Abstract
Objectives
To quantify longitudinal change in financial and health literacy and examine the associations of declining literacy with incident Alzheimer’s disease (AD) dementia and mild cognitive impairment (MCI).
Methods
Data came from 799 participants of an ongoing cohort study. Literacy was measured using a battery of 32 questions. Clinical diagnoses were made annually following uniform structured procedures. The associations of declining literacy with incident AD dementia and MCI were tested using a joint model for longitudinal and time-to-event data.
Results
We observed an overall decline in total literacy score over up to 6 years of follow-up (p<0.001). Faster decline in literacy was associated with higher risks for incident AD dementia (hazard ratio: 4.526, 95% confidence interval: 2.993–6.843, p<0.001) and incident MCI (hazard ratio: 2.971, 95% confidence interval: 1.509–5.849, p=0.002).
Discussion
Declining literacy among community-dwelling older persons predicts adverse cognitive outcomes and serves as an early indicator of impending dementia.
Keywords: Aging, Domain specific literacy, AD dementia, Mild cognitive impairment
INTRODUCTION
Maintenance of functional literacy, particularly in the domains of financial and health matters, is essential for independence and well-being in late life. Lower financial literacy is associated with poor financial outcomes including suboptimal retirement planning and less wealth accumulation(Lusardi & Mitchell, 2011). Lower health literacy is associated with adverse health outcomes, including all-cause mortality(D. W. Baker et al., 2007), hospital admission(D. W. Baker, Parker, Williams, & Clark, 1998) and readmissions(Bailey et al., 2015), as well as poorer overall physical and mental health(Wolf, Gazmararian, & Baker, 2005). Further, older persons with higher financial and health literacy are more likely to engage in health-promoting behaviors(J. S. Bennett, Boyle, James, & Bennett, 2012; L. C. Kobayashi, Wardle, Wolf, & von Wagner, 2016), and exhibit better decision making(Bryan D James, Boyle, Bennett, & Bennett, 2012). Importantly, cross-sectional data suggest that many older persons exhibit low levels of financial and health literacy(David W Baker, Gazmararian, Sudano, & Patterson, 2000; Kutner, Greenburg, Jin, & Paulsen, 2006), but data on possible age-related changes in literacy are just beginning to emerge. One recent study in England reported a decrease in health literacy over time in a cohort of non-cognitively impaired adults aged 52 years and older(Lindsay C Kobayashi, Wardle, Wolf, & von Wagner, 2015), but findings were based on only two waves of data. Thus, the degree to which low literacy in old age reflects a longstanding phenomenon versus an aging-related process remains unclear.
Although prospective studies examining the relationship of functional literacy with the risk of Alzheimer’s disease (AD) and its precursor, mild cognitive impairment (MCI), are limited, emerging data suggest that low literacy may be a harbinger of adverse cognitive health outcomes. One study reported that low health literacy was associated with an increased risk of “likely dementia”(Kaup et al., 2014). Further, we recently reported that higher levels of financial and health literacy were associated with a reduced risk of AD dementia(Wilson, Yu, James, Bennett, & Boyle, 2017), and the association of literacy with AD was independent of traditional measures of cognition(Yu, Wilson, Schneider, Bennett, & Boyle, 2017). However, because measurement of literacy at a single timepoint is influenced by preexisting factors such as education, occupation and prior experience, it is unclear whether the relationship between literacy and cognitive impairment is driven by an underlying disease process. It is therefore of particular importance to examine whether literacy declines with advancing age and to determine whether age-related changes in literacy are related to the risk of AD dementia or MCI.
In this study, we quantified the rate of change in literacy over many years in a large cohort of well-characterized and community based older persons without dementia, and tested the hypothesis that faster decline in literacy are associated with incident AD dementia and incident MCI. To do so, we integrated up to 7 years of annual literacy assessments with annual clinical diagnoses of AD dementia by employing a novel shared-parameter model. The approach allows examination of longitudinal data for literacy and time-to-event data for incident AD dementia in a single modeling framework. In a separate model, we examined the association with incident MCI.
METHODS
Participants
Data came from participants in the Rush Memory and Aging Project (MAP), a community based longitudinal cohort study of aging and dementia(D. A. Bennett et al., 2012). Started in 1997, the study primarily recruits residents from continuous care retirement communities in northeastern Illinois. Participants are enrolled in the study without known dementia, and agree to detailed clinical evaluation every year and organ donation after death. The study was approved by the Institutional Review Board of Rush University Medical Center and each participant signed a written consent form.
At time of the analyses, MAP had recruited 1,850 older persons, of which 1,803 had completed the baseline evaluation. The assessment of literacy did not start until 2010. By then, 571 participants had died and 67 had withdrawn from the parent study. In addition, 73 participants had severe language, hearing, or vision difficulty or no longer lived in the geographical area. This left 1,092 participants eligible for the literacy assessment. Of those, 996 had completed at least 1 literacy assessment; 61 had yet to be approached and 35 (3.2%) had refused the assessment. Since the analysis was primarily focused on the relationship of change in literacy with incident AD dementia, we further restricted the sample to 799 participants who had valid literacy data, were not demented at baseline, and had at least 1 follow-up clinical evaluation.
