Abstract
Documentation requirements for the Indonesian integrated antenatal care (ANC) program suggest the need for electronic systems to address gaps in existing paper documentation practices. Our goals were to quantify midwives' documentation completeness in a primary healthcare center, understand documentation challenges, develop a tool, and assess intention to use the tool. We analyzed existing ANC records in a primary healthcare center in Bangkalan, East Java, and conducted interviews with stakeholders to understand needs for an electronic system in support of ANC. Development of the web-based Electronic Integrated ANC (e-iANC) system used the System Development Life Cycle method. Training on the use of the system was held in the computer laboratory for 100 midwives chosen from four primary healthcare centers in each of five regions. The Unified Theory of Acceptance and Use of Technology (UTAUT) questionnaire was used to assess their intention to adopt e-iANC. The midwives' intention to adopt e-iANC was significantly influenced by performance expectancy, effort expectancy and facilitating conditions. Age, education level, and computer literacy did not significantly moderate the effects of performance expectancy and effort expectancy on adoption intention. The UTAUT results indicated that the factors that might influence intention to adopt e-iANC are potentially addressable. Results suggest that e-iANC might well be accepted by midwives.
Keywords: midwives, antenatal care, integrated antenatal care, Unified Theory of Acceptance and Use of Technology (UTAUT) Model
Introduction
In 2012, the Indonesian maternal mortality ratio (MMR) was 359 per 100,000 live births.1, 2 This is very high compared with that of neighboring countries, such as Singapore (3 per 100,000 live births), Malaysia (5 per 100,000 live births), Thailand (8 to 10 per 100,000 live births), and Vietnam (50 per 100,000 live births).3 Indonesian MMR is far above the target Millennium Development Goal of 102 per 100,000 live births in 2015. The Indonesian MMR has also increased in recent years, from 307 per 100,000 in 2002 to 359 per 100,000 in 2012. This increase happened despite improvements in coverage over the same period in obstetric care (92 to 98 percent), delivery by healthcare providers (66 to 83 percent), and delivery in healthcare facilities (40 to 63 percent).
In response to this situation, the Ministry of Health of the Republic of Indonesia created a national program, called Rencana Aksi Nasional Percepatan Penurunan Angka Kematian Ibu (RAN-PPAKI), or National Action Plan for Improving Mother and Child Health, containing multiple initiatives, including integrated antenatal care (ANC).4 Integrated ANC refers to comprehensive and quality ANC given to all pregnant women at every healthcare facility.5
In an integrated ANC program, healthcare providers must be able to ensure that the pregnancy is normal, to detect early problems and illnesses, and to intervene adequately so that pregnant women are ready to undergo a normal delivery. Specifically, integrated ANC refers to providing healthcare, including nutrition counseling and early detection of problems, diseases, and complications of pregnancy. Integrated care also covers preparation for safe deliveries, including early preparation for referral in case of complications.
ANC services provided by Indonesian midwives include taking vital measurements, assessing nutritional status, measuring fundal height, assessing the presentation of the fetus and fetal heart rate, screening for tetanus toxoid immunization status and giving tetanus toxoid if needed, dispensing iron supplementation tablets, ordering laboratory tests (routine and special), managing cases, and counseling.6
Midwives must complete several forms to document provision of integrated ANC, including basic medical records, detailed pregnancy-related information on a document known as a “Mother Card,” the “Mother and Child Health Handbook” (a record provided to the mother), public health reporting forms used for local and national monitoring (known as “Mother Cohort” forms), and district health reports. Data on these paper forms are often incomplete and/or inaccurate, thus limiting possibilities for quality improvement analyses.7
A national integrated ANC program was implemented throughout Indonesia in 2013, with provinces making local adaptations as necessary. One such adaptation was made in East Java to incorporate risk screening. Specifically, each pregnancy is rated during each trimester as being low, high, or very high risk.8
Our goal was to develop an electronic ANC record that would enable improved collection of risk screening and other assessment data, provide better access to health information for patients and client, and facilitate quality assessment and improvement efforts. Our development efforts were guided by an initial survey of the completeness of existing paper records and preliminary design interviews with stakeholders. We developed the Electronic Integrated ANC (e-iANC) system as a web-based graphical interface, which was presented to midwives through training sessions. The Unified Theory of Acceptance and Use of Technology (UTAUT)9, 10 was used to assess midwives' attitudes toward adoption of the system.
Methods
Survey of Records for Completeness
To understand documentation quality with existing paper forms, we examined the records of one primary health center in Bangkalan, East Java, in March 2014. Specifically, we attempted to examine integrated ANC records collected in February 2014, pertaining to 42 pregnant women. Our analyses focused on the medical record, the Mother Card, and the public health reporting forms. Documents were examined to determine whether key details were reported. Fields considered included patient identification, midwifery documentation (Subjective, Objective, Assessment, and Plan [SOAP]) including the history of the pregnancy and current condition, treatments, diagnosis, follow-up, referral of patients (if applicable), and authentication of health record entries by midwives or other healthcare providers.11, 12
Stakeholder Interviews
The Joint Commission model identifies several key principles for information management, including the following:
Needs assessment,
Planning and designing,
Capturing and reporting,
Processing and analyzing,
Storing and retrieving,
Dissemination and display, and
Information use.13
To understand user needs for an electronic ANC system, we conducted in-depth interviews with representatives of key stakeholder perspectives.14, 15 Seven informants were interviewed:
the head of the Indonesian Sub-Directorate of Maternal and Child Health, in the Directorate of Maternal and Child Health and Nutrition,
the head of the Health Services Section of the East Java provincial health office,
the head of the Family Health Section of the East Java provincial health office,
the head of the Indonesian Midwives Association of East Java,
the head of the Bangkalan primary health center,
the Midwives Coordinator from the Bangkalan primary health center, and
a midwife.
