Abstract
Introduction
There is limited research on why women do or do not choose a career in urology. Considering the increasing proportion of female medical students, we assessed for trends in female applicants to urology programs in Canada and their post-residency career choices.
Methods
Data from the Canadian Residency Matching Service (CaRMS) was used (1998–2015). Trends in the proportions of females applying and matching to surgical subspecialties, and applying and matching to urology were computed. Surveys were sent to urology program directors to assess female residents’ chosen career paths over the last decade.
Results
A significant increasing trend in the proportion of females applying to urology as their first choice program was found (0.19 in 1998–99 to 0.27 in 2012–15; p=0.04). An increasing trend in the proportion of females successfully matching to urology was found, although it was not statistically significant (0.13 in 1998–99 to 0.24 in 2012–15; p=0.07). This was in keeping with the trends found for surgical programs overall. Female graduates choose a variety of career paths, with urogynecology being the most common fellowship (26%).
Conclusions
The last two decades has seen an increase in the proportion of female students applying to urology in Canada. Female urology graduates pursue a variety of career paths. It remains imperative that both female and male medical students have early exposure and education about our subspecialty to ensure we continue to recruit the most talented candidates.
Introduction
In the mid-1970s, the first woman graduated from a Canadian urology residency program.1 Subsequently, many more females have completed residency and joined the ranks of practicing urologists across Canada. Yet, the majority of practicing urologists are male.
The male predominance is not unique to urology. In the U.S., urology has the third lowest proportion of female residents across all surgical specialties, higher only than orthopedics and neurosurgery.2 Canadian data indicate that the only surgical specialty that has enrolled a consistently genderneutral cohort over the past two decades is general surgery.3 Many factors have been cited to explain the gender disparity across most surgical training programs. In earlier years, a sheer lack of women entering medical school contributed to the higher number of male surgical residents; however, since the 1970s, the enrolment of women in medical schools across Canada and the U.S. has been increasing such that currently, females occupy approximately half of the seats.3–5
There is emerging research that examines why medical students choose to pursue a career in surgery6,7 and urology in particular.8 Common themes regarding why women are dissuaded from applying to a surgical residency include: lack of female role models, perceived unattractive lifestyle, negative experiences in surgery, and supposed inability to fit into a masculine career.7,9,10 To date, there is limited research on why female medical students do or do not choose a career in urology. In addition, information regarding the experiences and outcomes of women in urology is lacking.
Given the changing gender ratio of graduating medical students, our primary objective was to assess the trends in the proportion of female applicants to Canadian urology programs. Our second objective was to explore if there was a propensity for women in urology to pursue particular fellowships, enter community practice, or leave Canada to practice elsewhere. We hypothesized that the proportion of female medical graduates who ranked urology as their first choice and who matched to urology has increased over the last 15 years.
Methods
This retrospective study used data collected from two sources. First, publically available data from the Canadian Resident Matching Service (CaRMS) website on residency match results for Canadian medical school graduates from 1998–2015 was accessed.3 We used data starting in 1998, as this is when CaRMS began to report the gender of the matched student online. The data we collected included total number of:
CaRMS applicants
Surgical discipline residency positions
Applicants who ranked a surgical program as first choice
Applicants who matched to a surgical program
Urology positions
Applicants who ranked urology as their first choice
Applicants who matched to urology
Although it was not our primary outcome, we collected data on “surgical disciplines” in addition to the data on urology alone. Available CaRMS data for surgical disciplines included: cardiac surgery, general surgery, neurosurgery, ophthalmology, orthopedic surgery, otolaryngology – head & neck surgery, plastic surgery, urology, and vascular surgery. Of note, obstetrics and gynecology was not included in the surgical disciplines grouping by CaRMS. We elected to collect these data to act as a baseline comparison to the trends we assessed in urology programs alone.
The second part of our study consisted of a survey of Canadian urology residency program directors (PDs). The current PDs were sent an email with a letter detailing the study intent and requested information. The letter was written in both English and French. The information requested from 2005 until 2015 included (Appendix 1):
Appendix 1.