Assessment of longitudinal literacy
We define literacy as the ability to access, comprehend and use financial and health information and concept to function effectively in society. Literacy assessment was administered annually using a battery of 32 questions, from which change in literacy was determined. The complete panel of questions has been published previously(Bryan D James et al., 2012). Briefly, two components of literacy were available. A health literacy component was based on 9 questions which covered topics including Medicare, following prescription instruction, vaccination, leading causes of death in elderly, and ability of assessing drug risk. Each of the 9 questions was scored as correct or incorrect, and the health literacy score was the percent of total correct. Separately, a financial literacy component was based on 23 questions, many of which were adapted from the Health and Retirement Survey(Juster & Suzman, 1995). This component assessed a broad range of knowledge on financial information, concepts and numeracy. Each of the 23 questions was scored as correct or incorrect, and the financial literacy score was the percent of total correct. A composite score for total literacy was obtained by averaging the financial and health literacy scores. The total literacy score had adequate internal consistency(Bryan D James et al., 2012) and was correlated with health promoting behaviors and health status in older persons(J. S. Bennett et al., 2012; Han, Boyle, James, Yu, & Bennett, 2015; Han et al., 2014). For the purpose of this study, literacy measures collected after the clinical events were not included in the analysis.
Diagnosis of AD dementia and cognitive impairment
Each participant underwent uniform annual clinical evaluations which included a medical history, neurologic examination, and cognitive tests. Details of the diagnostic process have been described in prior publications(D. A. Bennett, Schneider, Bienias, Evans, & Wilson, 2005; Schneider, Arvanitakis, Leurgans, & Bennett, 2009). Briefly, cognitive tests were scored by computer, and a neuropsychologist reviewed the scores and rated the presence of cognitive impairment in multiple cognitive domains including memory. AD dementia was diagnosed by a clinician using the recommendations of the joint working group of the National Institute of Neurologic and Communicative Disorders and Stroke and the Alzheimer's Disease and Related Disorders Association (NINCDS/ADRDA)(McKhann et al., 1984). MCI was determined for persons with cognitive impairment but without dementia.
Other covariates
Common chronic medical conditions, including hypertension, diabetes, heart disease, cancer, thyroid disease, head injury and stroke, were recorded. A composite score was obtained by adding up the number of conditions present, with higher score indicating greater burden of medical conditions (Wilson, Mendes De Leon, et al., 2002). A 30-item Mini Mental State Examination (MMSE) was administered as a standard screening measure for dementia severity. The measure of instrumental activities of daily living (IADL) was adapted from the Duke Older Americans Resources and Services project, which assesses the ability of performing 8 household management and self-care activities including telephone use, meal preparation, light housekeeping, heavy housekeeping, medication handling, finance handling, shopping and traveling within the community. A composite score was obtained by adding up the number of activities that needed for help with higher score indicating greater disability (P. A. Boyle, Buchman, Wilson, Bienias, & Bennett, 2007). Number of depressive symptoms was measured using a 10-item version of the Center for Epidemiologic Studies Depression scale (CES-D) with higher score indicating greater depressive symptoms (Wilson, Barnes, et al., 2002). The ability to read was assessed based on the National Adult Reading Test (NART), which measures the total number of 10 words correctly pronounced and higher score indicates better reading ability.
Statistical analysis
Pearson and Spearman correlations and t-tests examined the bivariate relationship between literacy measures and demographics, MCI status as well as comorbid conditions at baseline. We assessed longitudinal change in literacy using a linear mixed model with random intercept and slope. In this model, the scores of annual literacy assessment were the continuous longitudinal outcome. For subject i, denote the longitudinal literacy scores by a vector yi, the model (M1) took the form yi(t) = β0 + β1t + b0i + b1it + εi. Note that the predictors included a term for time in years since the analytic baseline (t), and its coefficient β1 captures the mean rate of change in literacy (slope). Person-specific deviation from mean change in literacy is captured by random slope (b1i).
Next, a joint modeling approach for longitudinal and time to event data was used to examine the association of change in literacy with risk of incident AD dementia, and separately incident MCI. The statistical properties of the model are discussed in detail elsewhere(Rizopoulos, 2012). Briefly, in our analysis, the joint model was composed of a longitudinal submodel, as in M1, and a survival submodel (M2) of the form . Here, h0(t) is the baseline hazard, yi(t) is the literacy at time t as in M1 and the derivative captures the rate of decline (slope) in literacy. As the result, exp(α1) estimates the hazard ratio (HR) with every 1 %/year slower of decline in literacy. The estimates were derived by maximizing the joint likelihood function of the two submodels. Baseline characteristics Xi including age, sex, years of education and level of literacy were included in all the models. In sensitivity analyses, we added additional model terms to control for potential confounding due to chronic medical conditions, MMSE score, IADL disability, depressive symptoms and NART reading ability.