Semistructured interviews included questions discussing integrated ANC data sources; the collection, processing, analysis, and reporting of Integrated ANC data; stakeholder perceptions of integrated ANC data quality; the impact of data quality on maternal health; and expectations of an electronic ANC record. Content analysis techniques16, 17 were used to interpret the interview responses.
E-iANC Development and Design
We used the System Development Life Cycle (SDLC) method to guide the development of e-iANC. Steps in this method are as follows:
Identify problems, opportunities, and objectives;
Determine the information needs;
Analyze the system requirements;
Design the recommended system;
Develop and document software;
Test and maintain the system; and
The prototype e-iANC information system was built as a web-based application using PHP 5 and JavaScript, a Firebird database (www.firebirdsql.org), and an Apache web server. All components are open-source.
Training and Measurement of Intention to Adopt e-iANC
To assess prospects for broad adoption of e-iANC, we trained midwives in the use of the system and then used the UTAUT survey to assess their intention to adopt the tool.
Training was provided in computer labs to 100 midwives working in primary health centers in five districts/cities in East Java. Specifically, four primary health centers were identified in each of the five districts, for a total of 20 health centers. Five midwives from each of these 20 centers participated, for a total of 100 midwives. All participants were involved in integrated ANC at least part time, and all provided informed consent.
After attending the training, all respondents completed a questionnaire containing sociodemographic items such as age, educational level, and computer literacy. Seventeen questions were based on the UTAUT model (including the domains of performance expectancy [PE]; effort expectancy [EE]; social influence [SI]; facilitating conditions [FC]; and behavior intention [BI])20, 21 as adapted by Yu.22 Because our goal was to measure intention to adopt the tool and respondents had not yet used the tool, the usage behavior (UB) questions were omitted. The response scale for all UTAUT items was a six-point scale, ranging from 1 (extremely unlikely) to 6 (extremely likely).
Statistical analyses were carried out with SPSS software and the SmartPLS 3.0 software package. Descriptive statistics (frequency and percentages) were used to analyze the distribution of the sociodemographic factors. As in prior UTAUT analyses, the partial least squares (PLS) method was used to test the model.23, 24, 25
Results
Record Completeness
Records for 42 visits were examined during a single visit to a primary health center in February 2014. Mother Cards were available for only 15 (37.5 percent) of these visits. Of the 15 available Mother Cards, only five (33.3 percent) were recorded in the Mother Cohort. None of the 15 Mother Cards listed the names of the midwives or healthcare providers, but three (20 percent) did include signatures. Only one of the 15 Mother Cards listed a medical record number, and 11 (73 percent) had incomplete midwifery information. Further details are presented in Table 1.
Table 1.
Antenatal Care Record Completeness in a Primary Health Center, February 2014 (n = 15)
| Components of Record Completeness | Complete | Not Complete | |||
|---|---|---|---|---|---|
| Frequency | Percentage (%) | Frequency | Percentage (%) | ||
| Patient identification | Name | 15 | 100.0 | 0 | 0.0 |
| Medical record number | 1 | 6.7 | 14 | 93.3 | |
| Midwifery documentation | Subjective | 4 | 26.7 | 11 | 73.3 |
| Objective | 4 | 26.7 | 11 | 73.3 | |
| Assessment | 4 | 26.7 | 11 | 73.3 | |
| Plan | 4 | 26.7 | 11 | 73.3 | |
| Midwives' authentication | Name | 0 | 0.0 | 15 | 100.0 |
| Signature | 3 | 20.0 | 12 | 80.0 | |
Stakeholder Interviews
Identification of Problems, Objectives, and Opportunities for 2e-iANC
Our interviews identified several difficulties with the paper-based integrated ANC processes at a primary health center in East Java, including redundancy in ANC data, leading to inconsistencies; difficulties in using and interpreting paper records, leading to delays in risk screening and service interventions; delays in accessing data; and inaccurate calculation and data analysis.
Participants found the integrated ANC forms to be burdensome and redundant. Some felt that completion of the forms interfered with providing necessary antenatal care:
“Frankly, I forget to record the data of pregnant women after conducting integrated ANC because [there are] too many forms to be filled, despite the same data.” (Informant 6)
“I sometimes give more priority to assuring the antenatal service and forget about the recording of data.” (Informant 7)
Informants also indicated that district health reporting requirements presented a burden. Primary health centers must implement district health reporting policies. Although this process has been computerized, all tasks are currently completed with commodity software (spreadsheets and word processors):
“In fact we want to do it with computerization, but we only run district health office policies, still using the existing software spreadsheet alone.” (Informants 5 and 6)
“Still manual applications (spreadsheets and word).” (Informant 7)
The need to manually count and collate information from paper forms was seen as delaying local area monitoring, leading to inaccuracies in screening risk scores and delaying antenatal care interventions.
