Abstract
Background
There is a concerted effort underway to evaluate and reform our nation’s approach to the health of people with ongoing or elevated needs for care, particularly persons with chronic conditions and/or disabilities.
Objective
This literature review characterizes the current state of knowledge on the measurement of chronic disease and disability in population-based health services research on working age adults (age 18–64).
Methods
Scoping review methods were used to scan the health services research literature published since the year 2000, including medline, psycINFO and manual searches. The guiding question was: “How are chronic conditions and disability defined and measured in studies of healthcare access, quality, utilization or cost?”
Results
Fifty-five studies met the stated inclusion criteria. Chronic conditions were variously defined by brief lists of conditions, broader criteria-based lists, two or more (multiple) chronic conditions, or other constructs. Disability was generally assessed through ADLs/IADLs, functional limitations, activity limitations or program eligibility. A smaller subset of studies used information from both domains to identify a study population or to stratify it by subgroup.
Conclusions
There remains a divide in this literature between studies that rely upon diagnostically-oriented measures and studies that instead rely on functional, activity or other constructs of disability to identify the population of interest. This leads to wide ranging differences in population prevalence and outcome estimates. However, there is also a growing effort to develop methods that account for the overlap between chronic disease and disability and to “segment” this heterogeneous population into policy or practice relevant subgroups.
Keywords: people with disabilities, chronic conditions, health service utilization, measurement
INTRODUCTION
It is well known that health service utilization is not uniform across the U.S. adult population. Certain individuals, such as those who experience exceptionally high rates of emergency department visits and/or hospitalizations, have been identified as “super-utilizers”.1–6 Growing concern over the health and associated health care costs of this population has sparked a number of initiatives at private4, 5, 7, 8 and federal9, 10 organizational levels to better characterize the population of working age adults with chronic conditions and disabilities and to better understand their healthcare needs. The ultimate goals of these efforts are to improve population health and to enhance the capacity and performance of the current health care system in order to better meet those needs while controlling costs.4, 7, 8, 11
Though defined and labeled in a variety of ways, this High-Need, High-Cost (HNHC) population is large and diverse, including those with chronic conditions, disabilities, or both, who may also experience social circumstances that compound the effects of their health conditions such as lack of stable housing or transportation, food insecurity, low income, limited access to care, and/or diminished social supports.5, 7, 8, 11–13 However, identification and categorization of this population has proved challenging. Although claims data and electronic health records have been used to predict high future utilization, the resultant models have not yet produced a coherent clinical picture of the type of patient who is consistently at risk. Such methods sometimes omit individuals who need, but do not receive, all necessary healthcare, or whose healthcare needs cannot be captured across different settings or data collection systems.5,13 While adults with Multiple Chronic Conditions (MCC) are known to be high healthcare users in the aggregate, the heterogeneity of their conditions, their health-related risks (and assets) and their service utilization patterns makes it difficult to develop and target specific interventions to meet their needs. In an issue brief on improving healthcare for high-need patients, the Peterson Center on Healthcare noted that “Absent a uniform research definition of high-need patients, it is difficult to generalize across studies how the system performs in its care for this population.”14 Thus, there is a pressing need for a straightforward means of prospectively identifying individuals with ongoing and elevated health care needs.15
Beginning in 2012, the Rehabilitation Medicine Department at the National Institutes of Health Clinical Center convened an expert measurement panel to develop a definition and brief survey instrument to bridge this gap.10 To inform our panel’s development of the instrument, we performed a scoping literature review to characterize the state-of-the-art in measurement of chronic conditions, disability, and their intersection among working age adults. We focused our search on the working age adult population (aged at least 18 but less than 65) for several reasons: 1) A greater number of working age adults have disabilities because the working age population is so large,16 representing an important subgroup of the high healthcare need population. 2) The diversity of healthcare use and need across the entire population presents measurement challenges, and 3) Long-term care needs and services have been more thoroughly studied among children and elders.
The purpose of this review was to provide a wide-angled lens on the current state of measurement of chronic conditions and disabilities in health services research. Our goal in performing this review was to support the development of methods for identification of working age adults with elevated and sustained health care needs, including a broad range of medical and non-medical, community-based services and supports. The results suggest that the existing literature is siloed in several important ways; greater attention to the points of intersection between chronic conditions, comorbidities, functional limitations and actitivites of daily living is needed in order to properly define and categorize the working age population with ongoing and elevated needs for care.
METHODS
We employed scoping literature review methods in this study.17 Scoping reviews are most appropriate for broad research questions that seek to map and categorize the main domains and types of knowledge available in a given topical area. We followed the tenets of proper scoping review closely, which include: 1) replicability; 2) explicit inclusion and exclusion criteria; 3) breadth of search strategies; 4) standardized approach to content extraction; 5) iterative analysis and charting of major themes; and 6) consultation with stakeholders.17 We provide a process map in figure 1 and further explanation of our methods below.
Figure 1.
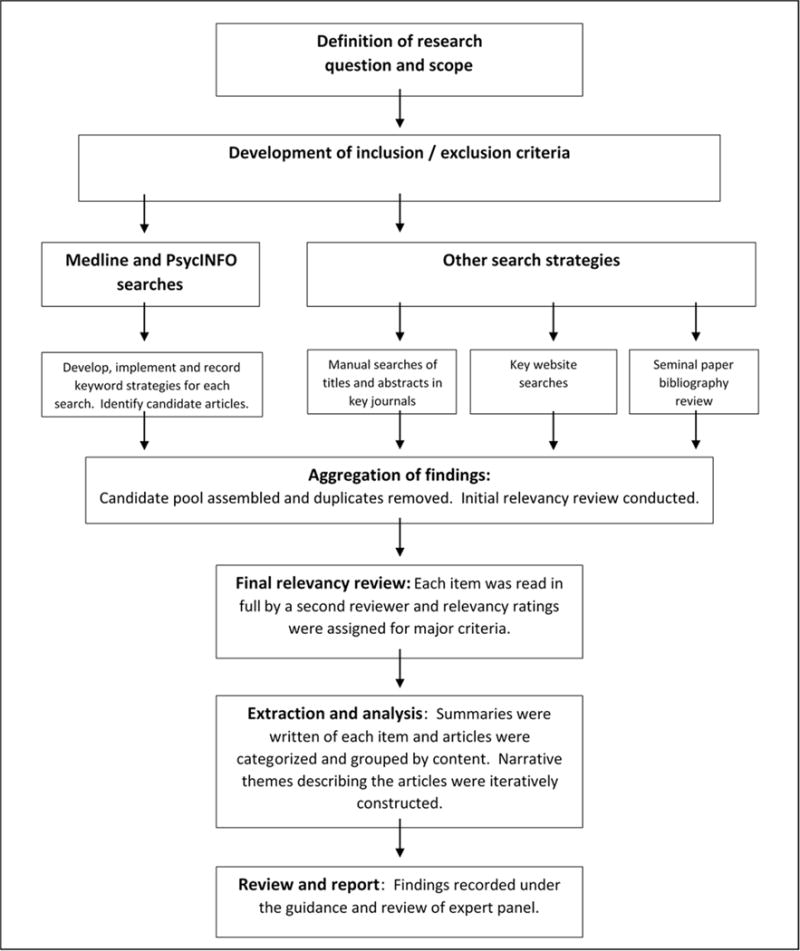
Scoping review process map
Definition of research question, scope and selection criteria
The expert panel members developed the primary guiding question for this literature review through a process that included a questionnaire and dedicated teleconferences. Example articles were drawn from the literature, selection criteria were developed, and a variety of test keyword searches were conducted and evaluated. The final research question for this literature review was stated as follows:
“How are chronic conditions and disability defined and measured in studies of healthcare access, quality, utilization or cost?”
The final inclusion and exclusion criteria for this question were:
Published in English after January 1, 2000
Include articles pertaining to broad categories of conditions or functional limitations (possible examples: psychiatric disorders; developmental disabilities; mobility impairments; neuromuscular disorders; cardiopulmonary disorders; renal diseases)
Exclude studies where the findings or conclusions are primarily applicable to persons with one highly specific disease or condition (for example, exclude: Primary care use among persons with allergic rhinitis; Quality of care among persons with arthritic knee impairment, but include: Primary care use among persons with one or more chronic conditions; Quality of care among persons with limited mobility)
- Include articles that are related to definition, operationalization or measurement of chronic conditions, disabilities or both.
- “Measurement” includes issues concerning psychometrics, self-report, reliability / validity, proxy effects, etc.
- Include articles written at a population level (exclude case studies or micro-level articles)
Include articles with a health services research focus (such as access to care, quality, utilization or cost)
Include articles on children or elders only if the findings or discussion also appear directly relevant to working age adults
Include international articles if published in English, strongly related to the question and clearly meeting all the above inclusion criteria.
