Parents of seriously ill children reported hopes over time. The specific hopes and domains vary over time, although most hopes fell within 4 major areas.
Abstract
BACKGROUND:
Hopes of parents of children with serious illness play an important role in decision-making and coping. Little is known about how parent hopes change over time. We describe the changes in parent hopes across multiple domains and time intervals, examine hopes in a subgroup of parents whose child died, and explore the maintenance of domains over time.
METHODS:
In a mixed-methods prospective cohort study on decision-making, parents of seriously ill children reported demographic characteristics and hopes at baseline and reported any changes in hopes at 4-, 8-, 12-, 16-, and 20-month follow-up visits. Hopes were coded into 9 domains. Hope changes and domain changes were identified for each parent at each visit.
RESULTS:
One hundred and ninety-nine parents of 158 patients most often reported hopes in the domains of quality of life (75%), physical body (69%), future well-being (47%), and medical care (34%). Hope percentages increased over time for quality of life (84%), future well-being (64%), and broader meaning (21%). The hope domains reported by parents of children who died were similar to the rest of the sample. The majority of parents who completed 5 to 6 follow-up visits changed at least 1 domain. At the individual parent level, some domains revealed considerable change over time, whereas other domains were stable among a subset of parents.
CONCLUSIONS:
The specific hopes and overall areas of hope of parents of seriously ill children vary over time, although most hopes fall within 4 major areas. Accordingly, clinicians should regularly check with parents about their current hopes.
What’s Known on This Subject:
Cross-sectional studies have revealed that hopes of parents of children with serious illness play an important role in decision-making and coping. Understanding parent hopes can help clinicians support parents and collaborate with them in this difficult situation.
What This Study Adds:
The specific hopes and overall areas of hope of parents of seriously ill children are not static over time, although most hopes fall within 4 major areas. Accordingly, clinicians should regularly check with parents about their current hopes.
Parents of children with serious illness often confront daunting health care decisions.1,2 In such circumstances, parents base their decisions on multiple factors, including recommendations from doctors, personal beliefs about what a good parent ought to do, personal values, beliefs about the child’s most urgent problems, and their hopes for their child’s future.3–9 Parental hopes in particular play an important role in how parents cope with their child’s illness.10–12 Understanding parental hopes can help clinicians support parents and collaborate effectively with them in this difficult situation.
Most of what we know about parental hopes, however, is based on cross-sectional studies in which researchers have examined what kinds of hopes a parent is most likely to report and how much they agree with the other parent and the physician.8,9,12,13 We do know, on the basis of several qualitative and smaller quantitative studies, that parental hope priorities may change as parents gain more knowledge and expertise about their child’s illness.14 For example, parental hopes may become more concrete and short-term as a child’s condition worsens (eg, getting through each day) or more general and long-term as a child’s condition improves (eg, the child’s future life).15 A study of parents of children being treated for cancer revealed that over time, parents focused more on “being there” for the child (eg, being present during painful procedures) and advocating for the child instead of assuming that medical staff knew best (eg, insisting on anesthesia for a painful spinal tap).16 One study revealed that some parents were able to find new meaningful goals even as their child was dying.17 Finally, in a previously reported cohort study, we found that hopes reported by dyads of parents of seriously ill children at baseline and then 24 months later had often changed.18 Collectively, it is suggested in these studies that changes in hopes are occurring but without sufficient detail to understand more precisely what types of hopes are changing and when the change is occurring.
In the current study of 199 parents of 158 children, we (1) describe the changes in hopes across multiple domains and at a greater number of time intervals, providing a much higher resolution description of the changes of hopes over time; (2) examine hopes in a subgroup of parents whose child died; and (3) explore the maintenance versus new onset of hope domains over time.
Methods
Study Design and Participants
Participants were parents of seriously ill children in the Decision Making in Serious Pediatric Illness study, a mixed-methods prospective cohort study on parental decision-making for children with serious illness conducted at the Children’s Hospital of Philadelphia from September 2010 to December 2014. The hospital’s institutional review board approved the protocol for this study.