“The information generated at this time only meets the needs that have been established according to the report of PWS, i.e., K1, K4 [district health reporting requirements] and birth attendants, and often too late.” (Informants 1 and 5)
Participants responded enthusiastically to the suggestion of an electronic ANC system:
“If there is an application that can generate necessary information on ANC, we would be delighted.” (Informants 2 and 3)
“Today midwives' duties are doing many reports. If only there were an application for generating mother cohort and PWS reports more easily, we would be very happy.” (Informants 3 and 4)
“Once we made a software application named ‘Kartini,’ but today many provinces are not using it, since each province has made an application according to its needs. If only there were applications that could replace Kartini and could be used by all midwives, we would certainly support this.” (Informant 1)
Requirements and Needs in the Design of e-iANC
Our goal in designing and developing e-iANC was to build a system that would computerize the capture of pertinent health information, both for use in individual care provision and for aggregate reporting. Perceived benefits of such a system included faster screening for pregnancy risks, faster antenatal care interventions, quick and accurate generation of Mother Cohort reports, and real-time generation of district health reports.
Our informants identified several key functions that should be included in the electronic ANC tool: registration; anamnesis; physical examination; communication, information, and education (CIE); treatment; diagnosis; and follow-up of pregnant women. Three tasks were identified as being of highest priority:
pregnancy risk factor screening,
Mother Cohort reporting, and
district health reporting.
Functional requirements include availability via a wired local area network (LAN).
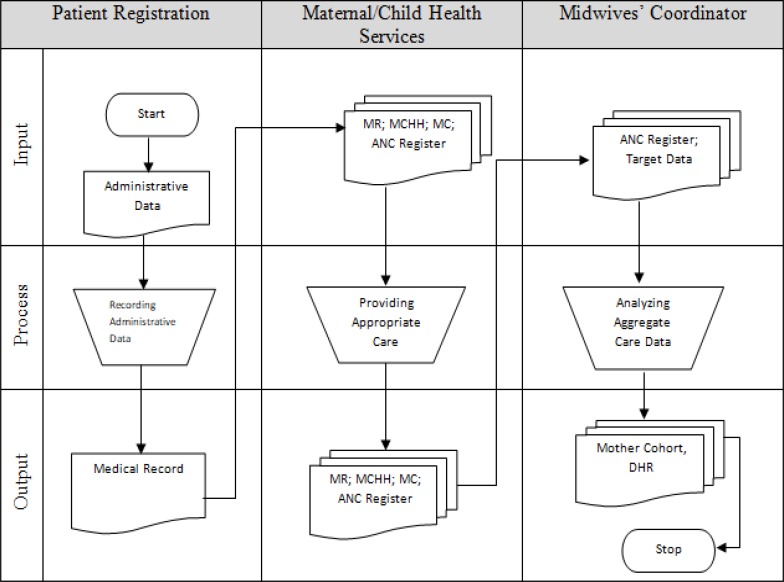
The data flow diagram in Figure 1 depicts the current paper-based integrated antenatal workflow, as described by interviewees. Responses divided the workflow into three discrete stages: administrative data collection, clinical data collection, and coordination/public health reporting. Administrative data collected during patient registration includes demographics, identification, and payment information. Administrative processes also include assignment of a unique medical record number to each patient. Administrative data are both recorded in the patient's medical record and sent to Maternal/Child Health Services. Clinical data collected during patient visits includes SOAP and CIE regarding the delivery plan, tetanus toxoid immunization, early initiation of breastfeeding, exclusive breastfeeding, nutritional problems, family planning, HIV/AIDS and other infectious diseases, and domestic violence. Administrative and clinical data were also recorded in the Mother and Child Health Handbook and the ANC register. The register is used as an input by the midwives' coordinator, who creates Mother Cohorts and the district health reports for dissemination to the head of the primary health center and the district health office.
Figure 1.
Integrated Antenatal Care Data Flow Diagram in a Primary Health Center
Abbreviations: ANC, antenatal care; DHR, District Health Reporting; MC: Mother Card; MCHH, Mother and Child Health Handbook.
Note: “Target Data” refers to the annual reporting of data on pregnant women by the District Health Official, consisting of the total number of pregnant women in each rural area, including high-risk pregnant and maternal women.
Features of e-iANC
The e-iANC system is a web-based information system designed to assist midwives in recording integrated ANC data, including patient registration; anamnesis and physical examination; treatment; diagnosis; and follow-up advice and service. Individual and aggregate data can be employed for clinical service and organization decision making, research, performance improvement, and education.
The following are the features of e-iANC:
Patient Registration: enabling entry of demographic and financial sources data, including whether a patient pays in cash or is financed by the Healthcare and Social Security Agency (see Figure 2).
Anamnesis, including history of current or previous pregnancy as well as labor history, as needed to identify high-risk patients. The first day of the last menstrual period is used to estimate the expected date of birth.
Physical Examination: results of physical examinations, including vital signs used to detect early pregnancy risks, such as cephalopelvic disproportion, preeclampsia, and other conditions.
Laboratory Results: Urine protein, hepatitis B surface antigen (HBsAg), mycobacterium tuberculosis, and other tests, as medically indicated.
Screening of Risk of Pregnancy: Described as low, high, or very high risk.
Communication, Information, and Education (CIE): Education materials related to factors such as delivery planning, nutritional problems, tetanus toxoid immunization, HIV/AIDS and other communicable diseases, exclusive breastfeeding, and other topics.