Medline and PsycINFO searches
Articles were initially judged to be candidates for the review based on brief examination of the title and abstract in light of the inclusion / exclusion criteria. When an article was judged to be a candidate, it was added to the study library for further review (together with the search date, the keyword combination used to locate it, and the database source).
Other search strategies
In addition to the Medline and PsycINFO searches, we examined 1) key journals, 2) relevant websites and 3) seminal articles, each as recommended by the expert panel. For each key journal, we examined every published title and relevant abstract from the year 2000 on in order to identify candidate articles. Regarding the key website / gray literature search, there were quite a number of reports, conference proceedings, white papers, monographs, etc. that potentially pertained to our research but which did not appear in the peer-reviewed literature. Some of these were from government sources, others from privately funded foundations or agencies, and still others from academic centers. The majority of these sources had a web presence, though the organization and search capabilities of their websites varied considerably. As a result, there was no single search strategy that could be applied, but in all cases, we sought health services research (access, utilization, quality or cost) on population groups with chronic conditions and/or disabilities. Additionally, when the websites in question provided search capabilities, we used keywords shown to be effective in our Medline and PsycINFO searches. Finally, the expert panel members directly contributed articles they believed to be seminal to the measurement of chronic conditions and disability in health services research. We examined each list of references at the end of these articles. The titles and abstracts of these citations were reviewed and when they appeared to satisfy the inclusion and exclusion criteria, they were identified as candidate articles.
Aggregation of candidate pools, final relevancy review and summarization
There was overlap in the articles identified by these five different search strategies and so we consolidated the article candidate pools to remove duplicates. We then assigned members of our expert panel and staff to read the candidate articles in full, while insuring that each article was assigned to an individual other than the person who initially identified it as a candidate. Each reviewer a) provided a decision for relevancy (accept / reject); b) wrote a brief summary of the article and c) provided relevance ratings on a series of Likert scales. The abstracts, summaries and relevancy ratings were used to identify the categorical themes and key points recorded in our results.
RESULTS
In all, 55 publications met the inclusion / exclusion criteria. Of these, 25 were quantitatively oriented studies in which large datasets were analyzed to estimate access to care, service use, quality of care or costs for persons with chronic health conditions, disabilities, or both. Another 14 publications directly addressed measurement issues in health survey or administrative contexts; the majority of these also included quantitative assessments of existing measures or data on persons with chronic conditions and/or disabilities. The remaining 16 publications were more methodologically oriented, including literature reviews, policy or practice guidelines or other scientific appraisals that were related to health services research and measurement in these populations.
In review of these 55 studies, the majority addressed either disability or chronic conditions, with fewer focusing upon the intersection of these domains. More generally, there appeared to be a divide in the literature between studies based upon diagnostic categorization (typically by condition listings) and disability assessment (typically by functional limitations, Activities of Daily Living (ADLs) or Instrumental Activities of Daily Living (IADLs) such as bathing, dressing or preparing meals, and/or activity participation such as work or school). In table 1, we provide an overview of the studies in this review by domain, conceptual approach, outcome measures and subpopulation; Additional details, including methods, sample sizes and narrative summaries are available in an online appendix.
Table 1.
Overview of studies by domain, conceptual approach, outcome measures and population group
| Study Domain | Conceptual approach | References | Outcome measure(s) or focus of study | Population or subpopulation |
|---|---|---|---|---|
| Chronic Conditions | Closed condition list | Schneider, O’Donnell & Dean (2009)19 | Utilization, costs | Medicare enrollees |
| Elrod & DeJong (2008)22 | Utilization and unmet need for treatment | Needing rehabilitation services | ||
| Balogh, Ouellette-Kuntz, Brownell &, Colantonio (2011)27 | Conditions associated with hospitalization | Intellectual disability | ||
| Schmittdiel et al (2008)28 | Self-management behaviors, health care ratings, quality of life | Appropriate conditions for Chronic Care Model | ||
| One or more conditions (criteria based) | Anderson & Horvath (2004)24 | Utilization, costs | Any chronic condition(s) | |
| Hwang, Weller, Ireys & Anderson (2001)25 | Out of pocket costs | Any chronic condition(s) | ||
| Kessler et al (2001)47 | Utilization and unmet need for treatment | Serious mental illness | ||
| Multiple chronic conditions | Parekh, Goodman, Gordon & Koh (2011)31 | Health, utilization, quality of life, care coordination & treatment system design | Two or more chronic conditions | |
| Kessler, Merikangas & Wang (2007)32 | Prevalence, utilization and comorbidity | Persons with mood disorders | ||
| Druss et al (2009)33 | Prevalence, utilization and comorbidity | Persons with mood disorders and chronic medical disorders | ||
| Methodological appraisal or review of other studies | Institute of Medicine (2012)26 | Macro-level conceptualization of chronic conditions and their treatment in the U.S. health care system | Any chronic condition(s) | |
| Diederichs & Bartels (2010)29 | Systematic review of multi-morbidity indices | Two or more chronic conditions | ||
| Valderas, Starfield, Sibbald, Salisbury & Roland (2009)35 | Conceptual relationships between comorbid conditions | Two or more chronic conditions | ||
| Disability | ADLs/IADLs | Federman et al (2009)44 | Longitudinal development of ADL / IADL limitations and utilization | Medicare enrollees |
| Olin & Dougherty (2006)45 | Expenditures and payment sources | Limitations including ADL/IADLs | ||
| Stineman et al (2011)46 | Health status, conditions and utilization of home modifications | ADL limitations | ||
| Kaye, Harrington & Laplante (2010)69 | Long term care utilization and unmet need, sources of care and payment | ADL/IADL limitations | ||
| Functional limitations | Dejong et al (2002)16 | Service utilization and unmet needs, sources of payment, costs | Functional and activity limitations | |
| Altman & Bernstein (2008)48 | Demographics, health status, healthcare access and use | Basic action difficulties and complex activity limitations | ||
| Rasch, Hochberg, Magder, Magaziner & Altman (2008)49 | Demographics, prevalent health conditions, access to care | Mobility limitations | ||
| Reichard, Stolzle & Fox (2011)50 | Health status, conditions, access and costs | Cognitive and/or physical limitations | ||
| Owens, Kerker, Zigler & Horowitz (2006)75 | Prevalence and treatment of vision and dental problems | Intellectual disability | ||
| Participation and activity limitations | Palsbo et al (2010)42 | Healthcare quality | Activity limitations | |
| Palsbo, Hurtado, Levine, Barrett & Mastal (2011)43 | Healthcare quality | Activity limitations | ||
| O’Day, Killeen, Sutton, Iezzoni (2005)74 | Access to primary care | Self-identified psychiatric disabilities | ||
| Iezzoni (2011)68 | Disparities in health and access to healthcare | Participation limitations | ||
| Gulley & Altman (2008)52 | Access, utilization, and satisfaction with care | Activity limitations | ||
| Program eligibility/participation | Chan et al (2008)53 | Utilization | Medicare enrollees | |
| Livermore, Stapleton & O’Toole (2011)71 | Costs | Federal and state disability program participants | ||
| Medical complexity / time | Arnow et al (2009)34 | Costs | Depression and/or chronic pain | |
| McColl & Shortt (2006)55 | Utilization | Chronic illness restricting activity | ||
| Stineman, Ross, Willams, Goin & Grander (2000)56 | Utilization | Functionally complex conditions | ||
| Fried, Ferrucci, Darer, Williamson & Anderson (2004)57 | Utilization and costs | Disability, frailty or comorbidity | ||
| Gulley, Rasch & Chan (2011)15 | Access to care and utilization rates | Complex combinations of chronic conditions and disability | ||
| Methodological appraisal or review of other studies | Fekete et al (2011)36 | Using the ICF for measurement selection | Spinal cord injury | |
| Altman & Gulley (2009)37 | Prevalence and demographics | People assessed as having disability by differing survey measures | ||
| Becker (2006)38 | Health measurement | People with disabilities | ||
| Madans, Loeb & Altman (2011)39 | Development of disability survey measures | People at risk of unequal participation due to disability | ||
| Livermore, Whalen, Stapleton (2011)40 | National disability surveys and data | People with disabilities | ||
| Iezzoni (2010)41 | Quality of care measurement | People with disabilities | ||
| National Council on Disability (2009)51 | Healthcare needs, access, utilization, cost and disparities | People with disabilities | ||
| Harniss, Amtmann, Cook, Johnson (2007)67 | Participation in health and healthcare survey research | People with disabilities | ||
| Krahn, Fox, Campbell, Ramon, Jesien (2010)70 | Improving surveillance systems | People with intellectual disabilities | ||
| McDermott & Turk (2011)72 | Improving disability measures | People with disabilities | ||
| Chronic Conditions and Disability | Combined analysis of chronic conditions and disability | Gulley, Rasch & Chan (2011)3 | Prevalence, demographics, health status, insurance coverage, utilization | Adults with chronic healthcare needs |
| Egede (2007)18 | Prevalence, correlates, utilization, lost productivity | Depression and chronic medical disorders | ||
| Alecxih, Shen, Chan, Taylor, Drabek (2010)20 | Utilization and costs | Chronic conditions and functional limitations | ||
| Anderson (2010)21 | Prevalence, demographics, insurance coverage, access to care & utilization | Chronic conditions, functional limitations and activity limitations | ||
| Gulley, Rasch & Chan (2011)23 | Prevalence, insurance status & source, access, utilization, costs | Adults with chronic healthcare needs | ||
| Callahan & Cooper (2006)65 | Insurance status, access to care | Disabling chronic conditions | ||
| Elhai (2007)66 | Utilization | Psychiatric diagnoses and disability | ||
| Agency for Healthcare Research and Quality (2012)73 | Health, disparities and healthcare access & quality | Select chronic conditions, limitations in basic activities and/or limitations in complex activities | ||
| Methodological appraisal or review of other studies | Iezzoni (2010)58 | Definitions, data and coding schemes for Comparative Effectiveness Research | People with disabilities and chronic conditions | |
| Bethell & Read (2002)60 | Definition, identification and measurement of special healthcare needs | Adults with special healthcare needs | ||
| Wolff, Boult, Boyd & Anderson (2005)59 | Onset of functional dependency | Chronic conditions, ADL limitations and/or long term care facility residency |
As further described below, among studies of persons with chronic conditions, the primary themes hinged upon how population groups were identified, whether on the basis of closed lists of conditions, criteria driven condition lists, or multimorbidity. Among studies concerning persons with disabilities, the themes included classification of disability such as through the ICF, comparative studies of disability surveys and measures, common areas of disability measurement (such as functional limitations, activity limitations or ADLs/IADLs), medical complexity / frailty, and/or the importance of time in disability measurement. A final, smaller cluster of studies examined health care access, utilization or cost on the basis of both chronic condition and disability measures.
