This study evaluates the association between parental adverse experiences and resilience and coping difficulty after pediatric discharge.
Abstract
BACKGROUND AND OBJECTIVES:
Adults with a history of adverse childhood experiences (ACEs) (eg, abuse) have suboptimal health outcomes. Resilience may blunt this effect. The effect of parental ACEs (and resilience) on coping with challenges involving their children (eg, hospitalization) is unclear. We sought to quantify ACE and resilience scores for parents of hospitalized children and evaluate their associations to parental coping after discharge.
METHODS:
We conducted a prospective cohort study at a children’s hospital (August 2015–May 2016). Eligible participants were English-speaking parents of children hospitalized on the Hospital Medicine or Complex Services team. The ACE questionnaire measured the responding parent’s past adversity (ACE range: 0–10; ≥4 ACEs = high adversity). The Brief Resilience Scale (BRS) was used to measure their resilience (range: 1–5; higher is better). The primary outcome was measured by using the Post-Discharge Coping Difficulty Scale via a phone call 14 days post-discharge (range: 0–100; higher is worse). Associations were assessed by using multivariable linear regression, adjusting for parent- and patient-level covariates.
RESULTS:
A total of 671 (81% of eligible parents) responded. Respondents were primarily women (90%), employed (66%), and had at least a high school degree (65%); 60% of children were white, 54% were publicly insured. Sixty-four percent of parents reported ≥1 ACE; 19% had ≥4 ACEs. The mean Brief Resilience Scale score for parents was 3.95. In adjusted analyses, higher ACEs and lower resilience were significantly associated with more difficulty coping after discharge.
CONCLUSIONS:
More parental adversity and less resilience are associated with parental coping difficulties after discharge, representing potentially important levers for transition-focused interventions.
What’s Known on This Subject:
Adults who experience adversity during childhood have suboptimal health outcomes; this may be blunted by resilience. However, little is known about how parental adverse childhood experiences and resilience affect a parent’s ability to cope with their child’s hospitalization.
What This Study Adds:
Parents exposed to more adversity during their childhoods, and those with lower levels of resilience, are more likely to face coping difficulties after their child is discharged from the hospital. Adversity and resilience may be important levers for transition-focused interventions.
Adverse childhood experiences (ACEs) result in poor health outcomes during childhood and into adulthood.1,2 ACEs include child abuse, neglect, and exposure to parental depression or substance abuse.2 A dose-response relationship exists between an individual’s number of ACEs and adult onset of mental and physical illnesses, including depression and obesity.2 Although there are many complex mechanisms through which ACEs affect health, there is agreement that this relationship is mediated partially through physiologic stress pathways.1 Exposure to ACEs may result in a persistent upregulation of the body’s stress response, which is known as toxic stress when it causes lasting, detrimental physiologic changes.3 With evidence linking ACEs and toxic stress to adverse health outcomes for adults, and presuming downstream effects on their children, the American Academy of Pediatrics recently released a policy statement urging pediatricians to screen for ACEs among children.4 Screening for ACEs among parents has been more controversial because they are static measures. However, preliminary literature reveals that parental ACEs may serve as a marker for childhood adversity.5
Although having experienced ACEs is not modifiable, resilience is an adaptable ability to cope with and bounce back from stressors.6–8 Resilience is a complex interplay among genetics, temperament, knowledge, skills, past experiences, social supports, and societal resources.9 Resilience may mitigate ACEs’ negative effects and is modifiable.10 For example, the Early Intervention Foster Care Program, in which caregivers learn how to create a positive environment, has resulted in a reduction in parental stress and improvements in childhood behavior.9
Despite growing recognition of the importance of ACEs, toxic stress, and resilience to adult health, there is a limited understanding of how these complex parental factors affect parents’ children and families, particularly during vulnerable periods. A child’s hospitalization is one such vulnerable period.11–13 Parental ACEs and limited resilience may reduce the parent’s ability to manage or cope with their child’s posthospital needs.14 Difficulty coping postdischarge is associated with higher rates of readmission and emergency department visits.15 Thus, we sought to quantify ACE and resilience scores among parents of hospitalized children and investigate their association with parent’s ability to cope with stress in the 14 days after discharge.
Methods
Participants and Study Design
We conducted a prospective cohort study of parents of hospitalized children recruited from the Hospital-to-Home Outcomes (H2O) study. H2O is a prospective, single-center, randomized controlled trial designed to determine the effectiveness of a nurse-led transitional home visit on 30-day unplanned health care reuse. H2O was approved by the Cincinnati Children’s Hospital Medical Center Institutional Review Board.
