Abstract
Objectives
The aim of this study was to survey podiatric residency directors to evaluate the proficiency of first-year podiatric medical residents in the use of electronic medical records and its potential impact on medical care.
Methods
An online survey consisting of Likert-scale, multiple-choice, and open-ended questions was sent via email to 216 podiatric residency directors. Questions were directed toward the level of proficiency in electronic medical records expected at the beginning of residency training and the impact on patient care of residents' inexperience with electronic medical records.
Results
A total of 54 of the 216 podiatric medical residency directors completed the survey. Results indicated that 70.3 percent of respondent directors expected a moderate level of proficiency in the use of electronic medical records; however, 35.2 percent indicated that less than 50 percent of the new residents had experience with electronic medical records prior to starting residency training. Only 51.5 percent of respondent directors felt that the new residents were successful or highly successful in using their hospital's electronic medical record upon arrival, but that figure increased to 98.2 percent upon completion of the first year of residency. Of importance, 29.7 percent of respondent directors reported that inexperience in electronic medical record use resulted in a more-than-average to high impact on patient care, with open-ended responses including concerns about potential HIPAA violations, data breaches, or lost data.
Conclusion
Residency directors deem it important that incoming first-year residents have a basic understanding of electronic medical records and related health informatics concepts; however, in-depth knowledge is not expected because of the high number of software programs available. Nonetheless, nearly one-third of respondents reported that inexperience in electronic medical record use does have a significant impact on patient care.
Keywords: electronic medical record, medical education, PGY1 resident, informatics, quality patient care
Introduction
Health information technology (IT) is transforming how patient data are captured, retrieved, and displayed. Since the American Recovery and Reinvestment Act (ARRA) and the Health Information Technology for Economic and Clinical Health (HITECH) Act (2009/2010), health IT and electronic medical records (EMRs) have proliferated in use in hospitals across the United States.1 As a result, EMRs have become an integral component of healthcare delivery. In order for clinicians and medical personnel to care for patients within the hospital, they need to know how to use EMR software in the workflow of patient care. EMR systems are evolving and improving, but take time for clinicians to master in a workflow. Adding to the difficulty of effectively and efficiently using EMR systems are usability challenges that create inefficiencies and, in some cases, unintended consequences that can affect patient health outcomes and potentially cause patient harm.2
Medical Students and First-Year Residents
To effectively prepare medical residents for EMR use, medical schools need to include EMRs and health informatics in the curriculum. While the literature surrounding podiatric medicine students and postgraduate year one (PGY1) podiatric residents is scarce, we examined the literature regarding other medical residents and students. Only a few medical schools currently train or assess medical informatics competencies even though use of the EMR system is part of the routine workflow and expectations of PGY1 residents and directly affects their work. This lack of exposure may pose challenges for new PGY1 residents and, worse, may negatively affect patient care.
Concerns exist about how EMRs influence the doctor-patient relationship, with the focus placed on bad habits and mistakes made when using EMRs rather than on corrective measures or education.3, 4 The literature shows that EMR use is associated with residents asking more history questions because of EMR prompts; improved access and legibility; and improved likelihood that faculty would review a resident's documentation.5, 6, 7 Moreover, using an EMR is associated with essential information being generally easier to find than on paper records; improved documentation; and better likelihood of receiving feedback on EMR notes compared to paper charts. It is important to determine an agreed-upon set of expectations for EMR use for PGY1 residents, as well as for senior residents and attending staff, so that information can be captured and accessed in a reliable way. In doing so, care team clinicians can support each other in utilizing the EMR in the most effective ways possible to improve patient care. Otherwise, a number of techniques of EMR use could compromise patient safety. For example, studies of electronic documentation habits among residents and medical students have reported the use of copy-paste shortcuts8, 9 and have shown that that, despite believing that it is unacceptable, students used the shortcuts and indicated that they witnessed their supervisors also using this technique.10 Other problems around medical students' use of EMRs mentioned in the literature include failure to interpret data and low usage of tools such as medication interactions, health maintenance prompts, and online resources such as clinical guidelines, all of which underscore the need for additional training and basic competencies.11
As new residents or PGY1 clinicians start their residencies, they are expected, along with providing patient care, to learn and master health IT systems, workflows, procedures, and processes, including the use of the EMR system. While hospitals typically provide some form of training for the staff and medical personnel, no standard competency level has been established for EMR use before PGY1 residents arrive at their program. Recognizing the importance of medical residents' ability to use the EMR system, Nuovo and colleagues12 worked with an EMR training group to develop EMR competencies for first-year residents for both ambulatory care and in-patient care. In their study, first-year residents were given the newly developed training and later evaluated by senior residents three to four months after training. The types of skills with which interns needed the most assistance were as follows:
creating and routing a result note,
deleting a medication or changing a dose in reconciling medications, and
finding results for the past 90 days.