The analyses were done using SAS/STAT software, version 9.3 (SAS Institute, Cary, NC, USA) and the JM package for R, version 3.1.2(Rizopoulos, 2010). We applied a nominal α level of 0.05 to determine statistical significance.
RESULTS
A total of 799 participants were included in the primary analyses. The mean (standard deviation) baseline age was 81.7 years (SD=7.7), and 610 (76.4%) were females. The mean years of education was 15.3 (SD=3.0). At baseline, all participants were free of dementia, and 167 (20.9%) were diagnosed with MCI. On average, participants answered 67.8% (SD=14.5%) of the literacy questions correctly at baseline, with more correct answers on the financial literacy (mean=73.3%, SD=15.8%) than health literacy (mean=62.3%, SD=18.3%) questions (t=17.1, degrees of freedom=798, p<0.001). Age was correlated with financial and health literacy (Pearson correlations −0.25 and −0.30 respectively, ps<0.001), so was years of education (Pearson correlations 0.37 and 0.27 respectively, ps<0.001). Males showed better financial literacy than females (82.7% for males versus 70.4% for females, t=10.6, degrees of freedom=353.9, p<0.001) but no sex difference was found in health literacy. Consistent with a previous report(Han et al., 2015), we also found poorer baseline literacy in older persons with MCI, compared to those with no cognitive impairment (NCI). Specifically, the mean financial literacy score was 75.2% in NCIs versus 66.4% in MCIs (t=5.84, degrees of freedom=230.4, p<0.001), and the mean score for health literacy was 64.8% in NCIs versus 52.8% in MCIs (t=7.85, degrees of freedom=797, p<0.001). We observed a weak correlation between chronic medical conditions and health literacy (Spearman correlations 0.11, p=0.002), but there was no correlation with financial literacy (p=0.802). Higher MMSE score was correlated with higher financial and health literacy (Pearson correlations 0.29 and 0.40 respectively, ps<0.001), and higher NART reading ability was correlated with higher financial and health literacy (Spearman correlations 0.37 and 0.27 respectively, ps<0.001). On the other hand, participants with greater IADL disability had lower financial and health literacy (Spearman correlations −0.29 and −0.26 respectively, ps<0.001). There were also weak correlations between depressive symptoms and financial and health literacy (Spearman correlations −0.17 and −0.10 respectively, ps<0.005).
Longitudinal decline in literacy among older persons
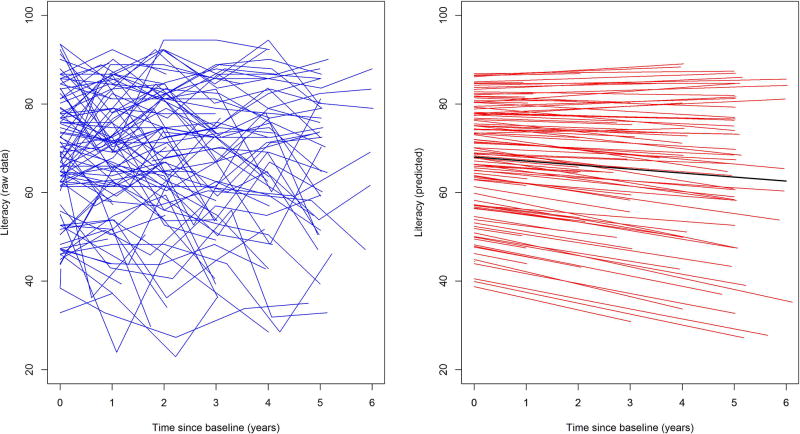
The participants in the study completed multiple years of literacy assessments (Median=4, Range=2–7). Figure 1 illustrates person-specific trajectories of total literacy over time. For a representative female participant of 80 years of baseline age and 15 years of education, the average annual rate of decline in total literacy was about 1 percent (Estimate=−0.919, standard error (SE)=0.117, p<0.001). A strong correlation was observed between the baseline literacy and the rate of decline such that subjects with higher score at baseline tended to have slower decline (p<0.001). Older age and female sex, but not education, were associated with faster decline in total literacy (Table 2). The result for health literacy was similar to that of total literacy. The rate of decline in financial literacy did not reach significance (p=0.056). In analyses restricted to participants with NCI at baseline, we also observed decline in total literacy (Table 2), which was largely driven by health literacy (p<0.001), not financial literacy (p=0.323).
Figure 1.
The spaghetti plots illustrate the person-specific trajectories of total literacy. The left panel shows the longitudinal total literacy scores over time for 100 randomly selected participants. The right panel shows the corresponding predicted decline (red) in same subjects and the predicted mean decline (black), estimated from a linear mixed model.
Table 2.