Details of H2O recruitment and design have been described previously.16 Briefly, children were eligible for inclusion in H2O if they were admitted to our institution’s general Hospital Medicine Service or one of the Complex Services (Neurosurgery, Neurology, or Complex Hospital Medicine) teams. Patients were excluded if they were discharged to a residential facility, lived outside the home health care nurse service area, were eligible for skilled home health care services (eg, intravenous antibiotics), or if the participating parent was non-English speaking.16 Of note, children on one of the Complex Services teams were eligible if they did not require skilled nursing services after discharge; this would include children with chronic diseases such as epilepsy. Families enrolled in H2O were randomly assigned to receive either a single nurse home visit within 96 hours of discharge or the standard of care. For the analyses presented here, we focused on a subset of parents, ≥18 years of age, whose children were enrolled between August 2015 and May 2016.
Outcomes and Predictors
Our primary outcome was postdischarge parental coping, measured during a telephone call conducted 14 days after the hospital discharge. Coping was enumerated by using the Post-Discharge Coping Difficulty Scale (PDCDS), a measure of stress and recovery after hospitalization. It is a 10-item instrument with a score ranging from 0 to 100; higher scores represent more coping difficulties.15,17 Sample questions include “Since you have been home from the hospital, how stressful has your life been?” and “How much difficulty have you had with caring for your child?”18 Additional attributes assess factors including self-management, availability of supports, and confidence in management.15 Among parents of hospitalized children, higher PDCDS scores have been associated with health care service use postdischarge.15,17
Our primary predictors were parental ACEs and resilience. Parents were recruited close to discharge and after obtaining consent; research assistants facilitated completion of the ACE and Brief Resilience Scale (BRS) questionnaires. The widely-used ACE questionnaire has 10 items and results in scores that range from 0 to 10, representing a count of reported adverse experiences.2 Questions are used to assess previous exposures to challenges including substance abuse; physical, emotional, or sexual abuse; and/or mental health issues. We defined a parent with 0 ACEs as having low risk, a parent with 1 to 3 ACEs as having moderate risk, and a parent with 4 to 10 ACEs as having high risk. We defined these cut points a priori, given that a score ≥4 has been associated with multiple comorbidities in adult studies.19 The BRS is used to quantify a respondent’s resilience. It has been used in an inpatient setting, but not with parents of hospitalized children. Studies have revealed a positive correlation of the scale with optimism and social support, and in the inpatient setting, they have revealed a negative correlation with fatigue.7 The scale employs 6 items, each on a 5-point Likert scale; higher scores indicate higher resilience.7,20 Example statements include “I tend to bounce back quickly after hard times” and “It does not take me long to recover from a stressful event.” BRS responses are averaged yielding a final score ranging from 0 to 5; we treated this as a continuous variable. The BRS was completed as part of the inpatient face-to-face H2O questionnaire and was administered before the ACE questions. Given the sensitive nature of these questions, the ACE questionnaire was completed privately by the parent and then returned to the research assistant in a sealed envelope.
Covariates
Parent and child sociodemographic variables were also obtained during the H2O survey. Parental variables included age, sex, educational attainment, household income, employment status, and financial and social strain. Educational attainment was analyzed in 2 categories –(high school or less and more than high school) because most discharge instructions are written at a high school reading level.21 Parents reported their annual household income in the following categories: <$15 000, $15 000 to $29 999, $30 000 to $44 999, $45 000 to $59 999, $60 000 to $89 999, $90 000 to $119 999, and ≥$120 000. Employment was dichotomized as not employed and/or student versus any employment. Financial and social strain were assessed by using a series of previously described questions.22 These questions were used to assess, via self-report, a family’s ability to make ends meet; ability to pay the rent, mortgage, or utilities; need to move in with others because of finances; and ability to borrow money if needed, as well as home ownership and parental marital status. Strain questions were all dichotomous (yes or no, single or not single). A composite variable was then constructed, categorizing those reporting 0, 1 to 2, 3 to 4, and ≥5 strain items.23
Child variables included race, ethnicity, age, primary care access,24 payer, and admitting team. Race categories were white or Caucasian; black or African American; American Indian or Alaskan Native; Asian American or Pacific Islander; and other. Ethnicity categories were Hispanic or Latino, non-Hispanic or non-Latino, and unknown. Race and ethnicity were combined into a single variable, categorized as non-Hispanic white, non-Hispanic black or African American, and multiracial or Hispanic or other. Primary care access was assessed by using the access subscale to the Parent’s Perception of Primary Care, including assessment of a family’s ability to travel to their doctor, to see their doctor for routine or sick care, and to get help or advice on evenings or weekends. Scores range from 0 (no access) to 100 (perfect access).24 The payer was categorized as private or as public or self-pay. The admitting team was either Hospital Medicine or Complex Services.
