Abstract
Prescription drug monitoring programs (PDMP) enable registered prescribers to obtain real-time information on patients’ prescription history of controlled medications. We sought to describe the impact of a state-mandated PDMP on opioid prescribing by Emergency Medicine providers. We retrospectively analyzed electronic medical records of 122,732 adult patients discharged with an opioid prescription from 15 Emergency Departments in a single health system in Pennsylvania from July 2015 to March, 2017. We used an interrupted time-series design to evaluate the percentage of patients discharged each month with an opioid prescription before and after state law mandated PDMP use on August 25th, 2016. From August (pre-PDMP) to September, 2016 (post-PDMP), the opioid prescribing rate decreased from 12.4% (95% CI 10.8% to 14.1%) to 10.2% (95% CI 8.8% to 11.8%). For each month between September, 2016 to March, 2017, there was a mean decline of 0.46% (95% CI −0.38% to −0.53%) in the percentage of patients discharged with an opioid prescription. There was heterogeneity in opioid prescribing across hospitals as well as by patient diagnosis.
Keywords: opioids, prescription, emergency
INTRODUCTION
In the United States, prescription opioid misuse is a major and urgent public health concern. Rates of prescription opioid deaths are climbing, with 22,598 deaths due to prescription opioid overdoses in 2015, more than deaths due to illicit opioids.13 Using the most recent available data, acute care visits involving the misuse of prescription opioids appear to be increasing20 and there is evidence that prescription opioid misuse often leads to downstream illicit opioid use, further amplifying risks.8 Given that many of these trends coincide with increases in prescribing of opioid analgesics7, health care providers have become a target for interventions aimed at reducing opioid prescribing12.
One way to assist providers in reducing inappropriate opioid prescribing is through access to real-time data on a patient’s past use of controlled medications. Currently, 49 states maintain Prescription Drug Monitoring Programs (PDMPs) with electronic databases containing records of controlled substances dispensed from pharmacies that can be accessed and queried by prescribers.9 The belief is that implementation of PDMPs will reduce opioid prescribing by providers to individuals at greater risk for opioid diversion and misuse and thus lower frequency of negative consequences such as opioid abuse and mortality associated with overdose.3 Studies examining the association between PDMP implementation and opioid prescribing do not indicate a consistent pattern of effects4,14,15,18 which is thought to be due to the variability in both legislated components and implementation strategies. For example, only 29 states currently mandate prescribers to check the PDMP for each patient to whom they are considering prescribing an opioid.
In this study, we sought to determine if implementation of state-mandated PDMP in a single health system through an email awareness campaign altered opioid prescribing among Emergency Medicine (EM) providers. EM is a medical specialty that has received significant attention related to opioid prescribing.2,5 Reasons include the high frequency of pain related EM care21 and the high proportion of patients who receive an opioid prescription by EM providers16. Our primary hypothesis was that the percentage of adult patients discharged by EM providers with an opioid prescription would decrease immediately after implementation of the mandatory PDMP. To explore any heterogeneity, we sought to identify any differences in the total number of opioid prescriptions by (1) site characteristics (EM training vs. non-training; major metropolitan vs. non-metro), (2) EM provider type (MD/DO vs. midlevel), and key patient characteristics (age, sex, pain severity, diagnosis categories). To understand how the PDMP affected higher count prescriptions, we examined the change in the percentage of opioid prescriptions for >12 tablets (equivalent to 3 days of treatment based on most common dosing schedules) over time.
METHODS
Study Design and Setting
We used interrupted time series analyses of retrospective electronic medical record data from 15 EDs in a single health system to compare monthly rates of opioid prescribing by EM providers before and after a state law mandated PDMP went live in Pennsylvania on August 25th, 2016. The state law required all prescribing providers to query the PDMP and to document their query “each time a patient is prescribed an opioid drug product or benzodiazepine.” Around one month prior to the “go-live” date, EM providers in our health system received an email from the health system which instructed them to register an account with the state PDMP by August 25, 2016. Around one week prior to the “go-live” date, EM providers were reminded through a follow-up email that they are mandated by state law to query the PDMP “each time a patient is prescribed an opioid drug product or benzodiazepine or if a prescriber believes or has reason to believe, using sound clinical judgment, that a patient may be abusing or diverting drugs”. When indicated, providers opened a web browser, navigated to the state PDMP web site (www.pennsylvania.pdmpaware.net/login), logged in with their credentials, and entered patient name and birth date into the search fields. The web site would then list all prescriptions for controlled substances filled at a pharmacy in Pennsylvania in the past 12 months.
In addition to describing the change in rates from before to after an intervention, interrupted time series designs identify any underlying trend and changes in trends post-intervention. We chose to examine pre-implementation rates of change up to greater than 1 year prior to PDMP to control for other cultural-temporal changes and examine at least 6 months post-implementation to understand durability of changes. This study was approved by the Institutional Review Board at The University of Pittsburgh with a waiver of individual consent of patients and providers.