Baseline Level and Decline in Literacy among Community Dwelling Older Persons
| Non-demented at baseline (N=799) | |||
| Total literacy | Financial literacy | Health literacy | |
| Baseline level | 67.567 (0.491), <0.001 | 71.548 (0.536), <0.001 | 63.521 (0.626), <0.001 |
| Age | −0.540 (0.056), <0.001 | −0.471 (0.061), <0.001 | −0.611 (0.071), <0.001 |
| Male sex | 4.267 (1.011), <0.001 | 10.726 (1.104), <0.001 | −2.157 (1.290), 0.095 |
| Education | 1.452 (0.144), <0.001 | 1.429 (0.157), <0.001 | 1.474 (0.184), <0.001 |
| Rate of change | −0.919 (0.117), <0.001 | −0.238 (0.124), 0.056 | −1.407 (0.175), <0.001 |
| Age | −0.073 (0.014), <0.001 | −0.055 (0.015), <0.001 | −0.086 (0.022), <0.001 |
| Male sex | 0.629 (0.246), 0.011 | 0.251 (0.261), 0.337 | 1.019 (0.368), 0.006 |
| Education | −0.012 (0.036), 0.736 | −0.027 (0.038), 0.484 | 0.007 (0.054), 0.890 |
| No Cognitive impairment at baseline (N=632) | |||
| Total literacy | Financial literacy | Health literacy | |
| Baseline level | 69.145 (0.511), <0.001 | 72.981 (0.556), <0.001 | 65.297 (0.668), <0.001 |
| Age | −0.463 (0.058),<0.001 | −0.388 (0.063), <0.001 | −0.539 (0.076), <0.001 |
| Male sex | 4.278 (1.097), <0.001 | 10.798 (1.195), <0.001 | −2.288 (1.435), 0.111 |
| Education | 1.318 (0.153), <0.001 | 1.291 (0.167), <0.001 | 1.345 (0.201), <0.001 |
| Rate of change | −0.526 (0.128), <0.001 | 0.138 (0.140), 0.323 | −1.047 (0.194), <0.001 |
| Age | −0.069 (0.016), <0.001 | −0.053 (0.017), 0.002 | −0.080 (0.024), <0.001 |
| Male sex | 0.658 (0.284), 0.021 | 0.417 (0.310), 0.179 | 0.971 (0.431), 0.024 |
| Education | −0.005 (0.041), 0.907 | −0.030 (0.045), 0.499 | 0.035 (0.062), 0.573 |
Statistics presented in each cell are estimate (standard error), p values. Education was centered at 15 years and age was centered at 80 years.
Declining literacy and incident AD dementia and MCI
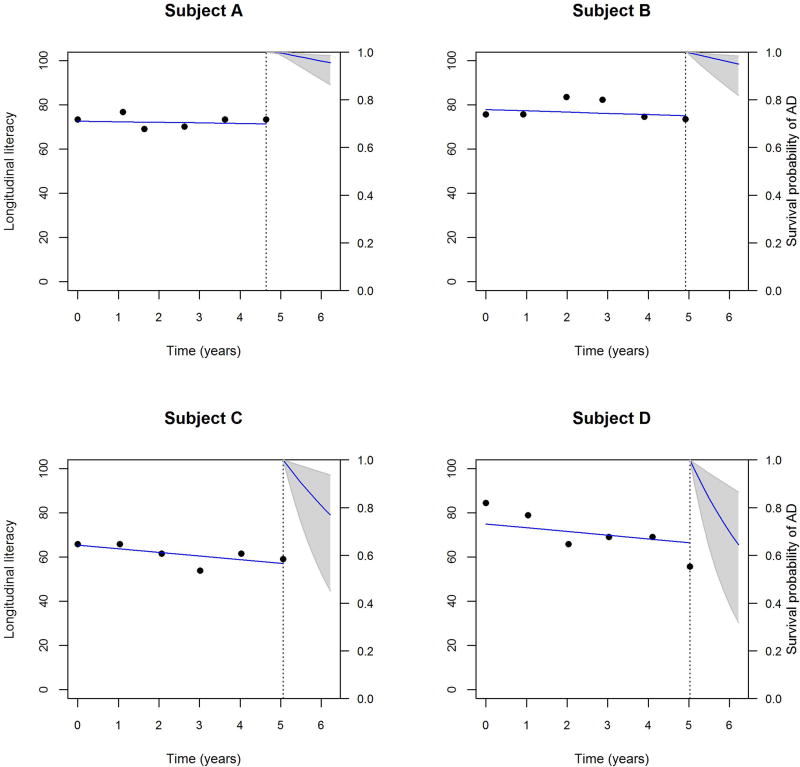
Over up to 6 years of follow-up, 94 (11.8%) participants developed AD dementia. Using the joint model, we observed that, after adjusting for age, sex, education and baseline literacy level, faster decline in total literacy was associated with a higher risk for incident AD dementia, such that with annual rate of decline in total literacy increased by 1% per year, the risk of developing incident AD dementia was increased by more than 4 fold (Hazard Ratio (HR) =4.526, 95% Confidence Intervals (CIs): 2.993–6.843, p<0.001). Since the mean decline in financial literacy didn’t reach statistical significance, we repeated our analysis only for health literacy. Similar to the result for total literacy, every 1% per year increase in the rate of health literacy decline increased the risk for incident AD dementia by more than 3 fold (HR=3.828, 95% CIs: 2.549–5.749, p<0.001). Figure 2 illustrates predicted conditional survival probabilities of AD for representative participants with different rates of decline in literacy. Notably, participants with faster decline were much more prone to develop incident AD dementia later.