Statistical Analysis
We described the distribution of outcome, predictors, and covariates. We compared sociodemographic characteristics of respondents and nonrespondents to the ACE screen by using the χ2 test for categorical variables or the t test or nonparametric alternative for continuous variables. We also examined the distribution of BRS scores by ACE categorization using the Kruskal-Wallis test. We then pursued modeling to assess for independent relationships between predictors and outcomes.
Given that there are no agreed-on cut points for PDCDS, we opted to analyze it as a continuous variable. We used linear regression to assess for associations between the independent variables of interest and PDCDS. To build our adjusted, multivariable model, we decided a priori to include race and/or ethnicity, primary care access, and strain. Other covariates were included in multivariable models if bivariate associations were significant at the P < .1 level. We also assessed an ACE by resilience interaction term because we hypothesized that the effect of parental ACEs on postdischarge coping would depend on the parents’ resilience. Regression assumptions were verified for final models, including assessment of normal distribution of model residuals and the absence of multicollinearity. All analyses were performed with Stata version 13 (StataCorp, College Station, TX).
Results
A total of 824 parent-child dyads were enrolled in H2O during the study period. Of these, we included 671 (81% of enrolled) parents who completed both ACE and BRS questionnaires. One parent for each hospitalized child completed both questionnaires (for data on respondents and nonrespondents, see Table 1). PDCDS was completed by 657 of the 671 parents at 14 days postdischarge. Included parents were primarily women, employed, and had more than a high school education; 11% reported ≥5 strain items (Table 1). There were significant demographic differences between respondents and nonrespondents in family income and child race and/or ethnicity, insurance, and hospital team.
TABLE 1.
Characteristics of Included Participants, Defined as Those Completing the ACE Questionnaire (n = 671) Compared With Those Not Completing the Questionnaire
| Participant Characteristic | Respondents (n = 671) | Nonrespondents (n = 147) | P |
|---|---|---|---|
| Patient demographics | |||
| Child race, no. (%) | .03 | ||
| White | 404 (61) | 71 (49) | |
| Black or African American | 183 (28) | 53 (37) | |
| Multiracial, Hispanic, or other | 74 (11) | 20 (14) | |
| Public insurance or self-pay, no. (%) | 362 (54) | 94 (62) | .03 |
| Primary service: Hospital Medicine, no. (%) | 594 (89) | 118 (80) | .01 |
| Primary-care access score, mean (SD) | 86.6 (18.9) | 88.8 (18.5) | .21 |
| Parent demographics | |||
| Caregiver age, y, mean (SD) | 32.9 (7.9) | 32.4 (8.4) | .54 |
| Caregiver, female sex, no. (%) | 602 (90) | 129 (88) | .49 |
| Education, no. (%) | .08 | ||
| High school or less | 232 (35) | 62 (42) | |
| Part- or full-time employment, no. (%) | 446 (66) | 99 (67) | .84 |
| Household income | .01 | ||
| <$15 000 | 134 (20) | 34 (23) | |
| $15 000–$29 999 | 111 (17) | 42 (29) | |
| $30 000–$44 999 | 90 (13) | 15 (10) | |
| $45 000–$59 999 | 77 (11) | 14 (10) | |
| $60 000–$89 999 | 101 (15) | 12 (8) | |
| $90 000–$119 999 | 62 (9) | 12 (8) | |
| ≥$120 000 | 95 (14) | 16 (11) | |
| Strain items, no. (%)a | .84 | ||
| 0 | 202 (30) | 39 (27) | |
| 1–2 | 240 (36) | 57 (39) | |
| 3–4 | 154 (23) | 34 (23) | |
| ≥5 | 75 (11) | 12 (12) |
χ2 tests were used for categorical variables; t tests were used for continuous variables.
Assessed difficulty making ends meet or paying rent, mortgage, or utilities; the need to move in with others because of finances; the ability to borrow money if needed; home ownership; and parental marital status.
