In 4594 children with family homelessness, elevated emotional health risks were mitigated by developmental assets but not to the same extent as for nonhomeless youth.
Abstract
BACKGROUND AND OBJECTIVES:
Youth who are homeless with adult family members comprise 37% of the US homeless population, yet mental health among this group has not yet been well described. We aimed to compare the risk of suicidality, and factors that may protect against it, between family-homeless and nonhomeless youth.
METHODS:
We used cross-sectional data, representing 62 034 eighth- to 12th-graders, to estimate the adjusted odds ratio (aOR) of emotional distress, self-injury, suicidal ideation, and attempted suicide in the past 12 months for youth who experienced family homelessness in the past 12 months compared with housed youth, controlling for covariates. We then tested whether developmental assets moderated these outcomes.
RESULTS:
Four percent (n = 4594) of youth (mean age 14.9 years) were homeless with an adult family member. Among these, 29.1% (n = 1317; aOR: 2.52, 95% confidence interval [CI] 2.34–2.69) reported self-injury, 21% (n = 940; aOR: 2.30, 95% CI: 2.14–2.48) reported suicidal ideation, and 9.3% (n = 416; aOR: 3.24, 95% CI: 2.91–3.60) reported suicide attempts. Developmental assets decreased the odds of these outcomes for all youth but were less protective for homeless youth.
CONCLUSIONS:
Youth experiencing recent family homelessness are at higher risk of suicidality than their nonhomeless peers, suggesting homelessness itself as a marker of risk. Factors that protect emotional health are less impactful among youth experiencing recent family homelessness. Thus, interventions among homeless youth may need to address social determinants of health such as stable housing and adversity in addition to developmental assets.
What’s Known on This Subject:
Youth who are homeless are at risk for problems with health and behavior, but no studies have compared the risk of suicide or risk and protective factors for emotional health between youth in family-homeless and family-housed contexts.
What This Study Adds:
The risk of suicide and other emotional health problems is increased among youth who have experienced family homelessness, and though developmental assets reduce this risk, they are less protective than for housed youth.
In 2013, nearly 2.5 million youth were homeless in the United States. These youth are at an increased risk of physical and mental health problems.1 Overwhelming negative experiences that are associated with homelessness in early childhood can threaten brain development, learning, and lifelong health.2 We know less about outcomes for older youth who are homeless with their families, despite there being evidence about negative outcomes in unaccompanied homeless adolescents. For example, although suicide is the second leading cause of death among people aged 10 to 24 years in the United States,3 it is the leading cause of death among unaccompanied homeless youth.4 These youth also have a lifetime prevalence of major depression that is almost twofold the prevalence among housed youth.5 Although mental health and suicide are highly prevalent among unaccompanied homeless and runaway youth, less is known about youth who are homeless with their families.
Children in families that are homeless are a distinct subgroup of homeless individuals, differing in many ways from unaccompanied youth as well as single adults.6,7 Family-homeless youth constitute 37% of the overall homeless population8 and make up the fastest-growing group of homeless persons in the United States.9 However, this population is often overlooked in terms of research and intervention. Authors of a recent systemic review found that there are currently no evidence-based programs or practices to address family homelessness and its consequences (eg, whether providing stable housing, positive family supports, and/or trauma-informed mental health services influences child outcomes for the better).10 One way to better meet the needs of families and youth experiencing homelessness is to understand which factors influence which risks in this population compared with housed youth to best target and tailor future intervention efforts.
Factors that positively influence behavior and development can mitigate negative emotional health outcomes in high-risk children, including those who have experienced family homelessness.6 We do not yet know how these so-called developmental assets11 (such as social competency, self-esteem, school connectedness, empowerment, parent connectedness, and academic orientation) impact emotional health outcomes for youth who have experienced family homelessness compared with those who have not.
We aimed to characterize the risk of emotional distress and suicidality among youth affected by family homelessness. We hypothesized that these negative outcomes would be more common in the context of family homelessness compared with nonhomelessness, controlling for sociodemographic covariates, and that developmental assets would be more protective for homeless youth than housed youth.
Methods
Study Design and Subjects
Data came from the 2013 Minnesota Student Survey (MSS), a statewide survey of 113 197 fifth, eighth, ninth and 11th graders attending Minnesota public schools (exclusive of students in juvenile detention centers and alternative learning centers). All public school districts were invited to take part; 280 out of 334 districts in the state participated (84%). Parents were notified of the survey administration and could decline consent to participate; most youth participated but actual response rates are not kept. The data collection was anonymous. Additional details about MSS administration and data-validation procedures are discussed elsewhere.12–14 Fifth graders were not asked about their housing status and were excluded from the analysis. The remaining sample included 62 034 students from eighth, ninth, and 11th grades. The University of Minnesota Institutional Review Board determined that this analysis was exempt from review because of the use of existing anonymous data.
Measures
Family Homelessness
We classified recent family homelessness among based on adolescents’ responses to the following dichotomous question: “During the past 12 months, have you stayed in a shelter, somewhere not intended as a place to live, or someone else’s home because you had no other place to stay?” Youth who answered “Yes, I was with my parents or an adult family member” were categorized as having experienced family homelessness15 (for the purposes of this study and its hypotheses, youth who answered “Yes, I was on my own without any adult family” were excluded from analyses).