I. People with chronic conditions
Chronic conditions and the people experiencing them have been defined and studied in many different ways in health services research. Perhaps the most common method is the selection of a population group on the basis of a single shared diagnosis, such as diabetes or depression. This approach creates “populations” on the basis of a single diagnosis (e.g. “diabetes patients”) even though the majority of persons with chronic conditions actually have more than one at a time. Such studies were formally excluded by our criteria, but they were frequently mentioned (and sometimes criticized) in the methodological literature we gathered. The approaches we directly documented, as shown in table 1, included closed lists of high prevalence or high ‘burden’ conditions, open lists (e.g. one or more of many possible conditions meeting a given set of criteria) and multiple chronic conditions (e.g. co-morbidity, multi-morbidity or secondary conditions, each of which implying at least two conditions most often defined as chronic). In nearly all of the studies we gathered that included chronic conditions, the diagnoses selected were believed to lead to higher rates of morbidity or mortality,18, 19 higher need for or use of health care or related services,20–21 difficulties paying for or accessing those services,22–23 or higher costs.24–25 Three main categories of definitions are reviewed below.
The closed list
At the population level, researchers must find some means by which to select a subset of the many hundreds of conditions that modern medicine cannot cure, or which otherwise are expected to persist for a lengthy period of time. The Institute of Medicine (IOM) notes that this is a process involving multiple tradeoffs between such constructs as time course, chronicity, downstream consequences, variation in etiology and pathogenesis, late stage manifestations, symptom patterns, management burden, social or economic consequences, and many others.26
When selecting a closed list of priority chronic conditions, the contents of that list will thus depend upon how researchers resolve these tradeoffs in light of the specific aims of their studies. For example, an expert panel convened by Balogh et al (2011)27 developed a list of Ambulatory Care Sensitive (ACS) chronic conditions that they recommend for inclusion in studies of persons with intellectual disabilities. The final list included 15 conditions (such as asthma, congestive heart failure, gastrointestinal ulcer, hypertension, dental conditions and epilepsy). In another example, Schmittdiel 200828 sought to validate the Patient Assessment of Chronic Illness Care (PACIC) survey instrument as a measure of the chronic care model (CCM). Consequently, a random sample of persons was drawn from patient registries with five possible conditions for which the chronic care model is itself particularly appropriate. These included diabetes, chronic pain, heart failure, coronary artery disease, or asthma. Thus, the selection of conditions depends not only on the tradeoffs outlined by the IOM, but on the primary purposes and populations of concern in each particular study as well. The result is many possible closed lists for many possible purposes. This may lead to inconsistent population definitions, and thus findings, in the related literature.29
One or more chronic conditions (criteria based)
Another approach to defining or identifying people with chronic conditions is to use a large (essentially open) list of health and mental health conditions that are each clinically expected to conform to specific time and health consequence criteria. The clearest example of this approach is a definition and condition list available from the Agency for Healthcare Quality and Research (AHRQ) Health Care Utilization Project (HCUP).30 A condition is defined as chronic by this definition if it lasts or is expected to last 12 months or longer and is known to either place limitations on self-care, independent living or social interactions or require ongoing intervention with medical products, services, or special equipment. AHRQ annually updates a list of hundreds of International Classification of Disease Clinical Modification (ICD-CM) condition codes that, from the medical point of view, are believed to meet these criteria. A growing body of research on persons with chronic conditions has been amassed using versions of this list. This research provides estimates of the prevalence of people with chronic conditions in the US, the number and type of chronic (and acute) health conditions they have, their health care utilization, access to care and costs.3,20,21,23–25
Two or more chronic conditions
There is an increasing emphasis being placed upon what is variously referred to as Multiple Chronic Conditions (MCC), multimorbidity, comorbidity or secondary conditions in this literature. Numerous studies have quantified the extent to which people with one chronic condition are actually prone to having additional chronic conditions.31 A particular focus can be found on the impact and costs of comorbid conditions within the domain of mental health32 as well as across both mental and physical health domains 33–34. However, the relatively “flat” distribution of these conditions across the population (e.g. low prevalence rates for most given two-disease combinations), results in significant challenges when choosing which disease pairs or approaches should be prioritized for study.29
Numerous comorbidity indices and classification algorithms have also been created. One of the most frequently applied is the Charlson Index. This is a prognostic instrument for chronic conditions that in combination might alter the risk of death. More complex indices, such as the “Index of Coexisting Disease”, measure the severity of 14 chronic diseases and the resulting functional limitations in two separate steps.29
Strong evidence now suggests that the coexistence of multiple chronic conditions increases mortality risk and is related to impairments in physical and mental functioning.21,33 Further, MCCs are associated with longer hospital stays, postoperative complications, and a higher overall health care utilization.3,29 However, in a systematic review, Diederichs et al (2010)29 conclude that, in contrast to this rather advanced research on the effects—and to a lesser extent on risk factors—of multimorbidity, only few studies have explicitly concentrated on methodological questions, such as defining actual criteria for the selection of diseases. Valderas et al (2009)35 provide a further exploration of the definitions and criteria that are common (and different) among various approaches to measuring multiple chronic conditions.
One key federal initiative on people with MCC warrants direct mention. In order to identify options for improving the health of this heterogeneous population, Health and Human Services (HHS) convened a departmental workgroup on individuals with MCC. The workgroup published a strategic framework on MCC in 201131 that included four overarching goals: 1) Foster health-care and public health system changes to improve the health of people with MCC; 2) Maximize the use of proven self-care management and other services by individuals with MCC; 3) Provide better tools and information to health-care, public health, and social services workers and 4) Facilitate research to fill knowledge gaps about, and interventions and systems to benefit, individuals with MCC. All of these goals were provided with objectives and strategies to effect change, though the proper definition and measurement of “multiple chronic conditions” was little addressed.
The most commonly applied definitions and measures used in recent health services research on people with chronic conditions therefore fall into 4 main categories: A) studies of individuals with a specific diagnosis (typically a high prevalence condition of concern because of related service needs, access problems, or high cost); B) studies of individuals with at least one of a brief list of conditions known to be chronic and appropriate to the interests or focus of the researchers; C) studies that employ criteria-based lists which, at minimum, specify an expected time frame for the chosen conditions, as well as some additional inclusion criteria pertaining to functional, health, or health care consequences and D) studies which explicitly focus upon individuals with two or more simultaneous chronic conditions. This last approach includes several subtypes, such as those which focus explicity on secondary conditions, comorbidities or multimorbidity.
III. People with disabilities
Researchers interested in going beyond medical conditions as the means for identifying population groups sometimes turn to measures of disability, a higher level of analysis that subsumes not only the effects of the individual’s medical conditions, but the associated impacts in functioning, activities and/or participation. Among studies focused upon persons with disabilities, the themes we identified included disability classification and measurement, comparative studies of disability surveys and measures, common areas of disability measurement, medical complexity or frailty, and/or the importance of time in disability measurement.