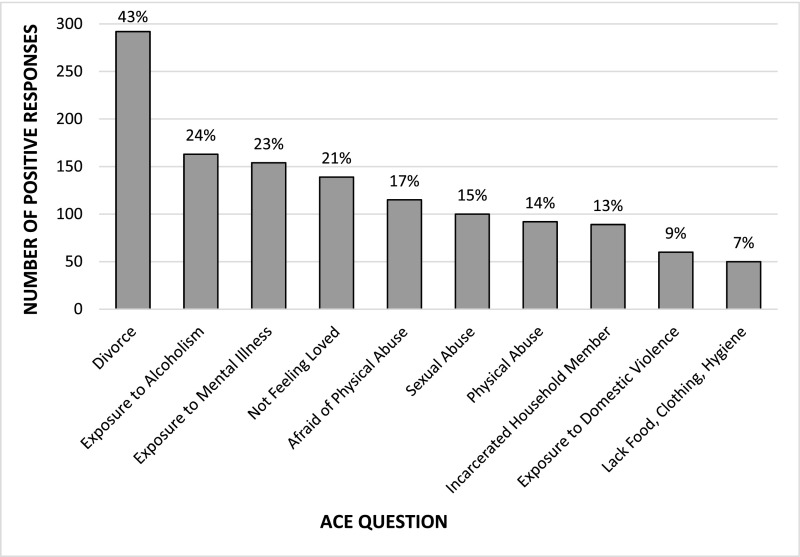
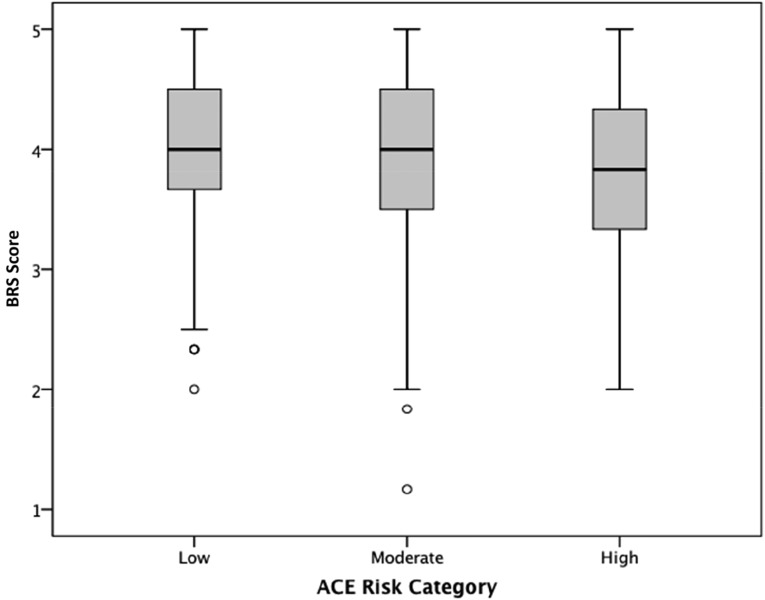
Sixty-four percent of parents reported ≥1 ACE (range: 0–9); 45% reported 1 to 3 ACEs, and 19% reported ≥4 ACEs. The most commonly reported ACEs included divorce (n = 292; 43%), exposure to alcoholism (n = 163; 24%), or to mental illness (n = 154; 23%; Fig 1). Parents had a mean BRS score of 3.95 (range: 1.00–5.00). Higher ACE scores were associated with lower BRS scores (P = .005). However, there was variability of resilience noted within each ACE category (Fig 2). Neither ACE nor BRS scores differed between those who did or did not receive the H2O study nurse home visit.
FIGURE 1.
The frequency of positive responses to each included ACE question posed in descending order (n = 671).
FIGURE 2.
Boxplots of BRS by ACE risk category. ACE categories include the following: low (0 ACEs), moderate (1–3 ACEs), and high (≥4 ACEs). With increasing ACE risk, the BRS median score decreases (Kruskal-Wallis P = .005).
PDCDS scores ranged from 0 (no difficulty coping) to 96 (high difficulty coping), with a median of 14.5 (interquartile range: 6.4–26.4). In bivariate analyses, higher ACE categories and lower resilience scores were associated with higher PDCDS scores (Table 2). There was also evidence of a dose-response relationship between the ACE risk category and increasing coping difficulty (moderate-risk β = 3.14; high-risk β = 5.73). Primary care access, insurance, education, employment, and hospital team met our significance threshold for inclusion in the multivariable model. The ACE by resilience interaction term was not significant. In the multivariable model, moderate (β = 2.76; 95% confidence interval [CI]: 0.18 to 5.33) and high risk (β = 5.18; 95% CI: 1.80 to 8.57) ACE categories remained significantly associated with worse postdischarge coping scores. In contrast, higher resilience was associated with better postdischarge coping (β = −4.25; 95% CI: −5.92 to −2.59). Surprisingly, public insurance and those not employed were associated with better postdischarge coping; patients admitted to a Complex Services team reported worse coping.
TABLE 2.