“Parents” were defined as the adults who had primary decision-making responsibilities for the index patient and included biological parents, adoptive or foster parents, and members of the extended family. Parents were eligible if they and their children met all of the following conditions: the child was a patient at Children’s Hospital of Philadelphia; the child had been admitted to the PICU, NICU, cardiac ICU, or had been referred to the pediatric advanced care team for palliative care services; the patient’s attending physician thought that the patient had a serious illness, and the parents would likely have to make a major medical decision in the next 12 to 24 months; the parents were responsible for medical decisions because of the age of the patient (<18 years old) or because the patient was cognitively impaired; and the parents spoke English. Parents were not eligible if they were deemed by the physician to be emotionally overwhelmed by the clinical situation, did not speak English, or had lost custody rights, or if the child had died, had been discharged, had experienced a nonaccidental injury, or (to accommodate the longitudinal design of the study) if the physician thought the child might die within a month or less. Parents consented to participate and were asked to complete a 1-hour interview at baseline and 20-minute interviews at 4, 8, 12, 16, and 20 months. Additional details about recruitment have been reported previously.6,18
Measures and Interviews
At study entry, parents reported demographic characteristics. All patients who met the criteria for the study had 1 or more complex chronic conditions, which were obtained from medical records. As part of the baseline interview, parents answered an open-ended question: “Please think of 3 major goals or hopes you have for your child.” The interviewer wrote down up to 3 hopes mentioned by each parent. At 4-, 8-, 12-, 16-, and 20-month follow-up visits, parents were reminded of the 3 hopes they had reported previously and were asked if there were any changes. Informed consent and baseline interviews took place in person at the hospital. Follow-up interviews were conducted either in person or by phone. Each parent was interviewed separately. One author (K.W.C.) and 1 research assistant conducted all interviews.
Coding Hope Domains, Hope Changes, and Domain Changes
We defined “hopes” as anything the parent stated in response to the open-ended question above, even if the hope was phrased in a negative way such as, “I really worry that he will suffer.” We used an emergent coding approach as recommended by Creswell19 to code hopes reported by parents into domains. We started with 9 domains and definitions that had been used successfully to categorize problems and hopes reported by parents of palliative care patients in previous studies.13,18 Three authors (K.W.C., P.G.N., and T.E.S.) coded a sample of the hopes, met to review their results, and updated the domain definitions to more clearly classify some hopes. The same 3 authors then coded all of the remaining hopes into the 9 domains using the updated definitions (see Table 1 for domain definitions). We coded each hope on the basis of what was specifically stated by the parent, not what might be implied or assumed to happen as a consequence of the stated hope. Some statements could be coded into multiple domains (see Table 2 for examples of how hopes were coded). Coders agreed on domains for 56% of the hopes coded (from the complete sample), after which they discussed and resolved all disagreements.
TABLE 1.
Hope Domain Definitions
| Domain | Definition |
|---|---|
| Miracle or cure | Cure, complete recovery, complete disappearance of the problem, or something that will lead to a cure. |
| Length of life | Length of life, staying alive, surviving, or making child’s life longer. |
| Physical body | General improvement or recovery (or general decline and/or worsening of condition). Specific sickness or problem with organ or part of body. Organ or part of the body getting better or healing. Physical ability hindered because of condition (walking, eating, sight, etc). |
| Medical care | Treatment plans, procedures, plan of care for child. Any logistical complication with medical care and support services being provided to the patient or family. Note that specific mentions of a treatment without any mention of the underlying condition, uncertainty, or other issues like quality of life will be coded only as medical care. Does not include unspecified “complications,” which may refer to child’s condition becoming more complicated as opposed to complications associated with treatment. |
| Medical knowledge | Doubts, concern, or uncertainty about whether treatment, procedure, or medical care is right for the child or whether treatment will be successful. Desire for more information about child’s condition, treatment, or care. Confidence or doubts about medical decisions. |
| Pain and suffering | Mentioning pain, suffering, the absence of pain and suffering, or explicit parts of child’s condition that causes them pain. Mentioning comfort alone is not enough to count as pain and suffering. |
| Quality of life | Strength of family ties, finding friends, making friends, fitting in with peers. Communication and social skills. Desire to not be in hospital, hope for discharge. Child’s ability to have fun and enjoy doing things. Child’s ability to manage on their own and lead a normal life. A goal for the child that affects child’s quality of life that does not fit into another domain (eg, reading a book, walking, feeding, eating). Desire for child to experience feelings such as happiness, contentedness, peace. Being able to attend school and learn. Desire for child to be comfortable. |
| Broader meaning | God or higher being and/or power. Fulfillment in life, rewarding life, learning something about life from experience of illness. Child’s self-identity and confidence. Advocating for child. |
| Future well-being | Broader concerns about future, including future health, development problems, achieving developmental milestones, and living a normal life. This domain does not include specific, practical hopes for the near future such as “that she’s off the trach in 2 weeks.” |
TABLE 2.