Emotional Distress
The MSS included the Global Appraisal of Individual Needs–Short Screener (GAIN-SS),16 which consists 5 items (range 0–5; α = .80; eg, “During the last 12 months, have you had significant problems with feeling very trapped, lonely, sad, blue, depressed or hopeless about the future?”) to assess the risk of emotional-behavioral problems. Higher scores on the GAIN-SS reflect a greater risk of internalizing disorders in need of formal assessment and intervention. A score of 3 or more was defined as a “high level of emotional distress” as recommended by the GAIN-SS developers.16
Self-Harm and Suicidality
Youth who reported ever doing something to purposefully hurt or injure themselves without wanting to die, such as cutting, burning, or bruising themselves on purpose in past 12 months, were categorized as engaging in self-injurious behaviors (SIBs) (in response to “During the last 12 months, how many times did you do something to purposely hurt or injure yourself without wanting to die, such as cutting, burning, or bruising yourself on purpose? 0 times, 3 to 5 times, 6 to 9 times, 1 or 2 times, 10 to 19 times, or 20 or more times.” This variable was dichotomized to 0 times versus 1 or more because of a non-normal distribution highly skewed toward 0 times). Students who reported seriously considering suicide in the past year (a frame of time chosen to overlap with the question about family homelessness within the past year) were categorized as having suicide ideation (in response to “Have you ever seriously considered attempting suicide? Mark all that apply: No, or Yes during the last year, or Yes over a year ago”). Youth who reported actually attempting suicide in the past year were categorized as having made a suicide attempt (in response to “Have you ever actually attempted suicide? Mark all that apply: No, or Yes during the last year, or Yes over a year ago”).
Developmental Assets
The MSS included the following 3 subscales from the Developmental Assets Profile, which is a validated measure of child and adolescent internal strengths and external resources17: positive identity (8 items; α = .82; eg, “I feel in control of my life and future”), social competency (6 items; α = .84; eg, “I express my feelings in proper ways”), and empowerment (3 items; e.α = .81; eg, “I feel valued and appreciated by others”). The questions used a 4-point scale with responses ranging from “not at all or rarely” to “extremely or almost always.” Youth who answered fewer than 5 items for positive identity, 6 items for social competency, and 2 items for empowerment were excluded from the analyses. Academic orientation was measured as a mean of 3 items (range 1–4; α = .60; eg, “How often do you care about doing well at school?”). These questions used a 4-point scale with responses ranging from “none of the time” to “all of the time.” Positive teacher connectedness was measured as the mean of 4 items18 (range 1–4; α = .84; eg, “Most teachers at my school are interested in me as a person”). These questions used a 4-point scale with responses ranging from “strongly disagree” to “strongly agree.” Youth who answered fewer than 3 of these items were excluded from analyses. Finally, we used a dichotomous measure of parent connectedness using responses from 2 items19 that asked youth whether they can talk about their problems with their father and/or mother. Students who responded “yes, most of the time” or “yes, some of the time” to either of these questions were categorized as having high connectedness with their parent(s) (responses of “my father and/or mother is not around” were categorized as low connectedness).
Additionally, we measured multiple sociodemographic variables that have well-established associations with housing status and/or emotional health. Binary variables for sex (male or female) and grade (eighth, ninth, or 11th) were based on student report. Race and/or ethnicity groups were defined as Hispanic, non-Hispanic white, black or African or African American, Asian American or Pacific Islander, American Indian, multiple races, and other. We included receipt of free or reduced-price lunch at school as a binary marker for poverty status. Finally, a binary variable for location of the school delineated the 7-county Minneapolis, St. Paul metropolitan area versus all other nonmetropolitan and rural areas of Minnesota.
Statistical Analysis
χ2 and t test analyses compared sample characteristics by housing status. Separate logistic regression models tested hypotheses regarding associations between housing status and each emotional health outcome, using confidence intervals (CIs) to estimate statistical significance (ie, 95% CIs were statistically significant if they did not include 1.0). First, unadjusted models tested main effects; then, fully adjusted models controlled for covariates (age, sex, race and/or ethnicity, poverty, and school location); finally, models stratified by housing status estimated the odds of each emotional health outcome according to the levels of each developmental asset. Given sex-based differences in levels of assets and outcomes in prespecified analyses, models adjusted for age, race and/or ethnicity, poverty, and location were also sex-stratified in a post hoc analysis. Analyses were conducted by using SAS 9.2 (SAS Institute, Inc, Cary, NC).
Results
Prevalence of Family Homelessness
The mean age of the sample was 14.9 years (SD 1.34). The prevalence of family homelessness was 4.1% (Table 1). Homeless youth were more likely to be boys (54.9% vs 49.1%, P < .001), youth of color (40.7% vs 24%, P < .001), receiving free school lunch (45.5% vs 24.8%, P < .001), and located in nonmetropolitan or rural Minnesota (49.5% vs 48.2%, P < .001) than nonhomeless youth. The prevalence of family homelessness decreased by grade (42.6% in eighth grade versus 21.22% in 11th grade).