Females in urology in Canadian residency programs:
| Please complete this table with as much information as you have available. Spaces should be filled in with a number (no identifying data) except for the columns specifying fellowship types. | |||||||
|
| |||||||
| University: __________________________ | |||||||
|
| |||||||
| Year | Females matched to PGY1 | Total matched positions | Females completed residency | Total residency graduates | Female graduate began a fellowship* | Female graduate began working in community | Female graduate started working in USA |
|
| |||||||
| 2015 | |||||||
| 2014 | |||||||
| 2013 | |||||||
| 2012 | |||||||
| 2011 | |||||||
| 2010 | |||||||
| 2009 | |||||||
| 2008 | |||||||
| 2007 | |||||||
| 2006 | |||||||
| 2005 | |||||||
| *Please indicate what fellowship the female urology graduate went in to | |||||||
| Additional comments: | |||||||
| Example table | |||||||
|
| |||||||
| Please complete this table with as much information as you have available. Spaces should be filled in with a number (no identifying data) except for the columns specifying fellowship types. | |||||||
|
| |||||||
| University: Jon Snow Memorial University | |||||||
|
| |||||||
| Year | Females matched to PGY1 | Total matched positions | Females completed residency | Total residency graduates | Female graduate began a fellowship* | Female graduate began working in community | Female graduate started working in USA |
|
| |||||||
| 2015 | 1 | 5 | 3 | 5 | |||
| 2014 | 0 | 5 | 5 | ||||
| 2013 | 0 | 5 | 4 | ||||
| 2012 | 0 | 5 | 5 | 1 | |||
| 2011 | 0 | 5 | 2 | 5 | 1 - Pediatrics | 1 | |
| 2010 | 3 | 5 | 4 | ||||
| 2009 | 0 | 5 | 5 | ||||
| 2008 | 0 | 5 | 5 | ||||
| 2007 | 0 | 5 | 5 | ||||
| 2006 | 2 | 5 | 1 | 5 | 1 – UroGyne | ||
| 2005 | 0 | 5 | 5 | ||||
| *Please indicate what fellowship the female urology graduate went in to | |||||||
| Additional comments: | |||||||
Number of females entering their residency program
Number of female graduates
Number of female graduates entering community practice in Canada or the U.S.
Number of graduates pursuing fellowship training
Type of subspecialty training
To help improve the accuracy of the survey results, the Canadian Urological Association (CUA) provided the individual PDs with anonymous data on the 2008–2015 female graduates from their respective programs. It was sent in a reminder email to PDs as a reference for their survey responses. This was information that had been provided to the CUA by the PDs in past years. The identity of the residents was not requested at any point in time for the purpose of this study.
Local research ethics board approval was obtained prior to the commencement of this study.
Analysis
We analyzed the proportion of female and male applicants to CaRMS, the proportion of female and male applicants who ranked a surgical program as first choice, the proportion of female and male applicants who matched to a surgical program, the proportion of female and male applicants who ranked urology as first choice, and the proportion of female and male applicants who matched to urology. Proportions were calculated for each of five time periods (1998–1999, 2000–2003, 2004–2007, 2008–2011, and 2012–2015). Changes across time periods were assessed using the chi-square test for trends.
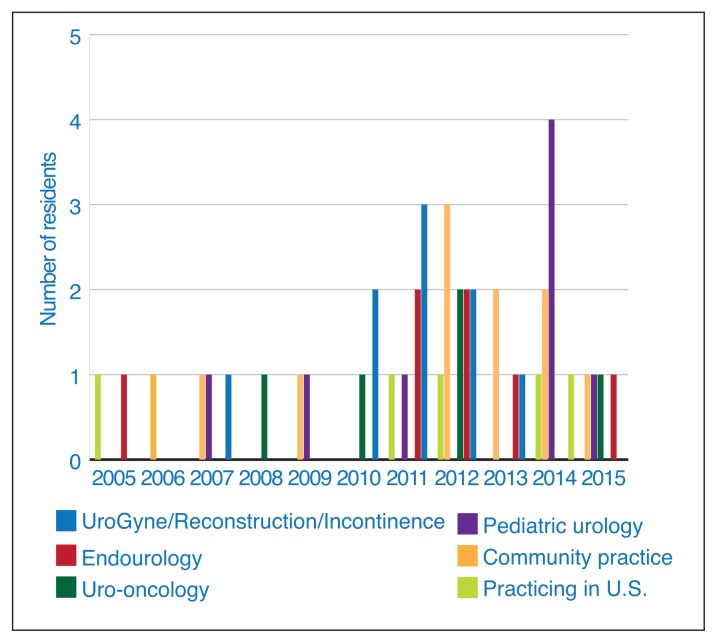
Descriptive statistics were used to report survey data from PDs and visually displayed using histograms.