Examples of Hope Domain Coding From Current Sample
| Examples From Current Sample | Miracle or Cure | Length of Life | Physical Body | Medical Care | Medical Knowledge | Pain and Suffering | Quality of Life | Broader Meaning | Future Well-Being |
|---|---|---|---|---|---|---|---|---|---|
| “That all this will go away magically” | X | — | — | — | — | — | — | — | — |
| “That he survives” | — | X | — | — | — | — | — | — | — |
| “Starts to breathe normally” | — | — | X | — | — | — | — | — | — |
| “That she does well with this next heart surgery; for this surgery to fix the heart” | X | — | X | X | — | — | — | — | — |
| “Off oxygen at night” | — | — | — | X | — | — | — | — | — |
| “Find out what is going on and getting her well and/or pain free and leave the hospital” | — | — | X | — | X | X | X | — | — |
| “Making him feel loved” | — | — | — | — | — | — | X | — | — |
| “Grows up and understands everything; doesn’t feel left out because of medical issues” | — | — | — | — | — | — | X | X | X |
| “Successful and makes good choices in life” | — | — | — | — | — | — | — | X | X |
X, selected coding domain; —, not applicable.
We identified hopes in the data set that had changed in any way (eg, wording, punctuation, etc) compared with the hopes reported at the previous visit. Two authors (P.G.N. and D.L.H.) reviewed all differences to determine if the difference counted as a meaningful change. Slight changes in wording (eg, “Having a normal life” versus “Have a normal life”) or punctuation (eg, whether a period occurred at the end of a statement) were not considered changes, but adding a hope with new or different content was considered a change. The coders agreed on 93% of the cases and discussed and resolved all disagreements. We then identified 2 levels of hope change: any meaningful change at all (hope change) and a change in the broader topic or domain of the hope (domain change). For example, at baseline, a parent might report a specific hope about the child’s physical body or health (eg, “That he starts to breathe normally).” At the 4-month visit, the parent might report a hope that was different but still in the same broad domain of physical body or health (“heart function improves”). This would be identified as a hope change. The parent might, in contrast, report a hope in a completely different domain of quality of life (eg, “Making him feel loved”), which would be called a domain change.
We identified domain changes by comparing the domains coded for each visit by each parent. We recorded whether each domain was new as of a particular visit (ie, the parent had not reported hopes in that domain in the previous visit) or if a domain was no longer present (ie, the parent no longer reported any hopes in a domain when they had done so at the previous visit). For each parent, we counted the total number of domains gained or lost across all 3 hopes. Instances in which parents lost a domain on one hope but gained the domain on another hope were not counted as domain changes because the overall domains did not change.
In our analysis, we calculated the percentage of parents who endorsed each domain at each visit both for all parents and for parents of children who died. We calculated the total number of domains endorsed by each parent at each visit, with each parent having a potential maximum of 9 domains at each visit (because each hope could be coded into multiple domains, the potential maximum was determined by the number of domains). We calculated the number of domain changes for each parent at each visit. For the remaining analyses, because the number of parents who completed each visit varied, we used a subset of parents who had completed at least 5 of the 6 visits. For each domain, we calculated the percentage of parents who “maintained” the domain, meaning those specific parents who continued to endorse that domain at each follow-up interview they completed. We also calculated the cumulative percentage of parents who “gained” each domain. Parents were included in this percentage if they did not report a given domain at baseline and reported it at any future visit.
Results
Two hundred and ninety-five parents were approached. Ninety-five parents declined to participate, most often because they did not have time, were too stressed, were worried about confidentiality, or were not interested. A total of 200 parents of 158 patients participated in the study (see Table 3 for demographic characteristics of parents and patients). The sample size at each visit, the mean number of domains endorsed by parents, the number of parents with 5 to 6 visits total, and the number of parents who completed each visit and whose child later died during the study can be seen in Table 4. One hundred and ninety-nine parents (99%) reported at least 1 hope at the baseline visit (1 parent did not report any hopes at baseline), and 147 parents (74%) reported at least 1 hope at a follow-up visit. Over the follow-up visits, 125 parents (85%) experienced a hope change, and 121 parents (82%) experienced at least 1 domain change.
TABLE 3.