TABLE 1.
Sample Characteristics
| Demographics | Family-Homeless Adolescents | Nonhomeless Adolescents | P | aORa (95% CI) |
|---|---|---|---|---|
| n (%) | 4594 (4.1) | 108 603 (95.9) | <.0001 | — |
| Sex, n (%) | <.0001 | |||
| Male | 2522 (54.9) | 53 307 (49.1) | — | |
| Female | 2072 (45.1) | 55 296 (50.9) | — | |
| Grade, n (%) | <.0001 | |||
| 8 | 1956 (42.6) | 37 681 (34.70) | — | |
| 9 | 1663 (36.2) | 37 312 (34.4) | — | |
| 11 | 975 (21.22) | 33 610 (31) | — | |
| Race, n (%) | <.0001 | |||
| White | 2687 (59.3) | 81 683 (76) | — | |
| Black, African, or African American | 342 (7.6) | 4812 (4.5) | — | |
| Hispanic | 516 (11.4) | 7319 (6.8) | — | |
| Asian American | 432 (9.5) | 5279 (4.9) | — | |
| American Indian | 116 (2.6) | 1166 (1.1) | — | |
| Mulitracial or unknown | 416 (9.2) | 7077 (6.6) | — | |
| Free school lunch, n (%) | 2055 (45.5) | 26 617 (24.8) | <.0001 | — |
| School location, n (%) | <.0001 | |||
| Metropolitan | 2319 (50.5) | 56 289 (51.8) | — | |
| Nonmetropolitan | 2275 (49.5) | 52 314 (48.2) | — | |
| Emotional health outcomes, n (%) | ||||
| High emotional distress (last 12 mo) | 1884 (42) | 28 417 (26.6) | <.0001 | 2.0 (1.9–2.1) |
| SIB | 1317 (29.1) | 15 116 (14.0) | <.0001 | 2.5 (2.3–2.7) |
| Suicidal ideation | 940 (21) | 11 081 (10.4) | <.0001 | 2.3 (2.1–2.5) |
| Suicide attempt | 416 (9.3) | 3286 (3.1) | <.0001 | 3.2 (2.9–3) |
| Developmental assets, mean [SD] | ||||
| Positive identity | 2.7 [0.7] | 2.9 [0.7] | <.0001 | — |
| Social competency | 2.8 [0.7] | 3.1 [0.6] | <.0001 | — |
| Empowerment | 2.7 [0.8] | 3.0 [0.8] | <.0001 | — |
| Academic orientation | 3.1 [0.5] | 3.3 [0.5] | <.0001 | — |
| Positive teacher | 2.9 [0.7] | 3 [0.6] | <.0001 | — |
| High parent connectedness, n (%) | 2504 (97.8) | 68 791 (99) | <.001 | — |
—, not applicable.
aOR for family-homeless youth compared with housed youth. Adjusted for age, race and/or ethnicity, poverty (free and reduced-price school lunch), and school location (metropolitan versus nonmetropolitan).
Emotional Distress, Self-Harm, and Suicide Outcomes
Of youth who experienced family homelessness, 42% had high levels of emotional distress, 29.1% had SIB, 21% had suicidal ideation, and 9.3% attempted suicide within the last 12 months (Table 1). In unadjusted analyses, these outcomes occurred over twice as often in homeless youth versus housed youth. These results remained after controlling for age, sex, race, socioeconomic status, and school location (emotional distress adjusted odds ratio [aOR]: 2.0, 95% CI: 1.9–2.1; SIB aOR: 2.5, 95% CI: 2.3–2.7; suicidal ideation aOR: 2.3, 95% CI: 2.1–2.5; suicide attempt aOR: 3.2, 95% CI: 2.9–3). Among both homeless youth and housed youth, all negative emotional health outcomes were most prevalent among homeless girls (Table 2).
TABLE 2.