Disability classification and measurement: The ICF
The World Health Organization proposed a common language to describe the various aspects of disablement by introducing the International Classification of Functioning, Disability and Health (ICF) which has now been generally adopted as the world standard. The ICF depicts disability as one end of a continuum of functioning and as an umbrella term for impairments, activity limitations and participation restrictions. It uses the terms body functions and structures, activity, and participation to represent the continuum of human functioning, influenced by health conditions, environmental factors, and personal factors.36 Disability thus represents a quite complex process comprised of multiple, interactive, and inter-related components which are rarely, if ever, measured in their entirety in health services research.36 Instead, even when setting out to collect their own primary data, researchers are typically forced to choose among measures and instruments on the basis of the purposes of their study. These might include the measurement of the outcomes of health interventions, describing the health or functioning of a community, determining resource allocation, comparing variables associated with health and health behaviors or measuring participation opportunities.37–39 As an overarching classification system, the ICF is perhaps most useful as a catalogue of the domains and subdomains of functioning, health and activities that might be appropriate for a given study’s purpose, as well as a gold standard reminder of those elements of the disablement process that will, inevitably, be excluded from measurement.36
Examples and comparisons of disability survey measures
A review of the disability content in 40 major national surveys (health and otherwise) was conducted by the Office of Disability, Aging and Long-Term Care Policy within the office of the Assistant Secretary for Planning and Evaluation (ASPE).40 The review reached many conclusions and offered a number of recommendations, among them:
Disability measurement is currently inadequate. The health and functional measures used to identify people with disabilities vary markedly in concept, detail, and quality across surveys. Except for surveys that explicitly focus upon health, most do not capture in-depth information on the health issues and functional limitations experienced by people with disabilities.
The specific measures of disability and wording of questions designed to elicit information about a particular type of disability (for example, visual impairment), differ markedly across surveys. Nearly all of the national surveys reviewed have questions that can be used to identify people with disabilities, but a few do not.
There is inadequate longitudinal data. Existing longitudinal data fail to reasonably identify persons with disabilities and do not provide a life course perspective on disability.
A concerted effort is being made to use a uniform set of disability indicators across surveys. The six-question series included in the American Community Survey (known as the ACS-6), the Current Population Survey (CPS), the American Housing Survey (AHS), and the National Health Interview Survey (NHIS) have each been a part of this effort. The ACS-6 questions are dichotomous (yes/no), with content areas covering hearing, sight, cognitive difficulties, mobility and ADLs/IADLs. These questions do not include items related to the environment around the person which, though a significant portion of the disablement process, is typical of the national surveys.
As the ASPE report suggests, there are many different disability measures that can be seen across the major US surveys. However, there is now a concerted effort to develop specific healthcare quality measures and surveys that are relevant for people with disabilities. This is crucial because the type and extent of healthcare service needs in populations with disability are frequently different than they are among people without disabilities and the needed settings and processes of care delivery may differ as well. As a result, the items of national health care quality surveys (such as CAHPS, the Consumer Assessment of Healthcare Providers and Systems) may require alterations to include the types, settings and processes of care most relevant to people with disabilities, as well as a means to accurately identify respondents with disabilities within the context of healthcare. An expert meeting convened by AHRQ (2010)41 and studies by Palsbo et al in 201042 and 2011,43 have directly addressed these issues.
In sum, the selection of disability measures for health service and related survey research must be purposive. Four categories of disability measures most used in studies of health care access, quality, utilization or cost are considered next. Typically, depending upon their definition of disability and their substantive interests, researchers will use elements from several of these categories together in a given study.
ADLs and IADLs
Activities of Daily Living (ADLs, including eating, using the toilet, dressing, transferring in and out of bed and chairs, walking in the home, and bathing) and Instrumental Activities of Daily Living (IADLs, including cooking, housework, shopping for groceries or clothing, taking medications, managing money, using a telephone, as well as using technology and transportation in some studies) are key disability measures. This is for a number of reasons, including that a) they are directly used for programmatic eligibility for services such as home health care, b) they are activities that all human beings must either do or have done on their behalf in modern societies, c) they correlate with severe disability, and d) they have been shown to be related to chronic health conditions, health service need and use in a number of studies.3,20,23,44–46 ADLs and IADLs are also used within definitions and measures of severity among people with mental health conditions33 and can be related to Serious Mental Illness (SMI).47 Sets of individual ADL and IADL items can also be “staged”, segmenting the population according to the level of and qualitative nature of needed supervision, support with personal care or domestic life activities, and possibly general health care utilization as well.46
Functional limitations
Functional limitations (referred to as activity limitations in the ICF and as basic actions by Altman & Bernstein (2008)48) sit “close to the skin” as difficulties that arise in a fairly direct fashion because of underlying impairments at the body / structural level. They are measured at the level of the whole person (such as walking, lifting, or learning a new task). Hence, macular degeneration may lead to limitations in seeing, spinal cord injury may lead to limitations in walking, and stroke may lead to limitations in communication. However, functional limitations may or may not go on to cause ADL or IADL limitations, depending upon the severity of the underlying health condition(s), access to rehabilitative care, assistive technology use and other related factors at the environmental level. Similarly, they need not interfere with other forms of participation such as work or school if those activities are designed with the needs of people with functional limitations in mind.
Measures of limitations in functioning in such areas as movement, sensory functioning, and cognitive functioning can be found in many major surveys with disability content such as the National Health Interview Survey (NHIS), the Medical Expenditure Panel Survey (MEPS), the Survey of Income and Program Participation (SIPP) and the Panel Study of Income Dynamics (PSID). Selected elements of emotional functioning—in particular, feelings that interfere with accomplishing daily activities, can be found in some surveys as well. Altman & Bernstein (2008)48 characterize functional limitations such as these as “basic action difficulties” and as building blocks that shape an individual’s overall functional profile. In turn, researchers who examine health care access or utilization use these functional limitation measures in many different combinations to capture some portion of the overall disablement process 3, 14, 20, 21 23 or a disability subgroup of interest, such as persons with mobility limitations49 or cognitive limitations.50
Participation and Activity limitations
Limitations in major activities and social roles appear in many of the national surveys. Be it work, school, recreation or socialization, these major activities involve multiple elements of participation and as such are particularly sensitive to the design of the social, attitudinal, architectural or public policy environment around the person. In this way they do not sit “close to the skin” as functional limitations do. Altman et al (2008)48 characterize them as “complex activity limitations”, in part because they depend on an individual’s functional profile, and just as much because they equally depend on many complicated factors that shape the physical and social world around the individual.
Access to and utilization of medical, social and related services (or goods) are enabling factors that are generally intended to 1) reduce or mitigate impairments and functional limitations, 2) increase independence in or management of ADLs and IADLs or 3) provide supportive, community-based or institutional care for individuals who cannot care for themselves.51 While these services and supports can and do enable fuller participation in social roles and activities, this may situate activity limitation more as an outcome measure and less as a means for defining or identifying people with disabilities, particularly in studies of general healthcare access, use or cost. However, limitations in activities such as work, school or socialization and days spent “out of role” nevertheless play an important part in assessing the severity of symptoms among persons with psychiatric disorders and other disabilities as well.33,52
Program eligibility/participation
An additional way of identifying people with disabilities is via their eligibility for or participation in public programs. Data from these sources provide large sample sizes, usually associated with health delivery records like those kept by the Medicare or Medicaid programs. While administrative data can be used to develop information about individuals with particular health conditions (as via claims files)19, disability measures are sparse in most of these sources and the scope is typically limited to medical visits, diagnoses or costs.37 While one advantage of these data sources is that they are usually kept in longitudinal fashion53, they remain tied to the specific criteria which define individuals eligible for services under the program and are thus not representative of the general population.54 Furthermore, in survey contexts, respondents frequently confuse the Medicare and Medicaid programs, and the SSI/SSDI programs as well.40
Cross-cutting issues: Complexity and time
This literature review revealed two additional conceptual themes relevant to disability measurement, be it in survey, clinical or administrative data contexts. The first of these concerns identifying individuals due to the complexity of their medical service needs,55–56 the extent of their co-morbidities34 or their “frailty”.57 For example, recognizing that comorbidity is the norm in rehabilitation settings, Stineman et al (2010) developed the Functional Diagnostic Complexity Index for Rehabilitation (FDC).56 This index is based on ICD-9-CM codes that are weighted to reflect their likely functional and medical impact. The authors found that increasing scores on the resulting index were highly predictive of functional dependence at admission and that patients in the highest medical complexity category had up to a 35% increase in rehabilitation length of stay. McColl & Short (2006)55 were also concerned with identifying persons with complex medical needs and high service use patterns, but as opposed to a specific focus on underlying medical conditions, they also turned to functional and activity limitations as predictors of high service use. Finding that disability had a significant independent effect on utilization, even after chronic disease and self-reported health were taken into account, they concluded that “there is something in the experience of functional limitations and participation restrictions that increases the likelihood of having contact with health professionals” (p.79).
