Abstract
Early care and education (ECE) centers that require lunch brought from home provide an uncluttered view of parent-child dietary interactions in early childhood. Children’s eating from parent-provided bag lunches was observed at 30 ECE centers in Texas, with 15 randomly assigned to the Lunch is in the Bag intervention to improve the lunch meal and 15 to a wait-list control condition. Study participants were parent and child aged 3 to 5 years (N=633 dyads). Data were collected at baseline (pre-intervention) and follow-ups at weeks 6 (post-intervention), 22 (pre-booster), and 28 (post-booster). Changes effected in the children’s lunch eating—e.g., increase of 14 percent in prevalence of children eating vegetables (SE=5, P=0.0063)—reciprocated changes in parent lunch-packing. Irrespective of intervention, however, the children consumed one-half to two-thirds of the amounts of whatever foods the parents packed, and the eat-to-pack ratio did not change across time. Thus, children’s lunch eating at the ECE centers appeared to be regulated by perceptual cues of food availability rather than food preferences or internal cues of hunger and satiety.
INTRODUCTION
Most preschool children, like most people of all ages in the United States (U.S.), eat much less than recommended amounts of vegetables, fruit, and whole grains (U.S. Department of Health and Human Services, 2015). Vegetables intakes in 2013–14 averaged 0.6 cup equivalents for children in the age group 2 to 5 years (Bowman et al, 2017), substantially less than the 1 to 1.5 cups recommended in the 2015–2020 Dietary Guidelines, and a small but significant reduction compared to intakes in 2003–2004. Average fruit intakes were 1.3 cup equivalents for children in the age group 2 to 5 years which was within but not at the top of the recommended range of 1 to 1.5 cups. Although more than half of the total population had grain intakes that met or exceeded recommendations, very few people in the United States have diets that meet the recommendation to make half of all grains consumed be whole grains. For the period 2013–2014, whole grains intakes by children in the age group 2 to 5 years averaged 0.9 ounces compared to refined grains intakes that averaged 4.4 ounces per day.
This situation indicates continued high need for effective interventions to increase vegetables, fruit, and whole grains in the diets of young children because these foods are key dietary components for maintaining healthy weight, protecting against certain cancers, and reducing risks for diabetes and other chronic diseases (U.S. Department of Health and Human Services, 2015). Preschoolers with increased vegetables, fruit, and whole grains in their diets have improved nutrient intake and energy balance (Kranz, Hartman, Siega-Riz & Herring, 2006), and there is some evidence that children with preferences for fruit and vegetables are less likely to be overweight at age 8 and 9 (Lakkakula, Zanovec, Silverman, Murphy, & Tuuri, 2008).
Because food preferences are thought to be established by the time a child is 4 years old, there is broad recognition of the need to increase vegetables, fruit, and whole grains in the diets and preferences of preschool children. Early introduction and frequent exposure to vegetables and fruit are shown to be strongly related to children’s later acceptance and intake of these foods (Cooke et al, 2004).
Early care and education (ECE) settings is an important portal for reaching children, parents, and caregivers with interventions to increase vegetables, fruit, and whole grains in their diets (Feine, 2008). As more mothers have entered the labor force, the number of center-based ECE facilities in the United States has increased dramatically. The most recent estimate is 129,000 (National Survey of Early Care and Education Project Team, 2014). More than one-third of children 3 to 5 years of age in the United States regularly attend center-based ECE facilities (Laughlin, 2013) where, depending on their hours of attendance, they should receive as much as one-half to two-thirds of their meals and snacks (Benjamin Neelon & Briley, 2011).
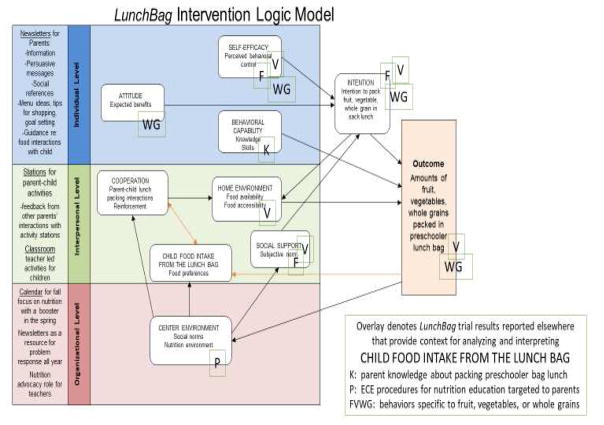
Lunch is in the Bag (LunchBag) is a multi-component, multi-level intervention to increase vegetables, fruit, and whole grains in preschool children’s lunch meal at ECE centers that require the parent to supply bag lunch (Sweitzer et al, 2010). When children bring bag lunch, they can eat vegetables, fruit, and whole grains only when their parents have packed those foods in the lunch. But parents often pack young children’s bag lunches with little or no vegetables or whole grain foods and large amounts of foods with added sugars, fat, and salt such as sweets and salty snack foods (Romo-Palafox et al, 2015). As is depicted in the intervention logic model shown in Figure 1, this situation may be traceable to multiple psychosocial and environmental factors including parents’ lack knowledge, self-efficacy, or intention to pack a healthy, safe, and appealing lunch for their preschoolers (Adamo & Brett, 2013); conflicts in parents’ expectations about the benefits of packing a healthy meal relative to the expected benefits of expressing care by catering to the child’s food preferences (Hughner & Maher, 2006); parental coercive feeding practices or child fussiness rather than cooperative parent-child lunch packing interactions (Webber, Cooke, Hill, & Wardle, 2010); lack of availability of vegetables, fruit, whole grains, or other healthy foods in the home environment (Wyse, Campbell, Nathan & Wolfenden, 2011); lack of social support from other parents, teachers, or leaders of the child’s ECE center for packing a lunch that aligns with the dietary guidelines (Sweitzer et al, 2011); or children’s greater acceptance and intake of the sweets and salty snack foods in preference to the vegetables and other healthy foods packed in their parent-provided bag lunch.
Figure 1.
Schematic of the intervention logic model with an overlay denoting trial results reported elsewhere that provide context for evaluating child food intake from the lunch bag
Parents have the power to influence their children’s food preferences and eating habits by providing repeated opportunities for the child to see and to taste the foods (Fildes, van Jaarsveld, Wardle, & Cooke, 2014), talking with and teaching the child about food (Vollmer & Baietto, 2017), and modeling food preferences and eating habits (Fisk et al, 2011). The bag lunch instantiates in loco parentis modeling of foods to eat and enjoy for lunch. When the parent regularly packs vegetables, fruit, whole grains, and other nutrient-dense foods while minimizing foods that are high in added sugar, fat and salt such as sweets and salty snack foods, the child is provided repeated exposures to a healthy meal pattern. A plausible outcome is the child’s acceptance and habit of eating vegetables, whole grains, and other healthy foods instead of surfeits of sugary beverages and cheesy crackers.
Grounded in Social Cognitive Theory (Bandura, 2004), the Theory of Reasoned Action (Aijzen & Manstead, 2007), and an ecological approach (Bronfenbrenner & Morris, 2006), LunchBag targets multiple leverage points in the development of healthy eating habits in early childhood. To directly inform, cue, and support parents’ readiness to pack bag lunches that present a healthy meal pattern, the center-level kit provides the ECE center director with colorful, easy-to-read LunchBag newsletters to send to the parents. The newsletters present menu ideas, portion size information, goal setting and other home practice assignments, as well as suggestions for home-based parent-child fun-focused nutrition learning activities.
Parent-child activity stations are included in the center-level kit for the ECE director to install on site at the ECE center to prompt and support parent-child talking and learning together about vegetables, fruit, whole grains, and other aspects of a healthy, safe, attractive, and tasty bag lunch. The activity stations also provide a forum for idea sharing and feedback from other parents.
The classroom kit contains lesson plans and resources for teacher-led activities to encourage and support the child’s learning about and becoming willing to request, expect, and enjoy foods from all five My Plate groups including vegetables, fruit, and whole grain foods. Classroom activities each week include a project (e.g., building a “Grain Train” around the classroom walls using empty boxes from whole grain products), a food-related book to read at circle time, favorite food show-and-tell at one or two snack times, and daily using a Lunch Colors placemat to unpack the lunch bag and receive a “Gold Medal Lunch” certificate to take home when the bag contains foods from all five of the My Plate groups. Notes are provided for the teacher to send to the parents describing the plan for the week and requesting needed items (e.g., favorite vegetable for Vitamin Vegetable Wednesday snack time).
Immediately preceding launch of the intervention, the program developers provide training to the ECE teachers as well as resource copies of the newsletters and other materials to support the ECE center’s role as nutrition educator and advocate. The calendar that is included in the center-level kit and covered as a topic in the training specifies the intervention sequence for 5 consecutive weeks in the fall of the school year followed approximately 23 weeks later by one week of intervention in the spring of the school year--i.e., a “booster” to the initial five-week dose of intervention (Sweitzer et al, 2014). Implementation is estimated to demand approximately 3.25 hours for the ECE center director and 3.5 hours for the classroom teacher each week of intervention. Estimated engaged time when the intervention is implemented as designed is 16.5 hours for the child accumulated at the rate of 2.75 hours per week and 9 hours for the parent accumulated at 1.5 hours per week.