Demographic and Clinical Characteristics of 200 Parents and 158 Children at Baseline Interview
| n (%) | |
|---|---|
| Parents | |
| Mother | 136 (68) |
| Father | 60 (30) |
| Other | 4 (2) |
| Age, y | |
| 21–34 | 27 (64) |
| 35–38 | 5 (12) |
| 39–55 | 10 (24) |
| Race | |
| White | 161 (81) |
| African American | 22 (11) |
| Asian American | 2 (1) |
| Multiracial | 6 (3) |
| Other | 6 (3) |
| Did not answer | 3 (2) |
| Ethnicity | |
| Hispanic | 17 (9) |
| Non-Hispanic | 180 (90) |
| Did not answer | 3 (2) |
| Marital status | |
| Married and/or partnered | 171 (86) |
| Divorced or separated or widowed | 6 (3) |
| Single | 23 (12) |
| Education | |
| High school or less | 33 (17) |
| Some college or college graduate | 123 (62) |
| Some graduate school or graduate school | 44 (22) |
| Employment and financial | |
| Full-time employment | 99 (50) |
| Financial hardship | 91 (46) |
| Faith-based community | |
| Member of | 127 (64) |
| Active in | 116 (58) |
| Children | |
| Age, y | |
| ≤1 | 109 (69) |
| 1–4 | 17 (11) |
| 5–9 | 11 (7) |
| 10–17 | 21 (13) |
| Conditiona | |
| Metabolic | 17 (11) |
| Neuromuscular | 63 (40) |
| Malignancy | 15 (9) |
| Congenital | 111 (70) |
| Respiratory | 89 (56) |
| Cardiovascular | 77 (49) |
| Renal | 16 (10) |
| Other | 53 (34) |
Conditions are not mutually exclusive because a child can have multiple conditions. Therefore, the sum of the percentages adds up to more than 100%.
TABLE 4.
Sample Size at Each Visit, Mean Number of Domains, Number of Parents With 5–6 Visits, and Number of Parents Who Completed the Visit Whose Child Died During the Study
| Visit | No. Parents | Mean No. Domains | No. Parents With 5–6 Visits | No. Parents Whose Child Dieda |
|---|---|---|---|---|
| Baseline | 199 | 2.7 | 68 | 47 |
| 4 mo | 119 | 1.7 | 63 | 10 |
| 8 mo | 122 | 1.8 | 65 | 6 |
| 12 mo | 102 | 1.5 | 66 | 6 |
| 16 mo | 80 | 1.2 | 62 | 1 |
| 20 mo | 70 | 1.1 | 49 | 0 |
Although the majority of parents of children who died did not complete later visits because of the child’s death (eg, 36 parents did not complete the 4-mo visit because the child had died), in 1 case, a parent missed the 4- and 8-mo visits but completed the 12-mo visit before the child died.
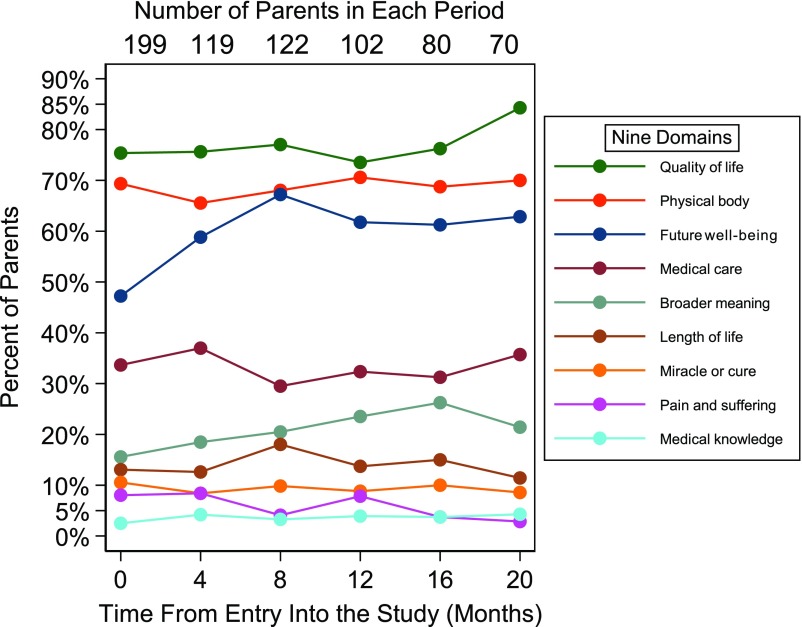
In this cohort, the prevalence of the 9 hope domains changed over time (Fig 1). At baseline, parents most often reported hopes in the domains of quality of life (75%), physical body (69%), future well-being (47%), and medical care (34%), with <20% of parents reporting hopes in each of the remaining domains. At 20 months, the percentage of parents reporting hopes was similar to baseline in the domains of physical body (70%), medical care (35%), length of life (11%), miracle or cure (9%), and medical knowledge (4%). In contrast, there was an increase in the percentage of parents reporting other domains, including quality of life (84%), future well-being (64%), and broader meaning (21%). The percentage of parents reporting hopes in the domain of pain and suffering decreased from 8% to 3%.