Figure 2.
Predicted probabilities of not having incident AD for 4 representative individuals with various rates of decline in literacy. The vertical dotted lines represents the time in years of the last literacy assessment. To the left of the vertical lines are the longitudinal data (black dots) as well as fitted trajectories (blue lines) for change in literacy. To the right of these vertical lines are the mean predicted probabilities of not having incident AD diagnosis, conditional on the history of decline in literacy. Shaded area represents 95% confidence band.
Next, we investigated the association of change in literacy with incident MCI in analyses restricted to the 632 participants who were free of cognitive impairment at baseline; of those, 176 (27.8%) were diagnosed with MCI during the subsequent visits. Adjusting for age, sex, education, and baseline level of literacy, a faster rate of decline in total literacy was also associated with a higher risk for incident MCI (HR=2.971, 95% CIs: 1.509–5.849, p=0.002). The result was similar for the association of decline in health literacy with incident MCI (HR=2.397, 95% CIs: 1.603–3.585, p<0.001).
We performed several sensitivity analyses to assess the robustness of these findings. First, we examined potential confounding due to chronic medical conditions, MMSE score, IADL disability, depressive symptoms and NART reading ability. Additional terms corresponding to these confounders were added to the models, each separately. In these analyses, we observed that MMSE score, IADL disability and depressive symptoms were associated with the risk of AD dementia. In addition, MMSE score and IADL disability were also associated with incident MCI. Notably, however, the association of declining literacy persisted even after controlling for these covariates (e-Table 1 and 2). Further, considering that individuals who develop AD or MCI are likely to perform worse on the literacy measure, we conducted an additional analysis to ensure that our results were not driven by the literacy score at the time of clinical diagnosis. To do so, we excluded the last literacy measure from the models. The results were similar, suggesting that the core finding was not driven by the literacy performance at the time of diagnosis (e-Table 3).
DISCUSSION
In this study of almost 800 well characterized older persons without dementia, we show that longitudinal decline in domain specific literacy is associated with adverse cognitive outcomes. The study offers new insight into age-related changes in financial and health literacy among community-based older persons without dementia. To our knowledge, only one prior study examined change in literacy and this analysis was focused on health literacy. It reported that about 20% of participants 52 years of age and older showed a decrease in health literacy, and the odds of being a decliner were greater among older persons and those with cognitive decline(Lindsay C Kobayashi et al., 2015). Notably, however, these findings were based on only two waves of literacy data, leaving open the question as to how literacy actually declines with advancing age. One innovation of our study is that, by leveraging up to 7 annual assessments of financial and health literacy, we were able to quantify person specific rates of literacy decline in older persons who were not demented at baseline. We showed that there is an average decline in total literacy, and health literacy in particular. Further, these analyses revealed considerable heterogeneity in rates of change across subjects. About 20% of the participants in our analysis managed to maintain literacy (that is, showed no decline or even improvement), while others experienced decline in literacy over the years. It is noteworthy as well that, in our cohort, we observed an overall decline in literacy even among older persons without any cognitive impairment at baseline (no dementia or even MCI). The results provide additional information regarding the dynamic nature of literacy and suggest that literacy is not a trait but rather degrades over time and with advancing age.
The study shows that declining literacy in old age substantially increases the risk for AD dementia and MCI. It was previously reported that literacy (measured at a single timepoint) was related to the risk of AD dementia; however the mechanisms underlying such an association remain unknown. Two plausible hypotheses are that (1) poor literacy represents a very early manifestation of an underlying disease process and therefore is a harbinger of impending cognitive deficits, and (2) better literacy is related to health promoting behaviors which protects against cognitive impairment. Findings from this study on declining literacy and cognitive impairment lend support to the first hypothesis. It is now widely acknowledged that AD is the result of a sequence of pathophysiological events(Sperling et al., 2011) and that AD pathology accumulates slowly over years or even decades prior to the onset of overt clinical symptoms(Markesbery, 2010). Indeed, studies that include longitudinal assessment of cognition prior to dementia diagnosis provide objective evidence of the consequences of this unfolding disease process. Thus, while prior work examining the relation of literacy (measured at a single timepoint) with dementia was informative, the level of literacy performance at one time may be confounded by a variety of pre-existing factors such as education, occupation and other life experiences. In contrast, with these confounding factors being relatively stable in old age, we believe change in literacy serves as a more sensitive marker for progression of an age-related disease process. Thus, the relationship between literacy and AD is likely multifaceted. In the present results, both the baseline level of literacy and subsequent decline in literacy were associated with incident AD dementia, suggesting that the two measures may capture different aspects of this complex relationship. By demonstrating the relation of declining literacy with the onset of AD dementia and MCI, this study suggests that declining literacy reflects an emerging disease process and may signal impending cognitive impairment.