The schematic of the intervention logic depicted in Figure 1 has an overlay showing which aspects of the trial results already are published or disseminated via presentations at professional conferences. The intervention effected positive changes in (1) parents’ knowledge about how to pack a healthy, safe, appealing bag lunch; (2) parents’ self-efficacy and intentions to pack vegetables, fruit, and whole grain foods in the children’s lunches; (3) availability of vegetables in the children’s home food environments; (4) parental experience of social support via communication from the ECE center about packing vegetables and whole grain foods in the children’s lunches; (5) parental expectations regarding the benefits of packing whole grains in the lunch; (6) center-level policies and procedures for providing nutrition education to the children’s parents; and (7) numbers of servings of vegetables and whole grains packed in the children’s lunches and prevalence of parents packing fruit, vegetables, and whole grain foods (Potratz et al, 2014; Sharma et al, 2015; Sweitzer et al, 2011; Roberts-Gray et al, 2016a).
This current study examined changes in the preschool children’s lunch eating in the context of the changes that LunchBag effected in the parents’ lunch packing. The hypothesis stated for this secondary aim of the efficacy trial was that, compared to the control condition, children in the intervention condition would attain greater frequency of eating vegetables, fruit, and whole grain foods at the 6- and 28-week follow-up periods. The study design also enabled investigation of the ways in which the changes effected in parents’ packing and children’s eating vegetables, fruit, and whole grain foods was accompanied by changes in other aspects of the bag lunch —e.g., increases in children’s vegetable intake may be accompanied by changes in their intake of meat/beans/eggs/nuts (Leahy, Birch, Fisher, & Rolls, 2008), or increase in children’s eating whole grain foods may be accompanied by decrease in their consumption of refined grains (Burgess-Champoux et al, 2008).
Children’s acceptance and intake of vegetables, fruit, whole grains, and other healthy foods in preference to less nutrient dense foods such as sweets (e.g., sweetened beverages and confections such as cookies) and chips (e.g., potato chips or cheesy crackers) is at the heart of the intervention logic model. To measure changes in the children’s food preferences, servings of the target foods and of sweets and other foods consumed by the children were evaluated in proportion to the servings parents packed. Parent-reported frequency of the preschool child’s asking for, approving, talking of, and reminding the parent to pack vegetables, fruit, and whole grain foods in the lunch bag was evaluated to measure change in parent-child cooperation in lunch packing. Effects of the intervention on the children’s weight status also were examined.
METHODS
Study Design
LunchBag’s cluster-randomized efficacy trial employed direct observation of the bag lunches supplied by the parents and of the children’s eating from those same lunches. This measurement strategy provided a clear view of types and amounts of food the parent served directly to that specific preschool-aged child via the lunch bag and, in return, which and how much of the available foods the child consumed. In line with the timing of the intervention, foods packed and consumed were observed at baseline (pre-intervention) and follow-ups at weeks 6 (post-intervention), 22 (pre-booster), and 28 (post-booster).
ECE centers that required parents to supply bag lunches were recruited during 2010 and 2011 via telephone survey and snow-ball referral methods in three metro areas of Texas: Austin, San Antonio, and Houston. The centers were randomized to the intervention (N=15 centers, 351 study-consented parent-child dyads) or to a wait-list control condition (N=15 centers, 282 study-consented parent-child dyads). The repeated measures enabled analyses of initial behavior change achieved with five weeks of intervention in the fall of the school year, maintenance of the behavior change after removal of the weekly messages and activities, and “boosting” or recovery or other response to reintroduction of all components of the intervention for a sixth and final week in the spring of the school year. The study was powered to detect change of 0.60 servings of vegetable in the child’s lunch. The Child and Adult Care Food Program (CACFP) serving size guide in 2010–2011 for vegetables in the lunch meal of children 3 to 5 years of age was ½ cup raw or cooked.
At intervention ECE centers, LunchBag was made available to all families whose children were in classrooms with ages 3 to 5 years irrespective of whether any given family enrolled in the study. At control ECE centers, LunchBag was made available at the beginning of the school year following completion of the centers’ participation in the trial.
Study Population
Families at the ECE centers were recruited as parent-child dyads. “Parent” was defined as the adult family member primarily responsible for packing the child’s lunch. Enrollment in the study was limited to one dyad per family. Informed consent procedures and research protocol were approved by the Institutional Review Boards of The University of Texas Health Science Center in Houston and The University of Texas at Austin.
Data Collection
A structured food record was used in a validated procedure (Sweitzer et al, 2015) for direct observation of the contents of the children’s parent-provided bag lunches on two randomly selected non-consecutive week days at each of the four measurement periods. The food record provided columns for the trained observers to record the types and amounts of foods packed in the lunch bag, and then to record during the lunch period the amount of each food item the child consumed. A separate food record was completed for each lunch by the single observer assigned to that lunch bag. The observer recorded a nominal description of each item and specified in standard measuring units (such as 1/2 cup of carrots or 1 slice of bread or 4 Tablespoons of raisins) the amount packed and the amount consumed. A total of 11 observers were trained and supervised to conduct the observations with each observer usually having responsibility for observing as many as 5 children’s lunch eating within any given classroom or lunch room.
A Registered Dietitian post-coded the food groups and numbers of servings. The coded food groups were vegetables, fruit, whole grain, refined grain, dairy, meat/beans/eggs/nuts, sweets, and chips. CACFP 2010–2011 serving sizes for the lunch meal of children 3 to 5 years of age were ½ cup of vegetables or fruit or both, ½ serving of grains, 1 ½ ounces of meat or alternate, and ¾ cup of fluid milk. Sweets as coding category was comprised of sugary beverages and confections such as candy and cookies. Because the CACFP lunch meal pattern requires fluid milk as the beverage, sugary beverages were coded as sweets and 100% fruit juices were coded as fruit. Although the CACFP meal pattern allows yogurt and cheese to be counted as meat alternates, these items were coded as dairy for LunchBag’s efficacy trial. Chips as a coding category was comprised of snack foods that are high in added fat and sodium such as potato chips, corn chips, and cheese crackers. The rule for items for which there was no CACFP serving size guideline (e.g., potato chips) was to assign one-half of an adult serving size.
Occurrence was the primary measure of frequency of children’s eating the foods. Numbers of servings consumed also were analyzed. Because children cannot eat a food that the parent does not pack in the lunch bag, analyses were conducted to control for presence of the food. To measure changes in children’s food preferences, separate analyses were conducted to estimate proportion consumed of the available food in each of the coded groups.
Data to measure cooperation in parent-child lunch-packing interactions via the child’s requesting and approving the parent’s packing of fruit, vegetables, and whole grain foods in the lunch bag were collected with the questionnaire completed by the parent at baseline and at each of the follow-up periods. The separate scales for vegetables, fruit, and whole grains were adapted from validated instruments for measuring perceived social support for purchasing fruits and vegetables (Baranowski et al, 2006). The four items asked “how often” (1=never, 2= rarely, 3=sometimes, 4=most of the time, 5=always) the child interacted with the parent regarding the food as follows: (1) approved when you packed the food in his or her lunch, (2) asked you to pack the food in his or her lunch, (3) reminded you to buy the food for his or her lunch, and (4) talked to you about that food for his or her lunch. Range of possible scores was 4 to 20 for each of vegetables, fruit, and whole grain foods.
Children’s weight status was measured by the trained data collectors using standard protocols previously used in nutrition research with school children to document the child’s height and weight. Body Mass Index (BMI) was calculated using the standard method and values compared to the U.S. Centers for Disease Prevention and Control (CDC) age and gender standards for weight status. Overweight was indicated by BMI between 85th and 95th percentile and obesity was indicated by BMI at or above the 95th percentile (Barlow et al, 2007). Children’s height and weight were measured again after the 28-week follow-up observations of the lunch meals.
Data to measure LunchBag implementation were collected at the intervention ECE centers during the trial. The ECE directors and teachers completed weekly activity logs to document completeness and fidelity of their implementing actions. Trained members of the research team used Innovation Configuration rubrics to record their direct observations of qualities of implementing actions for the classroom and activity station components. A summary questionnaire self-administered by the participating parents and ECE personnel immediately following the initial five weeks of intervention provided data to measure acceptability and dose. Debriefing interviews were conducted with parents, teachers, and ECE directors to evaluate qualities of use, usefulness, and usability of the intervention. More detail about the structure and content of each of these tools and procedures is reported elsewhere (Roberts-Gray et al, 2016b).
Data to measure center characteristics and family demographics were collected at baseline. A questionnaire for the ECE center director asked about center size, affiliation, classroom groupings, and nutrition-related policies and procedures. Questionnaires for the parents asked for demographic information about self and child.
Statistical Analyses
Data representing parents’ lunch packing and children’s lunch eating were analyzed in separate multi-level models for each type of food. The hypotheses tested for this current study were that the intervention would increase children’s eating vegetables, fruit, and whole grain foods from their bag lunches. Intervention effects on children’s eating others of My Plate foods and of foods that are high in added sugar, fat, and salt (i.e., sweets and chips) were examined to enable inspection of extent to which the changes in intake of vegetables, fruit, and whole grains were accompanied by changes in other components of the bag lunch meal. Each multi-level model compared the follow-up with the baseline measure. Three-level regression models were constructed to allow random effects at the center level, as well as at the family level, within and across time periods. Percentage of children eating any amount of the given type of food, number of servings eaten, and frequency of the children’s requesting or approving the parents’ packing of the food were estimated at each measurement period and treatment condition. Intervention effects were evaluated with a time-by-treatment interaction term. Analyses were conducted using Proc Mixed or Proc Glimmix, depending on the distribution of the outcome, in SAS (version 9.2, SAS Institute, Inc., Cary, NC, USA) for restricted maximum likelihood (REML) estimation. Multi-attribute evaluation (MAE) methods (Edwards & Newman, 1982) and thematic analysis (Braun & Clarke, 2006) were applied to the implementation data. Center characteristics and family demographics were analyzed with descriptive statistics.