FIGURE 1.
All 199 parents with hopes at baseline.
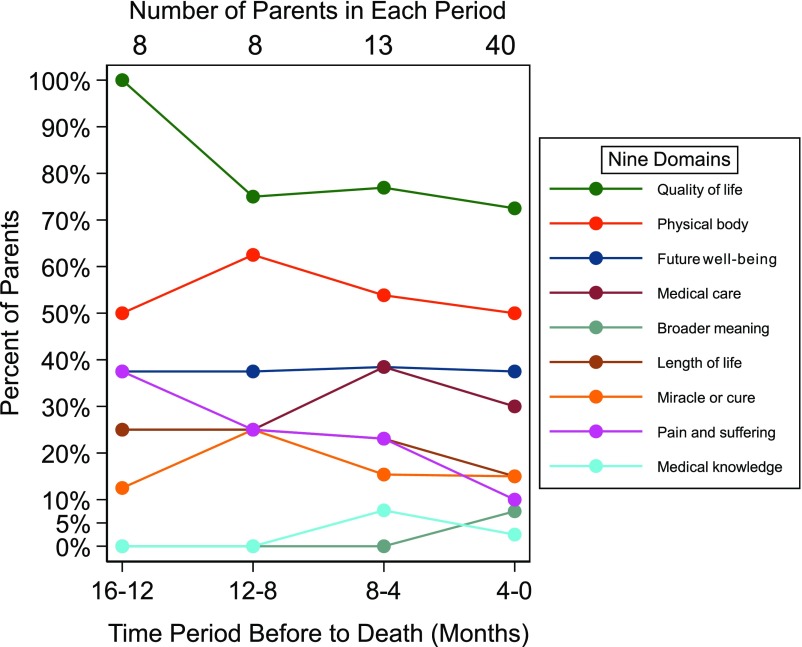
Of the 47 parents of children who died during the study, 10 completed the 4-month visit, 6 completed the 8- and 12-month visits, and 1 completed the 16-month visit (Fig 2). The order of the hope domains in terms of prevalence at 16 to 12 months before death was similar to the rest of the sample at baseline, other than physical body being somewhat less prevalent. The order of domain prevalence did not greatly change as the child’s death became imminent, although quality of life became less prevalent (from 100% to 77%) as did pain and suffering (from 38% to 10%) and length of life (from 25% to 15%).
FIGURE 2.
Parents of children who died during the study. n = 47 at baseline.
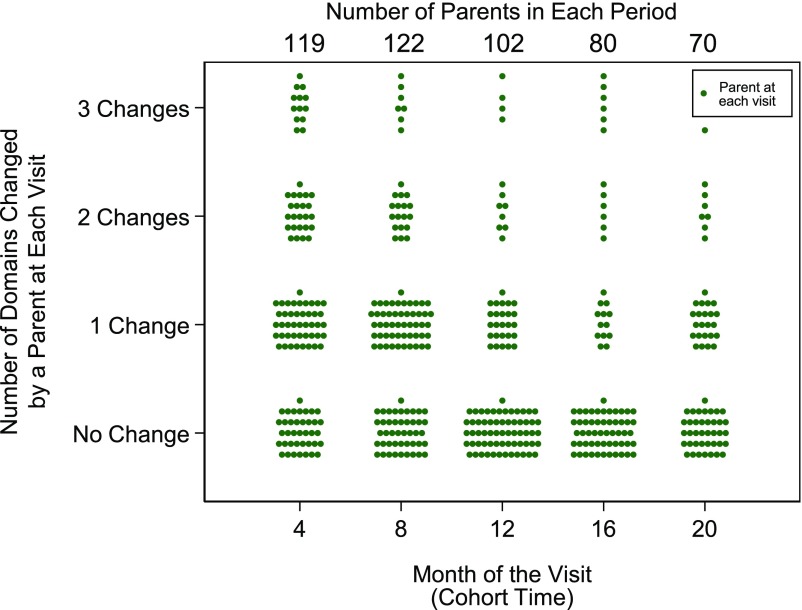
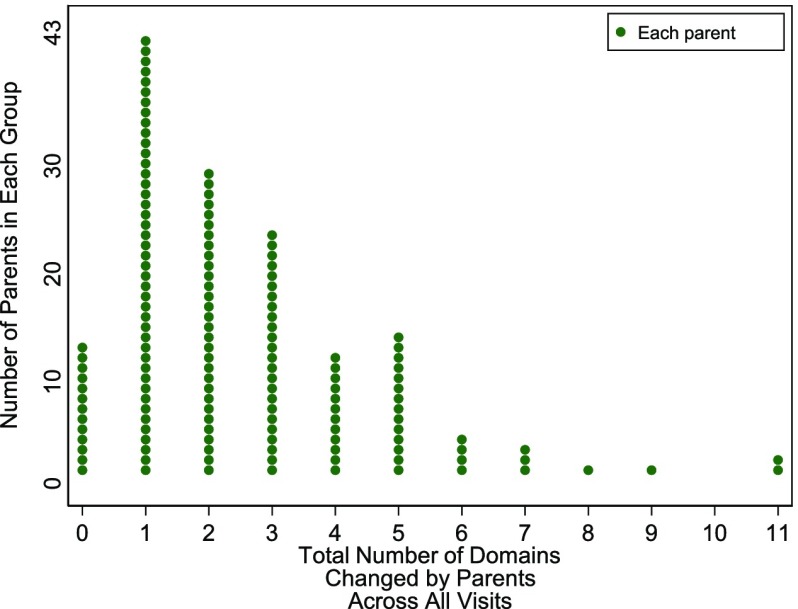
Many parents changed 1 or more domains at each visit, with a small number changing 2 or 3 domains (Fig 3). Over the course of the study, the majority of parents who completed at least 1 follow-up visit changed at least 1 domain, with a small number of parents changing more than 6 domains across visits (Fig 4).
FIGURE 3.
Number of domain changes at each visit among 199 parents who reported hopes.
FIGURE 4.
Total number of changes across all visits for 147 parents with follow-up visits.
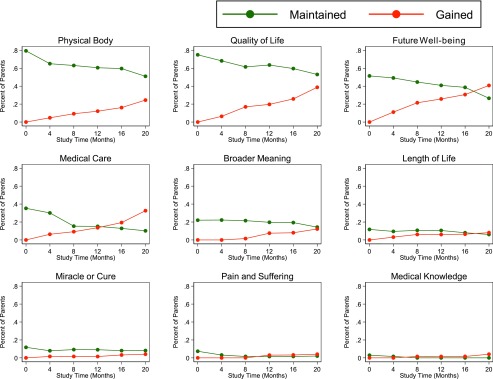
The 68 parents who completed 5 to 6 visits showed considerable change in domains over time, with only a subset of parents maintaining even the most prevalent domains across all visits and many parents gaining new domains at later visits (Fig 5). Less change over time was shown in some domains, however, including broader meaning, length of life, and miracle or cure, with a small percentage of parents maintaining these domains across the visits.
FIGURE 5.
Percent of parents who maintained or gained each domain at each visit among 68 parents who completed 5 to 6 visits.