Any of these areas with which respondents appeared to have difficulty could directly affect patient care and outcomes.
As medical educators work to improve training on EMR systems, it is important to take into account that patterns for using the EMR may change over time among physicians. Thus, a phased and continual approach to training beginning in medical school and continuing into the postgraduate years of residency and throughout the medical career may be warranted. In fact, one study found that third-year residents in family medicine spent more time on the EMR than their first- and second-year resident colleagues did during a patient office visit, perhaps indicating that increased proficiency and increased workload may incentivize extended use of EMR during the patient visit.13 Moreover, other researchers found varying degrees of learnability gaps between expert and novice physician groups that may impede the use of EMRs, and recommended improving EMR training programs by identifying usability issues faced by physicians through a more granular task analysis of EMR use.14
Other research has examined the impact that health IT has on the doctor-patient relationship, proposing health IT and communication training earlier for medical students. Wald and colleagues15 described concerns of “triangulation,” that is, how the doctor-patient relationship may be affected by reliance on an EMR or computer device. They described efforts at a medical school to introduce training on EMR use and communication skills necessary to improve patient outcomes in this new triangulated relationship. One study discussed that medical schools are beginning to prepare new physicians for the emerging models of care that require health IT as a means to treat patients, meet compliance standards, and be compensated through value-based payment models.16
Residency Directors
To further understand how PGY1 residents are prepared to use EMRs and apply health informatics principles, it is imperative to understand the perspectives of residency directors. A residency director serves as a supervisor, guide, and mentor to new residents as they begin postgraduate patient care, generally in hospital settings. Residency directors have a unique perspective on the demands of the residency, the necessary skills required of residents, and the potential impact of training on patient care. Little is known about the expectations of residency directors working with PGY1 residents relative to EMR use and health informatics principles. The research reported in this paper adds to a very limited literature on how residency directors consider and evaluate the extent to which their PGY1 residents are prepared to use a health IT knowledge base. Specifically, this study examines the preparedness of PGY1 podiatric residents for EMR use and the potential impact that this preparedness has on patient care, from the perspective of the residency director.
Materials and Methods
A cross-sectional survey study was conducted to determine how well prepared first-year podiatric medical residents were for EMR use. Published email addresses for 224 podiatric medical residency programs across the United States were obtained via the CASPR Directory on the American Association of Colleges of Podiatric Medicine (AACPM) website. Emails were sent to the listed email addresses to confirm the contact information for the residency directors. Email addresses for 216 of the 224 residency directors (96.4 percent) were confirmed. The link to the confidential survey was emailed to the 216 residency directors at the end of the 2014–2015 residency training year. This study was reviewed and approved by the Kent State University Institutional Review Board (IRB). By clicking on the link to the survey, the respondents provided consent to participate in the study.