All statistical analyses were performed using STATA version 13.1 (StataCorp. 2013. College Station, TX, U.S.). A p value of <0.05 was considered the threshold for statistical significance.
Results
CaRMS data
1. CaRMS applicants
Available CaRMS data broken down by gender was complete from 1998–2015 (Supplementary Tables 1, 2). During that timeframe, we found an increasing trend in the proportion of females applying in the CaRMS match (0.47 in 1998–99 to 0.56 in 2012–15; p<0.001).
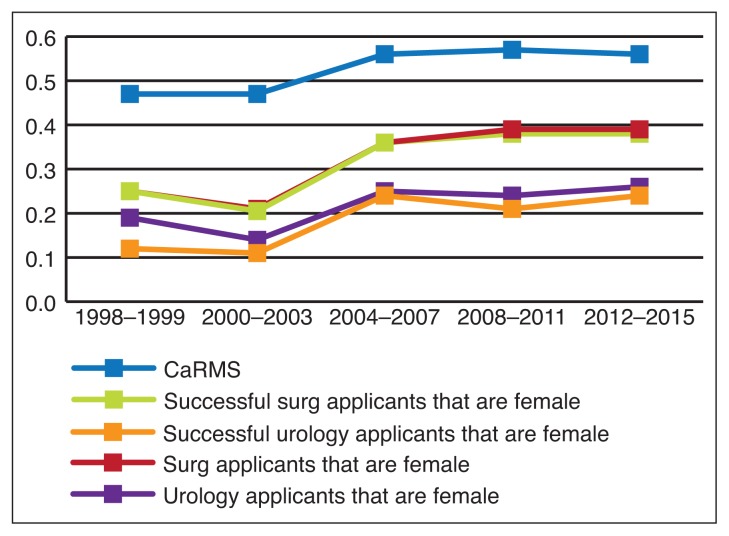
We assessed for trends in female medical students applying to surgical programs overall. First, we assessed the proportion of females applying to surgery as their first choice out of all the females applying in CaRMS. This analysis did not reveal a trend towards an increasing proportion of females applying to surgical programs (0.11 in 1998–99 to 0.10 in 2012–15; p=0.99). Conversely, when looking at the proportion of male students applying to surgical programs out of all the males applying to CaRMS, we identified a statistically significant decreasing trend in the proportion of male applicants to surgical programs (0.28 in 1998–99 to 0.19 in 2012–15; p<0.001) (Table 1, Fig. 1).
Table 1.
Applicants to CaRMS and surgical specialties based on gender
| Year cohort | Female applicants in CaRMS (%) | Females applying to surgical specialties (%)a | Males applying to surgical specialties (%) | Surgical applicants that are female (%)b | Matched to surgical programs (female)c |
|---|---|---|---|---|---|
| 2012–2015 | 56 | 10 | 19 | 40 | 38 |
| 2008–2011 | 57 | 12 | 24 | 40 | 38 |
| 2004–2007 | 56 | 12 | 27 | 36 | 36 |
| 2000–2003 | 47 | 9 | 28 | 22 | 21 |
| 1998–1999 | 47 | 11 | 28 | 25 | 25 |
Proportions of females applying to surgical specialties out of all the females applying to CaRMS.
Proportion of females ranking surgical programs first out of all the applicants ranking surgical programs as first choice.
Proportion of females who matched to a surgical program out of all the applicants that ranked a surgical program as first choice.
Fig. 1.
Comparison of trends in the proportions of female applicants to CaRMS, surgical specialties, and urology (1998–2015).
2. Applicants to surgical programs
The cohort of applicants who ranked surgical programs as their first choice was then assessed. We broke this cohort down by gender. This analysis revealed that there was a significant increasing trend in the proportion of female applicants who ranked a surgical program as their first choice (0.25 in 1998–99 to 0.40 in 2012–15; p=0.001).