Selection of Participants
We collected data from the electronic medical record of all patients age≥ 18 years discharged with an opioid prescription from the 15 Emergency Departments in the UPMC system from July 2015 to March 2017. During this study period, all opioid prescriptions in our health system were written and stored electronically. We included patients who may have been admitted for ED-based observation care and patients prescribed opioids by both physicians and advance practice non-physician-(i.e. midevel) providers. We collected the number of adults discharged each month from each site over the same time from the hospital registration system, which served as the denominator in our primary outcome measure.
Methods of Measurement
We extracted the following data from the electronic medical record: (a) patient age; (b) patient sex; (c) initial triage numeric pain scale (NPS) score (score ranges 0 to10); (d) discharge diagnosis codes (ICD-10; up to 3 per patient encounter); (e) site of patient encounter (i.e. hospital); (f) EM prescriber name and qualifications (MD, DO, NP, PA); and (g) date and time of encounter; (h) name of opioid, strength (i.e. 5 mg), and formulation (i.e. acetaminophen-oxycodone); and (i) opioid quantity dispensed. We categorized patient age into quartiles and NPS scores into tertiles and EM prescribers into MD/DO vs. physician assistant (PA)/nurse practitioner (NP). We categorized sites into EM training vs. non-EM training sites and into large central metropolitan vs. non-central metro/rural based on the 2013 NCHS Urban–Rural Classification Scheme for Counties.11 We created diagnosis categories of the most common pain-related diagnosis based on the National Hospital Ambulatory Care Survey (2014) 17 using ICD-10 codes as follows: (1) lower (S72; S82; S92) and upper extremity fractures (S42; S52; S62); (2) abdominal pain (R10); (3) low back sprain/strain (S33; S54.4; S54.5); (4) dental pain (K00-K08); (5) headache (G43; G89; R51); (6) renal colic (N20-N23).
Outcome Measures
The primary outcome of interest was the percentage of discharged adult patients prescribed an opioid by am EM provider. Our secondary outcome of interest was the percentage of opioid prescriptions for greater than 12 tabs. We also examined the number of opioid prescriptions written per month for exploratory aims.
Analysis
We used interrupted time series analyses (ITSA) with segmented linear regression models to compare epochs before and after PDMP was implemented. The primary analyses included 14 months pre-PDMP and 7 month post-PDMP. We included August, 2016 in the pre-PDMP period because the PDMP went live on August 25th, 2016. We tested one ITSA model separately for each outcome of interest. We assessed whether the introduction of the PDMP was associated with changes in (a) outcome level (intercept) and (b) trend of change over time (ordinary least squared regression slope). We adjusted for autocorrelation across time using the generalized Durbin-Watson test and included autocorrelation orders in our regression models. We also tested whether there were seasonality association by testing an interaction term of month.
Sensitivity analyses were conducted using varying pre-implementation periods (from 14 months to 7 months) and redefined secondary outcomes as total number of opioid prescriptions (as opposed to percentage of discharged patients) or percent of opioid prescribed for 28 tabs, following ACEP guidelines published in 2012 recommending opioids be prescribed for less than 7 days.6 We also conducted exploratory stratified interrupted time series analyses to investigate whether the PDMP may have had a differential impact on the number of opioid prescriptions written based on site characteristics (EM training vs. non-training; major central metropolitan vs. non-central metro/rural), provider type (MD/DO vs. NP/PA) and by key patient characteristics (age, sex, pain severity, diagnosis categories). We used Stata 14.0 (StataCorp, College Station, TX), including the itsa command for ITSA analyses.
RESULTS
Characteristics of Study Subjects
De-identified patient-level data from 122,825 encounters where an opioid was prescribed in the Emergency Department to an adult patient was provided by an honest broker. A clinician investigator further reviewed the data and excluded duplicate reports (n=93), resulting in a final cohort of 122,732 from 15 Emergency Departments over 21 months during the period of July 2015 to March 2017. Five EDs were training sites for an EM residency program. Eight sites were located in large central metropolitan areas, five were in non-central metro areas, and 2 were in rural areas.
Patient mean age was 44.6 (standard deviation [SD] 16.4) and 57.4% were female. Mean of NPS scores (available Sept 2015 to March 2017) was 7.9 (SD 2.1) and did not change over time. 5.6% of patients reported NPS score of 11 on a 10-point scale. For the selected pain-related diagnoses, 6.3% of all opioid prescriptions were for dental pain, 8.9% for abdominal pain, 7.3% for headaches, 4.6% for urolithiasis, 6.1% for low back pain, and 8.9% for extremity fractures.