Treatment and Follow-up: Key treatments administered, including injection of tetanus toxoid and the provision of multivitamins. Midwives can enter the number and doses defined and administration instructions.
Patient Disposition: Follow-up instructions including discharge or referral if necessary to other healthcare providers or healthcare facilities with more complete equipment.
Diagnosis: Entry of specific antenatal diagnoses, using ICD-10 codes as required to process claims for reimbursement.
Graphical Representation of the Maternal Weight and Body Mass Index (BMI): Can be used to monitor maternal weight before for each visit. This novel visualization of health information was seen as necessary to expedite.
Reports: Display and printing of Mother Cohort and district health reports on rural and primary health centers. Reports are available both to midwives and to the head of the primary health center.
Figure 2.
Master Patient Index for Patient Registration
Note: Information listed is for display purposes only and not from an actual patient.
Adoption Intention
The return rate for the questionnaire was 100 percent. Of the 100 respondents, more than one-third (37 percent) were younger than 30 years of age, 40 percent were between 31 and 40 years of age, 21 percent were between 41 and 50 years of age, and 2 percent were older than 50 years of age. Sixty-five percent of respondents had obtained a three-year diploma, with the remainder having completed a four-year bachelor's degree. Sixty-one percent described themselves as computer literate. Further information is presented in Table 2.
Table 2.
Sociodemographic Characteristics of Respondents (n = 100)
| Category | Number of Respondents | Percentage (%) | |
|---|---|---|---|
| Age | Less than 20 years | 0 | 0 |
| 20–30 years | 37 | 37 | |
| 31–40 years | 40 | 40 | |
| 41–50 years | 21 | 21 | |
| More than 50 years | 2 | 2 | |
| Education level | Diploma (3 years) | 65 | 65 |
| Bachelor's degree (4 years) | 35 | 35 | |
| Computer literacy | No | 39 | 39 |
| Yes | 61 | 61 |
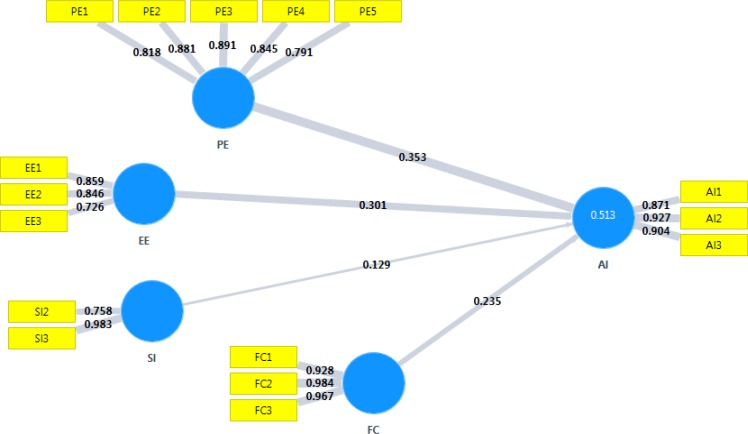
The data analysis was conducted in two stages with the use of SmartPLS. In the first stage, the reliability and validity of the constructs were assessed to ensure the appropriateness of the measurement model, and in the second stage, the structural model was assessed.26, 27
The convergent validity of reflective constructs was assessed by determining if the loadings on the expected constructs were high enough.28 As shown in Table 3, all item loadings were higher than 0.70, suggesting good convergent validity of the constructs. Examination of the social influence construct revealed a loading of −0.523 for the first item. After this item was removed, the loading of the remaining social influence scores SI2 and SI3 increased to 0.758 and 0.983. Discriminant validity can be assessed by testing whether the square roots of average variance extracted (AVE) are greater than the correlations.29, 30 All correlations were below the square roots of the AVEs, indicating that the constructs had good discriminant validity (see Table 4).
Table 3.
Loading Factors, Composite Reliability, and Average Variance Extracted of Constructs and Cronbach's Alpha
| Constructs | Indicators | Loading Factors | Composite Reliability | Average Variance Extracted | Cronbach's Alpha |
|---|---|---|---|---|---|
| Performance expectancy (PE) | PE1 PE2 PE3 PE4 PE5 |
0.818 0.881 0.891 0.845 0.791 |
0.926 | 0.715 | 0.901 |
| Effort expectancy (EE) | EE1 EE2 EE3 |
0.859 0.846 0.726 |
0.853 | 0.660 | 0.742 |
| Social influence (SI) | SI1 SI1 SI2 |
−0.523a 0.750 – 0.758 0.937 – 0.983 |
0.868 | 0.770 | 0.768 |
| Facilitating conditions (FC) | FC1 FC2 FC3 |
0.928 0.984 0.967 |
0.972 | 0.921 | 0.957 |
| Adoption intention (AI) | AI1 AI2 AI3 |
0.871 0.927 0.904 |
0.928 | 0.812 | 0.884 |
Examination of the social influence construct revealed a loading of −0.523 for the first item. After this item was removed, the loading of the remaining social influence scores SI2 and SI3 increased to 0.758 and 0.983.
Table 4.
Correlation and Discriminant Validity
| Constructs | Correlation and Discriminant Validity | ||||
|---|---|---|---|---|---|
| AI | EE | FC | PE | SI | |
| AI | 0.901 | ||||
| EE | 0.566 | 0.812 | |||
| FC | 0.430 | 0.252 | 0.960 | ||
| PE | 0.581 | 0.500 | 0.269 | 0.846 | |
| SI | 0.281 | 0.228 | 0.190 | 0.110 | 0.877 |
Abbreviations: AI, adoption intention; EE, effort expectancy; FC, facilitating conditions; PE, performance expectancy; SI, social influence.