In order to clarify these findings, we provide this example: Although consistently there are approximately 10% of all female medical students applying to surgical programs, as the overall number of female medical students increases this has resulted in a larger overall number of females in the surgical applicant pool. For example, if there were only 50 female medical students in Year A then five (or 10%) would apply to surgery. However, if there were 100 female medical students in Year B then 10 (or 10%) would apply. If the total number of surgical residency seats is 20, then the proportion of females in the surgical applicant pool has changed from 5/20 (25%) to 10/20 (50%).
We then examined the applicants that matched to any surgical program as their first choice. In this cohort, there was a significant increasing trend in the proportion of successful female applicants (0.25 in 1998–99 to 0.38 in 2012–15; p<0.001) (Table 1, Fig. 1).
3. Applicants to urology
We assessed for trends in the proportion of urology applicants that were female. We found a significant increasing trend in the proportion of females applying to urology as their first choice program from 1998–2015 (0.19 in 1998–99 to 0.27 in 2012–15; p=0.04). We found an increasing trend in the proportion of females successfully matching to urology, although it was not found to be statistically significant (0.13 in 1998–99 to 0.24 in 2012–15; p=0.07) (Table 2). When represented graphically, these data do suggest a positive trend towards an increasing proportion of successful female applicants to urology since 1998 (Fig. 1).
Table 2.
Applicants to Canadian urology programs based on gender
| Year cohort | Urology applicants that are female (%)a | Applicants who matched to urology that are female (%)b |
|---|---|---|
| 2012–2015 | 27 | 24 |
| 2008–2011 | 24 | 22 |
| 2004–2007 | 25 | 24 |
| 2000–2003 | 14 | 12 |
| 1998–1999 | 19 | 13 |
Proportion of females ranking urology as first choice out of all the applicants ranking urology first choice.
Proportion of females who matched to urology out of all the applicants who matched to urology.
Post-residency career paths
A total of 11 responses were obtained from the 13 Canadian urology residency PDs (85% response rate). The proportion of reported females beginning and graduating residency varied significantly by year.
Female graduates choose a variety of career paths following completion of their residency. Community practice, as well as urogynecology/reconstruction and pediatric urology were most prevalent. Urogynecology/reconstruction was the most common fellowship, pursued by 26% of female graduates. There were no reports of female graduates pursuing fellowships in the fields of transplantation, infertility, or male sexual dysfunction (Fig. 2).
Fig. 2.
Female graduate career paths after urology residency in Canada (2005–2015).
Discussion
As expected, our study confirms the increasing proportion of females applying in CaRMS from 1998–2015. In terms of surgical disciplines, our study suggests that approximately 10% of female medical students apply to surgical specialties each year and that this has not changed over time. However, of those students who apply to surgery, there has been an increase in the proportion that are female. This is reflected by the fact that there are now more female medical students and the percentage of male medical students who apply to surgery seems to be decreasing (from 28% in 1998–99 to 19% in 2012–15). We have also found an increasing trend in the proportion of females applying to surgery who are successful in matching.
There has been some concern in recent years that surgical programs have become less desirable and the reasons behind the decline in interest in surgical specialties has been studied.6,11,12 One study found that medical students value work-life balance and have a greater interest in having protected time for self and family.11 This lack of a “controllable lifestyle” is often cited as an important factor that dissuades students from pursuing a career in surgery and does not seem to be based on gender.11,13
One theory about the decreasing interest in surgery is that there are more women in medical school and therefore less people applying to surgical programs.7 Our data suggest that in Canada, the proportion of surgery applicants that are female is increasing. Perhaps the answer to why there are less applicants to surgery is multifaceted and may include: perceptions regarding the difficulty of residency, lack of knowledge and good role models, and misconceptions about future career satisfaction.7,11,12 In addition, our data did not report on the number of females applying to obstetrics and gynecology and it is possible that more females are taking on a surgical career in this field.