A total of 1373 unique EM providers prescribed at least one opioid at some point from July, 2015, to March, 2017, with 416 providers prescribing an average of at least one opioid per month. Of all opioid prescriptions, 69.3% were written by a physician (MD/DO) and 30.7% were written by a non-physician advanced provider (NP/PA). Analyzed by site, 42.8% of all prescriptions came from EM training and 57.2% came from non-EM training locations. 58.8% of all opioid prescriptions were written at hospitals in large central metro areas, 34.6% from non-central metro areas and 6.6% from rural areas.
The most frequently prescribed opioids were acetaminophen-hydrocodone (43.3%), acetaminophen-oxycodone (24.8%), oxycodone (17.9%) and tramadol (12.0%). Acetaminophen-codeine and codeine were prescribed 2,057 times, which was 1.7% of total opioids. The most common dosages were acetaminophen 325mg-hydrocodone 5mg (42.4%), acetaminophen 325mg-oxycodone 5mg (26.6%), oxycodone 5mg (18.3%), together composing 98% of all opioids prescribed. Only 195 (0.16%) prescriptions were for extended release formulations. The most common number of tabs prescribed was 12 (51.1%), with 30.5% of opioid prescriptions written for more than 12 tabs.
Selected prescription, patient, provider and site characteristics from the 7 months prior to PDMP compared to the 7-months after PDMP introduction are shown in Table 1 and detailed opioid prescribing data by month for the entire period studied are presented in Appendix Table A.
Table 1.
Characteristics of opioid prescriptions, patients, providers and sites from the 7 months prior to PDMP compared to the 7-months after PDMP introduction
| Pre-PDMP Feb 2016–Aug 2016 |
Post-PDMP Sept 2016–Mar 2017 |
Absolute Change | Percent Change | |||
|---|---|---|---|---|---|---|
|
|
||||||
| Common Prescriptions | Opioid formulation | acetaminophen 325mg-hydrocodone 5mg | 15,845 | 10,625 | −5,220 | −32.94 |
| acetaminophen 325mg-oxycodone 5mg | 9,391 | 6,341 | −3,050 | −32.48 | ||
| oxycodone 5mg | 6,523 | 4,524 | −1,999 | −30.65 | ||
| tramadol 50mg | 5,140 | 3,884 | −1,256 | −24.44 | ||
| Patient | Age | Q1: 18–30y | 9,479 | 6,068 | −3,411 | −35.98 |
| Q2: 31–42y | 9,523 | 6,009 | −3,514 | −36.90 | ||
| Q3: 43–56y | 9,545 | 6,381 | −3,164 | −33.15 | ||
| Q4: 56–113y | 9,405 | 6,871 | −2,534 | −26.94 | ||
| Sex | Female | 21,736 | 14,395 | −7,341 | −33.77 | |
| Male | 16,214 | 10,932 | −5,282 | −32.58 | ||
| Pain | NPS T1: 1–7 | 12,758 | 8,454 | −4,304 | −33.74 | |
| NPS T2: 8–9 | 14,162 | 9,186 | −4,976 | −35.14 | ||
| NPS T3: 10 | 11,032 | 7,689 | −3,343 | −30.30 | ||
| Diagnosis Category | Dental pain | 3,302 | 2,102 | −1,200 | −36.34 | |
| Abdominal pain | 4,614 | 3,106 | −1,508 | −32.68 | ||
| Headache | 3,855 | 2,460 | −1,395 | −36.19 | ||
| Urolithiasis | 2,306 | 2,047 | −259 | −11.23 | ||
| Low back pain | 3,193 | 2,238 | −955 | −29.91 | ||
| Extremity fracture | 2,958 | 2,272 | −686 | −23.19 | ||
| Provider | Type | Midlevel (PA/NP) | 11,918 | 8,482 | −3,436 | −28.83 |