Unadjusted Frequencies by Sex
| Homeless, n (%) | P | Nonhomeless, n (%) | P | |||
|---|---|---|---|---|---|---|
| n = 4594 (2.8) | n = 108 603 (67.02) | |||||
| Boys | Girls | Boys | Girls | |||
| Total, n (%) | 2522 (3.1) | 2072 (2.6) | <.001 | 53 307 (65.3) | 55 296 (68.9) | <.001 |
| Emotional health outcomes, % | ||||||
| Emotional distress | 29.2 | 57.3 | <.0001 | 18.1 | 34.8 | <.0001 |
| SIB | 20.5 | 39.6 | <.001 | 7.9 | 19.9 | <.001 |
| Suicidal ideation | 13.2 | 30.6 | <.001 | 6.4 | 14.2 | <.001 |
| Suicidal attempt | 6.3 | 12.8 | <.001 | 1.7 | 4.4 | <.001 |
| Developmental assets | ||||||
| Positive identity, mean [SD] | (2.8) [0.72] | (2.5) [0.70] | <.0001 | (3.0) [0.6] | (2.8) [0.7] | <.0001 |
| Social competency, mean [SD] | (2.8) [0.7] | (2.8) [0.6] | 0.9 | 93.0) [0.6] | (3.1) [0.6] | <.0001 |
| Empowerment, mean [SD] | (2.8) [0.8] | (2.6) [0.6] | <.001 | (3) [0.7] | (3.0) [0.8] | <.001 |
| Academic orientation , mean [SD] | (3.1) [0.6] | (3.2) [0.6] | <.001 | (3.2) [0.5] | (3.4) [0.5] | <.001 |
| Positive teacher , mean [SD] | (2.9) [0.7] | (2.8) [0.6] | <.0001 | (3.0) [0.6] | (3.0) [0.5] | <.0001 |
| Parent connectedness, % | 97.74 | 97.91 | .7 | 99.05 | 99.02 | .7 |
Developmental Assets
Family-homeless youth experienced lower levels of developmental assets compared with housed youth (Table 1). Differences between these groups were small to moderate (Cohen’s d = 0.15–0.46). The developmental asset scores were concentrated toward the high end of the distribution for all assets (left skewed), regardless of housing status. For homeless youth, there were significant differences between boys and girls for positive identity, empowerment, academic orientation, and positive teacher assets (Table 2). There were no significant differences between homeless boys and girls for parent connectedness and social competency. For nonhomeless boys and girls, there were significant differences for all assets except parent connectedness.
Moderation of Emotional Health Outcomes by Developmental Assets
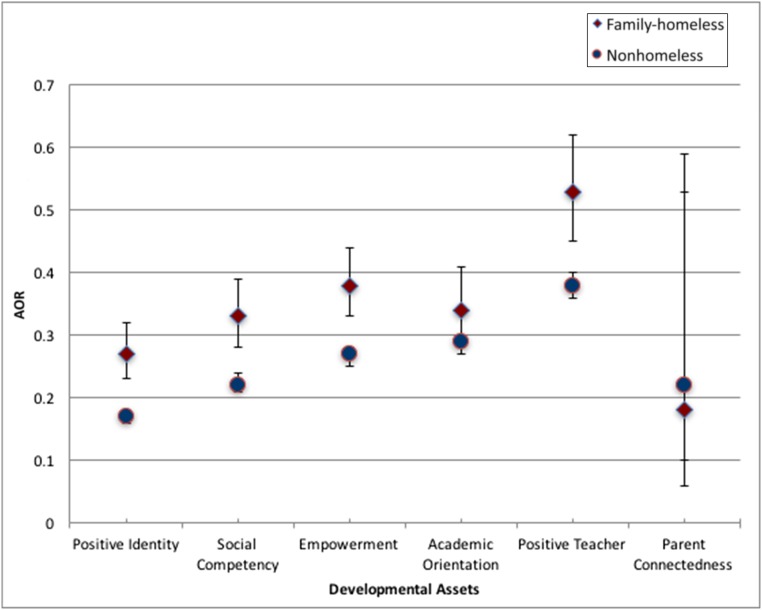
All developmental assets reduced the odds of emotional distress, SIB, suicidal ideation, and suicide attempts for all youth. Nonetheless, these developmental assets generally had a stronger protective effect among housed than homeless youth (Table 3, “Overall” columns). For example, although positive identity reduced the odds of attempted suicide by 82% among housed youth, this asset only reduced the odds among homeless youth by 72%. (Figure 1 illustrates the results for attempted suicide). These findings did not reach statistical significance for all assets and all emotional health outcomes (as demonstrated by overlapping CIs between aORs for homeless and housed youth); for example, positive identity and empowerment were significantly different across all 4 emotional health outcomes, whereas social competency was significantly different only for self-harm and suicide attempts, and academic orientation and parent connectedness were never significantly different. Stratification of these results by sex (Table 3) revealed that some assets were more protective for girls than boys. For example, homeless girls with high levels of parent connectedness had lower odds of suicidal ideation and SIB than homeless boys with high levels of this asset.
TABLE 3.