Discussion
In this large cohort of parents of seriously ill children, the hopes they initially most often reported were about the child’s quality of life, physical health, future well-being, and medical care. Gradual changes over time were shown in the most prevalent domains, with parents dropping and gaining these domains at each visit. Despite these changes, quality of life, physical body, future well-being, and medical care were still the most prevalent domains for hopes 20 months later. Although at the individual level, change occurred more consistently: the majority of parents who completed follow-up visits changed at least 1 hope, and many of these changed hopes were in different topic areas than the initial hopes. Importantly, less change over time was shown in some low-prevalence domains (broader meaning, length of life, and miracle or cure), indicating that the small number of parents who endorsed these domains maintained hopes in these domains over most visits.
Surprisingly, among those parents whose children died during the study period, the hope domains reported were similar to parents of children who survived, although these parents of children who died reported hopes in the domain of physical body less often. Notably, the reported hope domains did not change meaningfully as the child’s death drew closer, suggesting that although parents of seriously ill children may change their hopes over time, these hopes do not change radically as the child comes within a few months to weeks of death.
Although the overall group-level prevalence of the hope domains did not change markedly over 20 months, parents showed considerable change at the individual level. Many parents changed 1 or more domains at any given visit, and the majority of parents who completed follow-up visits changed domains, with some parents changing domains a total of 11 times across visits.