Similarly, the overall severity of co-morbidities and the extent of frailty have received attention in this literature. For example, in a study describing the additive severity of depression and chronic pain in relation to health care use/costs, Arnow et al (2009)34 conclude that identifying subgroups of persons who contribute significantly to high utilization among persons with depression could improve screening procedures designed to identify such patients in primary care settings, bring about more precise targeting of patients with depression for participation in enhanced treatment programs, and inform changes in treatment for specific subgroups. The susceptibility to chronic conditions and co-morbidities has also been suggested as a means to identify a “frail” population group (particularly among elders).57
A final important theme concerns the role of time in the experience of disability. Though there are of course examples of functional limitations that remain static such as those due to amputation or permanent blindness, many of the health conditions associated with disabilities are chronic and tend to follow a changing course over time, whether progressive (cancers) or relapsing/remitting (MS, depression). Of course, the environment around the person may also change over time. As noted in the ASPE report (described earlier), longitudinal data are in short supply in relation to disability, making it critical for future studies to adopt longitudinal designs and to examine the role of time in their measures.40, 53
III. At the intersection: Chronic conditions and disabilities
A growing number of researchers and reports have documented the overlap between persons with chronic conditions and disabilities.49, 55–56, 58–59 This research suggests that these populations cannot be fully understood in the context of health service research in the absence of definitions, survey methods and analyses which more consistently account for this overlap.
The Committee on Living Well with Chronic Disease of the Institute of Medicine published a Call for Public Health (2012)26 that merits direct mention because it provides a carefully researched, macro-level framework for the advancement of health and well-being among persons with chronic disease and disability, including references to measurement, population surveillance, and health care policy priorities (see figure 2). The overarching framework attends to three primary domains, including determinants of health, policies and interventions, and the spectrum of health. Within this framework, the IOM describes a distribution of population level subgroups ranging from healthy, to “at risk”, to chronic illness without impairment, to functional limitations, to disability. Generally, this call to action is less concerned with primary prevention and more concerned with policies, interventions and social determinants that lead to positive health outcomes for persons living with the consequences of chronic conditions and disabilities. This consequence-based approach began in the pediatric sector with the definition and measurement of Children with Special Health Care Needs in the 1990s and continued with the development of the Adults with Special Healthcare Needs Screener in the early 2000s.60 The IOM report documents this paradigm shift, by which chronic disease and disability are increasingly understood not solely as bad health outcomes to be prevented, but as markers of population groups for which specific interventions in policy or practice may be required.
Figure 2. An integrated framework for living well with chronic illness.
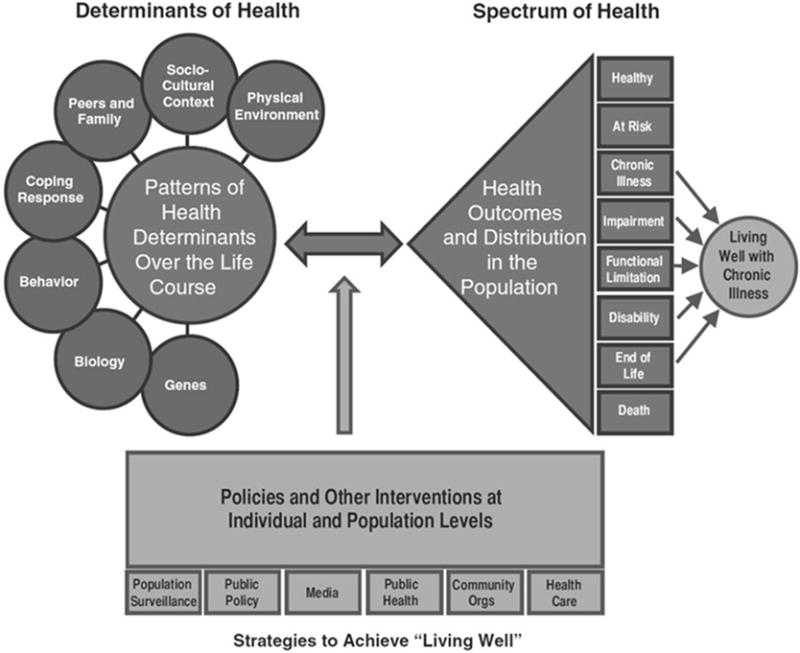
Source for figure 2:
Reprinted with permission from Living Well with Chronic Illness: A Call for Public Health Action, 2012, by the National Academy of Sciences, Courtesy of the National Academies Press, Washington, D.C.
One promising approach to the shared definition and measurement of chronic conditions, disability and healthcare service utilization is a new hybrid that is closely aligned with the IOM call for public health action. It begins with a criteria driven and exhaustive list of chronic medical conditions. Functional limitations and ADL/IADL needs are then separately utilized to segment the population with one or more chronic conditions into several groups with increasingly high service utilization profiles. The result is four primary groups 1) persons without chronic conditions, 2) persons with chronic conditions absent functional limitations or ADL/IADL support needs, 3) persons with chronic conditions and functional limitations that do not create the need for ADL/IADL supervision or support and 4) a final group with need for supports with ADLs or IADLs. In this way, whether an individual has one or many chronic conditions, functional limitations and ADL/IADL needs provide indicators of the possible complexity of the individual’s health care needs. Indeed, arrayed in this order, these groups have been shown to utilize progressively higher amounts of specialty care, hospitalizations, emergency department visits and home health care, making them particularly useful for population-based studies of healthcare access, care coordination and costs.3, 20–21
DISCUSSION
Since completion of this review, attention to the high need / high cost population has only accelerated,4, 11, 14, 61–64 but there remains little consensus over how best to conceptualize and identify these individuals. In a recent literature review on models of care for “people with complex needs”, Henkel, Hendricks & Church (2015)13 described the many disparate and overlapping population groups that potentially have such needs. These include not only persons with frequent ED visits, multiple hospital admissions, high rates of specialty care, or high burden conditions, but Medicaid enrolless with disabilities, individuals with severe mental illness or behavioral healthcare needs, individuals with unstable housing situations or food insecurity, as well as a variety of groups that may be at future risk. They go on to write:
“Outside of a general finding that programs are most effective when targeted to high-risk patients, the literature is not yet convincing on the most effective way to identify or calculate high risk. For example, some successful programs rely on predictive modeling, while others specifically target individuals with high rates of recent ED visits or inpatient admissions…Despite numerous efforts across the country to precisely predict who is likely to become a high-utilizer, gaps remain in these methods—many of which rely heavily on past claims data to identify high-risk patients. In fact, many risk prediction models only account for a quarter to a third of the factors that lead to individuals’ future expenditure, and typically do not perform well for high-need, high-cost patients” (pp 8 & 11).
It is notable that many of the subgroups that potentially compose this high need / high cost (or “complex”, or “super-utilizing”) population are being identified by researchers on the basis of what have traditionally been outcome measures such as ED visits, hospitalizations, program participation or costs. While these outcomes may be of great import to health policy, they may also be several steps removed from actual need for services or supports at the individual level. One risk of these approaches is that our research base grows increasingly convoluted as independent and dependent variables become further entangled. But a greater risk is that the clinical, care coordination or insurance programs designed around these scattershot definitions may exclude individuals who could most benefit from them, may include individuals who do not need the assistance, or may in some other way misallocate what are usually highly limited resources.
The way researchers define and measure population groups in health survey research thus shapes not only the estimates reported, but for whom they get reported. Our review raises several enduring questions about the proper scope, level and selection of measures in the existing literature, divided as it has primarily been between studies of chronic conditions and disability. More specifically, the results suggest that enhanced research upon the inter-relationships between medical conditions, functional limitations, ADLs/IADLs, and the environment around the person may serve to produce definitions and measures that will identify individuals in these population groups with greater accuracy, consistency and intepretability.
Studies of population groups based only upon a small subset of chronic conditions do provide useful information but at the cost of diverging, and at times, artificial scopes. Such studies can and do serve as bellwethers for how our healthcare system performs when confronted by individuals with particular conditions that require care beyond basic prevention, monitoring or health maintenance. They also can provide a window on the effectiveness of clinical practices for individuals with a select diagnosis, or perhaps for a category of closely related diagnoses. However, in the aggregate, the result is a body of literature with many different population groups, probably far more than clinicians or policymakers can reasonably be expected to follow. Further, such studies appear to vary widely by the methods used to control for the presence of additional chronic conditions. This is important, because roughly half of the working age who have a chronic condition actually have more than one at a time. Unless these additional conditions are properly and consistently controlled from one study to the next, the result is possibly a misattribution of the outcomes studied to the reference condition(s), as opposed to the full range of chronic conditions with which people actually live at the population level. The key point to remember would seem to be that conditions and populations are not analogous.