Association of Demographic Characteristics, Parental Strain, Parental ACEs, and Parental Resilience With Postdischarge Coping Difficulty
| Variable of Interest | Unadjusted β (95% CI) | Adjusteda β (95% CI) |
|---|---|---|
| Patient demographics | ||
| Child race | ||
| White | Reference | Reference |
| Black or African American | −2.66 (−5.39 to 0.08) | −1.83 (−4.86 to 1.20) |
| Multiracial, Hispanic, or other | −0.09 (−3.96 to 3.78) | 0.44 (−3.35 to 4.24) |
| Insurance | ||
| Private | Reference | Reference |
| Public | −2.62 (−4.99 to −0.25)* | −4.06 (−7.26 to −0.85)** |
| Service unit | ||
| Hospital Medicine | Reference | Reference |
| Complex Services | 7.01 (3.37 to 10.66)* | 7.35 (3.82 to 10.89)** |
| Primary-care access | −0.11 (−0.17 to −0.05)* | −0.06 (−0.13 to 0.003) |
| Parent demographics | ||
| Education | ||
| More than high school | Reference | Reference |
| High school or less | −2.43 (−4.92 to 0.06)* | −1.23 (−3.88 to 1.42) |
| Employment | ||
| Part- or full-time | Reference | Reference |
| Student or not employed | −4.31 (−6.80 to −1.81)* | −3.64 (−6.16 to −1.12)** |
| Parental strain itemsb | ||
| 0 | Reference | Reference |
| 1–2 | −2.13 (−5.04 to 0.79) | 0.27 (−2.98 to 3.52) |
| 3–4 | 1.09 (−2.18 to 4.37) | 3.54 (−0.52 to 7.59) |
| ≥5 | 1.06 (−3.06 to 5.18) | 2.41 (−2.42 to 7.25) |
| Parental ACE risk group | ||
| Low | Reference | Reference |
| Moderate | 3.14 (0.52 to 5.76)* | 2.76 (0.18 to 5.33)** |
| High | 5.73 (2.38 to 9.08)* | 5.18 (1.80 to 8.57)** |
| Parental resilience | ||
| BRS score | −4.17 (−5.79 to −2.55)* | −4.25 (−5.92 or −2.59)** |
Model adjusted for race and/or ethnicity, strain, primary-care access, insurance, education, employment, and service. A positive regression coefficient indicates worse coping difficulty (PDCDS range: 0–100).
Assessed difficulty making ends meet or paying rent, mortgage, or utilities; the need to move in with others because of finances; the ability to borrow money if needed; home ownership; and parental marital status.
Significant P < .10.
Significant P < .05.
Discussion
Childhood adversity is common in our cohort of parents of hospitalized children; more than 3 in 5 parents reported ≥1 ACE, and nearly 1 in 5 reported ≥4 ACEs, a score previously linked to poor health outcomes. That said, most parents considered themselves to be resilient. We found that higher ACE and lower resilience scores were associated with a parent’s coping ability in the 14 days after their child’s hospital discharge.
We found a higher prevalence of ACEs than that in the original ACE study.2 Within our sample, 19% reported ≥4 ACEs, whereas just 6.2% endorsed ≥4 ACEs in the original ACE sample.2, The difference in prevalence may be a reflection of differences in the sociodemographic characteristics of the 2 cohorts. It may also be that parents with more ACEs are more likely to have a child who is hospitalized. Despite the commonality of ACEs within our sample, we may be underestimating the true prevalence of ACEs, given that we excluded non-English speakers.
Although higher ACE scores correlated with less resilience, we found a wide range of resilience across each ACE grouping. One caregiver with an ACE score of 9 (very high) and BRS score of 5 (very high) wrote on their questionnaire, “Birth–18 is only a short period of time. I am a mentally/emotionally healthy adult. I love my life and wouldn’t change a thing.” Previous literature has suggested that in the face of adversity, some individuals may function at a higher level, otherwise known as “post-traumatic growth.”25 Our findings suggest that adversity likely complicates a parent’s coping ability, whereas resilience may help parents navigate postdischarge challenges.
The hospital-to-home transition is a vulnerable time; parents may be asked to do things for their children that are outside their comfort zone.11 We found that resilience was protective in postdischarge coping: with every 1-point increase on the resilience score, the PDCDS decreased by more than 4 points. Conversely, parents in the high-risk ACE group had more difficulty coping with a >5-point increase after discharge compared with parents in the low-risk ACE group. As such, resilience may help alleviate the negative effect of ACEs on postdischarge coping. Promoting coping by building resilience could be important because the authors of previous studies have highlighted that coping difficulty is associated with reuse.26
Parents have identified that hospitalizations and the transition home can be particularly stressful.11,13 Some have equated the surrounding stress with a fog, which limits one’s ability to process information and return to normal.11 One study demonstrated that parents of children hospitalized in an ICU who have had a history of stressors and psychological problems experienced more adjustment difficulty after discharge.27 We expected that we would find similar patterns with stressors related to socioeconomic factors. Interestingly, our data reveal that both the unemployed and publicly insured groups reported better coping than the employed and privately insured group. One explanation is that employed parents may be more stressed because of missing work; the privately insured group may have additional out-of-pocket costs. Alternatively, publicly insured and unemployed caregivers may have better coping if they are routinely accustomed to coping with the stresses of unemployment or lack of insurance. We suggest that an understanding of these factors may help identify parents who may have a more challenging transition home. Moreover, ACEs and resilience may be important levers for transition-focused interventions aimed at easing a difficult time for at-risk families.