The online survey (SurveyMonkey; Palo Alto, CA) consisted of up to 17 Likert-type scale, multiple-choice, and open-ended questions, using branch logic to ask more specific questions depending on the answers provided. The survey questions were directed toward the level of proficiency in EMR use expected at the beginning of first-year (PGY1) residency training and the impact of inexperience in EMR use on patient care (see Appendix 1). The questions were generated based on discussions among the research team members during the initial planning stages. In terms of reliability, with appropriate conversions of items with 4- and 5-point response categories, Cronbach's alpha scores on the set of Likert-type scale items was .72, which is in the acceptable range.17 The survey instrument was pre-tested among podiatry school faculty members who have served as residency directors in the past. Their feedback was gathered and informed edits to the instrument before it was sent to survey participants. Responses were analyzed to determine the most common responses to the questions.
Results
Residency Programs and EMRs
Fifty-four of the 216 podiatric medical residency directors invited to participate in the study (25.0 percent) completed the survey. Using the geographic regions from the US Census, the distribution of the study's respondents is directly aligned with the geographic distribution of podiatric residency programs in the United States. Specifically, in 2014–2015 (according to data at www.AACPM.org), of all podiatric residency programs, the Northeast had 37.5 percent, the Midwest had 26.8 percent, the South had 19.2 percent, and the West had 16.5 percent. Congruently, the respondents in this study came from the following geographic locations: Northeast, 41.5 percent; Midwest, 24.5 percent; South, 17 percent; and West, 17 percent. This parallel distribution allows us to more easily generalize the findings across residency programs.
The size of the programs varied, with the majority of the residency programs included in this study (75.0 percent) having two to four PGY1 residents. Five residency programs (9.6 percent) had only one PGY1 resident, while 15.4 percent of the programs had five or more PGY1 residents.
Epic Systems was the EMR software most often reported to be used at residency program hospitals (28.6 percent), followed by Cerner (24.5 percent), and Vista CPRS (22.4 percent). Allscripts (6.1 percent), eClinical Works (4.1 percent), GE (4.1 percent), McKesson (4.1 percent), QuadraMed QCPR (2.0 percent), and other programs (4.1 percent) were also used. Only 5.5 percent of respondents indicated that their hospital had been using their current EMR for one year or less, while 38.9 percent of the respondents specified that their hospital had been using the current program for five or more years. Three of the residency directors (5.6 percent) were unsure of how long their hospital had been using the current EMR software. The majority of the residency directors surveyed (85.2 percent) were at least moderately satisfied with their hospital's EMR software; however, 5.6 percent were not satisfied at all. Of the respondents, 74.1 percent found their hospital's EMR at least moderately easy to use.
PGY1 Medical Residents and EMRs
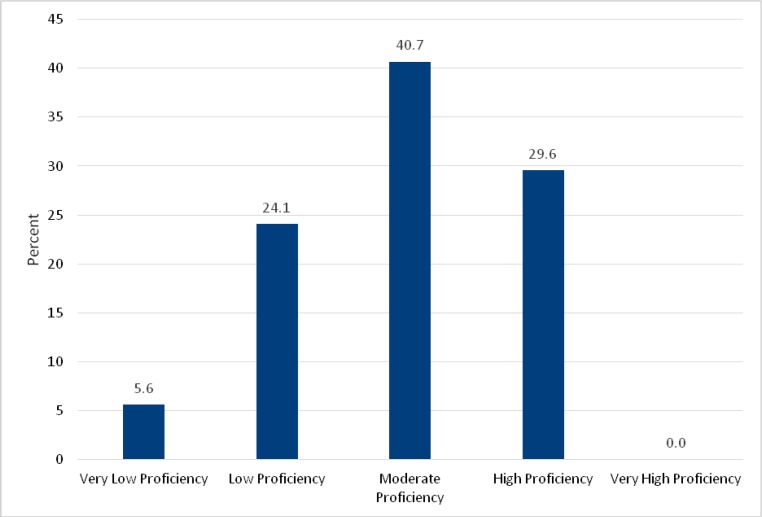
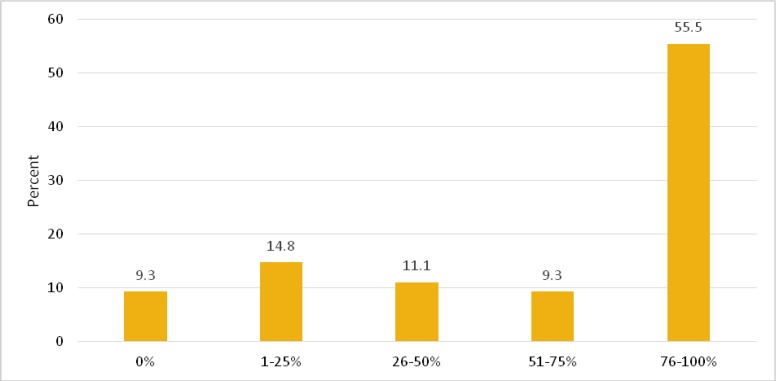
When queried as to the level of proficiency in EMR use that they expected from incoming PGY1 residents, 70.3 percent of respondent directors indicated that they anticipated at least a moderate level of proficiency (see Figure 1). Notably, however, 35.2 percent of respondent directors indicated that 50 percent or less of the PGY1 residents had experience with EMR prior to starting residency training (see Figure 2).