On the other hand, there are broader, criteria based approaches to the identification of people with chronic conditions, typically including a time frame referent (lasting one year or longer in some studies, or three months or greater in others) and a statement of additional qualifiers, such as a resulting need for particular kinds of medical care. Depending on the time frame and the extent of the qualifiers used with this approach (such as AHRQ’s HCUP list), the resulting number and sheer variability of conditions included, and thus people identified, leads to the selection of a population with a very wide scope and a medically heterogeneous make-up. This is, potentially, both a strength and a weakness of such methods. They serve to emphasize the sheer size (upwards of half of the working aged in some studies) and diversity of care needs among people experiencing chronic conditions. They also provide a much needed, if large, common denominator for use across studies where full enumeration of medical conditions is possible. However, they also lack specificity, and on their own, do not necessarily provide adequate handles for the identification of subgroups that are actionable at a level useful for policy or practice change. Reducing the scope to persons with 2 or more simultaneous chronic conditions may come closer to this level, but the result is still a large population (upwards of a quarter of the working aged in some studies). Further it remains difficult to establish whether persons with two or more chronic conditions (such as allergies and high blood pressure, for instance) are necessarily a better target for intervention in all instances than persons with just one chronic condition (such as cancer, for instance).
In this review, we found that measures associated with various aspects of the disablement process have also long been used in health survey research, though inconsistently from one study to the next. Currently, the ICF stands as perhaps the most fully articulated taxonomy of disability and health, but as several authors described, while useful as a guide, it is too complex for simple translation in health surveys which have only limited space to devote to disability measurement.36–37 Accordingly, there were many differences in the disability definitions and measures employed in this literature, yet there was also an unmistakable connection across the studies linking disability with an elevated need for / use of a wide range of medical and related services.
More specifically, it was noted that disability measures that focus on simple bodily tasks (such as functional limitations, ADLs and IADLs) may be more directly correlated with medical care than other measures of the disablement process. At least in a relative sense, participation in more complex activities such as work or school, or program participation such as in SSI or Medicaid, potentially depend upon a wider array of environmental variables more distant from the person, such as employment discrimination, accessible classrooms or health policy.
There is now a window for consolidation of these various approaches to measurement. Though its future may be uncertain, the ACS-6 now appears in many of the major government sponsored surveys of health, and with the express intent of improving the consistency of disability surveillance from one study to the next. HHS also published its strategic framework on multiple chronic conditions with the goal of aligning policies, practices and research to better meet the needs of persons with ongoing and significant medical needs. The Institute of Medicine published its own call for public health action on living well with chronic illness. This stresses patient-centered care across the spectrum of chronic disease and disability and advocates “segmenting” (or stratifying) this large and heterogeneous population into smaller, more actionable subgroups. Each of these developments is pointing in a new and common direction. At the population level, it is not merely which, nor how many, medical conditions people have, nor is it solely how severe their particular functional limitations may be, nor is it just how constrained their daily activities are, that may ultimately drive the ongoing need for and use of medical care and supportive services. From the vantage point of this review, it appears to be the interrelationships of each of these domains within the environment around the person that ultimately drive people to seek care.
There are some apparent steps researchers and other stakeholders might take next. First, additional theoretical work and quantitative analyses aimed at a better mapping of the relationships between chronic physical and mental health condition(s), functional and ADL/IADL limitations, and the need for medical care or related supports would likely benefit the consolidation of this field. Existing data sources such as the MEPS, NHIS, SIPP and PSID contain rich measures in these domains. Supplements to those surveys, whether to extend topical coverage of issues concerning people with ongoing and elevated needs for care, or to test novel measures, might be important first steps. Second, the development of a consensus population definition for adult healthcare, be it one focused upon high-need / high cost, special, chronic or complex healthcare needs may be crucial, much as it proved to be in the pediatric sector when the MCHB formally defined Children with Special Healthcare Needs. Third, the development of a brief screening instrument that is operationalized based on the work described above and that is designed for permanent inclusion in national health surveys could prove to be valuable for the field, providing as it would a common denominator for many different health services research topics.10 Last, new mechanisms for “segmenting” (or stratifying) this population that go beyond medical diagnoses will be needed, both because we should expect to identify a very large number of individuals under such a definition, and because such individuals will be likely to have numerous co-occurring conditions and circumstances.
STUDY LIMITATIONS
We focused our search efforts primarily on U.S. literature, academic centers and governmental agencies and limited our coverage to works published in English. The findings should thus be taken as having a U.S.-centric scope. Second, we used two search engines, medline and psycINFO which, while appropriate for our inquiry, are not exhaustive. Third, our list of key journals may have had a stronger focus on disability than upon chronic disease, though this would not have affected our other search strategies. Fourth, a well-grounded summary of the scientific study of chronic disease and disability at the population level will certainly include research dating further back; Though we now see a heightened focus upon high need / high cost individuals in health service research, particularly as regards coordination and costs of care for persons with chronic conditions and disabilities, some of the definitions and measures we rely upon are rooted in scholarship produced well before the new millennium.
CONCLUSION
Despite growing concern over the health and healthcare access, use and costs of working age adults with ongoing and elevated needs for services and supports, there is at present no uniform definition of this population in the health services research literature or means by which to identify them. The available measures are fragmentary and overlapping, leading to estimates that vary widely with the purposes for which they are selected. However, the Call for Public Health from the IOM marked what may be the beginning of a paradigm shift where chronic disease and disability are understood as markers of population groups for whom specific interventions may be required. Promising measurement approaches are beginning to emerge that account for the overlap between chronic disease and disability using a health consequence-based approach in order to “segment” this large and medically heterogeneous population into more actionable subgroups. There is a pressing need for more consistent methods to examine the performance of health systems in caring for this population and to inform the development of interventions that yield improved outcomes.
Supplementary Material
Acknowledgments
This research was supported by the NIH Intramural Research Program. The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the National Institutes of Health, the United States government or the other institutions with which the authors are affiliated. The authors gratefully acknowledge the contributions of the other members of the ACHCN expert panel, including: Barbara Altman, Ph.D. (Disability statistics consultant, Rockville, MD), Stephen Blumberg, Ph.D., (CDC/NCHS) and Margaret Grace Stineman, MD, (Perelman School of Medicine, University of Pennsylvania).
Support: NIH Intramural Research Program
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts: The authors have no funding or other conflicts of interest.
Prior dissemination: None.