Perhaps a more standard assessment of both parental ACEs and resilience should be considered in clinical settings to identify those at increased risk for postdischarge coping difficulties. Garner et al28 suggest that ACE screening should focus on parents and their ability to cope with their own past trauma. A recent report supported a 2-question ACE screen to reduce survey time, potentially making this assessment efficient.29 If the 2-question screener is equally effective in identifying families at risk for transition difficulties, the items could be incorporated into intake forms or history and physical documents. Our data also do not reveal if there is an advantage to screen for only ACEs or only resilience; it is likely that screening for both is important.
Addressing parental ACEs and resilience in the pediatric inpatient setting is novel, but feasibility is not understood. Barriers may include time, competing priorities (eg, medical acuity), and limited capacity to address positive responses. Our data reveal that risks are common within the pediatric setting; many parents report ACEs, along with financial and social strain. This breadth of risks highlights the broad needs of caregivers of hospitalized children. Another option may be to facilitate bidirectional communication of parental stressors between inpatient and outpatient providers. The authors of future studies should focus on utility and best methods for screening for adversity, as well as the effectiveness of interventions after screening, particularly in cases in which evidence remains limited.4 Inpatient supports may include providing more direct connections to hospital-based child life, psychologists, or pastoral care.14 Outpatient supports may include community health workers or care coordinators to follow-up with families in the postdischarge period. Clearly, there is ample room for further evaluation of how and where to both screen for risks and intervene on risks that are uncovered.30
Our study has several limitations. First, both adversity and resilience were assessed during hospitalization. Having a child hospitalized is likely stressful for any parent; that may have influenced how parents responded.14,31 Second, our cohort included parents of children hospitalized for both acute and chronic illnesses. Parents of children with chronic illnesses may cope differently from those with acute illnesses. We found that parents of children on one of the Complex Services teams had more coping difficulty than those on the Hospital Medicine team. The authors of future work should consider the distinction between these 2 populations. Third, the BRS tool measures one of the many constructs of resilience.7 We chose the BRS because it has previously been administered in an inpatient setting. We understand the BRS as a way to measure resilience that changes over time; however, if responders interpreted the items to be measuring a static trait, it may limit the scale’s effectiveness. Also, one of the PDCDS questions is used to assess the amount of stress one is facing; because stress is incorporated into the score, the tool may measure stress levels instead of coping. That said, postdischarge stress is inherently linked to discharge coping. Fourth, we collected household income in categories that included a range of incomes, generally in $15 000 increments. Thus, we are unable to calculate income with respect to household size. Similar income amounts may also mean different things to families or households of different sizes. Fifth, the demographic characteristics of our cohort limit the generalizability of our findings to other settings. Nonrespondents were more likely to have lower income and/or not have private insurance. This lower response rate may be due to limited trust with physicians,32 literacy, and/or fear of stigma. A small percentage of patients were ineligible for the study, given their limited English proficiency. This could potentially bias our results because limited English proficiency parents may have different ACE or resilience profiles. Finally, our population was limited to those recruited into a randomized controlled trial, which may introduce a sampling bias.
Conclusions
A parent’s history of adversity and their resilience may be integral to how they cope with a child’s hospitalization. Ultimately, identifying which families are at risk for difficulty coping after discharge may facilitate a targeted approach to deployment of hospital- and community-based resources that can be used to reduce the stress experienced during this challenging period.