These findings are consistent with previous research in which researchers showed that parents of sick children change their hopes over time because of changes in their child’s condition, knowledge and experience gained by parents, and parents learning new ways to think about the situation.14–18 With our study, we add to this literature by showing that although there is considerable change in the specific hopes reported by parents of sick children over time and some change in the broader topic or domain of these hopes, the most common topics of hopes over time continue to be the child’s quality of life, physical health, future well-being, and medical care. Additionally, we found that although fewer parents may discuss hopes about cures, finding meaning in their situation, and their child’s length of life, the parents that do raise these issues are likely to continue to be concerned about them over time.
These findings should be interpreted with the study’s strengths and limitations in mind. The large sample size (compared with previous studies) and employing a cohort design with multiple waves of data collection over a nearly 2-year period are strengths. Weakness include the attrition of parents over time, which reduced the sample size of this analysis. Parents who declined may have had different hopes than parents in the study. The subgroup of parents of children who died, although still larger than most previous studies, is small, with the majority completing only 1 visit, and thus the findings are less certain. Furthermore, all the parents came from 1 pediatric hospital, the racial composition of the study patients was disproportionately non-Hispanic white (similar to the population of Pennsylvania, which is 82.4% non-Hispanic white20), and most children were <1 year old, so the results may not be generalized to parents at other institutions, of different races, or with older children. The sample size precluded comparisons across diagnoses or patient age groups. In addition, hope domain coding was based on written summaries of each hope that the parent reported. In some cases, hopes were difficult to interpret because some hopes were broad and covered multiple domains (eg, “live a happy, normal life”), or the time frame for the hope was ambiguous. A low level of agreement between coders reveals the difficulties of coding responses to open-ended questions about hopes, and future projects may benefit from other research methods. Because longitudinal follow-up started with study entry and was not linked to a specific incident such as diagnosis or hospitalization, the trajectory of illness among the patients may have varied considerably. Diagnosis also varied considerably, and we were not able to explore whether parents of children with acute onset diseases had different hopes than parents of children with longstanding chronic conditions. We were also unable to differentiate between realistic hopes for a cure and unrealistic hopes for a miracle.
Overall, this study revealed that the specific hopes and overall areas of hope for parents of seriously ill children are not static over time, even if most hopes fall within 4 major areas. Accordingly, clinicians should regularly check with parents about their current hopes for their child to see if those hopes have changed, rather than assuming that they will remain static. A parent’s desire to advocate for their child can lead to mistrust and conflicts if medical staff are not able to communicate effectively with parents about how they are meeting the child’s needs as perceived by the parent and what the child’s future may look like.21,22 If clinicians are able to reassure parents that they are addressing the parents’ hopes, especially in the most common areas of hope, they will be able to build a stronger relationship with parents and provide more effective support for both parent and child.
Footnotes
Dr Hill helped develop coding criteria, helped resolve coder disagreements, conducted the final data analyses, and drafted the initial manuscript; Ms Nathanson helped develop coding criteria, coded parent interview data, and critically reviewed and revised the manuscript; Ms Carroll coordinated and supervised data collection, conducted parent interviews, helped develop coding criteria, coded parent interview data, and critically reviewed the manuscript; Mr Schall helped develop coding criteria, coded parent interview data, and critically reviewed the manuscript; Dr Miller conceptualized and designed the study, designed the study instruments, and critically reviewed the manuscript; Dr Feudtner obtained funding, conceptualized and designed the study, designed the study instruments, supervised data coding and data analyses, and critically reviewed the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by the National Institute of Nursing Research grant 1R01NR012026. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Mack JW, Wolfe J, Cook EF, Grier HE, Cleary PD, Weeks JC. Parents’ roles in decision making for children with cancer in the first year of cancer treatment. J Clin Oncol. 2011;29(15):2085–2090 [DOI] [PubMed] [Google Scholar]