Finally, a focus on constructs that involve complex abilities extending beyond those measured via traditional cognitive tests may facilitate early detection of persons at high risk of dementia or cognitive impairment. For example, in prior work, we showed that literacy involves cognitive function, particularly executive function and episodic memory, as well as other personality-related factors(Patricia A Boyle et al., 2013). Complex constructs such as literacy, which involve multiple skills and abilities, may be particularly vulnerable to age-related disease processes. In keeping with this idea, we and others have reported that cognition and other abilities are related to decision making in old age and that even very subtle (subclinical) age-related changes in cognition are associated with poor decision making(P. A. Boyle et al., 2012; B. D. James, Boyle, Yu, Han, & Bennett, 2015). Thus, changes in these more complex behaviors may manifest years before onset of evident dementia or even mild cognitive impairment. Our findings demonstrate that declining literacy precedes the onset of AD dementia and even MCI. Importantly, although literacy may to some extent resemble an IADL, attainment and maintenance of literacy involves an active learning process that supports the acquisition, use and integration of domain-specific information and concepts. The construct of domain specific literacy extends well beyond what is typically assessed by standard IADL measures or more basic tests of cognitive function. Indeed, declining literacy remains associated with AD dementia and MCI after adjustment for MMSE score, reading ability and IADL disability. Our results suggest that domain specific literacy may be helpful in facilitating the early detection of adverse cognitive outcomes.
The impact of declining literacy on our ever-growing aging population goes beyond the adverse cognitive outcomes studied here. Older persons are faced with many complex decisions that are essential to maintaining independence and wellbeing, including financial decisions (e.g., retirement spending, social security distributions) and healthcare choices, and we have shown that domain specific literacy is an important determinant of decision making in late life(Bryan D James et al., 2012). Other research also has shown that older persons are less engaged in medical decision making and more likely to defer to their physicians(Levinson, Kao, Kuby, & Thisted, 2005), and declining literacy may be a factor in this passivity. Finally, declining literacy may also increase the risk of falling victim to financial and other forms of fraud. Supporting evidence from this cohort shows that older persons with lower financial and health literacy are more susceptible to scams(B. D. James, Boyle, & Bennett, 2014). More research is needed to fully determine the public health implications of low and declining literacy among older persons.
To our knowledge, this is the first study which integrates longitudinal financial and health literacy data with annual clinical diagnosis in a large group of well characterized community dwelling older persons to quantify change in literacy over many years and document its associations with subsequent incident AD and MCI. The instruments for literacy assessments and clinical diagnoses are well validated and have been adopted in a number of prior studies. Longitudinal assessments of literacy are essential to provide objective measurement of change over time. Limitations are also noted. The analytic data come from a voluntary cohort and the findings may not be generalizable to other older population. While we show that declining literacy precedes the onset of cognitive impairment, which potentially reflects the process where accumulation of neuropathology degrades literacy, future clinical pathologic studies are planned to elucidate impact of neuropathology on change in literacy.
CONCLUSIONS
This study investigated longitudinal change in literacy and tested the hypothesis that faster decline in literacy was associated with a higher risk of AD dementia and MCI. We observed an overall decline in literacy, which was largely driven by change in health literacy. Older persons with faster decline in literacy had a substantially higher risk of incident AD dementia. Declining literacy also was associated with incident MCI. The findings from this study suggest that literacy declines with advancing age and that declining literacy may serve as an early indicator of adverse cognitive outcomes.
Supplementary Material
Table 1.
Baseline characteristics of the study participants
| Age in Years | 81.7, 7.7 |
| Females (N, %) | 610, 76.4% |
| Education in Years | 15.3, 3.0 |
| MCI (N, %) | 167, 20.9% |
| MMSE (Median, IQR) | 29, 27–30 |
| Total literacy | 67.8, 14.5 |
| Financial literacy | 73.3, 15.8 |
| Health literacy | 62.3, 18.3 |
| Number of literacy assessments (Median, IQR) | 4, 3–6 |
| Number of chronic medical conditions (Median, IQR) | 1, 0–2 |
| IADL disability (Median, IQR) | 1, 0–2 |
| CES-D (Median, IQR) | 0, 0–1 |
| NART (Median, IQR) | 9, 7–10 |
Unless otherwise noted, means and standard deviations (SD) are presented.