| MD/DO | 26,034 | 16,847 | −9,187 | −35.29 | ||
| Site | Training | EM residents | 16,228 | 10,223 | −6,005 | −37.00 |
| No EM residents | 21,724 | 15,106 | −6,618 | −30.46 | ||
| Location | Central metro | 25,337 | 16,751 | −8,586 | −33.89 | |
| Non-central metro | 15,056 | 10,361 | −4,695 | −31.18 | ||
| Rural | 2,699 | 2,101 | −598 | −22.16 | ||
Percentage of Discharged Adult ED Patients Receiving Any Opioid
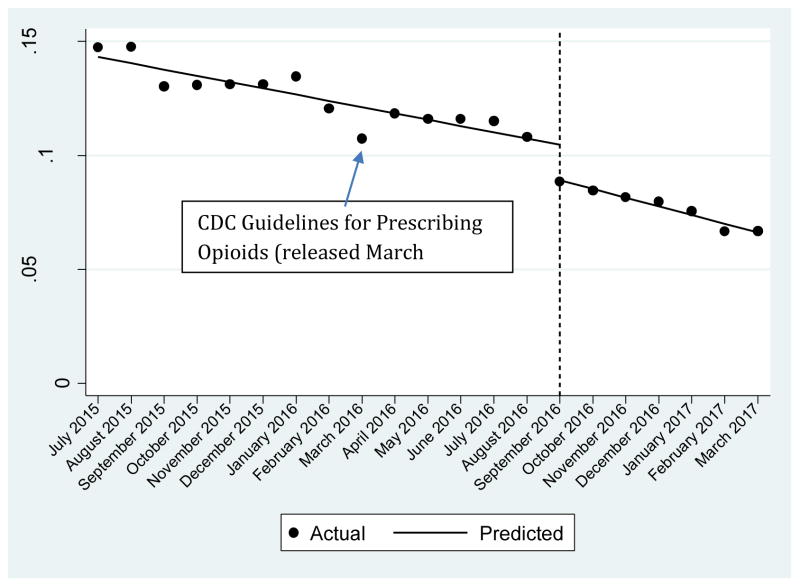
In July, 2015, 16.6% [95% Confidence Interval (CI) 16.3% to 17.0%] of discharged adult patients received an opioid prescription. For each month between July, 2015 and August, 2016, there was a mean decline of 0.29% (95% CI 0.22% to 0.37%) in the percentage of patients discharged with an opioid prescription. From August (pre-PDMP) to September, 2016 (post-PDMP), the opioid prescribing rate decreased from 12.4% (95% CI 10.8% to 14.1%) to 10.2% (95% CI 8.8% to 11.8%), equivalent to a relative reduction of 17.7%. For each month between September, 2016 to March, 2017, there was a mean decline of 0.46% (95% CI −0.38% to −0.53%) in the percentage of patients discharged with an opioid prescription. The results of the ITSA can be seen in Figure 1 and Table 2. Using total number of opioid prescriptions as the outcome, we found an immediate relative reduction of 19.5% from August (pre-PDMP) to September, 2016 (post-PDMP). Results were similar when we performed a sensitivity analysis by reducing the months pre-PDMP implementation and there were no seasonality effects.
Figure 1.
Predicted and Actual Proportion of Adults Discharged with an Opioid Prescription over Time Before and After PDMP
Table 2.
Interrupted Time-Series Analysis of Proportion of Adult ED Patients Discharged with an Opioid Prescription
| Full Segmented Regression Model | Coefficient | t-statistic | P-value | 95% Confidence Interval | |
|---|---|---|---|---|---|
|
|
|||||
| Intercept (β0) | 0.146 | 44.2 | <0.0001 | 0.139 | 0.153 |
| Baseline trend (β1) | −0.0028 | −8.02 | <0.0001 | −0.0035 | −0.002 |
| Level change after PDMP (β2) | −0.0156 | −5.41 | <0.0001 | −0.022 | −0.01 |
| Trend change after PDMP (β3) | −0.0011 | −2.36 | 0.03 | −0.002 | −0.0001 |
| Post-treatment linear trend | −0.004 | −12.8 | <0.0001 | −0.005 | −0.003 |
Percentage of Discharged Adult ED Patients Receiving >12 Tabs
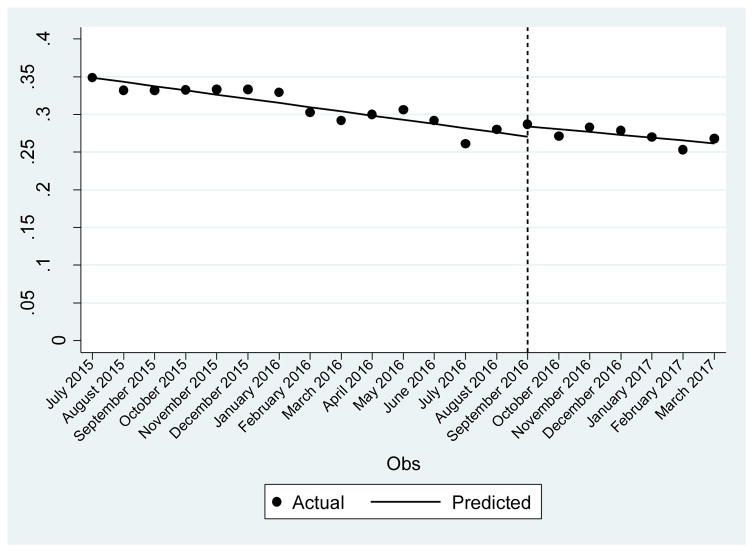
In July, 2015, 35.4% (95% CI 34.3% to 36.5%) of opioid prescriptions were written for >12 tabs. For each month between July, 2015 and August, 2016, there was a mean decline of 0.56% (95% CI −0.41 to −0.71) in the percentage of opioid prescriptions written for >12 tabs. There was no immediate reduction in the proportion of opioid prescriptions written for >12 tabs after mandatory PDMP implementation and no change in the trend (slope). These results can be seen in Figure 2 and Table 3. Results were similar when we performed a sensitivity analysis by increasing the threshold to 28 tabs.