- 2.Madrigal VN, Carroll KW, Hexem KR, Faerber JA, Morrison WE, Feudtner C. Parental decision-making preferences in the pediatric intensive care unit. Crit Care Med. 2012;40(10):2876–2882 [DOI] [PubMed] [Google Scholar]
- 3.Mack JW, Wolfe J, Grier HE, Cleary PD, Weeks JC. Communication about prognosis between parents and physicians of children with cancer: parent preferences and the impact of prognostic information. J Clin Oncol. 2006;24(33):5265–5270 [DOI] [PubMed] [Google Scholar]
- 4.Maurer SH, Hinds PS, Spunt SL, Furman WL, Kane JR, Baker JN. Decision making by parents of children with incurable cancer who opt for enrollment on a phase I trial compared with choosing a do not resuscitate/terminal care option. J Clin Oncol. 2010;28(20):3292–3298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hinds PS, Oakes LL, Hicks J, et al. “Trying to be a good parent” as defined by interviews with parents who made phase I, terminal care, and resuscitation decisions for their children. J Clin Oncol. 2009;27(35):5979–5985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Feudtner C, Walter JK, Faerber JA, et al. Good-parent beliefs of parents of seriously ill children. JAMA Pediatr. 2015;169(1):39–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hexem KR, Mollen CJ, Carroll K, Lanctot DA, Feudtner C. How parents of children receiving pediatric palliative care use religion, spirituality, or life philosophy in tough times. J Palliat Med. 2011;14(1):39–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tomlinson D, Bartels U, Hendershot E, Maloney AM, Ethier MC, Sung L. Factors affecting treatment choices in paediatric palliative care: comparing parents and health professionals. Eur J Cancer. 2011;47(14):2182–2187 [DOI] [PubMed] [Google Scholar]
- 9.Barrera M, Granek L, Shaheed J, et al. The tenacity and tenuousness of hope: parental experiences of hope when their child has a poor cancer prognosis. Cancer Nurs. 2013;36(5):408–416 [DOI] [PubMed] [Google Scholar]
- 10.Carroll KW, Mollen CJ, Aldridge S, Hexem KR, Feudtner C. Influences on decision making identified by parents of children receiving pediatric palliative care. AJOB Prim Res. 2012;3(1):1–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reder EA, Serwint JR. Until the last breath: exploring the concept of hope for parents and health care professionals during a child’s serious illness. Arch Pediatr Adolesc Med. 2009;163(7):653–657 [DOI] [PubMed] [Google Scholar]
- 12.Kylmä J, Juvakka T. Hope in parents of adolescents with cancer–factors endangering and engendering parental hope. Eur J Oncol Nurs. 2007;11(3):262–271 [DOI] [PubMed] [Google Scholar]
- 13.Hill DL, Miller VA, Hexem KR, et al. Problems and hopes perceived by mothers, fathers and physicians of children receiving palliative care. Health Expect. 2015;18(5):1052–1065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pyke-Grimm KA, Stewart JL, Kelly KP, Degner LF. Parents of children with cancer: factors influencing their treatment decision making roles. J Pediatr Nurs. 2006;21(5):350–361 [DOI] [PubMed] [Google Scholar]
- 15.Granek L, Barrera M, Shaheed J, et al. Trajectory of parental hope when a child has difficult-to-treat cancer: a prospective qualitative study. Psychooncology. 2013;22(11):2436–2444 [DOI] [PubMed] [Google Scholar]
- 16.Kars MC, Duijnstee MS, Pool A, van Delden JJ, Grypdonck MH. Being there: parenting the child with acute lymphoblastic leukaemia. J Clin Nurs. 2008;17(12):1553–1562 [DOI] [PubMed] [Google Scholar]
- 17.Kars MC, Grypdonck MH, Beishuizen A, Meijer-van den Bergh EM, van Delden JJ. Factors influencing parental readiness to let their child with cancer die. Pediatr Blood Cancer. 2010;54(7):1000–1008 [DOI] [PubMed] [Google Scholar]
- 18.Hill DL, Nathanson PG, Fenderson RM, Carroll KW, Feudtner C. Parental concordance regarding problems and hopes for seriously ill children: a two-year cohort study. J Pain Symptom Manage. 2017;53(5):911–918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Creswell JW. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. 4th ed. Thousand Oaks, CA: Sage Publications, Inc; 2014 [Google Scholar]
- 20.US Census Bureau QuickFacts Pennsylvania. 2016. Available at: https://www.census.gov/quickfacts/PA. Accessed November 9, 2017
- 21.Back AL, Arnold RM. Dealing with conflict in caring for the seriously ill: “it was just out of the question”. JAMA. 2005;293(11):1374–1381 [DOI] [PubMed] [Google Scholar]
- 22.Forbat L, Teuten B, Barclay S. Conflict escalation in paediatric services: findings from a qualitative study. Arch Dis Child. 2015;100(8):769–773 [DOI] [PMC free article] [PubMed] [Google Scholar]