-attendance/compliance with cardiac rehabilitation due to uncomfortable bodily sensations elicited why exercising). Simply being aware of bodily sensations is not the same as catastrophically interpreting the sensations. More work is needed to understand the nuances of awareness, cognitive interpretation/ misappraisal, and behavioral responses to bodily sensations among individuals with CVD.
There are several limitations to the current study. First, CVD was determined by self-reported presence of one of six indicators, thus was a crude assessment of CVD presence that does not capture severity of CVD. The results require replication in clinical samples of individuals with diagnosed CVD, and also take into account heterogeneity in CVD. Second, the pattern of results is likely not be unique to cigarette smokers and should be explored in other more representative sample of individuals with CVD. Third, all data were self-reported and collected via an online platform. Lastly, the sample was primarily white, well-educated, and had fairly high annual household income, thus the generalizability of these findings to more heterogeneous samples may be limited.
The tendency to be fearful of bodily sensations (anxiety sensitivity) appears to be prominent in individual with CVD and may therefore be an important target for treatment. Facilitating decreased emotional reactivity (i.e., fear) and increase adaptive responding to bodily sensations (Smits et al., 2008) could decrease subjective cardiac symptom severity and promote health protective behaviors (e.g., physical activity) for CVD patients.
References
- Aikens JE, Zvolensky MJ, Eifert GH. Differential fear of cardiopulmonary sensations in emergency room noncardiac chest pain patients. Journal of Behavioral Medicine. 2001;24(2):155–167. doi: 10.1023/a:1010710614626. [DOI] [PubMed] [Google Scholar]
- Allan NP, Raines AM, Capron DW, Norr AM, Zvolensky MJ, Schmidt NB. Identification of anxiety sensitivity classes and clinical cut-scores in a sample of adult smokers: Results from a factor mixture model. Journal of Anxiety Disorders. 2014;28(7):696–703. doi: 10.1016/j.janxdis.2014.07.006. http://doi.org/10.1016/j.janxdis.2014.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anestis MD, Holm-Denoma JM, Gordon KH, Schmidt NB, Joiner TE. The role of anxiety sensitivity in eating pathology. Cognitive Therapy and Research. 2008;32(3):370–385. http://doi.org/10.1007/s10608-006-9085-y. [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR. Distress tolerance and duration of past smoking cessation attempts. Journal of Abnormal Psychology. 2002;111(1):180–5. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11866171. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Summary Health Statistics: National Health Interview Survey. 2014. [Google Scholar]
- Clark AM, King-Shier KM, Spaling MA, Duncan AS, Stone JA, Jaglal SB, … Angus JE. Factors influencing participation in cardiac rehabilitation programmes after referral and initial attendance: qualitative systematic review and meta-synthesis. Clinical Rehabilitation. 2013;27(10):948–959. doi: 10.1177/0269215513481046. http://doi.org/10.1177/0269215513481046. [DOI] [PubMed] [Google Scholar]
- Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Medicince, Science, and Sport Exercise. 2003;35(8):1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- Edmondson D, Richardson S, Falzon L, Davidson KW, Mills MA, Neria Y, … Williams J. Posttraumatic stress disorder prevalence and risk of recurrence in acute coronary syndrome patients: A meta-analytic review. PLoS ONE. 2012;7(6):e38915. doi: 10.1371/journal.pone.0038915. http://doi.org/10.1371/journal.pone.0038915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farris SG, DiBello AM, Allan NP, Hogan J, Schmidt NB, Zvolensky MJ. Evaluation of the Anxiety Sensitivity Index-3 among treatment-seeking smokers. Psychological Assessment. 2015;27(3):1123–8. doi: 10.1037/pas0000112. http://doi.org/10.1037/pas0000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, … Turner MB. Heart disease and stroke statistics-2013 update: A Report from the American Heart Association. Circulation. 2013;127(1) doi: 10.1161/CIR.0b013e31828124ad. http://doi.org/10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hearon BA, Quatromoni PA, Mascoop JL, Otto MW. The role of anxiety sensitivity in daily physical activity and eating behavior. Eating Behaviors. 2014;15(2):255–8. doi: 10.1016/j.eatbeh.2014.03.007. http://doi.org/10.1016/j.eatbeh.2014.03.007. [DOI] [PubMed] [Google Scholar]
- Hearon BA, Utschig AC, Smits JAJ, Moshier SJ, Otto MW. The role of anxiety sensitivity and eating expectancy in maladaptive eating behavior. Cognitive Therapy and Research. 2013;37(5):923–933. http://doi.org/10.1007/s10608-012-9491-2. [Google Scholar]
- Jeejeebhoy FM, Dorian P, Newman DM. Panic disorder and the heart: a cardiology perspective. Journal of Psychosomatic Research. 2000;48(4):393–403. doi: 10.1016/s0022-3999(99)00103-8. http://doi.org/10.1016/S0022-3999(99)00103-8. [DOI] [PubMed] [Google Scholar]