aORs of Emotional Health Outcomes by Developmental Moderators, Sex, and Housing Status
| Boys | Girls | Overall | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Homeless | Nonhomeless | Homeless | Nonhomeless | Homeless | Nonhomeless | |||||||
| aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | |
| Emotional distress | ||||||||||||
| Positive identity | 0.37 | 0.32–0.43 | 0.26 | 0.25–0.27 | 0.29 | 0.24–0.34 | 0.2 | 0.19–0.2 | 0.33 | 0.28–0.39 | 0.23 | 0.22–0.24 |
| Social competency | 0.46 | 0.4–0.53 | 0.43 | 0.41–0.44 | 0.39 | 0.33–0.46 | 0.28 | 0.27–0.3 | 0.43 | 0.37–0.50 | 0.36 | 0.34–0.37 |
| Empowerment | 0.45 | 0.4–0.51 | 0.37 | 0.36–0.39 | 0.39 | 0.34–0.41 | 0.32 | 0.31–0.33 | 0.42 | 0.37–0.46 | 0.35 | 0.34–0.36 |
| Academic orientation | 0.48 | 0.4–0.56 | 0.46 | 0.44–0.48 | 0.47 | 0.39–0.57 | 0.35 | 0.33–0.36 | 0.48 | 0.40–0.57 | 0.41 | 0.39–0.42 |
| Positive teacher | 0.6 | 0.52–0.68 | 0.55 | 0.53–0.57 | 0.47 | 0.4–0.55 | 0.41 | 0.4–0.43 | 0.54 | 0.46–0.62 | 0.48 | 0.47–0.50 |
| Parent connectedness | 0.55 | 0.25–1.78 | 0.27 | 0.21–0.34 | 0.2 | 0.06–0.69 | 0.26 | 0.21–0.33 | 0.38 | 0.16–1.24 | 0.27 | 0.21–0.34 |
| Self-harm | ||||||||||||
| Positive identity | 0.36 | 0.31–0.42 | 0.27 | 0.26–0.29 | 0.30 | 0.26–0.36 | 0.18 | 0.17–0.19 | 0.33 | 0.29–0.39 | 0.23 | 0.22–0.24 |
| Social competency | 0.39 | 0.34–0.46 | 0.34 | 0.33–0.36 | 0.37 | 0.31–0.43 | 0.24 | 0.23–0.25 | 0.38 | 0.33–0.45 | 0.29 | 0.28–0.31 |
| Empowerment | 0.42 | 0.37–0.48 | 0.36 | 0.35–0.38 | 0.39 | 0.34–0.44 | 0.29 | 0.28–0.30 | 0.41 | 0.36–0.46 | 0.32 | 0.31–0.34 |
| Academic orientation | 0.41 | 0.34–0.49 | 0.37 | 0.35–0.39 | 0.37 | 0.30–0.44 | 0.31 | 0.29–0.32 | 0.39 | 0.32–0.47 | 0.34 | 0.32–0.36 |
| Positive teacher | 0.62 | 0.53–0.72 | 0.50 | 0.48–0.52 | 0.55 | 0.47–0.64 | 0.41 | 0.40–0.43 | 0.59 | 0.50–0.68 | 0.46 | 0.44–0.48 |
| Parent connectedness | 0.34 | 0.16–0.73 | 0.18 | 0.14–0.22 | 0.18 | 0.07–0.49 | 0.22 | 0.18–0.28 | 0.26 | 0.11–0.61 | 0.20 | 0.16–0.25 |
| Suicide ideation | ||||||||||||
| Positive identity | 0.26 | 0.21–0.31 | 0.21 | 0.19–0.22 | 0.27 | 0.23–0.32 | 0.17 | 0.16–0.18 | 0.27 | 0.22–0.32 | 0.19 | 0.18–0.20 |
| Social competency | 0.36 | 0.30–0.44 | 0.35 | 0.33–0.37 | 0.32 | 0.27–0.38 | 0.26 | 0.25–0.27 | 0.34 | 0.29–0.41 | 0.31 | 0.29–0.32 |
| Empowerment | 0.35 | 0.30–0.41 | 0.30 | 0.28–0.31 | 0.36 | 0.31–0.41 | 0.28 | 0.27–0.29 | 0.36 | 0.31–0.41 | 0.29 | 0.27–0.30 |
| Academic orientation | 0.40 | 0.32–0.49 | 0.39 | 0.37–0.42 | 0.43 | 0.36–0.52 | 0.34 | 0.32–0.35 | 0.41 | 0.34–0.51 | 0.37 | 0.34–0.39 |
| Positive teacher | 0.53 | 0.45–0.64 | 0.48 | 0.45–0.50 | 0.48 | 0.41–0.56 | 0.40 | 0.38–0.42 | 0.51 | 0.43–0.60 | 0.44 | 0.42–0.46 |
| Parent connectedness | 0.46 | 0.20–1.07 | 0.20 | 0.15–0.26 | 0.16 | 0.06–0.42 | 0.23 | 0.18–0.29 | 0.31 | 0.13–0.75 | 0.22 | 0.17–0.27 |
| Suicide attempts | ||||||||||||
| Positive identity | 0.25 | 0.20–0.32 | 0.20 | 0.18–0.22 | 0.30 | 0.24–0.37 | 0.16 | 0.15–0.17 | 0.28 | 0.22–0.35 | 0.18 | 0.17–0.20 |
| Social competency | 0.33 | 0.26–0.43 | 0.25 | 0.23–0.28 | 0.33 | 0.26–0.42 | 0.21 | 0.20–0.23 | 0.33 | 0.26–0.43 | 0.23 | 0.22–0.26 |
| Empowerment | 0.37 | 0.30–0.46 | 0.28 | 0.25–0.30 | 0.39 | 0.33–0.47 | 0.26 | 0.25–0.28 | 0.38 | 0.31–0.47 | 0.27 | 0.25–0.29 |
| Academic orientation | 0.29 | 0.22–0.38 | 0.31 | 0.28–0.35 | 0.38 | 0.30–0.49 | 0.27 | 0.25–0.30 | 0.33 | 0.26–0.43 | 0.29 | 0.27–0.32 |
| Positive teacher | 0.54 | 0.42–0.69 | 0.41 | 0.38–0.46 | 0.51 | 0.41–0.63 | 0.36 | 0.34–0.39 | 0.53 | 0.42–0.66 | 0.39 | 0.36–0.43 |
| Parent connectedness | 0.15 | 0.07–0.34 | 0.16 | 0.11–0.24 | 0.21 | 0.09–0.49 | 0.28 | 0.21–0.38 | 0.18 | 0.08–0.41 | 0.22 | 0.16–0.31 |
Adjusted for age, race and/or ethnicity, poverty (free and reduced-price school lunch), and school location (metropolitan versus nonmetropolitan).