Figure 1.
Level of Proficiency in Electronic Medical Record Use Expected by Residency Directors of Newly Arriving First-Year Residents
Figure 2.
Percentage of First-Year Residents Having Prior Experience with Electronic Medical Record Use
With respect to the success of PGY1 medical residents in EMR use, 51.9 percent of respondent residency directors conveyed that the new incoming PGY1 residents were successful or highly successful in using their hospital's EMR. In contrast, 98.2 percent of respondents felt that the residents were successful or highly successful in using their hospital's EMR upon completion of the first year of training (see Figure 3). Just over 44 percent of respondents indicated that PGY1 residents were moderately successful at the start of the PGY1 year. As indicated in other measures (e.g., those assessing the impact of inexperience with EMR use), it is important to understand the potential impact on patient care in the case of those PGY1 residents who are moderately successful and may still be acquiring EMR and related health informatics skills (e.g., awareness of HIPAA [Health Insurance Portability and Accountability Act] violations, prevention of data breaches or data loss, etc.) throughout their first year of residency.
Figure 3.
First-Year (PGY1) Residents' Success in Electronic Medical Record Use upon Arrival and at the End of the First Year of Residency
Of the medical residency directors surveyed, the majority (87.0 percent) indicated that onsite hospital training was a contributing factor to PGY1 residents' success in using the EMR, while 38.9 percent also believed that training in podiatric medical school was a determinant. All but one (98.2 percent) of the responding residency directors indicated that their hospital provided onsite EMR training. Of those, 94.3 percent were at least moderately satisfied with the training provided by the hospital. As indicated by the directors, the most common methods of training were classroom (77.4 percent) and in-person (64.1 percent) training. Online and one-on-one training were also reported (30.2 percent and 35.8 percent, respectively). The majority of respondents (66.0 percent) indicated that incoming PGY1 podiatric medical residents received one to two days of training, while 18.9 percent of the programs provided less than one day of training.
Considering the impact of inexperience with EMR use on patient care, 29.7 percent of respondents reported that inexperience in EMR use resulted in a more-than-average to high impact on patient care (see Figure 4). When those who indicated a moderate to high impact of inexperience on patient care are considered, the total increases to 55.6 percent. Open-ended comments associated with this question allowed respondents to list the specific effects of inexperience with EMR on patient care. These effects included the significant impact of possible data breaches; loss of data; HIPAA violations; the need to instruct students on how to practice if the EMR system is down for a period of time, and the need to increase training on encounter completion (ICD-10 and CPT coding). Other respondents discussed the need for proficiency with the EMR because the use of the EMR system should not obscure the personal relationship the physician establishes with their patients. One respondent encouraged training in coding, after describing the increased time commitment for residency directors that occurs if the PGY1 resident leaves a diagnosis code blank. Overall, more than half (55 percent) of respondents indicated at least a moderate impact on patient care by PGY1 residents related to inexperience with the EMR. Another respondent cautioned that the “EMR should never replace the art of being a physician. Being a doctor requires human skills of asking questions and touching people—an H&P [history and physical] is not done by reviewing an EMR.”