As with the overall surgical disciplines, we found the proportion of females applying to urology has increased over the past two decades. We also found the proportion of females matching to urology has increase over the past two decades, although this trend was not statistically significant. This is likely due to a small sample size. The most recent cohort for applicants to urology (2012–2015) indicates that nearly one-quarter of PGY-1 urology residents in Canada are female. This is comparable to recent data from the U.S. where 23% of urology residents in 2011 were female.14
A survey of medical students applying to urology commonly cited that the mix of medicine and surgery, the diversity of procedures, and clinical exposure to the field as main reasons why they were interested in pursuing a career in urology.8 There is little data regarding why female students in particular choose a career in urology. One small survey study of female urology residents inquired about the factors that influenced the residents’ decision to choose urology when they were a medical student.15 The three most important factors identified were: diversity of procedures, diversity of practice, and lifestyle. It remains imperative that both female and male medical students have early exposure and education about our subspecialty to ensure that we continue to recruit the most talented candidates. As well, access to mentorship seems to play a role in guiding trainees at different levels of training. This may be particularly important for women, as there is the perception that it is more challenging for women to find mentors than their male colleagues.16 The smaller number of female surgeons may be a hindrance in recruiting future female residents, as they may be discouraged by lack of mentorship availability.
For graduating female residents, fellowships in urogynecology/reconstruction or pediatrics, or starting practice as a community urologist were the most common career paths. Urogynecology/reconstruction was the most commonly pursued fellowship.
A recent study looking at gender differences in publications by academic urologists in the U.S. also found that females were more likely to do a fellowship in female pelvic medicine/reconstructive surgery or pediatric urology.17 Oberlin et al found that female urologists operated on many more female patients than did their male counterparts (54% vs. 32%, respectively), even when they were performing gender-neutral surgeries or had gender-neutral fellowship training, such as endourology.18 There are likely several reasons for this finding, including the fact that female urologists frequently have subspecialty training in urogynecology and reconstructive urology. As well, some literature shows that female patients have a gender preference for female physicians. 19
Other paths that female urology residents chose included fellowships in endourology and oncology, with reportedly no female graduates choosing fellowships in transplantation or infertility in the past decade. As mentioned above, one of the reasons for few residents choosing these subspecialties may be related to a lack of female mentors, such as female urological oncologists, in these areas of subspecialties.20
Our study does have some limitations. In regards to the data used from CaRMS, we were only able to use the information available online through their website. Although what was collected was robust, it is reported only for applicants who ranked the specialty as their first choice. It is conceivable that we may have missing data for applicants who matched to a surgical specialty but did not rank it as their first choice program.
A second limitation of our study is that we were evaluating small numbers of applicants and therefore finding statistically significant trends in the data may be difficult due to the large amount of variation from year to year. For this reason, we divided the CaRMS data into four-year cohorts.
Thirdly, our survey study of PDs may have been subject to recall bias about the career paths of graduating residents. Finally, we did not collect information from the PDs regarding the career paths of the male graduates so we are unable to draw a direct comparison between female and male career paths.
Conclusion and clinical implications
Over the last 18 years in Canada, there has been an increasing proportion of females applying and successfully matching to urology. As the proportion of female medical students is increasing, it is encouraging that we are seeing more interest in our specialty through the increasing trend in female applicants.
In Canada, female urology graduates pursue many career paths following residency. It remains important that female residents have early exposure to multiple subspecialty areas in urology and mentorship throughout their residencies, in order to choose a successful career path. Further data regarding the quality of life of females who have chosen a career in urology is needed.
Supplementary materials
Supplementary Table 1.