RESULTS
Center Characteristics
There was diversity of size (30 to 300 children, median = 90) and affiliation of the ECE centers. Twenty were affiliated with a church or synagogue, 5 were affiliated with local or nationwide organizations or chains, and 5 were stand-alone organizations. All 30 of the ECE centers were retained in the study through the 28-week follow-up. Other than increase at the 28-week follow-up in procedures for providing nutrition education to parents compared to baseline, there were no changes in the nutrition environment in the intervention or the control centers. Additional detail about characteristics of the ECE centers is presented elsewhere (Roberts-Gray 2016a; Potratz et al, 2014).
Family Demographics
With 42% of the participating ECE centers’ eligible parent-child dyads consenting to participate in the study, the total number of consented families was 633. Nearly all (91%) were retained in the study through the 28-week follow-up. Numbers consented per center ranged from 12 to 43 (median=22) in the intervention condition and from 6 to 30 (median=19) in the control condition. The differences in sizes of the centers and rates of families consented per center resulted in more study participants at the intervention centers than at the control centers. The intervention condition had relatively larger proportion of Hispanic children and parents, fewer parents older than 34, fewer parents with overweight or obesity, more parents with college degree, fewer single parents, and higher annual family income. These results are presented in Table 1. Statistical analyses of the outcomes data included adjustment for these demographic differences, with education preferred over income as a covariate because it had fewer missing values.
Table 1.
Baseline demographic characteristics of children and parents in the LunchBag trial
| Item | Control | Intervention | Total | P-value | n |
|---|---|---|---|---|---|
|
| |||||
| n (%) | n (%) | n (%) | |||
| Child | |||||
|
| |||||
| Age (Mean, SD) | 3.49 (0.74) | 3.53 (0.65) | 3.51 (0.69) | 0.50 | 616 |
| Child BMI categories | 0.22 | 584 | |||
| Under weight | 16 (6.2%) | 16 (4.9%) | 32 (5.5%) | ||
| Healthy weight | 178 (68.7%) | 243 (74.8%) | 421 (72.1%) | ||
| Over weight | 41 (15.8%) | 34 (10.5%) | 75 (12.8%) | ||
| Obesity | 24 (9.3%) | 32 (9.9%) | 56 (9.6%) | ||
| Parent reported child weight | 0.13 | 523 | |||
| Under weight | 18 (7.7%) | 38 (13.2%) | 56 (10.7%) | ||
| Average weight | 213 (91.0%) | 247 (85.5%) | 460 (88.0%) | ||
| Over weight | 3 (1.3%) | 4 (1.4%) | 7 (1.3%) | ||
| Race/heritage | <0.01 | 579 | |||
| White | 151 (58.1%) | 229 (71.8%) | 380 (65.6%) | ||
| Hispanic | 72 (27.7%) | 38 (11.9%) | 110 (19.0%) | ||
| Other | 37 (14.2%) | 52 (16.3%) | 89 (15.4%) | ||
| Gender | 1.00 | 627 | |||
| Boy | 146 (52.1%) | 181 (52.2%) | 327 (52.2%) | ||
| Girl | 134 (47.9%) | 166 (47.8%) | 300 (47.8%) | ||
|
| |||||
| Parent | |||||
|
| |||||
| Age (Mean, SD) | 35.35 (5.48) | 37.29 (5.33) | 36.44 (5.48) | <0.01 | 567 |
| Parent BMI categories | 0.12 | 565 | |||
| Under weight | 6 (2.5%) | 10 (3.1%) | 16 (2.8%) | ||
| Healthy weight | 135 (55.6%) | 208 (64.6%) | 343 (60.7%) | ||
| Over weight | 62 (25.5%) | 67 (20.8%) | 129 (22.8%) | ||
| Obesity | 40 (16.5%) | 37 (11.5%) | 77 (13.6%) | ||
| Gender | 0.46 | 576 | |||
| Male | 22 (8.8%) | 35 (10.7%) | 57 (9.9%) | ||
| Female | 227 (91.2%) | 292 (89.3%) | 519 (90.1%) | ||
| Race/heritage | <0.01 | 572 | |||
| Caucasian | 156 (62.9%) | 253 (78.1%) | 409 (71.5%) | ||
| Hispanic | 65 (26.2%) | 38 (11.7%) | 103 (18.0%) | ||
| Other | 27 (10.9%) | 33 (10.2%) | 60 (10.5%) | ||
| Annual family income | <0.01 | 548 | |||
| Less than $19,999 | 15 (6.4%) | 4 (1.3%) | 19 (3.5%) | ||
| $20,000–$39999 | 30 (12.8%) | 12 (3.8%) | 42 (7.6%) | ||
| $40,000–$59999 | 15 (6.4%) | 18 (5.8%) | 33 (6.0%) | ||
| $60,000–$79,999 | 23 (9.8%) | 32 (10.2%) | 55 (10.0%) | ||
| $80,000–$99,999 | 37 (15.7%) | 49 (15.7%) | 86 (15.7%) | ||
| Greater than $100,000 | 115 (48.9%) | 198 (63.3%) | 313 (57.1%) | ||
| Highest level of education | <0.01 | 575 | |||
| Some high school | 8 (3.2%) | 1 (0.3%) | 9 (1.6%) | ||
| High school diploma/GED | 10 (4.0%) | 7 (2.1%) | 17 (3.0%) | ||
| Some college | 45 (18.1%) | 30 (9.2%) | 75 (13.0%) | ||
| Associate or Bachelors | 123 (49.6%) | 161 (49.2%) | 284 (49.4%) | ||
| Masters or Doctorate | 62 (25.0%) | 128 (39.1%) | 190 (33.0%) | ||
| Marital status | 0.03 | 572 | |||
| Single | 12 (4.8%) | 11 (3.4%) | 23 (4.0%) | ||
| Married | 209 (84.3%) | 298 (92.0%) | 507 (88.6%) | ||
| Separated | 7 (2.8%) | 2 (0.6%) | 9 (1.6%) | ||
| Divorced | 9 (3.6%) | 9 (2.78%) | 18 (3.1%) | ||
| Widowed | 2 (0.8%) | 0 (0%) | 2 (0.003%) | ||
| With partner | 9 (3.6%) | 4 (1.2%) | 13 (2.3%) | ||
Across intervention and control conditions, the “parent” in more than half of the participating families possessed a college or advanced degree (82%), was of non-Hispanic white heritage (72%), provided height and weight self-report that yielded BMI indicative of healthy weight (61%), and had annual family income greater than $100,000 (57%). Nearly all were female (90%) and married or partnered (90%). Average age was 36.
Half (50%) of the “child” members were 2 to 3 years of age and half were 4 to 6 years of age; 52% were male; 22% had overweight or obesity; and 6% had underweight. A few of the parents (N=36) reported the primary language in the child’s home was other than English (Spanish=20; Hebrew, Vietnamese, Urdu, or other Asian language=14, European or African language=2). None of the parents requested or indicated need for translations of the consent documents, intervention materials, or data collection instruments.
Participation in data collection
Numbers of dyads with data at one or more of the lunch observations were 325 or 93% of those in the intervention condition and 253 or 90% of those in the control condition. Numbers of parents who answered the questionnaires at one or more of the measurement periods were 327or 93% of those in the intervention and 250 or 89% of those in the control condition.
Implementation of the intervention
Moderate to high scores for fidelity and completeness of implementation were obtained at 12 of the 15 intervention centers. Prevalence of specific implementing actions was consistent with the research team’s pre-trial forecasts except that more parents than expected read the newsletters (83% vs 50%) and fewer reported hearing their children talk about the classroom activities (4% vs 50%). More detail about implementation is presented elsewhere (Roberts-Gray et al, 2016b).
Effects of the intervention on percentage of children eating the different types of food
At the 6-week follow-up at the intervention centers the effect size was 14 percent more children eating vegetables (SE=5, P=0.0047) and this improvement was sustained through the 22-week follow-up (effect size 10 percent, SE=5, P=0.0349) and the 28-week follow-up (effect size 14 percent, SE=5, P=0.0063). Compared to baseline, 14 percent more children at the intervention centers consumed whole grain foods from their bag lunches at the 22-week follow-up (SE=6, P=0.0105). At this same time-point, there was a decrease at the intervention centers relative to the control condition in percent of children eating refined grain foods from their lunch bags (effect size= −10 percent, SE=5, P=0.0317). Neither of these changes, however, was sustained through the 28-week follow-up. There were no significant differences in prevalence of children eating fruit, meat/beans/eggs/nuts, or dairy. These results are presented in Table 2.
Table 2.