Acknowledgments
The following H2O members are nonauthor contributors: Division of Hospital Medicine, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio: Kathleen Bell, BS, Allison Loechtenfeldt, BS, Angela M. Statile, MD, MEd, and Christine M. White, MD, MAT; Division of General and Community Pediatrics, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio; Division of Biostatistics and Epidemiology, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio: Jane C. Khoury, PhD, Colleen Mangeot, MS, and Pierce Kuhnell MS; Division of Social Services, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio; University of Dayton, College of Arts and Sciences, Dayton, Ohio; Division of Infectious Diseases, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio; James M. Anderson Center for Health Systems Excellence, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio: Heather L. Tubbs-Cooley, PhD; Home Care Services, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio: JoAnne Bachus, BSN, RN, CPN, Monica L. Borell, BSN, RN, CPN, Patricia Crawford, RN, CPN, Jennifer M. Gold, BSN, Judy A. Heilman, MSN, Karen Lawley, BSN, RN, CPN, Lynn O’Donnell, BSN, RN, CPN, Karen P. Sullivan, BSN, RN, CPN, Heather L. Tubbs-Cooley, PhD, Susan Wade-Murphy, MSN, and Margo Moore, BSN; Department of Economics, University of Cincinnati, Cincinnati, Ohio: Lenisa V. Chang, PhD; College of Nursing, The Ohio State University, Columbus, Ohio; Rita H. Pickler, PNP, PhD; Pediatric Telemedicine Analyst, Department of Pediatrics, University of California, Davis Health, Sacramento, California; Hadley S. Sauers-Ford, MPH; SNS Research, Cincinnati, Ohio; Susan N. Sherman, DPA; and Division of Hospital Medicine, University of Rochester Golisano Children’s Hospital, Rochester, New York: Lauren G. Solan, MD, Med.
We also thank David Keller, MD, for his guidance in the review of the article.
Glossary
- ACE
adverse childhood experience
- BRS
Brief Resilience Scale
- CI
confidence interval
- H2O
Hospital-to-Home Outcomes
- PDCDS
Post-Discharge Coping Difficulty Scale
Footnotes
Drs Shah, Beck, and Auger conceptualized and designed the study, conducted the statistical analyses, and drafted the initial manuscript; Ms Litman conceptualized and helped design the study; Dr Sucharew conducted the statistical analyses; Ms Haney and Mr Pfefferman collected data; Drs Simmons and Shah conceptualized and designed the study; and all authors reviewed and revised the manuscript, approved the final manuscript as submitted, and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by funds from the Academic Pediatric Young Investigator Award (Dr A. Shah) and the Patient-Centered Outcomes Research Institute Award (IHS-1306-0081, to Dr S Shah), the National Institutes of Health (1K23AI112916, to Dr Beck), and the Agency for Healthcare Research and Quality (K08-HS024735-01A1, to Dr Auger). All statements in this report, including findings and conclusions, are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute, its Board of Governors, or the Methodology Committee. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Shonkoff JP, Garner AS; Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics . The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1). Available at: www.pediatrics.org/cgi/content/full/129/1/e232 [DOI] [PubMed] [Google Scholar]
- 2.Felitti VJ, Anda RF, Nordenberg D, et al. . Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) study. Am J Prev Med. 1998;14(4):245–258 [DOI] [PubMed] [Google Scholar]
- 3.Johnson SB, Riley AW, Granger DA, Riis J. The science of early life toxic stress for pediatric practice and advocacy. Pediatrics. 2013;131(2):319–327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garner AS, Shonkoff JP; Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics . Early childhood adversity, toxic stress, and the role of the pediatrician: translating developmental science into lifelong health. Pediatrics. 2012;129(1). Available at: www.pediatrics.org/cgi/content/full/129/1/e224 [DOI] [PubMed] [Google Scholar]
- 5.Randell KA, O’Malley D, Dowd MD. Association of parental adverse childhood experiences and current child adversity. JAMA Pediatr. 2015;169(8):786–787 [DOI] [PubMed] [Google Scholar]
- 6.Windle G. What is resilience? A review and concept analysis. Rev Clin Gerontol. 2010;21(2):152–169 [Google Scholar]
- 7.Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15(3):194–200 [DOI] [PubMed] [Google Scholar]
- 8.Masten AS. Resilience in developing systems: the promise of integrated approaches. Eur J Dev Psychol. 2016;13(3):297–312 [Google Scholar]
- 9.Traub F, Boynton-Jarrett R. Modifiable resilience factors to childhood adversity for clinical pediatric practice. Pediatrics. 2017;139(5):e20162569. [DOI] [PubMed] [Google Scholar]