FIGURE 1.
aORs for attempted suicide for homeless versus nonhomeless youth by developmental assents.
Discussion
This study documents the past-year incidence of emotional distress, suicidal ideation, nonsuicidal self-injury, and suicide attempts among youth living in families experiencing homelessness in the past year. These adolescents have over twice the risk of severe emotional distress, self-injury, suicidal thinking, and attempted suicide than their peers with homes. These findings remained even after controlling for sociodemographic factors linked to both homelessness and mental health problems.
The underlying risk factors that could explain these results are adverse childhood experiences (ACEs), which are common among homeless youth.20 For example, authors of a previous observational study found a twofold increased risk of depressed mood and a 2.5-fold increased risk of suicide attempts among adults who reported high residential mobility (>7 moves) during childhood, which was attenuated after statistically controlling for ACE scores.21 The increased odds of suicidality among homeless youth in our study is similar in magnitude to that in population-based samples of adults who experienced multiple ACEs (but not necessarily also homelessness).22,23 Our study did not assess ACE scores because of limitations of the school-based measures used. Our results imply that family homelessness during childhood and adolescence is itself a potential clinical marker of mental health risk, as reinforced by numerous epidemiologic studies that link residential mobility with adolescent emotional-behavioral problems.24 Housing status is often easily ascertained during routine clinical care, whereas ACEs are often impractical to obtain, difficult to interpret, or remain undisclosed.25,26 Clinicians should be prepared to provide more frequent and trauma-informed mental health surveillance, screening, and care when encountering youth who have experienced family homelessness.
Our results also highlight the mental health-promoting influence of developmental assets, such as parent connectedness and a sense of positive identity, for all youth. We found these to be strongly present even in homeless contexts; the relatively small differences between the mean self-reported levels of these assets in homeless and nonhomeless youth could be deemed clinically insignificant or undetectable (despite their statistical differentiation, which might be expected given the large sample size). Some of these factors were equally beneficial for homeless and housed youth (eg, parent connectedness). Nevertheless, some of these factors (eg, empowerment) were less protective for family-homeless youth. The reasons for this are unclear and should be explored by authors in future research and could include so-called developmental cascades of mutually-dependent factors operating across functional domains.2 In other words, it is plausible that the provision of stable housing is a critical factor that must be intervened on to fully “activate” the putative protective effects of some developmental assets on mental health risk among homeless youth. For example, young people who have a strong, positive sense of self might optimally manifest the full benefits of that asset when living in a safe and reliable home that allows them to invite friends over, complete their homework, and rely on supportive adults who live next door.
The methodological strengths of this study include the large, state-representative sample, allowing for robust comparisons of potential developmental moderators of low-frequency mental health outcomes (eg, suicide attempts) between groups such as homeless girls versus homeless boys. The delivery of the survey in schools also allows for the collection of data on adolescents who have been homeless with a family member, a group that is otherwise challenging to reach. Likewise, suicidality and emotional distress may be difficult for youth to disclose under other circumstances, and although these items in the current study are not otherwise validated, we know that youth self-report is more accurate than caregiver report for internalizing symptoms and suicidality.27–29 Our study is limited by its cross-sectional nature; thus, our results represent correlations, and causation or change over time cannot be inferred. Furthermore, besides ACEs, a number of other predictors of adolescent emotional health were not measured, such as coping behaviors, sleep, and daily hassles and/or minor stressors.30 Adolescent self-report of past-year family homelessness is of uncertain validity and reliability, and other information about housing status was not asked (such as duration of homelessness). However, self-report of housing status using a broad description of what constitutes family homelessness may be more accurate than head counts31,32; parent reports can also be a viable alternative.33 Furthermore, although the school-based nature of this study enabled data collection among this difficult-to-reach population, homeless youth are more likely than nonhomeless youth to experience school absenteeism,34 introducing a possible source of selection bias. The generalizability of our results is also limited by the regional and periodic administration of the MSS, representing a large cohort within just 1 year and 1 state; longitudinal research is needed to ascertain emotional health during and after episodes of homelessness. Finally, some of the stratified logistic regression models examining moderation of emotional health outcomes by developmental assets had small sample sizes, increasing the chances of type II errors (failing to reject false null hypotheses). Our analyses should thus be replicated in a nationally-representative longitudinal sample, and secular trends monitored over time, to better inform program and policy development.