Percentage of children eating any amount of fruit, vegetables, and whole grain items and other My Plate foods from their parent-provided bag lunch shown by time and treatment
| Time and domain of child eating | Intervention Percent (Standard Error) | Control Percent (Standard Error) |
|---|---|---|
| Vegetables | ||
| Pre-Intervention Baseline | 47 (5.0) | 42 (5.0) |
| Post-Intervention 6-week follow-up | 60 (5.0) *** †† | 41 (5.0) |
| Pre-Booster 22-week follow-up | 56 (5.0) ** † | 40 (5.0) |
| Post-Booster 28-week follow-up | 60 (5.0) *** †† | 41 (5.0) |
|
| ||
| Fruit | ||
| Pre-Intervention Baseline | 88 (5.0) | 77 (5.0) |
| Post-Intervention 6-week follow-up | 89 (5.0) | 74 (5.0) |
| Pre-Booster 22-week follow-up | 89 (5.0) | 73 (5.0) |
| Post-Booster 28-week follow-up | 88 (5.0) | 74 (5.0) |
|
| ||
| Whole grains | ||
| Pre-Intervention Baseline | 38 (5.0) | 39 (5.0) |
| Post-Intervention 6-week follow-up | 43 (5.0) | 36 (5.0) |
| Pre-Booster 22-week follow-up | 47 (5.0)* † | 34 (5.0) |
| Post-Booster 28-week follow-up | 40 (5.0) | 31 (5.0) |
|
| ||
| Refined grains | ||
| Pre-Intervention Baseline | 85 (4.0) | 82 (4.0) |
| Post-Intervention 6-week follow-up | 80 (4.0) | 84 (4.0) |
| Pre-Booster 22-week follow-up | 78 (4.0)* † | 85 (4.0) |
| Post-Booster 28-week follow-up | 83 (4.0) | 82 (4.0) |
|
| ||
| Meats/beans/eggs/nuts | ||
| Pre-Intervention Baseline | 88 (3.0) | 92 (3.0) |
| Post-Intervention 6-week follow-up | 89 (3.9) | 90 (3.0) |
| Pre-Booster 22-week follow-up | 91 (3.0) | 90 (3.0) |
| Post-Booster 28-week follow-up | 85 (3.0) | 87 (3.0) |
|
| ||
| Dairy | ||
| Pre-Intervention Baseline | 76 (4.0) | 76 (4.0) |
| Post-Intervention 6-week follow-up | 81 (4.0) | 77 (4.0) |
| Pre-Booster 22-week follow-up | 72 (4.0) | 77 (4.0) |
| Post-Booster 28-week follow-up | 74 (4.0) | 77 (4.0) |
within-groups change baseline to follow-up P<.05,
P<.01,
P<.001
treatment-by-time interaction baseline to follow-up P<.05,
P<.01,
P<.001
Percent (standard error) estimated in mixed-effects models of the treatment-by-time interaction that adjusted for repeated measures within families and nesting of families within ECE centers. The models were based on data from 4,712 lunches packed by parents for their preschool children. Each model compared the given measurement period to baseline. The models also were adjusted for child’s gender and age and for the parent’s gender, age, heritage, marital status and education. Percent of children eating the given foods was based on the occurrence of any amount of the food consumed on at least one of the two days in the measurement period.
At the 28-week follow-up, the percent of children consuming chips was similar in the intervention and control conditions (30% and 29%, respectively), but the difference compared to baseline was increase in the intervention condition versus decrease in the control condition (effect size 12 percent, SE=5, P=0.0152). In contrast, the percent of children consuming sweets decreased at the intervention centers and increased at the control centers. Effect size of the change from baseline to follow-up in the intervention compared to the control condition was −13 percent at the 22-week follow-up (SE=5, P=0.0099) and −13 percent at the 28-week follow-up (SE=5, P=0.0104). These results are presented in Table 3.
Table 3.
Percentage of children eating foods that are high in added sugar, fat, and salt from their parent-provided bag lunch shown by time and treatment
| Intervention Percent (Standard Error) | Control Percent (Standard Error) | |
|---|---|---|
| Chips | ||
| Pre-Intervention Baseline | 25 (4.0) | 36 (4.0) |
| Post-Intervention 6-week follow-up | 22 (4.0) | 31 (4.0) |
| Pre-Booster 22-week follow-up | 25 (4.0) | 30 (4.0) |
| Post-Booster 28-week follow-up | 30 (4.0) | 29 (4.5) † |
|
| ||
| Sweets | ||
| Pre-Intervention Baseline | 62 (5.0) | 56 (5.0) |
| Post-Intervention 6-week follow-up | 58 (5.0)* | 56 (5.0) |
| Pre-Booster 22-week follow-up | 54 (5.0)* †† | 61 (5.0) |
| Post-Booster 28-week follow-up | 55 (5.0) † | 63 (5.0) |
within-groups change baseline to follow-up P<.05,
P<.01,
P<.001
treatment-by-time interaction baseline to follow-up P<.05,
P<.01,
P<.001
Percent (standard error) estimated in mixed-effects models of the treatment-by-time interaction that adjusted for repeated measures within families and nesting of families within ECE centers. The models were based on data from direct observation of a total of 4,712 lunches packed by parents for their preschool children. Each model compared the given measurement period to baseline. The models also were adjusted for child’s gender and age and for the parent’s gender, age, heritage, marital status and education. Percent of children eating the given foods was based on the occurrence of any amount of the food consumed on at least one of the two days in the measurement period.
Effects of the intervention on numbers of servings the children consumed of the different types of food
At the 22-week follow-up there was significant increase in servings of vegetables consumed by children in the intervention group, but this effect was not sustained relative to the control group at the 28-week follow-up. The effect size of increase in whole grain foods consumed at the 6-week follow-up was 0.24 servings (SE=0.1, P=0.014) and this increase was maintained at the 22-week follow-up (effect size 0.37 servings, SE=0.1, P=0.0002) but not sustained through the 28-week follow-up. The number of servings of refined grains consumed by children in the intervention group remained the same through the 6- and 22-week follow-ups in contrast to steady increase in servings of refined grains consumed by children in the control group. The effect size of the difference in amount of change in servings of refined grains consumed at the 22-week follow-up relative to baseline for the intervention group compared to the control group was −0.34 servings (SE=0.13, P=0.125). This positive time by treatment effect was not sustained, however, through the 28-week follow-up. There were no changes in servings of fruit or meat/beans/eggs/nuts consumed by the children. The time by treatment analyses did show beneficial effect of the intervention on servings of dairy foods consumed at the 28-week follow-up (effect size 0.10 servings, SE=0.04, P=0.026). These results are presented in Table 4.
Table 4.
Number of servings of My Plate foods the children consumed from their parent-provided bag lunches shown by time and treatment
| Intervention Mean (Standard Error) | Control Mean (Standard Error) | |
|---|---|---|
| Vegetables | ||
| Pre-Intervention Baseline | 0.22 (0.03) | 0.15 (0.03) |
| Post-Intervention 6-week follow-up | 0.26 (0.03)† | 0.16 (0.03) |
| Pre-Booster 22-week follow-up | 0.25 (0.03) | 0.17 (0.03) |
| Post-Booster 28-week follow-up | 0.25 (0.03) | 0.16 (0.03) |
|
| ||
| Fruit | ||
| Pre-Intervention Baseline | 0.88 (0.09) | 0.81 (0.09) |
| Post-Intervention 6-week follow-up | 0.92 (0.09) | 0.79 (0.09) |
| Pre-Booster 22-week follow-up | 0.89 (0.09) | 0.80 (0.09) |
| Post-Booster 28-week follow-up | 0.94 (0.09) | 0.86 (0.09) |
|
| ||
| Whole grains | ||
| Pre-Intervention Baseline | 0.50 (0.10) | 0.61 (0.10) |
| Post-Intervention 6-week follow-up | 0.61 (0.10)† | 0.48 (0.10) |
| Pre-Booster 22-week follow-up | 0.70 (0.10)**††† | 0.44 (0.10)* |
| Post-Booster 28-week follow-up | 0.55 (0.10) | 0.51 (0.10) |
|
| ||
| Refined grains | ||
| Pre-Intervention Baseline | 1.42 (0.10) | 1.46 (0.10) |
| Post-Intervention 6-week follow-up | 1.39 (0.10) | 1.58 (0.10) |
| Pre-Booster 22-week follow-up | 1.43 (0.10)† | 1.81 (0.10)*** |
| Post-Booster 28-week follow-up | 1.63 (0.10) | 1.55 (0.10) |
|
| ||
| Meats/beans/eggs/nuts | ||
| Pre-Intervention Baseline | 0.75 (0.07) | 0.81 (0.07) |
| Post-Intervention 6-week follow-up | 0.79 (0.07) | 0.77 (0.07) |
| Pre-Booster 22-week follow-up | 0.81 (0.07) | 0.79 (0.07) |
| Post-Booster 28-week follow-up | 0.81 (0.07) | 0.79 (0.07) |
|
| ||
| Dairy | ||
| Pre-Intervention Baseline | 0.43 (0.05) | 0.45 (0.05) |
| Post-Intervention 6-week follow-up | 0.49 (0.05)* | 0.47 (0.05) |
| Pre-Booster 22-week follow-up | 0.46 (0.05) | 0.54 (0.05)** |
| Post-Booster 28-week follow-up | 0.49 (0.05)*† | 0.41 (0.05) |
within-groups change baseline to follow-up P<.05,
P<.01,
P<.001
treatment-by-time interaction baseline to follow-up P<.05,
P<.01,
P<.001
Means (standard errors) are based on mixed-effects models of the treatment-by-time interaction that adjusted for repeated measures within families and nesting of families within ECE centers. The models were based on data from direct observations of the total of 4,712 lunches packed by parents for their preschool children. Servings were aggregated across specific lunch items (e.g., vegetable servings included the amount of tomato sauce on pasta and the amount of vegetables in mixed dishes as well as the amount of whole vegetable items such as baby carrots. Each model compared the given measurement period to baseline. The models also were adjusted for child’s gender and age, and for parental heritage, marital status and education.
