Abstract
Objective. To evaluate pharmacists’ knowledge of celiac disease, and identify potential areas where additional continuing education may be needed.
Methods. A survey was sent to community pharmacists practicing in a national chain pharmacy in one region of New Jersey and New York.
Results. There were 418 pharmacists who responded to the survey with a response rate of 38%. Only 27% of all respondents who reported their understanding of celiac disease to be basic or advanced correctly defined celiac disease as both an autoimmune and a chronic lifelong disease. The majority (60%) of respondents correctly stated there are no federal regulations requiring manufacturers to designate medications as gluten-free. Twenty percent of respondents said they often recommended a change in diet to people suspected to have celiac disease before a confirmed diagnosis.
Conclusion. Community pharmacists possess some knowledge of the disease and would benefit from and desire additional education about this disorder.
Keywords: celiac, pharmacists, community
INTRODUCTION
Celiac disease is an important chronic autoimmune disease that is estimated to affect 1% of the U.S. population.1 This disorder is often overlooked or misdiagnosed, potentially leading to decreased quality of life for individuals with the disease and an increase in health care costs. People with celiac disease have a genetic intolerance to gluten and must therefore maintain a strict lifelong gluten-free lifestyle totally avoiding any ingestion of wheat, barley or rye. Although the major site of injury in celiac disease is the small intestine, resulting in various gastrointestinal problems, ingesting gluten by these patients may also result in a wide variety of other clinical manifestations including vitamin and other nutritional deficiencies, systemic inflammatory reactions, other autoimmune diseases, serious types of cancer and other illnesses.2 Pharmacists can play a key role in assisting patients with celiac disease by helping to identify people who may have the disease, providing information about gluten-free pharmaceutical products and food, and encouraging patients to maintain a gluten-free diet after diagnosis.3
Pharmacists have consistently been viewed as one of the most trusted health care professionals. Community pharmacists are also recognized as one of the most accessible health care providers. It is also noteworthy that for several consecutive years pharmacists have been highly ranked as ethical and honest professionals. In 2016, they were the second top ranked profession for honesty and ethics.4
Researchers have demonstrated that community pharmacists, working in collaboration with other health care providers, have helped to decrease readmission rates and reduce the number of medication-related problems experienced by patients with various disorders and have a positive impact on improving overall patient outcomes.5-7 For example, pharmacists with competent knowledge on celiac disease can potentially prevent and help patients and other health care providers identify complications from the disease which may lead to hospitalizations, readmissions and a decreased quality of life for patients.
Knowledgeable pharmacists can help patients to more effectively manage their medical conditions, which may potentially lower risks of disease-related complications and health care costs. Interventions led by community pharmacists have demonstrated to help patients with specific chronic diseases achieve better outcomes.8-10 While several continuing education programs on celiac disease do exist, the level of pharmacist knowledge regarding this disease specifically was never assessed in previous studies.
The objective of this study is to evaluate the extent of community pharmacists’ self-assessed and actual knowledge about celiac disease and to identify areas where additional training may be needed.
METHODS
This is an exploratory study designed to examine the perceived vs actual level of knowledge of celiac disease among community pharmacists. The survey was developed by faculty colleagues with clinical expertise in celiac disease, community pharmacy practice and Medication Therapy Management as well as a candidate in her final professional year of the doctor of pharmacy program. Survey questions were based on common facts on celiac disease published by Beyond Celiac (formerly known as the National Foundation for Celiac Awareness) and the American Society of Health-System Pharmacists and were further identified through accredited continuing education programs intended for pharmacists on celiac disease and other peer- reviewed publications.4,5
The questionnaire was pretested by a pharmacy faculty member who was not participating in the study and a senior pharmacist employed by the participating chain pharmacy. The survey instrument was then further developed and distributed using SurveyMonkey (San Mateo, CA) with the assistance of the college’s Office of Assessment. The study was approved by the St. John’s University Institutional Review Board.
Several national chain community pharmacies were invited to have their pharmacists participate in the study, of which one agreed to participate and requested to remain anonymous. A link to the survey instrument was electronically sent to individual pharmacists who practiced within one region of the chain pharmacy in New York and New Jersey in February 2014. Pharmacists received follow-up reminders to participate in the study one month later and then again approximately 6 weeks after the initial survey link was sent. An email with a brief description of the survey purpose, and information regarding the anonymity of participants was also sent. Participation was voluntary and consent was implied by completing the survey.
Responses to the survey questions were not limited to one answer to determine a participant’s full comprehension of the survey item. For a participant to be deemed correct in answering a question, they had to successfully identify all possible correct answers for that question and exclude any incorrect information. For example, participants had to identify all the ingredients a patient with celiac disease needs to avoid, from the list provided, to be considered correct. In another example, participants were considered to be correct if they were able to identify all of the main factors in the diagnosis of the disease.11 The resources that were used to develop the questions were also used to identify the correct responses to the survey questions. Key search terms used were celiac, pharmacy, pharmaceutical, pharmacist and treatment3,12-15
Based on their self-reported understanding of the disease, participants were categorized into two study groups: poor/limited or basic/advanced. Those who indicated their understanding to be poor or limited are referred to as the “PL” group. These individuals are considered lacking adequate knowledge about the disease as compared to those who indicated their understanding to be basic or advanced, referred to as the “BA” group. A comparison of the pharmacists’ self-assessed level of understanding and their actual knowledge and awareness of the disease was performed using Chi-Square testing. The survey data were analyzed using SAS 9.3 (SAS Institute, Cary, NC).