Figure 2.
Predicted and Actual Proportion of Opioid Prescriptions for >12 tabs over Time Before and After PDMP
Table 3.
Interrupted Time-Series Analysis of Proportion of Opioid Prescriptions for >12 tabs
| Full Segmented Regression Model | Coefficient | t-statistic | P-value | 95% Confidence Interval | |
|---|---|---|---|---|---|
|
|
|||||
| Intercept (β0) | 0.354 | 70.6 | <0.0001 | 0.344 | 0.365 |
| Baseline trend (β1) | −0.006 | −7.8 | <0.0001 | −0.004 | −0.007 |
| Level change after PDMP (β2) | 0.135 | 1.58 | 0.13 | −0.004 | 0.032 |
| Trend change after PDMP (β3) | 0.002 | 1.09 | 0.29 | −0.002 | 0.005 |
| Post-treatment linear trend | −0.004 | −2.45 | 0.02 | −0.001 | −0.007 |
Exploring Heterogeneity in Number of Discharged ED Patients Receiving Any Opioid
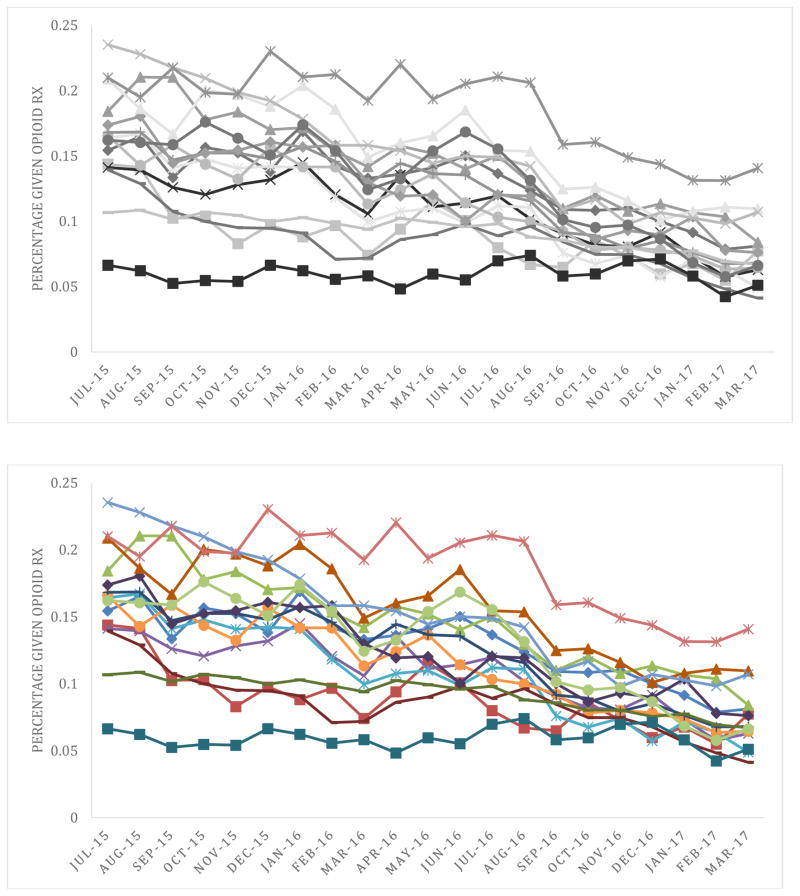
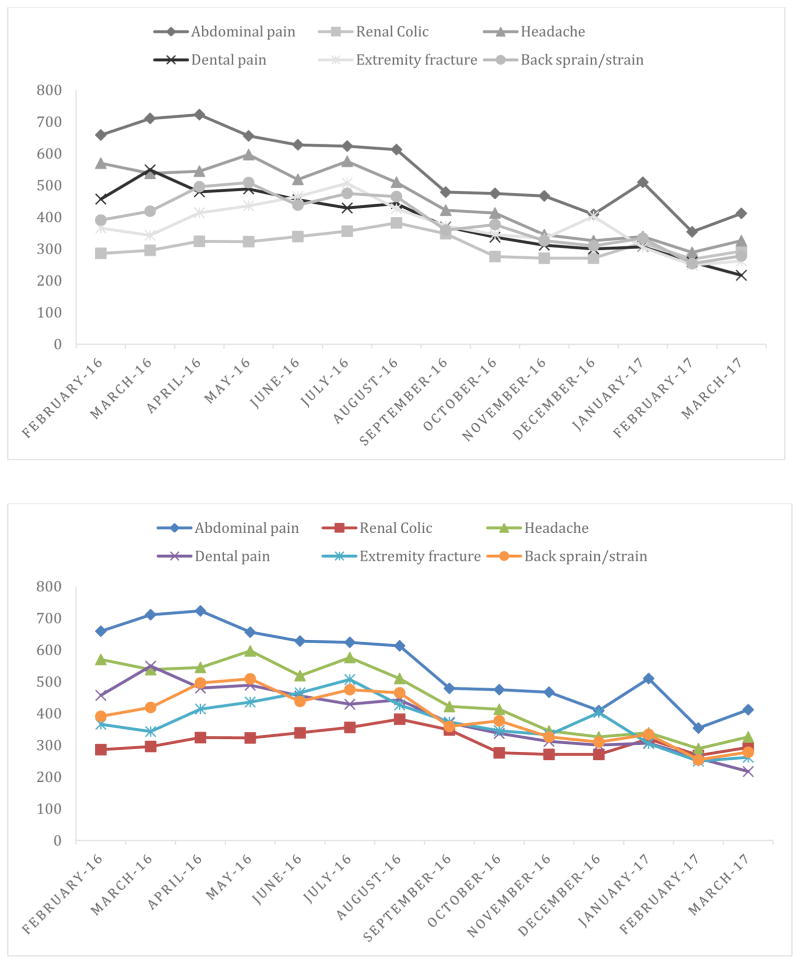
The heterogeneity in percentages of discharged patients prescribed an opioid across sites can be seen in Figure 3. For example, in August, 2016, there was a low of 6.7% at one site to a high of 21.1% at another site. In September, 2016 (post-PDMP), there was a low of 5.8% at one site to a high of 16.0% at another site. Greater reductions in opioid prescribing over time were observed in sites with higher pre-PDMP opioid prescribing. The only noticeable difference between EM training and non-training sites was in the slope of change after PDMP, such that EM training sites had a greater slope of decline in opioid prescribing than non-training sites. There were no differences in the immediate level or the slope of change between central metropolitan and non-central metro/rural hospitals, nor between provider types (MD/DO vs. NP/PA) or by key patient characteristics (age, sex, pain severity). There was heterogeneity in opioid prescribing between key diagnosis categories, with the least reductions in opioid prescribing over time among patients with renal colic and extremity fractures and the greatest reductions in opioid prescribing over time among patients with abdominal pain, as shown in Figure 4.
Figure 3.
Proportion of Adult ED Patients Discharged with an Opioid Prescription by Hospital
Figure 4.
Number of Opioid Prescriptions by Key Pain-Related Diagnoses
DISCUSSION
In this analysis of opioid prescribing across 15 Emergency Departments in a single health system in Pennsylvania, we found that there was an immediate relative reduction of 17.7% in the proportion of patients that were prescribed an opioid by EM providers from the month before to the month after PDMP implementation. As well, we found that there was an accelerated reduction in the proportion of discharged patients prescribed an opioid of around 0.5% every month after PDMP implementation, with only around 7.6% prescribed an opioid by March 2017. Although the intensity of association seemed to vary between sites, all except two sites (who were both low volume opioid prescribers prior to PDMP) showed immediate reductions in opioid prescribing. As well, we did not find that the type of opioid prescribed changed over time, suggesting that the PDMP did not result in providers substituting one opioid for another.