Composite reliability (CR), AVE, and Cronbach's alpha values were used to assess the reliability of reflective constructs.31, 32, 33, 34 As shown in Table 3, values of CR (0.853–0.972), AVE (0.660–0.921) and Cronbach's alpha (0.742–0.957) were all considerably above the suggested values of 0.80, 0.50, and 0.60 respectively, thus satisfying the criteria for reliability.
The structural model was assessed by checking the significance of path coefficients (β) between different factors. As illustrated in Table 5, the results showed that except for the relationship between social influences, all other proposed relationships with adoption intention were significant. Specifically, the results indicated that effort expectancy, facilitating conditions, and performance expectancy have a significant positive effect on adoption intention (β = 0.301, β = 0.235, and β=0.353, respectively; all p < 0.01). These factors fully explained 51.3% of variance of adoption intention, as shown in Figure 3.
Table 5.
Path Coefficients
| Constructs | β | Sample Mean | Standard Error | T Statistic | P Values |
|---|---|---|---|---|---|
| EE-AI | 0.301 | 0.307 | 0.089 | 3.376 | 0.001 |
| FC-AI | 0.235 | 0.238 | 0.080 | 2.934 | 0.004 |
| PE-AI | 0.353 | 0.350 | 0.081 | 4.371 | 0.000 |
| SI-AI | 0.129 | 0.132 | 0.075 | 1.716 | 0.087 |
Abbreviations: AI, adoption intention; EE, effort expectancy; FC, facilitating conditions; PE, performance expectancy; SI, social influence.
Figure 3.
R-Squared in Model of Adoption Intention for the Electronic Integrated Antenatal Care System
Abbreviations: AI, adoption intention; EE, effort expectancy; FC, facilitating conditions; PE, performance expectancy; SI, social influence.
The moderating effects of age, level of education, and computer literacy were examined through the significance of path coefficients as identified through multigroup analysis. None of these moderators had a significant effect on the contribution of performance expectancy and effort expectancy to adoption intention (p > 0.05), with the sole exception of education level, which had a marginally moderating effect on the influence of performance expectancy on adoption intention (p = 0.050). Further information is presented in Table 6.
Table 6.
Path Coefficients in Multigroup Analysis
| Moderator Variable | Constructs | Path-Coefficients Difference | P Values | |
|---|---|---|---|---|
| Education Level | Diploma vs. bachelor's degree | EE-AI | 0.239 | 0.904 |
| FC-AI | 0.056 | 0.632 | ||
| PE-AI | 0.314 | 0.050 | ||
| SI-AI | 0.095 | 0.708 | ||
| Age | <33 years vs. ≥33 years | EE-AI | 0.227 | 0.095 |
| FC-AI | 0.008 | 0.522 | ||
| PE-AI | 0.179 | 0.858 | ||
| SI-AI | 0.003 | 0.472 | ||
| Computer Literacy | No vs. yes | EE-AI | 0.084 | 0.665 |
| FC-AI | 0.110 | 0.239 | ||
| PE-AI | 0.186 | 0.856 | ||
| SI-AI | 0.182 | 0.126 | ||
Abbreviations: AI, adoption intention; EE, effort expectancy; FC, facilitating conditions; PE, performance expectancy; SI, social influence.
Discussion
Main Findings
The Indonesian government's integrated ANC program suggests a coordinated program to combat maternal mortality. All participating health providers are expected to collaborate in the conduct of ANC, including key processes such as anamnesis; physical and diagnostic examination; treatment and follow-up; data capture; and communication, information and education.35
Appropriate recording of patient data is a critical for encouraging all healthcare providers, particularly midwives at primary health centers, to communicate and exchange treatment details. Because midwives play a central role in this process, their acceptance of the ANC procedures and participation in the documentation of care is both critical for the success of ANC and required by law.
Our examinations of paper recording practices found that records were incomplete and often unnecessarily duplicated. Of 42 integrated ANC records that we attempted to examine, only 15 (37.5 percent) had an available Mother Card. Of those 15 Mother Cards, only four (27.6 percent) contained complete documentation of midwifery. None of the 15 Mother Cards listed the names of the midwives or healthcare providers, but three (20 percent) did include signatures. Although this small sample may not be representative of the entire population of maternal records included in these clinics, we expect that similar patterns of low rates of documentation adherence would be found at other, comparable clinics.
Midwives and other informants confirmed in the in-depth interviews that they felt that several of the ANC forms repeated data elements, leading to frequent duplication and omission as midwives often forgot to record ANC data. Our examination of the flow of ANC data in the primary health center (see Figure 1) identified multiple data recording redundancies, raising concerns about the validity of the data that can be used to monitor and measure the success of an integrated ANC program. These concerns motivated the development of the e-iANC electronic record.