IQR: Interquartile range; IADL: Instrumental activities of daily living; CES-D: Center for Epidemiologic Studies Depression scale; NART: National Adult Reading Test
Table 3.
Associations with Incident AD Dementia and MCI
| Incident AD dementia (N=799) | ||
| Age | −0.013 (0.027), 0.627 | −0.019 (0.033), 0.556 |
| Male sex | 1.228 (0.425), 0.004 | 1.465 (0.552), 0.008 |
| Education | −0.044 (0.060), 0.455 | −0.005 (0.071), 0.950 |
| Baseline total literacy | −0.022 (0.011), 0.037 | -- |
| Change in total literacy | −1.510 (0.211), <0.001 | -- |
| Baseline health literacy | -- | −0.025 (0.007), <0.001 |
| Change in health literacy | -- | −1.342 (0.208), <0.001 |
| Incident MCI (N=632) | ||
| Age | 0.022 (0.025), 0.381 | −0.021 (0.026), 0.416 |
| Male sex | 0.940 (0.405), 0.020 | 0.920 (0.425), 0.030 |
| Education | 0.007 (0.053), 0.893 | 0.030 (0.053), 0.575 |
| Baseline total literacy | −0.014 (0.012), 0.239 | -- |
| Change in total literacy | −1.089 (0.346), 0.002 | -- |
| Baseline health literacy | -- | −0.012 (0.005), 0.010 |
| Change in health literacy | -- | −0.874 (0.205), <0.001 |
Statistics presented in each cell are estimate of log hazard ratio (standard error), p values. The estimate refers to the log hazard ratio with every 1 %/year slower decline. A negative value for change in literacy means slower decline protects against risk for incident AD dementia or MCI.
MCI: Mild Cognitive Impairment
Acknowledgments
The authors thank the investigators and staff at the Rush Alzheimer’s Disease Center. Most importantly, the authors acknowledge the contribution of all the participants in the Rush Memory and Aging Project. To obtain data from the Rush Memory and Aging Project for research use, please visit RADC Research Resource Sharing Hub (www.radc.rush.edu).
FUNDING
This study is supported by the National Institute on Aging grants R01AG17917, R01AG34374, K23AG40625, and R01AG33678.
Footnotes
CONFLICT OF INTERESTS
The authors declare that there is no conflict of interests.
References
- Bailey SC, Fang G, Annis IE, O'Conor R, Paasche-Orlow MK, Wolf MS. Health literacy and 30-day hospital readmission after acute myocardial infarction. BMJ Open. 2015;5(6):e006975. doi: 10.1136/bmjopen-2014-006975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DW, Gazmararian JA, Sudano J, Patterson M. The association between age and health literacy among elderly persons. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2000;55(6):S368–S374. doi: 10.1093/geronb/55.6.s368. [DOI] [PubMed] [Google Scholar]
- Baker DW, Parker RM, Williams MV, Clark WS. Health literacy and the risk of hospital admission. J Gen Intern Med. 1998;13(12):791–798. doi: 10.1046/j.1525-1497.1998.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J. Health literacy and mortality among elderly persons. Arch Intern Med. 2007;167(14):1503–1509. doi: 10.1001/archinte.167.14.1503. [DOI] [PubMed] [Google Scholar]
- Bennett DA, Schneider JA, Bienias JL, Evans DA, Wilson RS. Mild cognitive impairment is related to Alzheimer disease pathology and cerebral infarctions. Neurology. 2005;64(5):834–841. doi: 10.1212/01.wnl.0000152982.47274.9e. [DOI] [PubMed] [Google Scholar]
- Bennett DA, Schneider JA, Buchman AS, Barnes LL, Boyle PA, Wilson RS. Overview and findings from the Rush Memory and Aging Project. Curr Alzheimer Res. 2012;9(6):646. doi: 10.2174/156720512801322663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett JS, Boyle PA, James BD, Bennett DA. Correlates of health and financial literacy in older adults without dementia. BMC Geriatr. 2012;12:30. doi: 10.1186/1471-2318-12-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle PA, Buchman AS, Wilson RS, Bienias JL, Bennett DA. Physical activity is associated with incident disability in community-based older persons. J Am Geriatr Soc. 2007;55(2):195–201. doi: 10.1111/j.1532-5415.2007.01038.x. [DOI] [PubMed] [Google Scholar]
- Boyle PA, Yu L, Wilson RS, Gamble K, Buchman AS, Bennett DA. Poor decision making is a consequence of cognitive decline among older persons without Alzheimer's disease or mild cognitive impairment. PLoS One. 2012;7(8):e43647. doi: 10.1371/journal.pone.0043647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle PA, Yu L, Wilson RS, Segawa E, Buchman AS, Bennett DA. Cognitive decline impairs financial and health literacy among community-based older persons without dementia. Psychol Aging. 2013;28(3):614. doi: 10.1037/a0033103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han SD, Boyle PA, James BD, Yu L, Bennett DA. Poorer Financial and Health Literacy Among Community-Dwelling Older Adults With Mild Cognitive Impairment. J Aging Health. 2015;27(6):1105–1117. doi: 10.1177/0898264315577780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han SD, Boyle PA, Yu L, Fleischman DA, Arfanakis K, Leurgans S, Bennett DA. Financial literacy is associated with medial brain region functional connectivity in old age. Arch Gerontol Geriatr. 