The relationship between homelessness and emotional health outcomes has important implications for clinical practice and policymaking. Our results reinforce the practices endorsed by the 2013 American Academy of Pediatrics Policy Statement, such as screening for housing status and innovating to deliver pediatric care across housing contexts (such as mobile services and shelter-based care).1 Clinicians can also use these results to discuss resilience with children and parents experiencing homelessness or unstable housing, including the importance of family-, school-, and individual-level factors that promote children’s emotional health even under circumstances of severe adversity. At the same time, our results highlight the importance of conducting clinical surveillance and screening (for all youth) that is sensitive to highly prevalent emotional-behavioral disorders (including doing so in nontraditional contexts such as acute visits to best meet the needs of youth with housing instability). Likewise, policy makers can advocate for programs and funding to provide “housing first” and related mental health supports to homeless children, youth, and families as preventive public health strategies.
Conclusions
Youth experiencing family homelessness are at greater risk of emotional distress, SIB, suicidal ideation, and attempted suicide than their nonhomeless peers. However, positive factors are frequently present in the lives of homeless youth as well. Although these factors serve to promote emotional well-being among all youth, they may not be as protective for youth who are homeless, implying a gap in programs and policies to fully meet their emotional health needs. Potential solutions that await further investigation include the provision of trauma-informed health and educational services, and policies that support stable and sustainable family housing.
Glossary
- ACE
adverse childhood experience
- aOR
adjusted odds ratio
- CI
confidence interval
- GAIN-SS
Global Appraisal of Individual Needs–Short Screener
- MSS
Minnesota Student Survey
- SIB
self-injurious behavior
Footnotes
Dr Barnes conceptualized and designed the study and drafted the initial manuscript; Mr Gilbertson conducted statistical analyses and drafted the initial manuscript; Dr Chatterjee provided statistical analyses, data interpretation, and critically reviewed the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Dr. Barnes was supported by the National Institutes of Health National Center for Translational Sciences Clinical and Translational Science Award at the University of Minnesota 8UL1TR000114-02. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Council on Community Pediatrics Providing care for children and adolescents facing homelessness and housing insecurity. Pediatrics. 2013;131(6):1206–1210 [DOI] [PubMed] [Google Scholar]
- 2.Masten AS. Ordinary Magic: Resilience in Development. New York, NY: Guilford; 2014 [Google Scholar]
- 3.Sullivan EM, Annest JL, Simon TR, Luo F, Dahlberg LL; Centers for Disease Control and Prevention (CDC) . Suicide trends among persons aged 10-24 years—United States, 1994-2012. MMWR Morb Mortal Wkly Rep. 2015;64(8):201–205 [PMC free article] [PubMed] [Google Scholar]
- 4.Roy E, Haley N, Leclerc P, Sochanski B, Boudreau J-F, Boivin J-F. Mortality in a cohort of street youth in Montreal. JAMA. 2004;292(5):569–574 [DOI] [PubMed] [Google Scholar]
- 5.Whitbeck LB, Johnson KD, Hoyt DR, Cauce AM. Mental disorder and comorbidity among runaway and homeless adolescents. J Adolesc Health. 2004;35(2):132–140 [DOI] [PubMed] [Google Scholar]
- 6.Masten AS, Cutuli JJ, Herbers JE, Hinz E, Obradovi J, Wenzel AJ. Academic risk and resilience in the context of homelessness. Child Dev Perspect. 2014;8(4):201–206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Toro PA. Toward an international understanding of homelessness. J Soc Issues. 2007;63(3):461–481 [Google Scholar]
- 8.Henry M, Shivji A, De Sousa T, et al. The 2015 annual homeless assessment report (AHAR) to Congress. Part 1: Point-in-time estimates of homelessness. 2015. Available at: https://www.hudexchange.info/resources/documents/2015-AHAR-Part-1.pdf. Accessed January 30, 2018
- 9.Tobin K, Murphy J. Addressing the challenges of child and family homelessness. J Appl Res Child. 2013;4(1):1–29 [Google Scholar]
- 10.Bassuk EL, DeCandia EJ, Beach CA, Berman F. America’s Youngest Outcasts: A Report Card on Child Homelessness. Waltham, MA: National Center on Family Homelessness; 2014 [Google Scholar]
- 11.Sesma A, Mannes M, Scales PC. Positive adaptation, resilience and the developmental assets framework In: Goldstein S, Brooks RB, eds. Handbook of Resilience in Children. 2nd ed Boston, MA: Springer; 2013:427–442 [Google Scholar]
- 12.Eisenberg ME, Gower AL, McMorris BJ. Emotional health of lesbian, gay, bisexual and questioning bullies: does it differ from straight bullies? J Youth Adolesc. 2016;45(1):105–116 [DOI] [PubMed] [Google Scholar]