There were no differences between the treatment groups in servings of chips consumed, but at the 22-week and 28-week follow-up periods, children in the intervention condition consumed fewer servings of sweets compared to baseline whereas children in the control condition consumed more servings of sweets compared to baseline. The effect size for intake of sweets at the 22-week follow-up was −0.23 servings (SE=0.08, P=0.0032) and at the 28-week follow-up was −0.17 servings (SE=0.08, P=0.0246). These results are presented in Table 5.
Table 5.
Number of servings of foods that are high in added sugar, fat, salt consumed by the children from their parent-provided bag lunches shown by time and treatment
| Intervention Mean (Standard Error) | Control Mean (Standard Error) | |
|---|---|---|
| Chips | ||
| Pre-Intervention Baseline | 0.15 (0.04) | 0.24 (0.03) |
| Post-Intervention 6-week follow-up | 0.14 (0.04) | 0.23 (0.04) |
| Pre-Booster 22-week follow-up | 0.15 (0.04) | 0.21 (0.04) |
| Post-Booster 28-week follow-up | 0.21 (0.04)* | 0.24 (0.04) |
|
| ||
| Sweets | ||
| Pre-Intervention Baseline | 0.75 (0.09) | 0.69 (0.08) |
| Post-Intervention 6-week follow-up | 0.68 (0.09) | 0.70 (0.08) |
| Pre-Booster 22-week follow-up | 0.64 (0.09)*†† | 0.81 (0.08)* |
| Post-Booster 28-week follow-up | 0.71 (0.09) † | 0.82 (0.08)* |
within-groups change baseline to follow-up P<.05,
P<.01,
P<.001
treatment-by-time interaction baseline to follow-up P<.05,
P<.01,
P<.001
Means and standard errors are based on mixed-effects models of the treatment-by-time interaction adjusted for repeated measures within families and nesting of families within ECE centers. The models were based on data from 4,712 lunches packed by parents for their preschool children. Each model compared the given measurement period to baseline. The models also were adjusted for child’s gender and age, and parental heritage, marital status and education.
Intervention effects on children’s food preferences
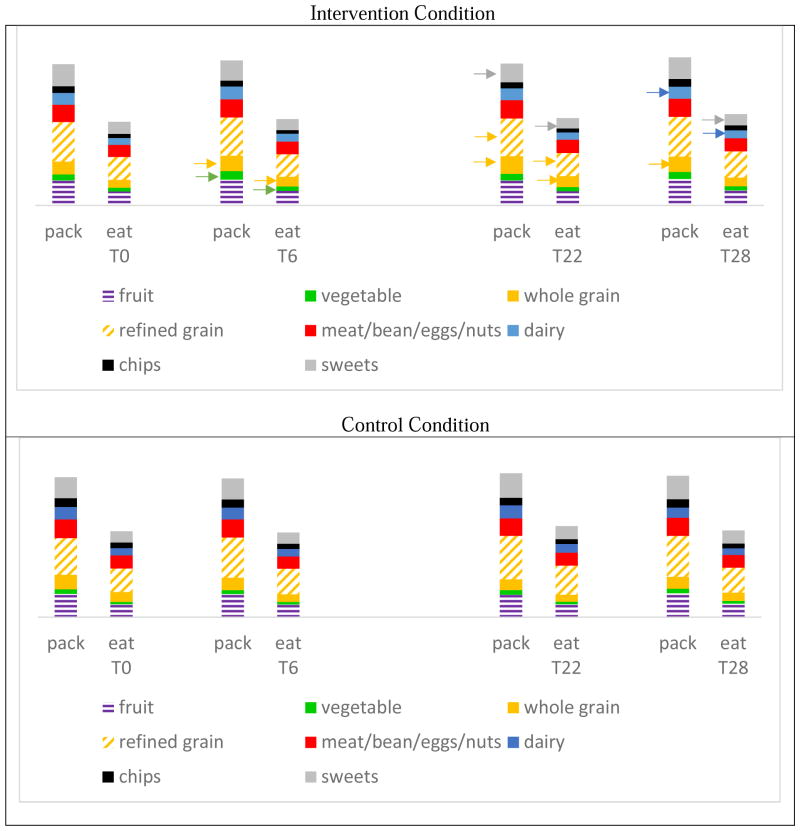
There was no evidence of change in the children’s food preferences. Results depicted in Figure 2 show that the children nearly always consumed some of whatever foods the parents packed in the lunch bag. The proportions of food consumed when the parent packed that food in the children’s lunch bag was approximately half to two-thirds of whatever amount the parents packed irrespective of time and treatment. The baseline proportions consumed were 72% of refined grain (SE=9), 70% of whole grain (SE=13), 64% of dairy (SE=9), 62% of meat/bean/eggs/nuts (SE=9), 61% of fruit (SE=10), 60% of vegetables (SE=14), 59% of sweets (SE=12), and 59% of chips (SE=17). The eat-to-pack ratios did not change with time or treatment. This pattern of results is observable in the results presented in Figure 3.
Figure 2.
Percent of children eating any amount of the food compared to percent of parents packing any amount of the food – Data displayed for the Intervention Condition. Results for which the time by treatment interaction was significant (P<0.05) are underlined. Results that favored the control group are marked
Figure 3.
Numbers of servings of food parents packed and numbers of servings of food eaten by the children – Outcomes for which the time by treatment interaction term was significant (P<.0.05) are marked with arrows for the group that benefited (baseline=T0, 6-week follow-up=T6, 22-week follow-up=T22, and 28-week follow-up=T28)
Intervention effects on children’s eating in the context of changes effected in parents’ packing of the children’s bag lunches
Inspection of Figure 2 and of Figure 3 reveals that there were no changes in the children’s eating without a preceding change in parental packing of the food. This pattern described the results when the outcomes were percentages of children eating the foods--e.g., at the 28-week follow-up, contrary to expectation, there was significant increase in the intervention parents’ packing of chips in the lunches and at that same time point there was significant increase in the intervention children’s eating chips from their lunch bags. This pattern also described the results when the outcomes were amounts of food eaten measured as numbers of servings--e.g., the significant decrease in servings of sweets consumed by intervention children at the 22-week follow-up and again at the 28-week follow-up was preceded by significant reduction at the 22-week follow-up in servings of sweets packed by intervention parents compared to the control group.
There were two occurrences of change in parents’ packing that were not followed by change in children’s eating. Percentage of parents packing fruit increased from 91 at baseline to 94 at the 6-week follow-up and to 93 at the 22-week follow-up while prevalence of children eating fruit remained constant at approximately 88 to 89 percent. At the 6-week follow-up, servings of vegetables packed by parents increased and children’s eating of vegetables appeared to move in the desired direction--i.e., increase from less than one-fourth serving to one-fourth serving consumed in the intervention condition whereas in the control condition servings of vegetables consumed was stable at less than one-fourth serving. But this result was not statistically significant.
Effects of the intervention on parent-child cooperation in lunch packing
In both the intervention and the control conditions, baseline scores indicated the children “never” express or exhibit support for packing vegetables, “rarely” provide support for packing whole grain foods, but “sometimes” approve, ask for, talk of, or remind the parent to pack fruit. The intervention had positive effects on children’s expressing support for parental packing of vegetables and whole grain items. Effect size for support of vegetables at the 6-week follow-up was 1.27 points (SE=0.30, P<.0.0001) and the increase was sustained at the 22- (effect size 0.93 points, SE=0.33, P=0.0049) and 28-week follow-up (effect size 0.79 points, SE=0.30, P=0.0083). Effect size for support of packing whole grain items at the 6-week follow-up was 0.75 points (SE=0.35, P=0.031) and was also positive at the 28-week follow-up (effect size 0.89 points, SE=0.35, P=0.0109). However, the scores remained below the mid-point on the scale measuring children’s approving, asking for, talking of, and reminding the parent to pack vegetables or to pack whole grain foods in their bag lunch. These results are presented in Table 6.
Table 6.
Scale scores for parental report of frequency of the child’s approving, asking for, talking of, and reminding to pack fruits, vegetables, whole grain items in the child’s bag lunch --Score of 20 translates to “child always exhibits all four behaviors” and score of 4 translates to “child never exhibits any of these four behaviors”.
| Time and domain of parents’ reports of child’s social support | Intervention Mean (Standard Error) | Control Mean (Standard Error) |
|---|---|---|
| Fruit | ||
| Pre-Intervention Baseline | 9.81 (0.28) | 9.86 (0.31) |
| Post-Intervention 6-week follow-up | 10.30 (0.29)* | 10.06 (0.31) |
| Pre-Booster 22-week follow-up | 10.35 (0.30)* | 9.98 (0.34) |
| Post-Booster 28-week follow-up | 10.22 (0.31) | 9.92 (0.31) |
|
| ||
| Vegetables | ||
| Pre-Intervention Baseline | 5.71 (0.30) | 5.72 (0.33) |
| Post-Intervention 6-week follow-up | 7.10 (0.31)*** ††† | 5.85 (0.33) |
| Pre-Booster 22-week follow-up | 7.12 (0.32)*** †† | 6.21 (0.35) |
| Post-Booster 28-week follow-up | 7.11 (0.31)*** †† | 6.34 (0.34)** |
|
| ||
| Whole grains | ||
| Pre-Intervention Baseline | 7.21 (0.28) | 7.47 (0.31) |
| Post-Intervention 6-week follow-up | 8.36 (0.29)*** † | 7.88 (0.31) |
| Pre-Booster 22-week follow-up | 8.45 (0.31)*** | 8.10 (0.34)* |
| Post-Booster 28-week follow-up | 8.38 (0.29)*** † | 7.76 (0.32) |
within-groups change baseline to follow-up P<.05,
P<.01,
P<.001
treatment-by-time interaction baseline to follow-up P<.05,
P<.01,
P<.001
Means and standard errors are based on mixed-effects models of the treatment-by-time interaction adjusted for repeated measures within families and nesting of families within ECE centers. The models were based on data from questionnaire responses supplied by 377 parents in the intervention condition and 251 in the control condition. Each model compared the given measurement period to baseline. The models also were adjusted for child’s gender and age, and parental heritage, marital status and education.