Our development of this tool was informed by discussion with users. After building the tool, we trained users and examined their intention to adopt the system. Results provide preliminary support for our tool, with performance expectancy, effort expectancy, and facilitating conditions exhibiting positive effects on midwives' intention to adopt the e-iANC system. Performance expectancy was the most powerful factor influencing the intention to adopt e-iANC, in accordance with earlier studies.36, 37, 38, 39, 40 The effort expectancy affecting midwives' intention to adopt e-iANC is also consistent with previous work.41, 42, 43, 44, 45
Discussions with midwives after training also identified enthusiasm for the tool. Midwives stated that they felt it would facilitate their work. Tools for electronic calculation of pregnancy risk were noted as being particularly important. Automated district health reporting was also seen as a significant benefit that might reduce errors in calculating ANC coverage indicators.
Our results suggest that facilitating conditions influence midwives' intention to adopt e-iANC. This is consistent without studies linking facilitating conditions to behavior intention,46, 47, 48 despite the absence of such a connection in the original UTAUT model.49 Midwives participating in our study identified several facilitating conditions, including adequate internet access and usage guidelines that would be easy to learn independently.
In contrast to some prior work,50, 51, 52, 53, 54 our results did not show any significant impact of social influences on intention to adopt e-iANC or on behavior intention. However, our study is consistent with other previous work.55, 56 These results suggest that midwives have individually accepted the importance of e-iANC and that social motivators may not be necessary to encourage adoption.
Moderator age, education level, and computer literacy did not show any influence on the intention to adopt e-iANC, suggesting that e-iANC might be accepted by all groups of users. These results support a broader trial planned for healthcare centers in five districts/cities. Selected samples of midwives at these locations will be measured with complete UTAUT models, including usage behavior (UB).
The current e-iANC implementation is designed to be used not only by midwives but also by other healthcare providers contributing to the integrated ANC program, including doctors, nutritionists, and other care providers. Future plans include possible adoption of e-iANC midwife education, providing all midwives with training in providing electronic documentation and creating midwifery reports. Further future possibilities include implementations of the e-iANC system for mobile devices, possibly including features that might be used by pregnant women to assess their condition and access their own health information more easily.
Because this preliminary study focused only on midwives' acceptance of e-iANC, adoption costs and related economic benefits have not been explored. As all software components are open-source, there are no acquisition costs, leaving maintenance of computing hardware and connectivity as the main ongoing expense. A thorough cost-benefit analysis, including an examination of ongoing maintenance costs necessary for sustained use, would be an appropriate area for future work.
Because the design of e-iANC was informed by investigation of processes and information needs in a particular care context in Indonesia, the extent to which the design might be generalized to contexts with different policies and requirements is unclear. Elements of the system design regarding specific Indonesian regulatory requirements would almost certainly need to be reconsidered and redesigned for adoption in other countries. However, the development process described above, and the measurement of intention to adopt the system, provide a methodology that might be used to guide the revision of this tool for other contexts.
Limitations
The inclusion of records from only one clinic limits the generalizability of any claims regarding completeness of ANC records. Laboratory results from the UTAUT measures may fail to accurately predict actual adoption. Because the assessments occurred prior to any actual deployment, the UTAUT model included constructs measuring performance expectancy, effort expectancy, social influence, facilitating conditions, and behavior intention (adoption intention), but does not measure the construct of “usage behavior” in relation to e-iANC. Although the participation of midwives from five health centers does not provide a representative sample of Indonesian midwives, the selected centers represented a range of socioeconomic conditions.
Conclusion
The incomplete recording of ANC data, the need to improve data quality, and the adoption of information communication technology in healthcare motivated our decision to design and develop the e-iANC system. Interviews with midwives identified difficulties in processes and documentation that might be addressed through this computerization of the process. Our implementation of e-iANC includes features for registration; history and physical examination; laboratory tests; pregnancy risk screening; treatment; communication, information, and education; diagnosis; and documentation of patient disposition (dismissal or referral). Outputs from e-iANC include both individual reports and aggregate reports for both patient management and public health. Performance expectancy, effort expectancy, and facilitating conditions significantly impacted intention to adopt and suggest that e-iANC might be accepted by all groups of users. Planned implementation of the system in the five districts assessed and measurement with complete UTAUT models will provide insight into the use of the tool and additional understanding of users' intention.
Conflicts of Interest
The authors report no conflicts of interest.
Acknowledgments
We thank the respondents for their time and efforts in participating in the study. We also thank the Directorate General of Higher Education and the Ministry of Research Technology and Higher Education of Indonesia for the chance to engage in Peningkatan Kualitas Publikasi Internasional scholarships in the Department of Biomedical Informatics at the University of Pittsburgh, in Pittsburgh, PA.
Contributor Information
Hosizah Markam, Health Information Management Department at Universitas Esa Unggul in Jakarta, Indonesia.
Harry Hochheiser, Department of Biomedical Informatics at the University of Pittsburgh in Pittsburgh, PA.
Kuntoro Kuntoro, Department of Public Health Science at Universitas Airlangga in Surabaya, Indonesia.
Hari Basuki Notobroto, Department of Biostatistics at Universitas Airlangga in Surabaya, Indonesia.
Notes
- 1.Statistics Indonesia (Badan Pusat Statistik [BPS]), National Population and Family Planning Board (BKKBN), and Kementerian Kesehatan (Kemenkes), and ICF International . Indonesia Demographic and Health Survey 2012. Jakarta, Indonesia: BPS, BKKBN, Kemenkes, and ICF International; 2013. [Google Scholar]
- 2.Ministry of Health, Republic of Indonesia, Directorate General of Mother-Child Health and Nutrition Development. Guidelines Integrated Antenatal Care. 2nd ed. 2013.