Figure 4.
Residency Directors' Perception of the Impact of First-Year Residents' Inexperience with Electronic Medical Records on Patient Care
EMRs in the Medical School Curriculum
Medical residency directors recognize that, with many different EMR software options available, it is difficult to teach EMR use in the medical school curriculum such that students are competent in all programs at the time of graduation. A common recommendation regarding informatics and EMR preparation in the curriculum was to provide students with training on the basic function, process, and structure of an EMR and its role in patient care. Training should also include topics such as the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), ICD-10, CPT coding, and HIPAA implications. Students should generally know how to navigate an EMR and enter data into the system. Some residency directors suggested that podiatric medical students be exposed to as many EMR systems as possible, while others recommended that students become knowledgeable on the most popular EMR programs. Most directors felt that the students should be trained during the third year before they begin clerkship training; however, a few thought that students should be introduced to EMRs as early as the first year of medical school.
Discussion
This research reports on the expectations of podiatric residency directors regarding the training, proficiency, and impact of EMR preparedness among new PGY1 residents. An assessment of these factors from the perspective of the residency director exemplifies the unique challenges faced by residency directors and informs the development of suitable medical informatics competencies for EMR use among podiatric residents.
EMRs have revolutionized the way medical charting is achieved, with a purported increase in work efficiency and workflow. This newer method of charting patient information may come with unintended consequences, most importantly the erosion of the patient-provider relationship.18 In turn, this attention to computer data entry may negatively affect patient care, especially in settings that consistently have new learners with increased patient care responsibility, such as PGY1 residents. Rouf and colleagues19 found that most third-year medical students in their sample reported that the EMR is an improvement over paper records, but third-year students also reported concerns about the potential impact of the EMR on their ability to conduct the doctor-patient encounter. One study showed medical residents spending more time glancing at the EMR than at the patient, potentially causing negative perceptions of the encounter by patients.20 Another study21 found differences in novice and expert physicians' performance, with physicians' proficiency increasing with EMR experience. These findings from the literature align with findings from the current study in that a lack of experience with the EMR can have an impact on patient care. EMR training before and during the PGY1 year could help to address and alleviate some of these issues.
More than 70 percent of respondents expected at least a moderate level of proficiency in EMR use among their PGY1 residents. Yet, in this survey, more than one-third of residency directors thought that half or fewer of their new PGY1 residents had experience with the hospital's EMR system. In a period of time when the new resident is still building his or her medical and surgical knowledge base, the added burden of learning a new EMR system could result in a disconnect between patient and provider or risks to patient safety through unintended consequences.22, 23, 24, 25
More than 55 percent of respondents indicated that inexperience in EMR use had a moderate to high negative impact on patient care. Attention to EMR system exposure and EMR best-practice training in medical school may be necessary to improve clinical care by new PGY1 residents. Respondents mentioned their concerns over potential HIPAA violations and data breaches or data loss related to the impact of inexperience with EMRs among PGY1 residents; thus, additional training for medical students in health informatics is recommended. A number of ways to design the training are available. Nuovo and colleagues26 developed a competency for PGY1 residents to achieve in using the EMR, and recommended that future EMR training target the areas with the greatest performance deficits or be directed at underperforming groups. Open-ended responses in the current study are aligned with the competency training27 in that beyond improving overall competency in EMR use, some areas that require special attention (e.g., encounter completion and ICD-10 and CPT coding) were mentioned. Other research calls for medical education curricula to systematically incorporate the use of EMR health technology in order to optimize the effective triangulation of physician, patient, and computer.28
Our findings suggest that both global and more specified EMR training be provided to medical students at the end of their fourth year, prior to the students' graduation and postgraduate residency training. This coursework could be structured as a workshop or could be incorporated into existing business classes that are already part of the curriculum. Content would be developed and delivered in two weekly sessions. The first large group session would address comprehensive and wide-reaching elements of EMR issues, including best practices in charting, issues related to ICD-10 coding, and compliance with government regulations. The second, more specialized session would offer active participation methods to specific student groups according to their corresponding residency hospital match (i.e., separate groups for Epic Systems, Athena, Allscripts, Cerner, etc.). With the caveats that the EMR implementation, version number, peripheral systems, policies, and workflow will be different at each hospital, this proposed curricular enhancement is a starting point for addressing the concerns raised by residency directors in this project: that inexperience with EMR use does have an impact on patient care.