Online only appendix table: Chronic disease, disability and health services research: Scoping literature review results
References
- 1.Reichard A, Gulley S, Rasch E, Chan L. Diagnosis isn’t enough: Understanding the connections between high health care utilization, chronic conditions and disabilities among U.S. working age adults. Disabil and Health J. 2015;8(4):535–546. doi: 10.1016/j.dhjo.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rasch E, Gulley S, Chan L. Use of emergency departments among working age adults with disabilities: A problem of access and service needs. Health Serv Res. 2013;48(4):1–25. doi: 10.1111/1475-6773.12025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gulley S, Rasch E, Chan L. If we build it, who will come? Working age adults with chronic health care needs and the medical home. Med Care. 2011;49(2):149–155. doi: 10.1097/MLR.0b013e3182028380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hayes S, Salzberg C, McCarthy D, Radley D, Abrams M, Shah T, Anderson G. High-Need, High-Cost Patients: Who are they and how do they use healthcare? Vol. 26. New York, NY: Commonwealth Fund publication; 1897. Aug, 2016. [Google Scholar]
- 5.Hasselman D. Super-Utilizer summit: Common themes from innovative complex care management programs. Center for Health Care Strategies, Inc., Robert Wood Johnson Foundation, The Atlantic Philanthropies; Oct, 2013. pp. 1–31. [Google Scholar]
- 6.Gawande A. The hot spotters. The New Yorker; Jan 17, 2011. Accessed October 15, 2016. Available from: http://www.newyorker.com/magazine/2011/01/24/the-hot-spotters. [PubMed] [Google Scholar]
- 7.Anderson G, Knickman J. Changing the chronic care system to meet people’s needs. Health Aff. 2001;20(6):146–160. doi: 10.1377/hlthaff.20.6.146. [DOI] [PubMed] [Google Scholar]
- 8.Kronick R, Bella M, Gilmer T, Somers S. The faces of Medicaid II: Recognizing the care needs of people with multiple chronic conditions. Trenton, NJ: Center for Health Care Strategies, Inc.; Oct, 2007. Accessed on October 15 2016. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Reports/Downloads/Kronick.pdf. [Google Scholar]
- 9.U.S. Department of Health and Human Services. Multiple chronic conditions—A strategic framework: Optimum health and quality of life for individuals with multiple chronic conditions. Washington, DC: HHS; Dec, 2010. Accessed October 15, 2016. Available from: http://www.hhs.gov/sites/default/files/ash/initiatives/mcc/mcc_framework.pdf. [Google Scholar]
- 10.Gulley S, Rasch E, Altman B, Bethell C, Carle A, Druss B, Houtrow A, Reichard A, Chan L. Introducing the Adults with Chronic Healthcare Needs (ACHCN) definition and screening instrument: Rationale, supporting evidence and testing. Disabil Health J. 2017 doi: 10.1016/j.dhjo.2017.08.003. In press, available online ahead of print at: http://www.disabilityandhealthjnl.com/article/S1936-6574(17)30139-5/fulltext. [DOI] [PMC free article] [PubMed]
- 11.Blumenthal D, Chernof B, Fulmer T, Lumpkin J, Selberg J. Caring for high-need, high-cost patients – An urgent priority. N Engl J Med. 2016;375(10):909–911. doi: 10.1056/NEJMp1608511. [DOI] [PubMed] [Google Scholar]
- 12.Page-Reeves J, Kaufman W, Bleecker M, Norris J, McCalmont K, Ianakieva V, Ianakieva D, Kaufman A. Addressing social determinants of health in a clinic setting: The WellRx pilot in Albuquerque, New Mexico. J Am Board Fam Med. 2016;29(3):414–418. doi: 10.3122/jabfm.2016.03.150272. [DOI] [PubMed] [Google Scholar]
- 13.Thomas-Henkel C, Hendricks T, Church K. Opportunities to improve models of care for people with complex needs: Literature Review. New York, NY: The Robert Wood Johnson Foundation and the Center for Health Care Strategies; Nov, 2015. Accessed October 15, 2016. Available from: http://www.chcs.org/media/HNHC_CHCS_LitReview_Final.pdf. [Google Scholar]
- 14.Peterson Center on Healthcare. Issue brief – Improving healthcare for high-need patients. New York, NY: Peterson Center on Healthcare; 2016. Accessed on October 15, 2016. Available from: http://petersonhealthcare.org/high-need-patients/issue-brief. [Google Scholar]
- 15.Gulley S, Rasch E, Chan L. The complex web of health: Relationships among chronic conditions, disability, and health services. Public Health Reports. 2011;126(4):495–507. doi: 10.1177/003335491112600406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dejong G, Palsbo S, Beatty P, Jones G, Knoll T, Neri M. The organization and financing of health services for persons with disabilities. Milbank Q. 2002;80(2) doi: 10.1111/1468-0009.t01-1-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arksey H, O’Malley L. Scoping studies: toward a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 18.Egede L. Major depression in individuals with chronic medical disorders: Prevalence, correlates and association with health resource utilization, lost productivity and functional disability. Gen Hosp Psychiatry. 2007;29(5):409–416. doi: 10.1016/j.genhosppsych.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 19.Schneider K, O’Donnell B, Dean D. Prevalence of multiple chronic conditions in the United States’ Medicare population. Health Qual Life Outcomes. 2009;7(82):1–11. doi: 10.1186/1477-7525-7-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alecxih L, Shen S, Chan I, Taylor D, Drabek J. Individuals living in the community with chronic conditions and functional limitations: A closer look. Washington, DC: Office of the Assistant Secretary for Planning & Evaluation, U.S. Department of Health and Human Services; 2010. [Google Scholar]
- 21.Anderson G. Chronic Care: Making the Case for Ongoing Care. Princeton, NJ: Robert Wood Johnson Foundation; 2010. [Google Scholar]
- 22.Elrod C, DeJong G. Determinants of utilization of physical rehabilitation services for persons with chronic and disabling conditions: an exploratory study. Arch Phys Med Rehabil. 2008;89(1):114–120. doi: 10.1016/j.apmr.2007.08.122. [DOI] [PubMed] [Google Scholar]
- 23.Gulley S, Rasch E, Chan L. Ongoing coverage for ongoing care: access, utilization, and out-of-pocket spending among uninsured working-aged adults with chronic health care needs. Am J Public Health. 2011;101(2):368–375. doi: 10.2105/AJPH.2010.191569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anderson G, Horvath J. The growing burden of chronic disease in America. Public Health Rep. 2004;119(3):263–270. doi: 10.1016/j.phr.2004.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hwang W, Weller W, Ireys H, Anderson G. Out-Of-Pocket Medical Spending For Care Of Chronic Conditions. Health Aff. 2001;20(6):267–278. doi: 10.1377/hlthaff.20.6.267. [DOI] [PubMed] [Google Scholar]
- 26.Institute of Medicine. Living well with chronic illness: A call for public health action. Washington, DC: The National Academies Press; 2012. [Google Scholar]
- 27.Balogh R, Ouellette-Kuntz H, Brownell M, Colantonio A. Ambulatory care sensitive conditions in persons with an intellectual disability - Development of a consensus. J Appl Res Intellect Disabil. 2011;24:150–158. [Google Scholar]
- 28.Schmittdiel J, Mosen D, Glasgow R, Hibbard J, Remmers C, Bellows J. Patient assessment of chronic illness care (PACIC) and improved patient-centered outcomes for chronic conditions. Gen Intern Med. 2008;23(1):77–80. doi: 10.1007/s11606-007-0452-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Diederichs C, Bartels D. The measurement of multiple chronic diseases - a systematic review on existing multimorbidity indices. J Gerontol A Biol Sci Med Sci. 2010;66(3):301–311. doi: 10.1093/gerona/glq208. [DOI] [PubMed] [Google Scholar]
- 30.Agency for Healthcare Quality and Research. Chronic condition indicator (CCI) for ICD-9-CM. Rockville, MD: AHRQ; 2015. Accessed on October 15, 2016. Available from: http://www.hcup-us.ahrq.gov/toolssoftware/chronic/chronic.jsp. [Google Scholar]
- 31.Parekh A, Goodman R, Gordon C, Koh H. Managing multiple chronic conditions: a strategic framework for improving health outcomes and quality of life. Public Health Rep. 2011;126(4):460–471. doi: 10.1177/003335491112600403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kessler R, Merikangas K, Wang P. Prevalence, comorbidity, and service utilization for mood disorders in the United States at the beginning of the twenty-first century. Annu Rev Clin Psychol. 2007;3:137–158. doi: 10.1146/annurev.clinpsy.3.022806.091444. [DOI] [PubMed] [Google Scholar]
- 33.Druss B, Hwang I, Petukhova M, Sampson N, Wang P, Kessler R. Impairment in role functioning in mental and chronic medical disorders in the United States: results from the National Comorbidity Survey Replication. Mol Psychiatry. 2009;14(7):728–737. doi: 10.1038/mp.2008.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Arnow B, Blasey C, Lee J, Fireman B, Hunkeler E, Dea R, Robinson R, Hayward C. Relationships among depression, chronic pain, chronic disabling pain and medical costs. Psychiatr Serv. 2009;60(3):344–350. doi: 10.1176/ps.2009.60.3.344. [DOI] [PubMed] [Google Scholar]
- 35.Valderas J, Starfield B, Sibbald B, Salisbury C, Roland M. Defining comorbidity: implications for understanding health and health services. Ann Fam Med. 2009;7(4):357–363. doi: 10.1370/afm.983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fekete C, Bolt C, Post M, Eriks-Hoogland I, Cieza A, Stucki G. How to measure what matters: development and application of guiding principles to select measurement instruments in an epidemiologic study on functioning. Am J Phys Med Rehabil. 2011;90(11):29–38. doi: 10.1097/PHM.0b013e318230fe41. [DOI] [PubMed] [Google Scholar]