CaRMS data by year for surgical specialties
| Year | Total number of females in the match | Total number of males in the match | Female: 1st choice discipline = Surgery | Female: Matched to 1st choice surgical specialty | Male: 1st choice = Surgery | Male: Matched to 1st choice surgical specialty |
|---|---|---|---|---|---|---|
| 2015 | 1574 | 1288 | 147 | 108 | 211 | 164 |
| 2014 | 1599 | 1248 | 161 | 120 | 208 | 153 |
| 2013 | 1537 | 1158 | 153 | 98 | 276 | 202 |
| 2012 | 1536 | 1136 | 161 | 112 | 244 | 194 |
| 2011 | 1447 | 1081 | 173 | 124 | 254 | 190 |
| 2010 | 1419 | 1019 | 186 | 126 | 240 | 188 |
| 2009 | 1317 | 996 | 141 | 104 | 232 | 183 |
| 2008 | 1216 | 918 | 141 | 103 | 240 | 183 |
| 2007 | 1173 | 827 | 151 | 105 | 232 | 166 |
| 2006 | 1136 | 800 | 117 | 90 | 208 | 164 |
| 2005 | 786 | 619 | 83 | 66 | 155 | 123 |
| 2004 | 644 | 641 | 78 | 58 | 174 | 113 |
| 2003 | 610 | 621 | 58 | 39 | 176 | 129 |
| 2002 | 506 | 611 | 49 | 33 | 184 | 125 |
| 2001 | 520 | 612 | 40 | 28 | 159 | 113 |
| 2000 | 526 | 628 | 49 | 28 | 168 | 116 |
| 1999 | 565 | 584 | 61 | 34 | 161 | 116 |
| 1998 | 532 | 640 | 56 | 41 | 187 | 115 |
Supplementary Table 2.
CaRMS data for applicants to urology by year
| Year | Total # of applicants | Quota of positions offered to CMGs | Females who ranked Urology as 1st choice program | Females who matched to Urology as 1st choice | Males who ranked Urology as 1st choice program | Males who matched to Urology as 1st choice |
|---|---|---|---|---|---|---|
| 2015 | 49 | 33 | 5 | 3 | 27 | 23 |
| 2014 | 53 | 31 | 22 | 14 | 21 | 17 |
| 2013 | 69 | 33 | 8 | 4 | 38 | 28 |
| 2012 | 48 | 33 | 7 | 7 | 28 | 22 |
| 2011 | 47 | 31 | 7 | 5 | 35 | 23 |
| 2010 | 64 | 30 | 16 | 8 | 34 | 22 |
| 2009 | 52 | 31 | 7 | 5 | 25 | 23 |
| 2008 | 54 | 30 | 9 | 7 | 30 | 22 |
| 2007 | 52 | 28 | 11 | 7 | 27 | 21 |
| 2006 | 47 | 26 | 8 | 6 | 27 | 20 |
| 2005 | 28 | 18 | 8 | 7 | 14 | 11 |
| 2004 | 27 | 17 | 3 | 1 | 24 | 16 |
| 2003 | 45 | 17 | 5 | 1 | 23 | 14 |
| 2002 | 42 | 15 | 4 | 3 | 26 | 12 |
| 2001 | 36 | 15 | 2 | 1 | 17 | 12 |
| 2000 | 40 | 15 | 3 | 2 | 17 | 13 |
| 1999 | 44 | 17 | 4 | 1 | 19 | 14 |
| 1998 | 44 | 18 | 5 | 3 | 19 | 14 |
Footnotes
Competing interests: Dr. Tennankore has received a research grant from Amgen and has participated in clinical trials supported by Bayer and Pfizer. Dr. Cox has been an advisor for Astellas and Ferring; has received speaker fees from Astellas and Pfizer; and has participated in a clinical trial supported by Aquinox. The remaining author reports no competing personal or financial interests.
This paper has been peer-reviewed.
References
- 1.Hill C. On becoming the first woman urologist in Canada. CMAJ. 1980;3:356. [PMC free article] [PubMed] [Google Scholar]
- 2.Halpern JA, Lee UJ, Wolff EM, et al. Women in urology residency, 1978–2013: A critical look at gender representation in our specialty. Urology. 2016;92:20–5. doi: 10.1016/j.urology.2015.12.092. https://doi.org/10.1016/j.urology.2015.12.092. [DOI] [PubMed] [Google Scholar]
- 3.Canadian Resident Matching Service. CaRMS: R-1 match reports. [Updated 2015] [Accessed Sept. 1, 2016]. Available at http://www.carms.ca/en/data-and-reports/r-1/
- 4.Association of American Medical Colleges. Table B-1.2: Total Enrolment by U.S. Medical School and Sex, 2012–2013 through 2016–2017. [Accessed March 17, 2017]. [Updated December 2016]. Available at https://www.aamc.org/data/facts/
- 5.The Association of Faculties of Medicine of Canada. Table 8: Enrolment in Canadian Faculties of Medicine by Sex, 1968/69 2015/16. [Accessed June 12, 2017]. [Updated 2016]. Available at https://afmc.ca/sites/default/files/CMES2016-Section2-Enrolment.pdf.