- Kemp AH, Quintana DS, Felmingham KL, Matthews S, Jelinek HF, Ziegelstein R, … Thayer J. Depression, comorbid anxiety disorders, and heart rate variability in physically healthy, unmedicated patients: Implications for cardiovascular risk. PLoS ONE. 2012;7(2):e30777. doi: 10.1371/journal.pone.0030777. http://doi.org/10.1371/journal.pone.0030777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korczak DJ, Goldstein BI, Levitt AJ. Panic disorder, cardiac diagnosis and emergency department utilization in an epidemiologic community sample. General Hospital Psychiatry. 2007;29(4):335–9. doi: 10.1016/j.genhosppsych.2007.03.006. http://doi.org/10.1016/j.genhosppsych.2007.03.006. [DOI] [PubMed] [Google Scholar]
- Leventhal AM, Zvolensky MJ. Anxiety, depression, and cigarette smoking: a transdiagnostic vulnerability framework to understanding emotion-smoking comorbidity. Psychological Bulletin. 2015;141(1):176–212. doi: 10.1037/bul0000003. http://doi.org/10.1037/bul0000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer T, Hussein S, Lange HW, Herrmann-Lingen C. Anxiety is associated with a reduction in both mortality and major adverse cardiovascular events five years after coronary stenting. European Journal of Preventive Cardiology. 2015;22(1):75–82. doi: 10.1177/2047487313505244. http://doi.org/10.1177/2047487313505244. [DOI] [PubMed] [Google Scholar]
- Moshier SJ, Szuhany KL, Hearon BA, Smits JAJ, Otto MW. Anxiety sensitivity uniquely predicts exercise behaviors in young adults seeking to increase physical activity. Behavior Modification. 2016;40(1–2):178–198. doi: 10.1177/0145445515603704. http://doi.org/10.1177/0145445515603704. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Wolitzky-Taylor KB. Anxiety sensitivity and the anxiety disorders: a meta-analytic review and synthesis. Psychological Bulletin. 2009;135(6):974–99. doi: 10.1037/a0017428. http://doi.org/10.1037/a0017428. [DOI] [PubMed] [Google Scholar]
- Parker G, Hyett M, Hadzi-Pavlovic D, Brotchie H, Walsh W. GAD is good? Generalized anxiety disorder predicts a superior five-year outcome following an acute coronary syndrome. Psychiatry Research. 2011;188(3):383–389. doi: 10.1016/j.psychres.2011.05.018. http://doi.org/10.1016/j.psychres.2011.05.018. [DOI] [PubMed] [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24(1):1–8. doi: 10.1016/0005-7967(86)90143-9. http://doi.org/10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Seldenrijk A, van Hout HPJ, van Marwijk HWJ, de Groot E, Gort J, Rustemeijer C, … Stein JH. Sensitivity to depression or anxiety and subclinical cardiovascular disease. Journal of Affective Disorders. 2013;146(1):126–31. doi: 10.1016/j.jad.2012.06.026. http://doi.org/10.1016/j.jad.2012.06.026. [DOI] [PubMed] [Google Scholar]
- Smits JAJ, Berry AC, Rosenfield D, Powers MB, Behar E, Otto MW. Reducing anxiety sensitivity with exercise. Depression and Anxiety. 2008;25(8):689–99. doi: 10.1002/da.20411. http://doi.org/10.1002/da.20411. [DOI] [PubMed] [Google Scholar]
- Smits JAJ, Berry AC, Tart CD, Powers MB. The efficacy of cognitive-behavioral interventions for reducing anxiety sensitivity: A meta-analytic review. Behaviour Research and Therapy. 2008;46(9):1047–1054. doi: 10.1016/j.brat.2008.06.010. http://doi.org/10.1016/j.brat.2008.06.010. [DOI] [PubMed] [Google Scholar]
- Smits JAJ, Tart CD, Presnell K, Rosenfield D, Otto MW. Identifying potential barriers to physical activity adherence: anxiety sensitivity and body mass as predictors of fear during exercise. Cognitive Behaviour Therapy. 2010;39(1):28–36. doi: 10.1080/16506070902915261. http://doi.org/10.1080/16506070902915261. [DOI] [PubMed] [Google Scholar]
- Smits JAJ, Zvolensky MJ, Davis ML, Rosenfield D, Marcus BH, Church TS, … Baird SO. The efficacy of vigorous-intensity exercise as an aid to smoking cessation in adults with high anxiety sensitivity. Psychosomatic Medicine. 2015 Apr;:1. doi: 10.1097/PSY.0000000000000264. http://doi.org/10.1097/PSY.0000000000000264. [DOI] [PMC free article] [PubMed]
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–44. doi: 10.1001/jama.282.18.1737. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10568646. [DOI] [PubMed] [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, … Cardenas SJ. Robust dimensions of anxiety sensitivity: development and initial validation of the Anxiety Sensitivity Index-3. Psychological Assessment. 2007;19(2):176–88. doi: 10.1037/1040-3590.19.2.176. http://doi.org/10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- Tully PJ, Cosh SM, Baumeister H. The anxious heart in whose mind? A systematic review and meta-regression of factors associated with anxiety disorder diagnosis, treatment and morbidity risk in coronary heart disease. Journal of Psychosomatic Research. 2014;77(6):439–448. doi: 10.1016/j.jpsychores.2014.10.001. http://doi.org/10.1016/j.jpsychores.2014.10.001. [DOI] [PubMed] [Google Scholar]
- Tully PJ, Cosh SM, Baune BT. A review of the affects of worry and generalized anxiety disorder upon cardiovascular health and coronary heart disease. Psychology, Health & Medicine. 2013;18(6):627–644. doi: 10.1080/13548506.2012.749355. http://doi.org/10.1080/13548506.2012.749355. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Quantifying selected major risks to health. World Health Report 2002 - Reducing Risks, Promoting Healthy Life. 2002:47–97. Retrieved from http://www.who.int/whr/2002/en/
- Zvolensky MJ, Farris SG, Guillot CR, Leventhal AM. Anxiety sensitivity as an amplifier of subjective and behavioral tobacco abstinence effects. Drug and Alcohol Dependence. 2014;142:224–30. doi: 10.1016/j.drugalcdep.2014.06.023. http://doi.org/10.1016/j.drugalcdep.2014.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]