Effects of the intervention on children’s weight status
From baseline to the 28-week follow-up, BMI decreased in the intervention group from the 56th percentile to the 52nd percentile (4 percentage point reduction) while the control group increased from the 58th percentile to the 61st percentile (3 percentage points increase). The net time by treatment change was 6.9 percentage points (P=0.0462).
DISCUSSION
Results of this study provided some support for the hypothesis that young children’s frequency of eating vegetables, fruit, and whole grain foods for lunch would increase when the multi-level, multi-component LunchBag intervention was implemented at ECE centers that require lunch brought from home. The intervention increased the percentage of children eating vegetables and whole grain foods for lunch but did not increase the percentage of children eating fruit even when the percentage of parents packing fruit was increased. The intervention had the additional positive effects of preventing decrease in children’s lunch time consumption of dairy foods and preventing increase in occurrence and amounts of sweets consumed. The positive effects for vegetables and for sweets were maintained through the 28-week follow-up. The only negative effect was increase at the intervention centers in prevalence of parents packing and children eating chips at the 28-week follow-up. Potential explanations of this undesired result include the possibility that in their effort to increase vegetables some parents in the intervention group were misled by front-of-the-package claims (Abrams, Duff, & Evans, 2015) and added “veggie” chips to their lunch packing or that some control group parents became concerned across time about choking hazards of chips for young children.
A surprising result was finding that although the amount of intervention engaged time available to the children when the intervention was implemented as intended was substantially larger than the amount of intervention engaged time available to the parents, changes in children’s lunch eating always were preceded by changes in the parents’ lunch packing, and not vice versa. To some extent, that result is explained by the second surprise which was seeing that, irrespective of the changes that time and treatment effected in parents’ lunch packing and children’s lunch eating, the children consistently consumed half to two-thirds of whatever amount of whatever foods the parents packed in the lunch bags. This result of the current study parallels outcomes of food laboratory studies showing that, “if their parents are not around, elementary school children eat only 60% of the food they serve themselves” whereas adults consume 92% of the food they serve themselves (Wansink & Johnson, 2015). It also fits what appears to be a developmental pattern in children’s lunch eating that is discernable across many years of studies of child nutrition programs in the United States. Research on the CACFP showed preschool children consumed approximately 59% of their lunch food (U.S. Department of Agriculture, 1997), and a recent study of the Head Start lunch meal for preschool aged children showed “only 57% of the total food served was actually consumed” (Nicklas et al, 2013). Studies of the National School Lunch Program (NSLP) showed elementary students consumed 75% and “middle/secondary” students consumed 90% of their lunch selections (U.S. Department of Agriculture, 1992 summarized in Busby & Guthrie, 2009).
A spate of recent evaluations of the impacts of changes in requirements of the NSLP indicate that younger children persist in consuming a smaller proportion of the food available in their lunch meal compared to older students. Entrée is the meal component most frequently reported. Elementary school students consumed 70–80% of their lunch entrée while middle school students consumed 80–95% (Smith & Cunningham-Sabo, 2014; Cullen, Chen, Dave, & Jensen, 2015). Percent of entrée consumed by preschoolers in the study of Head Start lunch meals (Nicklas et al, 2013) was 61%, a figure remarkably akin to the 62% eat-to-pack ratio for meat/bean/eggs/nuts in the current study of LunchBag. Other than a study in Denmark that showed third and fourth grade school children consumed 77% of their school lunch food (Thorsen et al, 2015), information is lacking about proportions of food consumed versus conserved through the end of the meal by children in countries outside the United States.
Evidence that younger children conserve to the end of the meal a larger proportion of their food than do older children who in turn conserve a larger proportion than do adults points to a potential leverage point in the development of healthy eating habits. It seems important for parents to know that, in the absence of the parent, preschool aged children eat about half to two-thirds of whatever amount of whatever food is served. The current study’s unique contribution to this accumulation of evidence regarding the development of children’s eating behavior is indications that preschoolers consume (and conserve) proportionally the same amounts of vegetables as they do sweets and chips.
Potential explanations of children’s conserving substantial but developmentally diminishing amounts of food through the end of the meal have yet to be explored. One possibility is that young children’s stage of cognitive development may influence their eating behaviors (Contento, 1987; Zienestra, Koelen, Kok, & de Graaf, 2007). Another possibility is that conserving some of each of the available foods to the end of the meal is a component of the child’s early-emerging system for social reasoning about food (Liberman, Woodwards, Sullivan & Kinzler, 2016) such as food sharing (Gurven & Jaeggi, 2015). Or it may be that this behavior is a habit acquired from repeated experiences in toddlerhood of the parent responding to early language gestures and requests for “more” in ways that teach that having a certain amount of food left on the plate or tray is a way to signal “all done.” Finding multiple recent studies in the published literature that include statements such as “not clear why elementary students waste as much food as they do” and that “future studies should investigate why younger elementary school students wasted more food than older elementary students” reinforces the call for additional interdisciplinary and cross-cultural research to increase understanding of the development of eating behavior in human childhood (Epstein, Leddy, Temple, & Faith, 2007; Gahagan, 2012).
Given that early in life most infants and children have preference for sweet and salty flavors and aversion to pure vegetable tastes (e.g., Zienestra et al, 2009), it is surprising that perceptual cues of food availability rather than children’s preferences appeared to regulate young children’s lunch food eating in the current study. When LunchBag effected increases in percentage of parents packing vegetables, there was reciprocal increase in percentage of children eating vegetables. When the intervention prevented increase in servings of sweets packed by the parents it also prevented increase in servings of sweets consumed by the children but did not change the eat-to-pack ratio. These results suggest the children’s eating was more responsive to perceptual cues of food availability than to internal hunger and satiety cues (Birch & Fisher, 1998). Because servings of food packed and consumed in the current study were aggregated across multiple food items—e.g., vegetable servings included the tomato sauce on pasta and vegetables in mixed dish as well as whole vegetable items such as baby carrots—it does not appear that portion size per se (Birch, Savage & Fisher, 2015) played a systematic role in regulating the children’s eating of foods from their parent-provided bag lunches.
With or without the intervention, the parents provided and the children consumed ample fruit and meat/beans/eggs/nuts; less than recommended amounts of vegetables and fluid milk; and surfeits of refined grains and foods that are high in added fat, sugar, and salt. Separate analyses of baseline data from LunchBag’s efficacy trial showed that out of the possible 100 points on the Healthy Eating Index (HEI-2010), the average scores were 58 for the lunch meal the parent provided in the packed lunch and 52 for the lunch meal consumed by the child (Romo-Palafox et al, 2015). The amount of vegetables parents packed in their young children’s bag lunches averaged less than half a serving whereas they packed on average one to one and a half servings of sweets. It is unlikely that such lunches will assist the children to acquire and practice eating habits that help to achieve the nationwide objective in the United States to increase vegetables in the diets of persons 2 and older.
The current study indicated little parent-preschooler communication about food. Only 4% of the parents in the intervention condition recalled hearing their children talk about the LunchBag classroom activities, even though some of the classroom activities were presaged by notes from the teachers to the parents requesting that parents send specific items needed for the activity (e.g., sending favorite vegetable for snack time show-and-tell). The intervention effected increases in parents’ report of social support from the child for packing the lunch bag with vegetables and whole grain foods (i.e., asking for, approving, talking about, reminding to buy), but the amount of change only slightly lifted the scores from the baseline reports of “never” or “rarely.” These results are confirming of communications research indicating low levels of parent-child communication about food choices, as well as low involvement from children in food selection and preparation (Ndiyae et al, 2013).
CONCLUSIONS
Results of this study have implications for the further refinement of a bioecological process-person-context-time model (Bronfenbrenner & Morris, 2006) of how lunches brought from home contribute to the development of healthy eating habits in early childhood. Three main ways in which results of the current study were surprising relative to the a priori model undergirding LunchBag were as follows. First, parent disposition toward lunch packing appeared inconsistent with recommendations for healthy lunch meal and potentially developmentally disruptive (e.g., persistence in packing less than recommended amounts of vegetables but large amounts of sweets in the child’s lunch). Second, children’s lunch eating appeared to be regulated by perceptual cues of food availability rather than by preferences, hunger and satiety cues, or portion size per se. Third, although these circumstances place the parent squarely in control of nutrition gatekeeping for the child’s lunch meal, the quality of parent performance in packing healthy lunch fell far short of demanding that the child eat, enjoy, and learn to expect and to prefer healthy foods instead of surfeits of foods high in fat, sugar, and salt. These conclusions about the observed parent-preschooler dietary interactions align with those presented in a recent review of research on mother-child meal-time interactions during the preschool years (Bergmeier, Skouteris, & Hetherington, 2015). That review showed there was no association of maternal reports of feeding practices with observed feeding practices, that parenting style was not directly associated with children’s eating, and that, therefore, future studies should implement longitudinal observational methods to measure parent-child interactions that influence parental feeding practices and children’s eating behaviors. The current results suggest that an important variable to observe in such studies is the proportion consumed by the child of each type of food served.