While the proportion of opioid prescriptions written by EM providers for >12 tabs decreased over time, which is likely due to the accumulating evidence and awareness about the risks of higher volume opioid prescriptions, we did not find evidence of specific association of the PDMP. The lack of accelerated reduction in the proportion of opioid prescriptions for >12 tabs after implementation of PDMP may be due to the minority of patients (27%) being discharged with an opioid prescription for >12 tabs in the month prior to PDMP implementation, allowing for much less potential impact. Another reason is that at-risk patients should not be provided any opioid, not a lower number of tabs.
Our findings complement prior research. Bao et al.1 used data from a national survey to assess the effects of PDMPs on opioid prescribing in the ambulatory care setting in 24 states from 2001 to 2010 and found that their implementation was associated with a 30% reduction in the rate of opioid prescribing. Our findings are also comparable with Weiner et al., 201722, who examined the effect of Ohio’s opioid prescribing guidelines, which were implemented in April 2012, on EM provider prescriptions. They found similar yet smaller immediate reductions in the number of opioids prescribed by EM providers (12% vs. 17.7%), which could be due to Ohio not mandating use of the PDMP, resulting in lower utilization by EM providers.14
The heterogeneity in opioid prescribing across hospitals suggests that even within a single health system, there are different practice patterns or “norms” which develop. Although some of these differences may be related to different frequency of pain-related diagnoses, they do not completely explain differences. The sites with higher pre-PDMP opioid prescribing showed greater reductions post-PDMP, suggesting that these are the sites to focus on when instituting opioid policies. Also, it suggests that a floor is reached, beyond which reductions in opioid prescribing are not likely possible. The finding that EM training sites decreased opioid prescribing at a greater rate than non EM-training sites post-PDMP suggests that involving EM residents in patient care increases the likelihood of PDMP being queried or altering prescribing decisions based on PDMP findings. It also fits with prior studies showing higher rates of quality metrics being met at teaching hospitals than non-teaching hospitals.19
We did not find differential associations of PDMP with opioid prescribing based on patient age, sex or pain level, indicating that the PDMP does not seem to identify specific patient sub-groups. We found that there was heterogeneity in the reduction of opioid prescriptions provided over time across different diagnoses, with the least reductions among patients with diagnoses that have objective evidence of pain insult, such as occurs with kidney stones and broken bones. This suggests that EM providers are not withholding opioid analgesics when it is likely warranted.