- 6.Scott IM, Matejcek AN, Cowans MC, et al. Choosing a career in surgery: Factors that influence Canadian medical students’ interest in pursuing a surgical career. Can J Surg. 2008;5:371–7. [PMC free article] [PubMed] [Google Scholar]
- 7.Hill EJ, Bowman KA, Stalmeijer RE, et al. Can I cut it? Medical students’ perceptions of surgeons and surgical careers. Am J Surg. 2014;5:860–7. doi: 10.1016/j.amjsurg.2014.04.016. https://doi.org/10.1016/j.amjsurg.2014.04.016. [DOI] [PubMed] [Google Scholar]
- 8.Kerfoot BP, Nabha KS, Masser BA, et al. What makes a medical student avoid or enter a career in urology? Results of an international survey. J Urol. 2005;5:1953–7. doi: 10.1097/01.ju.0000177462.61257.4e. https://doi.org/10.1097/01.ju.0000177462.61257.4e. [DOI] [PubMed] [Google Scholar]
- 9.Peters K, Ryan M, Haslam SA, et al. To belong or not to belong: Evidence that women’s occupational disidentification is promoted by lack of fit with masculine occupational prototypes. J Pers Psychol. 2012;11:148–58. https://doi.org/10.1027/1866-5888/a000067. [Google Scholar]
- 10.Park J, Minor S, Taylor RA, et al. Why are women deterred from general surgery training? Am J Surg. 2005;1:141–6. doi: 10.1016/j.amjsurg.2005.04.008. https://doi.org/10.1016/j.amjsurg.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 11.Sanfey HA, Saalwachter-Schulman AR, Nyhof-Young JM, et al. Influences on medical student career choice: Gender or generation? Arch Surg. 2006;11:1086–94. doi: 10.1001/archsurg.141.11.1086. https://doi.org/10.1001/archsurg.141.11.1086. [DOI] [PubMed] [Google Scholar]
- 12.Minor S, Poenaru D, Park J. A study of career choice patterns among Canadian medical students. Am J Surg. 2003;2:182–8. doi: 10.1016/s0002-9610(03)00181-8. https://doi.org/10.1016/S0002-9610(03)00181-8. [DOI] [PubMed] [Google Scholar]
- 13.Lambert EM, Holmboe ES. The relationship between specialty choice and gender of U.S. medical students, 1990–2003. Acad Med. 2005;9:797–802. doi: 10.1097/00001888-200509000-00003. https://doi.org/10.1097/00001888-200509000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Grimbsy G, Wolter C. The journey of women in urology: The perspective of a female urology resident. Urology. 2013;1:3–6. doi: 10.1016/j.urology.2012.07.050. [DOI] [PubMed] [Google Scholar]
- 15.Jackson I, Bobbin M, Jordan M, et al. A survey of women urology residents regarding career choice and practice challenges. J Womens Health (Larchmt) 2009;11:1867–72. doi: 10.1089/jwh.2008.1236. https://doi.org/10.1089/jwh.2008.1236. [DOI] [PubMed] [Google Scholar]
- 16.Samunjak D, Straus SE, Marusic A. Mentoring in academic medicine: A systematic review. JAMA. 2006;9:1103–15. doi: 10.1001/jama.296.9.1103. https://doi.org/10.1001/jama.296.9.1103. [DOI] [PubMed] [Google Scholar]
- 17.Mayer E, Lenherr S, Hanson H, et al. Gender differences in publication productivity among academic urologists in the United States. Urology. 2017;103:39–46. doi: 10.1016/j.urology.2016.12.064. https://doi.org/10.1016/j.urology.2016.12.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oberlin DT, Vo AX, Bachrach L, et al. The gender divide: The impact of surgeon gender on surgical practice patterns in urology. J Urol. 2016;5:1522–6. doi: 10.1016/j.juro.2016.05.030. https://doi.org/10.1016/j.juro.2016.05.030. [DOI] [PubMed] [Google Scholar]
- 19.Tempest HV, Vowler S, Simpson A. Patients’ preference for gender of urologist. Int J Clin Pract. 2005;5:526–8. doi: 10.1111/j.1368-5031.2005.00465.x. https://doi.org/10.1111/j.1368-5031.2005.00465.x. [DOI] [PubMed] [Google Scholar]
- 20.Harnisch BA, Stolzmann KL, Kerner LB. Mentoring, fellowship training, and academic careers of women urologists. BJU Int. 2010;12:1629–31. doi: 10.1111/j.1464-410X.2010.09391.x. https://doi.org/10.1111/j.1464-410X.2010.09391.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1.