Limitations of this study include the small sample size, as a higher response rate could improve generalizability and offer additional insight into the needs and potential solutions. Additionally, some of the questions in the survey and their options could be subject to personal interpretation. While the study did ask about the geographic location of the residency director's hospital, it is a limitation to not have a measure of the size and specific location of the hospital, which could have an impact on expectations. Future follow-up research will need to improve response rates by modifying data collection strategies (e.g., budget for additional financial incentives). While limited in generalizability, our study results speak to the ongoing concerns about how best to prepare PGY1 residents and medical students for addressing health informatics concepts and using EMRs. Future research should survey the PGY1 residents themselves to evaluate their preparedness, thoughts, and considerations around best practices for training on EMRs, both in medical school and in the hospital setting.
Conclusion
Residency directors deem it important that incoming PGY1 residents have a basic understanding of EMRs. Although in-depth knowledge is not expected because of the high number of EMR programs available, many respondent residency directors did recommend that some degree of EMR exposure or training during medical school be expected, at the very least to include elements of health information management, meaningful use, basic coding, and HIPAA patient data security. Nonetheless, more than half of the study respondents believe that inexperience in EMR use has an impact on patient care. It is therefore important that medical schools prepare fourth-year students to use a variety of EMR systems and that hospital systems provide training well in advance of new PGY1 residents' program start day. Surveys of residency directors and residents can serve to better direct medical schools in the development of medical informatics competencies.
Appendix 1
Survey Questions
| 1. As a residency director, what level of proficiency in Electronic Medical Records (EMR) do you expect of your PGY1 (new) residents when they first arrive? Very low proficiency; Low proficiency; Moderate proficiency; High proficiency; Very high proficiency |
| 2. How many PGY1 residents do you currently have in your program? 0; 1; 2; 3; 4; 5; 6; 7; 8; 9; 10; 11; 12; 13; 14; 15; 16; 17; 18; 19; 20 or more |
| 3. How many of your PGY1 residents had experience with EMR when they first arrived? 0%; 1-25%; 26-50%; 51-75%; 76-100% |
| 4. How successful were your PGY1 residents in using the EMR at your particular hospital when they first arrived? Unsuccessful; Moderately Successful; Successful; Highly Successful |
| 5. How successful are your PGY1 residents in using the EMR today (compared to when they first arrived)? Unsuccessful; Moderately Successful; Successful; Highly Successful |
| 6. To what extent does inexperience with EMR impact patient care? No impact; Low impact; moderate impact; more than average impact; high impact |
| 7. What factors contribute to more successful use of the EMR for your PGY1 residents? Onsite hospital training; Training in podiatric medical school; Other |
| 8. Does your hospital provide onsite EMR training? Yes; No |
| 9. How satisfied are you with the hospital's EMR training? Not at all satisfied; Low level of satisfaction; Moderately satisfied; Highly satisfied |
| 10. What format of EMR training is used? Online; In-person; Classroom; One on one teaching; Other (please specify) |
| 11. How much training time on EMR is provided to new residents? Less than 1 day; 1 day; 2 days; 3 days; 4 or more days |
| 12. What system of EMR are you running at the hospital presently? Allscripts; Athena Health; Care360; Cerner; eClinical Works; EPIC; GE; Greenway; McKesson; NextGen; Optum Insight; Practice Fusion; SuccessEHS; Vista CPRS; Unsure; Other |
| 13. How satisfied are you with the hospital's EMR? Not at all satisfied; Low level of satisfaction; Moderately satisfied; Highly satisfied |
|
14. How easy is the system to use? Very difficult; Somewhat difficult; Moderately easy; Easy; Very easy |
| 15. How long has your hospital been using the current EMR? Less than a year; 1 year; 2 years; 3 years; 4 years; 5+ years; Unsure |
| 16. As a Residency Director, what recommendations would you make to podiatric medical school curricula around informatics and EMR preparation? (This was an open-ended comment item.) |
| 17. In what region of the country is your hospital residency program based? West; South; Midwest; Northeast |
Contributor Information
Rebecca Meehan, School of Information at Kent State University in Kent, OH.