Several limitations should be noted. We do not know for sure that the implementation of the state mandated PDMP within a single health system was the singular reason for reduced opioid prescribing rates. Implementation coincided with other reasons for changes in prescribers’ behavior, notably the CDC Guidelines for Opioid Prescribing10, released around 5 months prior to PDMP implementation (shown in Figure 1). Also, we do not know for what percentage of patient encounters EM providers accessed the PDMP. In a follow-up survey completed by 42 EM providers sampled from 10 out of the 15 hospitals in our health system, 38 (90%) reported “accessing the PDMP always or most of the time when considering prescribing an opioid for pain”. We do not know whether the reductions in opioid prescribing would be seen within EM providers from other health systems in mandated states or within other providers within the same health system. Future studies could examine how EM providers, who do not have longitudinal relationships with patients, compare with other specialties (e.g. medicine) that do. Although we did find greater reductions in opioid prescribing at EM training hospitals than non-training hospitals, we cannot isolate the effect of resident participation on opioid prescribing. Finally, we did not seek to determine the appropriateness of opioid prescribing. There are lay reports of reduced access to opioid prescriptions resulting in illicit substance use and suffering, but no peer-reviewed literature to confirm this possibility. Future studies should study how often patients with high-risk PDMP activity (e.g. multiple prescribers) seek and use illicit analgesic substances when refused opioid prescriptions.
In conclusion, the implementation of state-mandated PDMP in a single health system was associated with additive and sustained decreases in opioid prescribing by EM providers in a large healthcare system. Finding support current PDMP mandates in reducing opioid prescriptions which could curb the prescription opioid epidemic and may ultimately reduce abuse, misuse, and overdose death.
Supplementary Material
HIGHLIGHTS.
A state-mandated PDMP reduced opioid prescribing among emergency medicine providers.
There was heterogeneity in opioid prescribing across hospitals as well as by patient diagnosis.
PDMP-associated reductions in opioid prescriptions could curb the prescription opioid epidemic.
Perspective.
This study examined the impact of a state-mandated PDMP on opioid prescribing among emergency medicine providers from 15 different hospitals in a single health system. Finding support current PDMP mandates in reducing opioid prescriptions which could curb the prescription opioid epidemic and may ultimately reduce abuse, misuse, and overdose death.
Footnotes
Conflict of Interest Disclosures: Authors have no conflicts of interest related to this study. Research funding was provided by an internal grant from the Department of Emergency Medicine at the University of Pittsburgh. B. Suffoletto is supported by a K23 from NIAAA (AA023284-01).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bao Y, Pan Y, Taylor A, Radakrishnan S, Luo F, Pincus HA, Schackman BR. Prescription Drug Monitoring Programs Are Associated With Sustained Reductions In Opioid Prescribing By Physicians. Health Aff (Millwood) 2016;1(35):1045–51. doi: 10.1377/hlthaff.2015.1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barnett ML, Olenksi AR, Jena AB. Opioid Prescribing by Emergency Physicians and Risk of Long-Term Use. N Engl J Med. 2017;376:1896. doi: 10.1056/NEJMc1703338. [DOI] [PubMed] [Google Scholar]
- 3.Bohnert AS, Valenstein M, Bair MJ, Ganoczy D, McCarthy JF, Ilgen MA, Blow FC. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305:1315–21. doi: 10.1001/jama.2011.370. [DOI] [PubMed] [Google Scholar]