CaRMS data by year for surgical specialties
| Year | Total number of females in the match | Total number of males in the match | Female: 1st choice discipline = Surgery | Female: Matched to 1st choice surgical specialty | Male: 1st choice = Surgery | Male: Matched to 1st choice surgical specialty |
|---|---|---|---|---|---|---|
| 2015 | 1574 | 1288 | 147 | 108 | 211 | 164 |
| 2014 | 1599 | 1248 | 161 | 120 | 208 | 153 |
| 2013 | 1537 | 1158 | 153 | 98 | 276 | 202 |
| 2012 | 1536 | 1136 | 161 | 112 | 244 | 194 |
| 2011 | 1447 | 1081 | 173 | 124 | 254 | 190 |
| 2010 | 1419 | 1019 | 186 | 126 | 240 | 188 |
| 2009 | 1317 | 996 | 141 | 104 | 232 | 183 |
| 2008 | 1216 | 918 | 141 | 103 | 240 | 183 |
| 2007 | 1173 | 827 | 151 | 105 | 232 | 166 |
| 2006 | 1136 | 800 | 117 | 90 | 208 | 164 |
| 2005 | 786 | 619 | 83 | 66 | 155 | 123 |
| 2004 | 644 | 641 | 78 | 58 | 174 | 113 |
| 2003 | 610 | 621 | 58 | 39 | 176 | 129 |
| 2002 | 506 | 611 | 49 | 33 | 184 | 125 |
| 2001 | 520 | 612 | 40 | 28 | 159 | 113 |
| 2000 | 526 | 628 | 49 | 28 | 168 | 116 |
| 1999 | 565 | 584 | 61 | 34 | 161 | 116 |
| 1998 | 532 | 640 | 56 | 41 | 187 | 115 |
Supplementary Table 2.
CaRMS data for applicants to urology by year
| Year | Total # of applicants | Quota of positions offered to CMGs | Females who ranked Urology as 1st choice program | Females who matched to Urology as 1st choice | Males who ranked Urology as 1st choice program | Males who matched to Urology as 1st choice |
|---|---|---|---|---|---|---|
| 2015 | 49 | 33 | 5 | 3 | 27 | 23 |
| 2014 | 53 | 31 | 22 | 14 | 21 | 17 |
| 2013 | 69 | 33 | 8 | 4 | 38 | 28 |
| 2012 | 48 | 33 | 7 | 7 | 28 | 22 |
| 2011 | 47 | 31 | 7 | 5 | 35 | 23 |
| 2010 | 64 | 30 | 16 | 8 | 34 | 22 |
| 2009 | 52 | 31 | 7 | 5 | 25 | 23 |
| 2008 | 54 | 30 | 9 | 7 | 30 | 22 |
| 2007 | 52 | 28 | 11 | 7 | 27 | 21 |
| 2006 | 47 | 26 | 8 | 6 | 27 | 20 |
| 2005 | 28 | 18 | 8 | 7 | 14 | 11 |
| 2004 | 27 | 17 | 3 | 1 | 24 | 16 |
| 2003 | 45 | 17 | 5 | 1 | 23 | 14 |
| 2002 | 42 | 15 | 4 | 3 | 26 | 12 |
| 2001 | 36 | 15 | 2 | 1 | 17 | 12 |
| 2000 | 40 | 15 | 3 | 2 | 17 | 13 |
| 1999 | 44 | 17 | 4 | 1 | 19 | 14 |
| 1998 | 44 | 18 | 5 | 3 | 19 | 14 |