Jill Kawalec, College of Podiatric Medicine at Kent State University in Kent, OH.
Bryan Caldwell, College of Podiatric Medicine at Kent State University in Kent, OH.
David Putman, College of Podiatric Medicine at Kent State University in Kent, OH.
Notes
- 1.Swain M., Charles D., Patel V., Searcy T.Health Information Exchange among U.S. Non-federal Acute Care Hospitals: 2008–2014. ONC Data Brief No. 24. Office of the National Coordinator for Health Information Technology, 2015.
- 2.Middleton B., Bloomrosen M., Dente M. A., Hashmat B., Koppel R., Overhage J.M., Payne T.H., Rosenbloom S.T., Weaver C., Zhang J. “Enhancing Patient Safety and Quality of Care by Improving the Usability of Electronic Health Record Systems: Recommendations from AMIA.”. Journal of the American Medical Informatics Association. 2013;20:e2–e8. doi: 10.1136/amiajnl-2012-001458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peled J. U., Sagher O., Morrow J.B., Dobbie A.E. “Do Electronic Health Records Help or Hinder Medical Education?”. PLoS Medicine. 2009;6 doi: 10.1371/journal.pmed.1000069. e1000069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Embi P. J., Yackel T.R., Logan J.R., Bowen J.L., Cooney T.G., Gorman P.N. “Impacts of Computerized Physician Documentation in a Teaching Hospital: Perceptions of Faculty and Resident Physicians.”. Journal of the American Medical Informatics Association. 2004;11:300–309. doi: 10.1197/jamia.M1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ibid.
- 6.Rouf E., Chumley H.S., Dobbie A.E. “Electronic Health Records in Outpatient Clinics: Perspectives of Third Year Medical Students.”. BMC Medical Education. 2008;8:8–13. doi: 10.1186/1472-6920-8-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keenan C. R., Nguyen H.H., Srinivasan M. “Electronic Medical Records and Their Impact on Resident and Medical Student Education.”. Academic Psychiatry. 2006;30:522–27. doi: 10.1176/appi.ap.30.6.522. [DOI] [PubMed] [Google Scholar]
- 8.Heiman H. L., Rasminsky S., Bierman J.A., Evans D.B., Kinner K.G., Stamos J., Martinovich Z., McGaghie W.C. “Medical Students' Observations, Practices, and Attitudes Regarding Electronic Health Record Documentation.”. Teaching and Learning in Medicine. 2014;26:49–55. doi: 10.1080/10401334.2013.857337. [DOI] [PubMed] [Google Scholar]
- 9.Thielke S., Hammond K., Helbig S. “Copying and Pasting of Examinations within the Electronic Medical Record.”. International Journal of Medical Informatics. 2007;76(suppl. 1):S122–S128. doi: 10.1016/j.ijmedinf.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 10.Heiman H. L., Rasminsky S., Bierman J.A., Evans D.B., Kinner K.G., Stamos J., Martinovich Z., McGaghie W.C. “Medical Students' Observations, Practices, and Attitudes Regarding Electronic Health Record Documentation.”. doi: 10.1080/10401334.2013.857337. [DOI] [PubMed] [Google Scholar]
- 11.Rouf E., Chumley H.S., Dobbie A.E. “Electronic Health Records in Outpatient Clinics: Perspectives of Third Year Medical Students.”. doi: 10.1186/1472-6920-8-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nuovo J., Hutchinson D., Balsbaugh T., Keenan C. “Establishing Electronic Health Record Competency Testing for First-Year Residents.”. Journal of Graduate Medical Education. 2013;5:658–61. doi: 10.4300/JGME-D-13-00013.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Asan O., Kushner K., Montague E. “Exploring Residents' Interactions with Electronic Health Records in Primary Care Encounters.”. Family Medicine. 2015;47:722–26. [PMC free article] [PubMed] [Google Scholar]