- 4.Brady JE, Wunsch H, DiMaggio C, Lang BH, Giglio J, Li G. Prescription drug monitoring and dispensing of prescription opioids. Public Health Rep. 2014;129:139–47. doi: 10.1177/003335491412900207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Butler MM, Ancona RM, Beauchamp GA, Yamin CK, Winstanley EL, Hart KW, Ruffner AH, Ryan SW, Ryan RJ, Lindsell CJ, Lyons MS. Emergency Department Prescription Opioids as an Initial Exposure Preceding Addiction. Ann Emerg Med. 2016;68:202–8. doi: 10.1016/j.annemergmed.2015.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cantrill SV, Brown MD, Carlisle RJ, Delaney KA, Hays DP, Nelson LS, O’Connor RE, Papa A, Sporer KA, Todd KH, Whitson RR American College of Emergency Physicians Opioid Guideline Writing Panel. Clinical policy: critical issues in the prescribing of opioids for adult patients in the emergency department. Ann Emerg Med. 2012;60:499–525. doi: 10.1016/j.annemergmed.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 7.Compton WM, Boyle M, Wargo E. Prescription opioid abuse: Problems and responses. Prev Med. 2015;80:5–9. doi: 10.1016/j.ypmed.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 8.Compton WM, Jones CM, Baldwin GT. Relationship between Nonmedical Prescription-Opioid Use and Heroin Use. N Engl J Med. 2016;374:154–63. doi: 10.1056/NEJMra1508490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Department of Health and Human Services, & Assistant Secretary for Planning and Evaluation. Opioid abuse in the U.S. and HHS actions to address opioid-drug related overdoses and death. 2017 doi: 10.3109/15360288.2015.1037530. https://aspe.hhs.gov/basic-report/opioid-abuse-us-and-hhs-actions-address-opioid-drug-related-overdoses-and-deaths. [DOI] [PubMed]
- 10.Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016. MMWR Recomm Rep. 2016;65(RR-1):1–49. doi: 10.15585/mmwr.rr6501e1. http://dx.doi.org/10.15585/mmwr.rr6501e1. [DOI] [PubMed] [Google Scholar]
- 11.Ingram DD, Franco SJ. 2013 NCHS urban–rural classification scheme for counties. National Center for Health Statistics. Vital Health Stat. 2014;2(166) [PubMed] [Google Scholar]
- 12.Jones CM, Lurie P, Woodcock J. Addressing prescription opioid overdose: data support a comprehensive policy approach. JAMA. 2014;312:1733–4. doi: 10.1001/jama.2014.13480. [DOI] [PubMed] [Google Scholar]
- 13.National Center for Health Statistics. Multiple Cause of Death 1999–2015 on CDC WONDER Online Database. Atlanta, GA: Centers for Disease Control and Prevention; 2017. [Google Scholar]
- 14.Patrick SW, Fry CE, Jones TF, Buntin MB. Implementation Of Prescription Drug Monitoring Programs Associated With Reductions In Opioid-Related Death Rates. Health Aff (Millwood) 2016;35:1324–32. doi: 10.1377/hlthaff.2015.1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paulozzi LJ, Kilbourne EM, Desai HA. Prescription drug monitoring programs and death rates from drug overdose. Pain Med. 2011;12:747–54. doi: 10.1111/j.1526-4637.2011.01062.x. [DOI] [PubMed] [Google Scholar]
- 16.Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in Opioid Prescribing by Race/Ethnicity for Patients Seeking Care in US Emergency Departments. JAMA. 2008;299:70–8. doi: 10.1001/jama.2007.64. [DOI] [PubMed] [Google Scholar]
- 17.Rui P, Kang K. National Hospital Ambulatory Medical Care Survey: 2014 Emergency Department Summary Tables. Available from: http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2014_ed_web_tables.pdf.
- 18.Rutkow L, Chang HY, Daubresse M, Webster DW, Stuart EA, Alexander GC. Effect of Florida’s Prescription Drug Monitoring Program and Pill Mill Laws on Opioid Prescribing and Use. JAMA Intern Med. 2015;175:1642–9. doi: 10.1001/jamainternmed.2015.3931. [DOI] [PubMed] [Google Scholar]
- 19.Shahian DM, Nordberg P, Meyer GS, Blanchfield BB, Mort EA, Torchiana DF, Normand SL. Contemporary performance of U.S. teaching and nonteaching hospitals. Acad Med. 2012;87:701–8. doi: 10.1097/ACM.0b013e318253676a. [DOI] [PubMed] [Google Scholar]
- 20.The DAWN report: highlights of the 2011 Drug Abuse Warning Network (DAWN) findings on drug-related emergency department visits. Rockville, MD: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality; 2013. [PubMed] [Google Scholar]
- 21.Todd KH, Ducharme J, Choiniere M, Crandall CS, Fosnocht DE, Homel P, Tanabe P PEMI Study Group. Pain in the Emergency Department: Results of the Pain and Emergency Medicine Initiative (PEMI) Multicenter Study. J Pain. 2007 Jun;8:460–6. doi: 10.1016/j.jpain.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 22.Weiner SG, Baker O, Poon SJ, Rodgers AF, Garner C, Nelson LS, Schuur JD. The Effect of Opioid Prescribing Guidelines on Prescriptions by Emergency Physicians in Ohio. Ann Emerg Med. 2017 doi: 10.1016/j.annemergmed.2017.03.057. pii: S0196-0644(17)30353-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.