- 10.Bethell CD, Newacheck P, Hawes E, Halfon N. Adverse childhood experiences: assessing the impact on health and school engagement and the mitigating role of resilience. Health Aff (Millwood). 2014;33(12):2106–2115 [DOI] [PubMed] [Google Scholar]
- 11.Solan LG, Beck AF, Brunswick SA, et al. ; H2O Study Group . The family perspective on hospital to home transitions: a qualitative study. Pediatrics. 2015;136(6). Available at: www.pediatrics.org/cgi/content/full/136/6/e1539 [DOI] [PubMed] [Google Scholar]
- 12.Beck AF, Solan LG, Brunswick SA, et al. . Socioeconomic status influences the toll paediatric hospitalisations take on families: a qualitative study. BMJ Qual Saf. 2017;26(4):304–311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Snowdon AW, Kane DJ. Parental needs following the discharge of a hospitalized child. Pediatr Nurs. 1995;21(5):425–428 [PubMed] [Google Scholar]
- 14.Shah AN, Jerardi KE, Auger KA, Beck AF. Can hospitalization precipitate toxic stress? Pediatrics. 2016;137(5):e20160204. [DOI] [PubMed] [Google Scholar]
- 15.Weiss M, Johnson NL, Malin S, Jerofke T, Lang C, Sherburne E. Readiness for discharge in parents of hospitalized children. J Pediatr Nurs. 2008;23(4):282–295 [DOI] [PubMed] [Google Scholar]
- 16.Tubbs-Cooley HL, Pickler RH, Simmons JM, et al. ; H2O Study Group . Testing a post-discharge nurse-led transitional home visit in acute care pediatrics: the Hospital-To-Home Outcomes (H2O) study protocol. J Adv Nurs. 2016;72(4):915–925 [DOI] [PubMed] [Google Scholar]
- 17.Weiss ME, Sawin KJ, Gralton K, et al. . Discharge teaching, readiness for discharge, and post-discharge outcomes in parents of hospitalized children. J Pediatr Nurs. 2017;34:58–64 [DOI] [PubMed] [Google Scholar]
- 18.Fitzgerald Miller J, Piacentine LB, Weiss M. Coping difficulties after hospitalization. Clin Nurs Res. 2008;17(4):278–296 [DOI] [PubMed] [Google Scholar]
- 19.Felitti VJ. The relationship of adverse childhood experiences to adult health: turning gold into lead [in German]. Z Psychosom Med Psychother. 2002;48(4):359–369 [DOI] [PubMed] [Google Scholar]
- 20.O’Malley DM, Randell KA, Dowd MD. Family adversity and resilience measures in pediatric acute care settings. Public Health Nurs. 2016;33(1):3–10 [DOI] [PubMed] [Google Scholar]
- 21.Baker DW, Parker RM, Williams MV, Clark WS. Health literacy and the risk of hospital admission. J Gen Intern Med. 1998;13(12):791–798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Auger KA, Mueller EL, Weinberg SH, et al. . A validated method for identifying unplanned pediatric readmission. J Pediatr. 2016;170:105–12.e1, 2 [DOI] [PubMed] [Google Scholar]
- 23.Auger KA, Kahn RS, Davis MM, Simmons JM. Pediatric asthma readmission: asthma knowledge is not enough? J Pediatr. 2015;166(1):101–108 [DOI] [PubMed] [Google Scholar]
- 24.Seid M, Varni JW, Bermudez LO, et al. . Parents’ perceptions of primary care: measuring parents’ experiences of pediatric primary care quality. Pediatrics. 2001;108(2):264–270 [DOI] [PubMed] [Google Scholar]
- 25.Colville G, Cream P. Post-traumatic growth in parents after a child’s admission to intensive care: maybe Nietzsche was right? Intensive Care Med. 2009;35(5):919–923 [DOI] [PubMed] [Google Scholar]
- 26.LaManna JB, Bushy A, Norris AE, Chase SK. Early and intermediate hospital-to-home transition outcomes of older adults diagnosed with diabetes. Diabetes Educ. 2016;42(1):72–86 [DOI] [PubMed] [Google Scholar]
- 27.Bronner MB, Peek N, Knoester H, Bos AP, Last BF, Grootenhuis MA. Course and predictors of posttraumatic stress disorder in parents after pediatric intensive care treatment of their child. J Pediatr Psychol. 2010;35(9):966–974 [DOI] [PubMed] [Google Scholar]
- 28.Garner AS, Forkey H, Szilagyi M. Translating developmental science to address childhood adversity. Acad Pediatr. 2015;15(5):493–502 [DOI] [PubMed] [Google Scholar]
- 29.Wade R Jr, Becker BD, Bevans KB, Ford DC, Forrest CB. Development and evaluation of a short adverse childhood experiences measure. Am J Prev Med. 2017;52(2):163–172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Beck AF, Klein MD. Moving from social risk assessment and identification to intervention and treatment. Acad Pediatr. 2016;16(2):97–98 [DOI] [PubMed] [Google Scholar]
- 31.Cohen E, Horváth-Puhó E, Ray JG, et al. . Association between the birth of an infant with major congenital anomalies and subsequent risk of mortality in their mothers. JAMA. 2016;316(23):2515–2524 [DOI] [PubMed] [Google Scholar]
- 32.Ross S, Grant A, Counsell C, Gillespie W, Russell I, Prescott R. Barriers to participation in randomised controlled trials: a systematic review. J Clin Epidemiol. 1999;52(12):1143–1156 [DOI] [PubMed] [Google Scholar]