- 37.Altman B, Gulley S. Convergence and divergence: differences in disability prevalence estimates in the United States and Canada based on four health survey instruments. Soc Sci Med. 2009;69(4):543–552. doi: 10.1016/j.socscimed.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 38.Becker H. Measuring health among people with disabilities. Fam Community Health. 2006;29(1S):70–77. doi: 10.1097/00003727-200601001-00011. [DOI] [PubMed] [Google Scholar]
- 39.Madans J, Loeb B, Altman B. Measuring disability and monitoring the UN Convention on the rights of persons with disabilities: The work of the Washington Group on Disability Statistics. BMC Public Health. 2011;11(Suppl4):S4. doi: 10.1186/1471-2458-11-S4-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Livermore G, Whalen D, Stapleton D. Assessing the Need for a National Disability Survey: Final Report. Washington, DC: Assistant Secretary for Planning and Evaluation, US Department of Health and Human Services; 2011. [Google Scholar]
- 41.Iezzoni L. Developing Quality of Care Measures for People with Disabilities: Summary of Expert Meeting. Rockville, MD: Agency for Healthcare Research and Quality; 2010. [Google Scholar]
- 42.Palsbo S, Diao G, Palsbo G, Tang L, Rosenberger W, Mastal M. Case-mix adjustment and enabled reporting of the health care experiences of adults with disabilities. Arch Phys Med Rehabil. 2010;91(9):1339–1346. doi: 10.1016/j.apmr.2010.06.018. [DOI] [PubMed] [Google Scholar]
- 43.Palsbo S, Hurtado M, Levine R, Barrett K, Mastal M. Enabling a survey of primary care to measure the health care experiences of adults with disabilities. Disabil Rehabil. 2011;33(1):73–85. doi: 10.3109/09638288.2010.485671. [DOI] [PubMed] [Google Scholar]
- 44.Federman S, Penrod J, Livote E, Hebert P, Keyhani S, Doucette J, Siu A. Development of and recovery from difficulty with activities of daily living: an analysis of national data. J Aging Health. 2009;22(8):1081–1098. doi: 10.1177/0898264310375986. [DOI] [PubMed] [Google Scholar]
- 45.Olin G, Dougherty D. Characteristics and Medical Expenses of Adults 18 to 64-Years Old with Functional Limitations, Combined Years 1997-2002. Rockville MD: Agency for Healthcare Research and Quality; 2006. (Working Paper No. 06002). [Google Scholar]
- 46.Stineman M, Xie D, Pan Q, Kurichi J, Saliba D, Streim J. Activity of daily living staging, chronic health conditions, and perceived lack of home accessibility features for elderly people living in the community. J Am Geriatr Soc. 2011;59(3):454–462. doi: 10.1111/j.1532-5415.2010.03287.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kessler R, Berglund P, Bruce M, Koch J, Laska E, Leaf P, Manderscheid R, Rosenheck R, Walters E, Wang P. The prevalence and correlates of untreated serious mental illness. Health Serv Res. 2001;36(6Pt1):987–1007. [PMC free article] [PubMed] [Google Scholar]
- 48.Altman B, Bernstein A. Disability and Health in the United States, 2001-2005. Hyattsville, MD: National Center for Health Statistics; 2008. [Google Scholar]
- 49.Rasch E, Hochberg M, Magder L, Magaziner J, Altman B. Health of community-dwelling adults with mobility limitations in the United States: prevalent health conditions (part I) Arch Phys Med Rehabil. 2008;89(2):210–218. doi: 10.1016/j.apmr.2007.08.146. [DOI] [PubMed] [Google Scholar]
- 50.Reichard A, Stolzle H, Fox M. Health disparities among adults with physical disabilities or cognitive limitations compared to individuals with no disabilities in the United States. Disabil Health J. 2011;4(2):59–67. doi: 10.1016/j.dhjo.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 51.National Council on Disability. The Current State of Health Care for People with Disabilities. Washington, DC: National Council on Disability; 2009. [Google Scholar]
- 52.Gulley S, Altman B. Disability in two health care systems: access, quality, satisfaction, and physician contacts among working-age Canadians and Americans with disabilities. Disabil Health J. 2008;1(4):196–208. doi: 10.1016/j.dhjo.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 53.Chan L, Marcia A, Shumway-Cook A, Yorkston K, Dudgeon B, Asch S, Hoffman J. A Longitudinal Evaluation of Persons With Disabilities: Does a Longitudinal Definition Help Define Who Receives Necessary Care? Arch Phys Med Rehabil. 2008;289(6):1023–1030. doi: 10.1016/j.apmr.2007.10.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Iezzoni L. Using administrative data to study persons with disabilities. Milbank Q. 2002;80(2):347–379. doi: 10.1111/1468-0009.t01-1-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.McColl M, Shortt S. Another way to look at high service utilization: the contribution of disability. J Health Serv Res Policy. 2006;11(2):74–80. doi: 10.1258/135581906776318848. [DOI] [PubMed] [Google Scholar]
- 56.Stineman M, Ross R, Willams S, Goin J, Grander C. A functional diagnostic complexity index for rehabilitation medicine: measuring the influence of many diagnoses on functional independence and resource use. Arch Phys Med Rehabil. 2000;81(5):549–557. doi: 10.1016/s0003-9993(00)90033-9. [DOI] [PubMed] [Google Scholar]
- 57.Fried L, Ferrucci L, Darer J, Williamson J, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: Implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59(3):255–263. doi: 10.1093/gerona/59.3.m255. [DOI] [PubMed] [Google Scholar]
- 58.Iezzoni L. Multiple chronic conditions and disabilities: implications for health services research and data demands. Health Serv Res. 2010;45(5part2):1523–1540. doi: 10.1111/j.1475-6773.2010.01145.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wolff J, Boult C, Boyd C, Anderson G. Newly reported chronic conditions and onset of functional dependency. J Am Geriatr Soc. 2005;53(5):851–855. doi: 10.1111/j.1532-5415.2005.53262.x. [DOI] [PubMed] [Google Scholar]
- 60.Bethell C, Read D. Approaches to Identifying Children and Adults with Special Health Care Needs: A resource manual for state Medicaid agencies and managed care organizations. Portland, OR: The Child and Adolescent Health Measurement Initiative; [Google Scholar]
- 61.Salzberg C, Hayes S, McCarthy D, Radley D, Abrams M, Shah T, Anderson G. Health system performance for the high-need patient: A look at access to care and patient care experiences. Vol. 27. New York, NY: Commonwealth Fund publication; 1898. Aug, 2016. [PubMed] [Google Scholar]
- 62.Ryan J, Abrams M, Doty M, Shah T, Schneider E. How high-need patients experience health care in the United States: Findings from the 2016 Commonwealth Fund survey of high-need patients. Vol. 43. New York, NY: Commonwealth Fund publication; 1919. Dec, 2016. [PubMed] [Google Scholar]
- 63.Thomas-Henkel C, Schulman M. Screening for Social Determinants of Health in Populations with Complex Needs: Implementation Considerations. New York, NY: The Robert Wood Johnson Foundation and the Center for Health Care Strategies; Oct, 2017. Accessed November 25, 2017. Available from: https://www.chcs.org/media/SDOH-Complex-Care-Screening-Brief-102617.pdf. [Google Scholar]
- 64.Long M, Abrams A, Milstein G, Anderson K, Lewis-Apton M, Dahlberg L, Whicher D. Effective Care for High-Need Patients: Opportunities for Improving Outcomes, Value, and Health. Washington, DC: National Academy of Medicine; 2017. [PubMed] [Google Scholar]
- 65.Callahan T, Cooper W. Access to health care for young adults with disabling chronic conditions. Arch Pediatr Adolesc Med. 2006;160(2):178–182. doi: 10.1001/archpedi.160.2.178. [DOI] [PubMed] [Google Scholar]
- 66.Elhai J, Ford J. Correlates of mental health service use intensity in the national comorbidity survey and national comorbidity survey replication. Psychiatric Serv. 2007;58(8):1108–1115. doi: 10.1176/ps.2007.58.8.1108. [DOI] [PubMed] [Google Scholar]
- 67.Harniss M, Amtmann D, Cook D, Johnson K. Considerations for developing interfaces for collecting patient reported outcomes that allow the inclusion of individuals with disabilities. Med Care. 2007;4(5suppl1):48–54. doi: 10.1097/01.mlr.0000250822.41093.ca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Iezzoni L. Eliminating health and health care disparities among the growing population of people with disabilities. Health Aff. 2011;30(10):1947–1954. doi: 10.1377/hlthaff.2011.0613. [DOI] [PubMed] [Google Scholar]
- 69.Kaye S, Harrington C, LaPlante M. Long-Term Care: Who Gets It, Who Provides It, Who Pays, And How Much? Health Aff. 2010;29(1):11–21. doi: 10.1377/hlthaff.2009.0535. [DOI] [PubMed] [Google Scholar]
- 70.Krahn G, Fox M, Campbell V, Ramon I, Jesien G. Developing a Health Surveillance System for People With Intellectual Disabilities in the United States. J Policy Pract Intellect Disabil. 2010;7(3):155–166. [Google Scholar]
- 71.Livermore G, Stapleton D, O’Toole M. Health Care Costs Are A Key Driver Of Growth In Federal And State Assistance To Working-Age People With Disabilities. Health Aff. 2011;30(9):1664–1672. doi: 10.1377/hlthaff.2011.0247. [DOI] [PubMed] [Google Scholar]
- 72.McDermott S, Turk M. The myth and reality of disability prevalence: measuring disability for research and service. Disabil Health J. 2011;4(1) doi: 10.1016/j.dhjo.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 73.National Healthcare Disparities Report, 2011. Rockville MD: Agency for Healthcare Research and Quality; 2012. [Google Scholar]
- 74.O’Day B, Killeen M, Sutton J, Iezzoni L. Primary Care Experiences of People with Psychiatric Disabilities: Barriers to Care and Potential Solutions. Psychiatric Rehabil J. 2005;28(4):339–345. doi: 10.2975/28.2005.339.345. [DOI] [PubMed] [Google Scholar]
- 75.Owens P, Kerker B, Zigler E, Horwitz S. Vision and oral health needs of individuals with intellectual disability. Ment Retard Dev Disabil Res Rev. 2006;12(1):28–40. doi: 10.1002/mrdd.20096. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