- 13.Eisenberg ME, Gower AL, McMorris BJ, Bucchianeri MM. Vulnerable bullies: perpetration of peer harassment among youths across sexual orientation, weight, and disability status. Am J Public Health. 2015;105(9):1784–1791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gower AL, McMorris BJ, Eisenberg ME. School-level contextual predictors of bullying and harassment experiences among adolescents. Soc Sci Med. 2015;147:47–53 [DOI] [PubMed] [Google Scholar]
- 15.US Department of Housing and Urban Development The McKinney-Vento homeless assistance act. As amended by S. 896 the homeless emergency assistance and rapid transition to housing (HEARTH) act of 2009. 2009. Available at: https://www.hudexchange.info/resources/documents/HomelessAssistanceActAmendedbyHEARTH.pdf. Accessed January 30, 2018
- 16.Dennis ML, Chan Y-F, Funk RR. Development and validation of the GAIN Short Screener (GSS) for internalizing, externalizing and substance use disorders and crime/violence problems among adolescents and adults. Am J Addict. 2006;15(suppl 1):80–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Scales PC. Youth developmental assets in global perspective: results from international adaptations of the developmental assets profile. Child Indic Res. 2011;4(4):619–645 [Google Scholar]
- 18.Appleton JJ, Christenson SL, Kim D, Reschly AL. Measuring cognitive and psychological engagement: validation of the student engagement instrument. J Sch Psychol. 2006;44(5):427–445 [Google Scholar]
- 19.Hicks MS, McRee A-L, Eisenberg ME. Teens talking with their partners about sex: the role of parent communication. Am J Sex Educ. 2013;8(1–2):1–17 [Google Scholar]
- 20.Herbers JE, Cutuli JJ, Monn AR, Narayan AJ, Masten AS. Trauma, adversity, and parent-child relationships among young children experiencing homelessness. J Abnorm Child Psychol. 2014;42(7):1167–1174 [DOI] [PubMed] [Google Scholar]
- 21.Dong M, Anda RF, Felitti VJ, et al. . Childhood residential mobility and multiple health risks during adolescence and adulthood: the hidden role of adverse childhood experiences. Arch Pediatr Adolesc Med. 2005;159(12):1104–1110 [DOI] [PubMed] [Google Scholar]
- 22.Felitti VJ, Anda RF, Nordenberg D, et al. . Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. the adverse childhood experiences (ACE) study. Am J Prev Med. 1998;14(4):245–258 [DOI] [PubMed] [Google Scholar]
- 23.Fuller-Thomson E, Baird SL, Dhrodia R, Brennenstuhl S. The association between adverse childhood experiences (ACEs) and suicide attempts in a population-based study. Child Care Health Dev. 2016;42(5):725–734 [DOI] [PubMed] [Google Scholar]
- 24.Jelleyman T, Spencer N. Residential mobility in childhood and health outcomes: a systematic review. J Epidemiol Community Health. 2008;62(7):584–592 [DOI] [PubMed] [Google Scholar]
- 25.Van Niel C, Pachter LM, Wade R Jr, Felitti VJ, Stein MT. Adverse events in children: predictors of adult physical and mental conditions [published correction appears in J Dev Behav Pediatr. 2014;35(9):581]. J Dev Behav Pediatr. 2014;35(8):549–551 [DOI] [PubMed] [Google Scholar]
- 26.Kerker BD, Storfer-Isser A, Szilagyi M, et al. . Do pediatricians ask about adverse childhood experiences in pediatric primary care? Acad Pediatr. 2016;16(2):154–160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Walker M, Moreau D, Weissman MM. Parents’ awareness of children’s suicide attempts. Am J Psychiatry. 1990;147(10):1364–1366 [DOI] [PubMed] [Google Scholar]
- 28.Cantwell DP, Lewinsohn PM, Rohde P, Seeley JR. Correspondence between adolescent report and parent report of psychiatric diagnostic data. J Am Acad Child Adolesc Psychiatry. 1997;36(5):610–619 [DOI] [PubMed] [Google Scholar]
- 29.Martin JL, Ford CB, Dyer-Friedman J, Tang J, Huffman LC. Patterns of agreement between parent and child ratings of emotional and behavioral problems in an outpatient clinical setting: when children endorse more problems. J Dev Behav Pediatr. 2004;25(3):150–155 [DOI] [PubMed] [Google Scholar]
- 30.Seiffge-Krenke I. Causal links between stressful events, coping style, and adolescent symptomatology. J Adolesc. 2000;23(6):675–691 [DOI] [PubMed] [Google Scholar]
- 31.Cutuli JJ, Steinway C, Perlman S, Herbers JE, Eyrich-Garg KM, Willard J. Youth homelessness: prevalence and associations with weight in three regions. Health Soc Work. 2015;40(4):316–324 [DOI] [PubMed] [Google Scholar]
- 32.Cutuli JJ. Homelessness in high school: population-representative rates of self-reported homelessness, resilience, and risk in Philadelphia. Soc Work Res. 2017, In press. [Google Scholar]
- 33.Jetelina KK, Reingle Gonzalez JM, Cuccaro PM, et al. . The association between familial homelessness, aggression, and victimization among children. J Adolesc Health. 2016;59(6):688–695 [DOI] [PubMed] [Google Scholar]
- 34.Kearney CA. School absenteeism and school refusal behavior in youth: a contemporary review. Clin Psychol Rev. 2008;28(3):451–471 [DOI] [PubMed] [Google Scholar]