2014;59(2):429–438. doi: 10.1016/j.archger.2014.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James BD, Boyle PA, Bennett DA. Correlates of susceptibility to scams in older adults without dementia. J Elder Abuse Negl. 2014;26(2):107–122. doi: 10.1080/08946566.2013.821809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James BD, Boyle PA, Bennett JS, Bennett DA. The impact of health and financial literacy on decision making in community-based older adults. Gerontology. 2012;58(6):531–539. doi: 10.1159/000339094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James BD, Boyle PA, Yu L, Han SD, Bennett DA. Cognitive decline is associated with risk aversion and temporal discounting in older adults without dementia. PLoS One. 2015;10(4):e0121900. doi: 10.1371/journal.pone.0121900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juster FT, Suzman R. An overview of the Health and Retirement Study. Journal of Human Resources. 1995:S7–S56. [Google Scholar]
- Kaup AR, Simonsick EM, Harris TB, Satterfield S, Metti AL, Ayonayon HN, Yaffe K. Older adults with limited literacy are at increased risk for likely dementia. J Gerontol A Biol Sci Med Sci. 2014;69(7):900–906. doi: 10.1093/gerona/glt176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi LC, Wardle J, Wolf MS, von Wagner C. Cognitive function and health literacy decline in a cohort of aging English adults. J Gen Intern Med. 2015:1–7. doi: 10.1007/s11606-015-3206-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi LC, Wardle J, Wolf MS, von Wagner C. Health Literacy and Moderate to Vigorous Physical Activity During Aging, 2004–2013. Am J Prev Med. 2016;51(4):463–472. doi: 10.1016/j.amepre.2016.02.034. [DOI] [PubMed] [Google Scholar]
- Kutner M, Greenburg E, Jin Y, Paulsen C. The Health Literacy of America's Adults: Results from the 2003 National Assessment of Adult Literacy. NCES 2006-483. National Center for Education Statistics 2006 [Google Scholar]
- Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making. A national study of public preferences. J Gen Intern Med. 2005;20(6):531–535. doi: 10.1111/j.1525-1497.2005.04101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lusardi A, Mitchell OS. Financial literacy and planning: Implications for retirement wellbeing: National Bureau of Economic Research 2011 [Google Scholar]
- Markesbery WR. Neuropathologic alterations in mild cognitive impairment: a review. J Alzheimers Dis. 2010;19(1):221–228. doi: 10.3233/JAD-2010-1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease Report of the NINCDS - ADRDA Work Group* under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984;34(7):939–939. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- Rizopoulos D. JM: An R package for the joint modelling of longitudinal and time-to-event data. Journal of Statistical Software. 2010;35(9):1–33. [Google Scholar]
- Rizopoulos D. Joint models for longitudinal and time-to-event data: With applications in R. CRC Press; 2012. [Google Scholar]
- Schneider J, Arvanitakis Z, Leurgans S, Bennett D. Neuropathology of probable AD and amnestic and non-amnestic MCI. Ann Neurol. 2009;66:200–208. doi: 10.1002/ana.21706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sperling RA, Aisen PS, Beckett LA, Bennett DA, Craft S, Fagan AM, Phelps CH. Toward defining the preclinical stages of Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7(3):280–292. doi: 10.1016/j.jalz.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson RS, Barnes LL, Mendes de Leon CF, Aggarwal NT, Schneider JS, Bach J, Bennett DA. Depressive symptoms, cognitive decline, and risk of AD in older persons. Neurology. 2002;59(3):364–370. doi: 10.1212/wnl.59.3.364. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Mendes De Leon CF, Barnes LL, Schneider JA, Bienias JL, Evans DA, Bennett DA. Participation in cognitively stimulating activities and risk of incident Alzheimer disease. JAMA. 2002;287(6):742–748. doi: 10.1001/jama.287.6.742. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Yu L, James BD, Bennett DA, Boyle PA. Association of financial and health literacy with cognitive health in old age. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn. 2017;24(2):186–197. doi: 10.1080/13825585.2016.1178210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf MS, Gazmararian JA, Baker DW. Health literacy and functional health status among older adults. Arch Intern Med. 2005;165(17):1946–1952. doi: 10.1001/archinte.165.17.1946. [DOI] [PubMed] [Google Scholar]
- Yu L, Wilson RS, Schneider JA, Bennett DA, Boyle PA. Financial and health literacy predict incident Alzheimer’s disease dementia and pathology. Journal of Alzheimer’s Disease. 2017 doi: 10.3233/JAD-161132. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.