The current study converges with other calls for continued development and implementation of innovative and effective parent-and-child focused interventions to facilitate the establishment of healthy eating habits in early childhood. Current options include age-appropriate parent-child food-focused reading and arts activities (Heath, Houston-Price, & Kennedy, 2014), mobile games for training vegetable parenting practices (Brand et al, 2015), multi-level and multi-component ECE-based interventions (Ward et al, 2016) such as LunchBag, and strategies that leverage other social and environmental influences (Johnson, 2016) to increase young children’s exposure to and their acceptance of healthy foods and healthy meal patterns.
Having a higher income and better educated sample relative to the general population of families with preschoolers is a limitation of the current study. Although the skew limits generalizability of the results, it is important to note that assessment of the children’s weight status showed 22% with overweight or obesity, and 6% with underweight thereby reinforcing the conclusion that there is need for healthy habit interventions across demographics.
Observation of child eating in the absence of the parent was a strength of the study design that enabled a view of parent-preschooler dietary transactions disentangled from direct social-emotional influence of the parent. An important research task for the future, however, is to determine the extent to which the proportions of food consumed versus conserved to the end of the meal by children in the presence of the parent is systematically different from the ratios obtained in the current study and represented in the research literature on children’s eating in nutrition research laboratories, schools, and ECE centers. Results of this study re-affirm identified need for additional work to understand the dispositions of parent and child in the development of eating habits to support a lifetime of good health.
Acknowledgments
Funding for this study was made possible by the National Cancer Institute (National Cancer Institute/NIH Grant R01CA149643, Clinical Trial Number NCT01292434) and the Michael and Susan Dell Foundation through the Michael and Susan Dell Center for Healthy Living. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute, the National Institutes of Health, or the Michael and Susan Dell Foundation. The authors express appreciation to the directors, teachers, and families of the early care and education centers that participated in the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Cindy Roberts-Gray, Senior Scientist, Third Coast R&D, Inc., 2728 Avenue Q, Galveston, Texas 77550.
Nalini Ranjit, Assistant Professor, Health Promotion/Behavioral Sciences, Michael & Susan Dell Center for Healthy Living, University of Texas School of Public Health Austin Regional Campus, 1616 Guadalupe Street, Suite 6.300, Austin, Texas 78701.
Sara J. Sweitzer, Lecturer, DPD Program Director, Nutritional Sciences, School of Human Ecology, The University of Texas at Austin, 200 W 24th Street, A2700, Austin, Texas 78712.
Courtney E. Byrd-Williams, Assistant Professor, Health Promotion/Behavioral Sciences, Michael & Susan Dell Center for Healthy Living, University of Texas School of Public Health Austin Regional Campus, 1616 Guadalupe Street, 6.300, Austin, Texas 78701.
Maria Jose Romo-Palafox, Postdoctoral Fellow, Michael & Susan Dell Center for Healthy Living, University of Texas School of Public Health Austin Regional Campus, 1616 Guadalupe Street, Suite 6.300, Austin, Texas 78701.
Margaret E. Briley, Professor, Nutritional Sciences, School of Human Ecology, The University of Texas at Austin, 200 W 24th Street, A2700, Austin, Texas 78712-1247.
Deanna M. Hoelscher, Director, Michael & Susan Dell Center for Healthy Living, Professor, Health Promotion/Behavioral Sciences, University of Texas School of Public Health Austin Regional Campus, 1616 Guadalupe Street, 6.300, Austin, Texas 78701.
References
- Abrams KM, Evans C, Duff BRL. Ignorance is bliss: How parents of preschool children make sense of front-of-package visuals and claims on food. Appetite. 2015;87:20–29. doi: 10.1016/j.appet.2014.12.100. [DOI] [PubMed] [Google Scholar]
- Adamo KE, Brett K. Parental perceptions and child dietary quality. Maternal and Child Health Journal. 2014;186:978. doi: 10.1007/s10995-013013266. [DOI] [PubMed] [Google Scholar]
- Aijzen I, Manstead ASR. Changing health related behaviors: An approach based on the Theory of Planned Behavior. In: Hewstone M, Schut H, De Wit J, Van Den Bos K, Stroebe MS, editors. The scope of social psychology: Theory and applications. New York: Psychology Press; 2007. pp. 43–63. [Google Scholar]
- Bandura A. Health promotion by social cognitive means. Health Education & Behavior. 2004;31:143–74. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Baranowski T, Missaghian M, Broadfoot A, Watson K, Cullen K, Nicklas T, Fisher J, Baranowski J, O’Donnell S. Fruit and vegetable shopping practices and social support scales: A validation. Journal of Nutrition Education and Behavior. 2006;38:340–351. doi: 10.1016/j.jneb.2006.06.005. [DOI] [PubMed] [Google Scholar]
- Barlow SE. Expert committee recommendations regarding prevention, assessment, and treatment of child and adolescent overweight and obesity. Pediatrics. 2007;120:S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- Benjamin Neelon SE, Briley ME. Position of the American Dietetic Association: Benchmarks for nutrition in child care. Journal of the American Dietetic Association. 2011;11:607–15. doi: 10.1016/j.jada.2011.02.016. [DOI] [PubMed] [Google Scholar]
- Bergmeier H, Skouteris H, Hetherington M. Systematic research review of observational approaches used to evaluate mother-child mealtime interactions during preschool years. American Journal of Clinical Nutrition. 2015;101:7–15. doi: 10.3945/ajcn.114.092114. [DOI] [PubMed] [Google Scholar]
- Birch LL, Fisher JO. Development of eating behaviors among children and adolescents. Pediatrics. 1998;101:539–549. [PubMed] [Google Scholar]
- Birch LL, Savage JS, Fisher JO. Right sizing prevention. Food portion size effects on children’s eating and weight. Appetite. 2015;88:11–16. doi: 10.1016/j.appet.2014.11.021. [DOI] [PubMed] [Google Scholar]
- Bowman SA, Clemens JC, Friday JE, Lunch KL, LaComb RP, Moshfegh AJ. NHANES 2003–2004 and 2013–2014. U.S. Department of Agriculture Food Survey Research Group; 2017. Food pattern equivalents intakes by Americans: What we eat in America. Dietary Data Brief No. 17 www.ars.usda.gov/nea/bhnrc/fsrg. [PubMed] [Google Scholar]
- Brand L, Beltran A, Buday R, Hughes S, O’Connor T, Baranowski J, Dababhov HR, Diep CS, Baranowski T. Training vegetable parenting practices through a mobile game: Interative qualitative alpha test. JMIR Serious Games. 2015;3:e6. doi: 10.2196/games.4081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3:77–101. [Google Scholar]
- Bronfenbrenner U, Morris PA. The bioecological model of human development. In: Damon W, Lerner RM, editors. Handbook of Child Psychology, Vol 1: Theoretical Models of Human Development. Hoboken, NJ: John Wiley & Sons, Inc; 2006. [Google Scholar]
- Burgess-Champoux TL, Chan HW, Rosen R, Marquart L, Reicks M. Healthy whole-grain choices for children and parents: A multi-component school-based pilot intervention. Public Health Nutrition. 2008;11:849–59. doi: 10.1017/S1368980007001346. [DOI] [PubMed] [Google Scholar]
- Busby JC, Gutherie JF. [Accessed 10/30/2016];Plate Waste in School Nutrition Programs: Final Report to Congress. 2009 E-FAN-02-009, https://naldc.nal.usda.gov/download/48204/PDF.
- CACFP. https://www.fns.usda.gov/sites/default/files/cacfp/CACFP_childadultmealstandards.pdf.
- Contento I. Children’s thinking about food and eating: A Piagetian-based study. Journal of Nutrition Education and Behavior. 1981;13:S86–90. [Google Scholar]
- Cooke LJ, Wardle J, Gibson EL, Sapochnik M, Sheihan A, Lawson M. Demographic, familial, and trait predictors of fruit and vegetable consumption by pre-school children. Public Health Nutrition. 2004;7:295–302. doi: 10.1079/PHN2003527. [DOI] [PubMed] [Google Scholar]
- Cullen K, Chen T, Dave JM, Jensen H. Differential improvements in student fruit and vegetable selection and consumption in response to the new National School Lunch Program regulations: A pilot study. Journal of the Academy of Nutrition and Dietetics. 2015;115:743–750. doi: 10.1016/j.jand.2014.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards W, Newman JR. Multiattribute Evaluation. Thousand Oaks, CA: Sage Publications; 1982. [Google Scholar]
- Epstein LH, Leddy JJ, Temple JL, Faith MS. Food reinforcement and eating: A multi-level analysis. Psychological Bulletin. 2007;133:884–906. doi: 10.1037/0033-2909.133.5.884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feine R. Using childcare programs as a portal for changing eating behaviors. In: Birch L, Dietz W, editors. Influences on Healthy Eating. American Academy of Pediatrics; Elk Grove Village, IL: 2008. pp. 247–278. [Google Scholar]
- Fildes A, van Jaarsveld C, Wardle J, Cooke L. Parent administered exposure to increase children’s vegetable acceptance: A randomized control trial. Journal of the Academy of Nutrition and Dietetics. 2014;114:881–888. doi: 10.1016/j.jand.2013.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisk C, Crozier S, Inskip H, Codgrey K, Cooper C, Robinson S. Influences on quality of young children’s diets: The importance of maternal food choices. British Journal of Nutrition. 2011;105:287–296. doi: 10.1017/S0007114510003302. [DOI] [PubMed] [Google Scholar]
- Gahagan S. The development of eating behavior: Biology and context. Journal of Developmental & Behavioral Pediatrics. 2012;33:261–271. doi: 10.1097/DBP.0b013e31824a7baa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurven M, Jaeggi AV. Food sharing. In: Scott R, Kosslyn S, editors. Emerging Trends in Social and Behavioral Sciences. John Wiley & Sons, Inc; 2015. [Google Scholar]
- Heath P, Houston-Price C, Kennedy OB. Let’s look at leeks! Picture books increase toddlers’ willingness to look at, taste, consume vegetables. Frontiers of Psychology. 2014;5:191. doi: 10.3389/fpsyg.2014.00191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughner RS, Maher JK. Factors that Influence Parental Food Purchases for Children: Implications for Dietary Health. Journal of marketing management. 2006;22:929–954. [Google Scholar]
- Johnson SL. Developmental and environmental influences on young children’s vegetable consumption. Advances in Nutrition. 2016;7:220S–231S. doi: 10.3945/an.115.008706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kranz S, Hartman T, Siega-Riz AM, Herring AH. A diet quality index for American preschoolers based on current dietary intake recommendations and an indicator or energy balance. J Am Diet Assoc. 2006;106:1594–1604. doi: 10.1016/j.jada.2006.07.005. [DOI] [PubMed] [Google Scholar]
- Laughlin L. Who’s minding the kids? Child care arrangements: Spring 2011. 2013 www.census.gov/prod/2013pubs/p70-135.pdf.