- 3.Hartanto W. “Indonesian Maternal Mortality Rate the Highest in ASEAN.”. National Population and Family Planning Board (BKKBN); 2013. [Google Scholar]
- 4.Ministry of Health, Republic of Indonesia “Ministry of Health Release RAN-PPAKI 2013–2015, RAN-PPIA 2013–2017 and Mother Health Care Handbook at Health Care Facilities.” 2013. Available at http://www.depkes.go.id/article/view/2417/menkes-luncurkan-ran-ppaki-2013–2015-ran-ppia-2013–2017-dan-buku-saku-pelayanan-kesehatan-ibu-di-fas.html
- 5.Ministry of Health, Republic of Indonesia, Directorate General of Mother-Child Health and Nutrition Development Guidelines Integrated Antenatal Care. 2nd ed.
- 6.Ibid.
- 7.Ibid.
- 8.Rochjati P. Screening of Risk Pregnancy Poedji Rochjati Method. Surabaya, Indonesia: Airlangga Press; 2002. pp. 65–73. [Google Scholar]
- 9.Venkatesh V., Morris M.G., Davis F.D., Davis G.B. “User Acceptance of Information Technology: Toward a Unified View.”. MIS Quarterly. 2003;27(3):425–78. [Google Scholar]
- 10.Venkatesh V., Moris M.G., Davis F.D., Davis G.B. ”A Theoretical Extension of the Technology Acceptance Model: Four Longitudinal Field Studies.”. Management Science Journal. 2000;46(2):186–204. [Google Scholar]
- 11.Russo R. “Best Practice in Health Records Documentation.”. In: Fahrenholz C. G., Russo R., editors. Documentation for Health Records. 2nd ed. Chicago, IL: American Health Information Management Association (AHIMA); 2013. [Google Scholar]
- 12.Johnson D. L., Spielman C.M. “Data and Information Management.”. In: LaTour K. M., Maki S. E., editors. Health Information Management: Concepts, Principles and Practice. 3rd ed. Chicago, IL: American Health Information Management Association; 2010. pp. 111–142. [Google Scholar]
- 13.Ibid.
- 14.Kendal K. E., Kendal J. E. Systems Analysis and Design. 8th ed. Upper Saddle River, NJ: Pearson; 2011. pp. 31–42. [Google Scholar]
- 15.Amatayakul M. A. “Health Information Systems Strategic Planning.”. In: Oachs P. K., Watters A. L., editors. Health Information Management: Concepts, Principles, and Practice. 5th ed. Chicago, IL: American Health Information Management Association; 2016. pp. 385–421. [Google Scholar]
- 16.Lazar J., Feng J. H., Hochheiser H. Research Methods in Human-Computer Interaction. Chichester, UK: Wiley; 2010. pp. 206–213. [Google Scholar]
- 17.Forrestal E. “Research Methods.”. In: Oachs P. K., Watters A. L., editors. Health Information Management: Concepts, Principles, and Practice. 5th ed. Chicago, IL: American Health Information Management Association; 2016. pp. 563–606. [Google Scholar]
- 18.Kendal K. E., Kendal J. E.Systems Analysis and Design. 8th ed.
- 19.Amatayakul M. A. “Health Information Systems Strategic Planning.”.
- 20.Venkatesh V., Morris M. G., Davis F. D., Davis G. B. “User Acceptance of Information Technology: Toward a Unified View.”.
- 21.Venkatesh V., Moris M. G., Davis F. D., Davis G. B. ”A Theoretical Extension of the Technology Acceptance Model: Four Longitudinal Field Studies.”.
- 22.Yu C.S. “Factors Affecting Individuals to Adopt Mobile Banking: Empirical Evidence from the UTAUT Model.”. Journal of Electronic Commerce Research. 2012;13(2):104–21. [Google Scholar]
- 23.Hair J. F., Hult G. T. M., Ringle C. M., Sarstedt M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM). Thousand Oaks, CA: Sage; 2014. [Google Scholar]
- 24.Fillion G., Braham H., Ekionea J.P.B. “Testing UTAUT on the Use of ERP Systems by Middle Managers and End-Users of Medium-to Large-Sized Canadian Enterprises.”. Academy of Information and Management Sciences Journal. 2012;15(2):1–28. [Google Scholar]
- 25.Sun Y., Wang N., Guo X., Peng Z. “Understanding the Acceptance of Mobile Health Services: A Comparison and Integration of Alternative Models.”. Journal of Electronic Commerce Research. 2013;14(2):183–200. [Google Scholar]
- 26.Hair J. F., Hult G. T. M., Ringle C. M., Sarstedt M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM).
- 27.Sun Y., Wang N., Guo X., Peng Z. “Understanding the Acceptance of Mobile Health Services: A Comparison and Integration of Alternative Models.”.
- 28.Yu C. S. “Factors Affecting Individuals to Adopt Mobile Banking: Empirical Evidence from the UTAUT Model.”.
- 29.Ibid.
- 30.Yu L. W., Tao Y.H., Yang P.C. “The Use of Unified Theory of Acceptance and Use of Technology to Confer the Behavioral Model of 3G Mobile Telecommunication Users.”. Journal of Statistics & Management Systems. 2008;11(5):919–49. [Google Scholar]
- 31.Hair J. F., Hult G. T. M., Ringle C. M., Sarstedt M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM).