- 14.Clark M. A., Belden J.L., Kim M.S. “How Does Learnability of Primary Care Resident Physicians Increase after Seven Months of Using an Electronic Health Record? A Longitudinal Study.”. JMIR Human Factors. 2016;3:e9. doi: 10.2196/humanfactors.4601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wald H., George P., Reis S., Taylor J.S. “Electronic Health Record Training in Undergraduate Medical Education.”. Academic Medicine. 2014;89:380–86. doi: 10.1097/ACM.0000000000000131. [DOI] [PubMed] [Google Scholar]
- 16.Abrams K., Kane A., Greenspun H.“Preparing the Doctor of the Future: Medical School and Residency Program Evolution.” Deloitte Center for Health Solutions, Deloitte University Press. 2016. Available at https://dupress.deloitte.com/dup-us-en/industry/health-care/doctor-of-the-future-medical-school-residency-programs.html (accessed November 17, 2016).
- 17.Nunnally J., Bernstein L. Psychometric Theory. New York, NY: McGraw-Hill; 1994. [Google Scholar]
- 18.Asan O., Smith P., Montague E. “More Screen Time, Less Face Time—Implications for EHR Design.”. Journal of Evaluation in Clinical Practice. 2014;20:896–901. doi: 10.1111/jep.12182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rouf E., Chumley H.S., Dobbie A.E. “Electronic Health Records in Outpatient Clinics: Perspectives of Third Year Medical Students.”. doi: 10.1186/1472-6920-8-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Asan O., Kushner K., Montague E. “Exploring Residents' Interactions with Electronic Health Records in Primary Care Encounters.”. [PMC free article] [PubMed] [Google Scholar]
- 21.Clark M. A., Belden J.L., Kim M.S. “How Does Learnability of Primary Care Resident Physicians Increase after Seven Months of Using an Electronic Health Record? A Longitudinal Study.”. doi: 10.2196/humanfactors.4601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meeks D. W., Takian A., Sittig D., Singh H., Barber N. “Exploring the Sociotechnical Intersection of Patient Safety and Electronic Health Record Implementation.”. Journal of the American Medical Informatics Association. 2014;21:e28–e34. doi: 10.1136/amiajnl-2013-001762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pirnejad H., Niazkhani Z., van der Sijs H., Berg M., Bal R. “Impact of A Computerized Physician Order Entry System on Nurse-Physician Collaboration in the Medication Process.”. International Journal of Medical Informatics. 2008;77:735–44. doi: 10.1016/j.ijmedinf.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 24.Balka E., Doyle-Waters M., Lecznarowicz D., Fitzgerald J.M. “Technology, Governance and Patient Safety: Systems Issues in Technology and Patient Safety.”. International Journal of Medical Informatics. 2007;76(suppl. 1):S35–S47. doi: 10.1016/j.ijmedinf.2006.05.046. [DOI] [PubMed] [Google Scholar]
- 25.Koppel R. “Role of Computerized Physician Order Entry Systems in Facilitating Medication Errors.”. JAMA. 2005;293:1197–1203. doi: 10.1001/jama.293.10.1197. [DOI] [PubMed] [Google Scholar]
- 26.Nuovo J., Hutchinson D., Balsbaugh T., Keenan C. “Establishing Electronic Health Record Competency Testing for First-Year Residents.”. doi: 10.4300/JGME-D-13-00013.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ibid.
- 28.Wald H., George P., Reis S., Taylor J.S. “Electronic Health Record Training in Undergraduate Medical Education.”. doi: 10.1097/ACM.0000000000000131. [DOI] [PubMed] [Google Scholar]