- Lakkakula AP, Zanovec M, Silverman L, Murphy E, Tuuri G. Black children with high preferences for fruits and vegetables are at less risk of being at risk of overweight or obesity. J Am Diet Assoc. 2008;108:1912–5. doi: 10.1016/j.jada.2008.08.019. [DOI] [PubMed] [Google Scholar]
- Leahy KE, Birch LL, Fisher JO, Rolls BJ. Reductions in entrée energy density increase children’s vegetable intake and reduce energy intake. Obesity. 2008;2008(16):1559–65. doi: 10.1038/oby.2008.257. [DOI] [PubMed] [Google Scholar]
- Liberman Z, Woodwards AL, Sullivan KR, Kinzler KD. Early emerging system for reasoning about the social nature of food. Proceedings of the National Academy of Sciences (PNAS) 2016;113:9480–9485. doi: 10.1073/pnas.1605456113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Survey of Early Care and Education Project Team. OPRE Report #201473a. Washington DC: Office of Planning, Research and Evaluation, Administration for Children and Families, U.S. Department of Health and Human Services; 2014. [Accessed 9/13/2017]. Characteristics of Center-based Early Care and Education Programs. Available http:/www.acf.hhs.gov/programs/opre/index.html. [Google Scholar]
- Ndiyae K, Silk K, Anderson J, Kranstuber Horstman H, Carpenter A, Hurley A, Proulx J. Using an ecological framework to understand parent-child communication about nutritional decision-making and behavior. Journal of Applied Communication Research. 2013;41:253–274. [Google Scholar]
- Nicklas TA, Liu Y, Stuff JE, Fisher JO, Mendoza JA, O’Neil CE. Characterizing lunch meals served and consumed by preschool children in Head Start. Public Health Nutrition. 2013;16:2169–2177. doi: 10.1017/S1368980013001377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potratz C, Byrd-Williams C, Sweitzer S, Roberts-Gray C, Briley ME, Hoelsher D. Directors’ perspectives on early care and education centers’ interactions with parents about food brought from home. Poster presentation at the meeting of the Society for Nutrition Education and Behavior.2014. [Google Scholar]
- Roberts-Gray C, Briley ME, Ranjit N, Byrd-Williams CE, Sweitzer SJ, Sharma SV, Palafox MR, Hoelscher DM. Efficacy of the Lunch is in the Bag intervention to increase parents’ packing of healthy bag lunches for young children: A cluster-randomized trial in early care and education centers. International Journal of Behavioral Nutrition and Physical Activity. 2016a;13:3. doi: 10.1186/s12966-015-0326-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts-Gray C, Swetizer SJ, Ranjit N, Potratz C, Rood M, Romo-Palafox MJ, Byrd-Williams CE, Briley ME, Hoelscher DM. Structuring process evaluation to forecast use and sustainability of an intervention: Theory and data from the efficacy trial for Lunch is in the Bag. Health Education & Behavior. 2016b doi: 10.1177/1090198116676470. pii: 1090198116676470. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Romo-Palafox MJ, Ranjit N, Sweitzer SJ, Roberts-Gray C, Hoelscher DM, Byrd-Williams CE, Briley ME. Dietary quality of preschoolers’ sack lunches as measured by the Healthy Eating Index. Journal of the Academy of Nutrition and Dietetics. 2015;115:1779–1788. doi: 10.1016/j.jand.2015.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma SV, Tasnuva R, Ranjit N, Byrd-Williams C, Chuang R, Roberts-Gray C, Briley ME, Hoelscher DM. Effectiveness of the Lunch is in the Bag program on communication between the parent, child and childcare provider around fruits, vegetables, and whole grain foods: A group randomized control trial. Preventive Medicine. 2015;81:1–8. doi: 10.1016/j.ypmed.2015.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith SI, Cunningham-Sabo L. Food choice, plate waste and nutrient intake of elementary- and middle-school students participating in the US National School Lunch Program. Public Health Nutrition. 2014;17:1255–1263. doi: 10.1017/S1368980013001894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swetizer SJ, Byrd-Williams C, Ranjit N, Briley ME, Roberts-Gray C, Hoelscher D. Development of a method to observe preschoolers’ packed lunches in Early Care and Education centers. Journal of the Academy of Nutrition and Dietetics. 2015;115:1249–1259. doi: 10.1016/j.jand.2015.03.012. [DOI] [PubMed] [Google Scholar]
- Sweitzer SJ, Ranjit N, Calloway EE, Hoelscher DM, Almansour F, Briley ME, Roberts-Gray C. Examining how adding a booster to a behavioral nutrition intervention prompts parents to pack more vegetables and whole grains in their preschool children’s sack lunches. Behavioral Medicine. 2014;42:9–17. doi: 10.1080/08964289.2014.935283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweitzer SJ, Briley ME, Roberts-Gray C, Hoelscher DM, Staskel D, Almansour F. Pyschosocial outcomes of Lunch is in the Bag, a parent program for packing healthful lunches for preschool children. Journal of Nutrition Education and Behavior. 2011;43:536–42. doi: 10.1016/j.jneb.2010.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweitzer SJ, Briley ME, Roberts-Gray C, Hoelscher DM, Staskel D, Almansour F. A Pilot Study of Lunch is in the Bag: Increasing Fruits, Vegetables and Whole Grains in Sack Lunches for Preschool-aged Children. Journal of the American Dietetic Association. 2010;110:1058–1064. doi: 10.1016/j.jada.2010.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorsen AV, Lassen AD, Anderson EW, Christensen LM, Biltoft-Jensen A, Andersen R, Damsgaard CT, Michaelsen KF, Tetens I. Plate waste and intake of school lunch based on the new Nordic diet and on packed lunches: A randomized controlled trial in 8- to 11-year old Danish children. Journal of Nutrition Science. 2015;4:e20. doi: 10.1017/jns.2015.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Agriculture. Early Childhood and Child Care Study: Summary of Findings. Food and Consumer Service, Office of Analysis & Evaluation; 1997. Jul, [Accessed 11/23/16]. http://www.fns.usda.gov/sites/default/files/CHLDCARE.PDF. [Google Scholar]
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. [accessed 9/12/17];2015–2020 Dietary Guidelines for Americans. (8). 2015 https://health.gov/dietaryguidelines/2015/
- Vollmer RL, Baietto J. Practices and preferences: Exploring the relationships between food-related parenting practices and child food preferences for high fat and/or sugar foods, fruits, and vegetables. Appetite. 2017;113:134–40. doi: 10.1016/j.appet.2017.02.019. [DOI] [PubMed] [Google Scholar]
- Wansink B, Johnson KA. Adults only: Why don’t children belong to the clean-plate club? International Journal of Obesity. 2015;39:375. doi: 10.1038/ijo.2014.205. [DOI] [PubMed] [Google Scholar]
- Ward DS, Welker E, Choate A, Henderson KE, Lott M, Tovac A, Wilson A, Sallis JF. Strength of obesity prevention interventions in early care and education settings: A systematic review. Preventive Medicine. 2016 doi: 10.1016/j.ypmed.2016.09.033. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Webber L, Cooke L, Hill C, Wardle J. Associations between children’s appetitive traits and maternal feeding practices. Journal of the American Dietetic Association. 2010;110:1718–22. doi: 10.1016/j.jada.2010.08.007. [DOI] [PubMed] [Google Scholar]
- Wyse R, Campbell E, Nathan N, Wolfenden L. Associations between characteristics of the home food environment and fruit and vegetable intake in preschool children: A cross-sectional study. BMC Public Health. 2011;11:938. doi: 10.1186/1471-2458-11-938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zienstra GG, Koelen MA, Kok FJ, deGraaf C. Cognitive development and children’s perceptions of fruit and vegetables: A qualitative study. International Journal of Behavioral Nutrition and Physical Activity. 2007;4:30. doi: 10.1186/1479-5868-4-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zienstra GG, Koelen MA, Kok FJ, deGraaf C. Children’s hard-wired aversion to pure vegetable tastes: A ‘failed’ flavor-nutrient learning study. Appetite. 2009;52:528–530. doi: 10.1016/j.appet.2008.11.006. [DOI] [PubMed] [Google Scholar]