- 32.Fillion G., Braham H., Ekionea J. P. B. “Testing UTAUT on the Use of ERP Systems by Middle Managers and End-Users of Medium-to Large-Sized Canadian Enterprises.”.
- 33.Zhou T. “Examining Location-Based Services (LBS) Usage from the Perspectives of Unified Theory of Acceptance and Use of Technology and Privacy Risk.”. Journal of Electronic Commerce Research. 2012;13(2):135–44. [Google Scholar]
- 34.Kijsanayotin B., Pannarunothai S., Speedie S.M. “Factors Influencing Health Information Technology Adoption in Thailand's Community Health Centers (CHCs): Applying the UTAUT Model.”. International Journal of Medical Informatics. 2009;78:404–16. doi: 10.1016/j.ijmedinf.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 35.Hartanto W. “Indonesian Maternal Mortality Rate the Highest in ASEAN.”.
- 36.Yu L. W., Tao Y. H., Yang P. C. “The Use of Unified Theory of Acceptance and Use of Technology to Confer the Behavioral Model of 3G Mobile Telecommunication Users.”.
- 37.Trimmer K., Cellucci L.W., Wiggins C., Woodhouse W. “Electronic Medical Records: TAM, UTAUT and Culture.”. International Journal of Healthcare Information Systems and Informatics. 2009;4(3):55–68. [Google Scholar]
- 38.Tibenderana P., Ogao P., Odongo J.I., Wokadala J. “Measuring Levels of End-Users' Acceptance and Use of Hybrid Library Services.”. International Journal of Education and Development Using Information and Communication Technology (IJEDICT) 2010;6(2):33–54. [Google Scholar]
- 39.Dino M. J. S., Guzman A.B. “Using Partial Least Squares (PLS) in Predicting Behavioral Intention for Telehealth Use among Filipino Elderly.”. Educational Gerontology. 2015;41:53–68. [Google Scholar]
- 40.Van Houwelingen C. T. M., Barakat A., Best R., Boot W.R., Charness N., Kort H.S.M. “Dutch Nurses' Willingness to Use Home Telehealth.”. Journal of Gerontological Nursing. 2015;41(4):47–56. doi: 10.3928/00989134-20141203-01. [DOI] [PubMed] [Google Scholar]
- 41.Zhou T. “Examining Location-Based Services (LBS) Usage from the Perspectives of Unified Theory of Acceptance and Use of Technology and Privacy Risk.”.
- 42.Trimmer K., Cellucci L. W., Wiggins C., Woodhouse W. “Electronic Medical Records: TAM, UTAUT and Culture.”.
- 43.Tibenderana P., Ogao P., Odongo J. I., Wokadala J. “Measuring Levels of End-Users' Acceptance and Use of Hybrid Library Services.”.
- 44.Dino M. J. S., Guzman A. B. “Using Partial Least Squares (PLS) in Predicting Behavioral Intention for Telehealth Use among Filipino Elderly.”.
- 45.Van Houwelingen C. T. M., Barakat A., Best R., Boot W. R., Charness N., Kort H. S. M. “Dutch Nurses' Willingness to Use Home Telehealth.”. [DOI] [PubMed]
- 46.Yu L. W., Tao Y. H., Yang P. C. “The Use of Unified Theory of Acceptance and Use of Technology to Confer the Behavioral Model of 3G Mobile Telecommunication Users.”.
- 47.Tibenderana P., Ogao P., Odongo J. I., Wokadala J. “Measuring Levels of End-Users' Acceptance and Use of Hybrid Library Services.”.
- 48.Moghavvemi S., Salleh N.A.M., Zhao W., Mattila M. “The Entrepreneur's Perception on Information Technology Innovation Adoption: An Empirical Analysis of the Role of Precipitating Events on Usage Behavior.”. Innovation: Management, Policy & Practice. 2012;14(2):231–46. [Google Scholar]
- 49.Venkatesh V., Morris M. G., Davis F. D., Davis G. B. “User Acceptance of Information Technology: Toward a Unified View.”.
- 50.Sun Y., Wang N., Guo X., Peng Z. “Understanding the Acceptance of Mobile Health Services: A Comparison and Integration of Alternative Models.”.
- 51.Yu C.S. “Factors Affecting Individuals to Adopt Mobile Banking: Empirical Evidence from the UTAUT Model.” [Google Scholar]
- 52.Yu L. W., Tao Y.H., Yang P.C. “The Use of Unified Theory of Acceptance and Use of Technology to Confer the Behavioral Model of 3G Mobile Telecommunication Users.” [Google Scholar]
- 53.Zhou T. “Examining Location-Based Services (LBS) Usage from the Perspectives of Unified Theory of Acceptance and Use of Technology and Privacy Risk.” [Google Scholar]
- 54.Tibenderana P., Ogao P., Odongo J.I., Wokadala J. “Measuring Levels of End-Users' Acceptance and Use of Hybrid Library Services.” [Google Scholar]
- 55.Zahra A., Kanwal F., Rehman M., Bashir K. “An Empirical Investigation of E-learning Adoption in Nursing Education of Pakistan.”. International Journal of Computer Science and Information Security. 2016;14(11):611–21. [Google Scholar]
- 56.Kusyanti A., Ma'ruf A.K.M. “The Role of Privacy Concerns and Trust in User Acceptance of Instant Messaging Usage Intention.”. International Journal of Computer Science and Information Security. 2016;14(12):584–88. [Google Scholar]