RESULTS
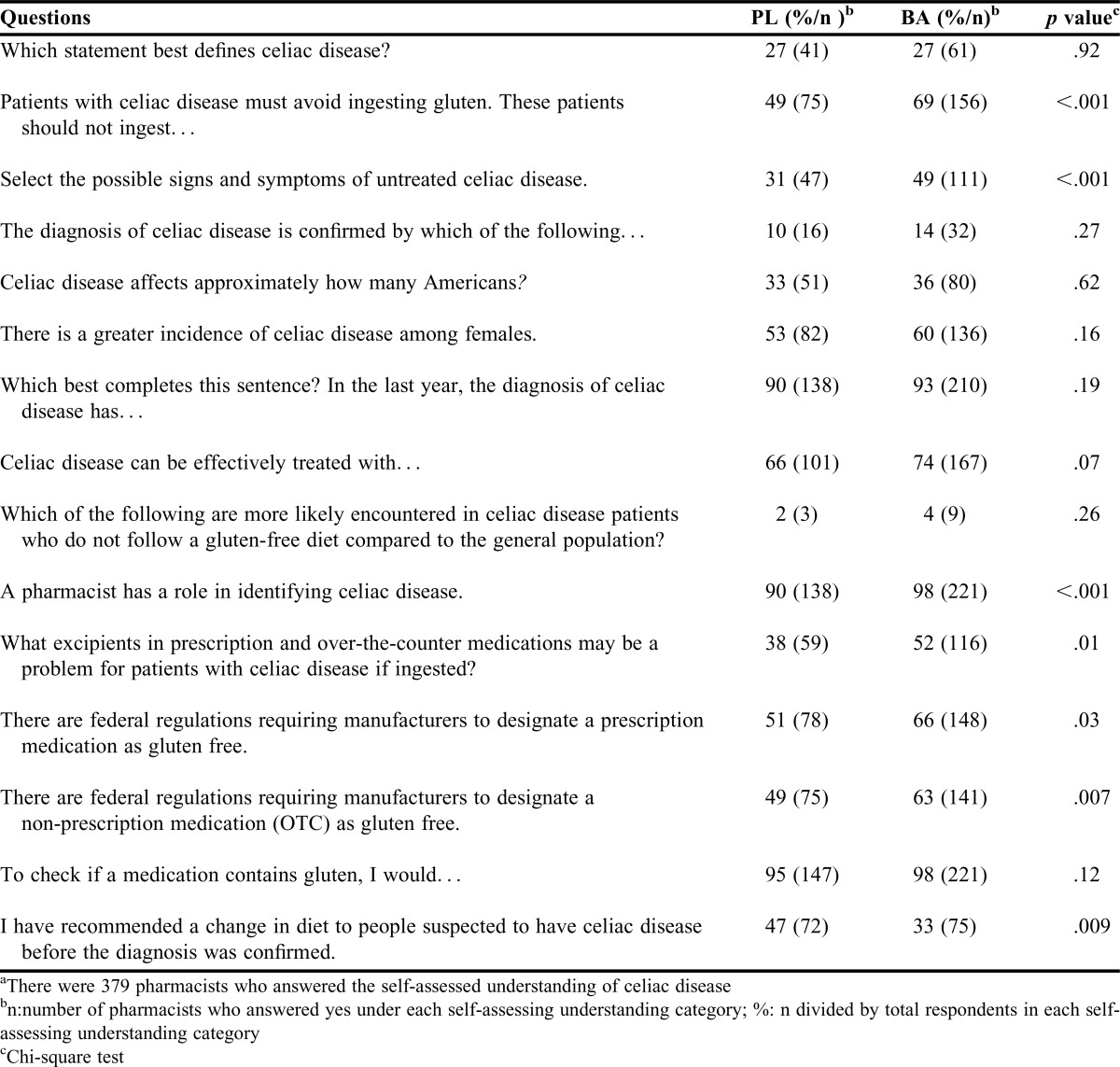
There were 418 community pharmacists who completed the survey for a response rate of 38%. These pharmacists practiced in a total of 308 pharmacies located in five counties of New Jersey and eight counties in New York. The demographic characteristics of the participants are listed in Table 1. Slightly higher than 90% of all participants (n=379) provided their self-reported level of understanding of celiac disease. Approximately 59% of respondents (n=225) considered their level of understanding to be basic or advanced, while 41% (n=154) of respondents considered their level to be limited or poor. The analysis based on this classification is provided in Table 2.
Table1.
Demographics of all Survey Respondents (N=418)
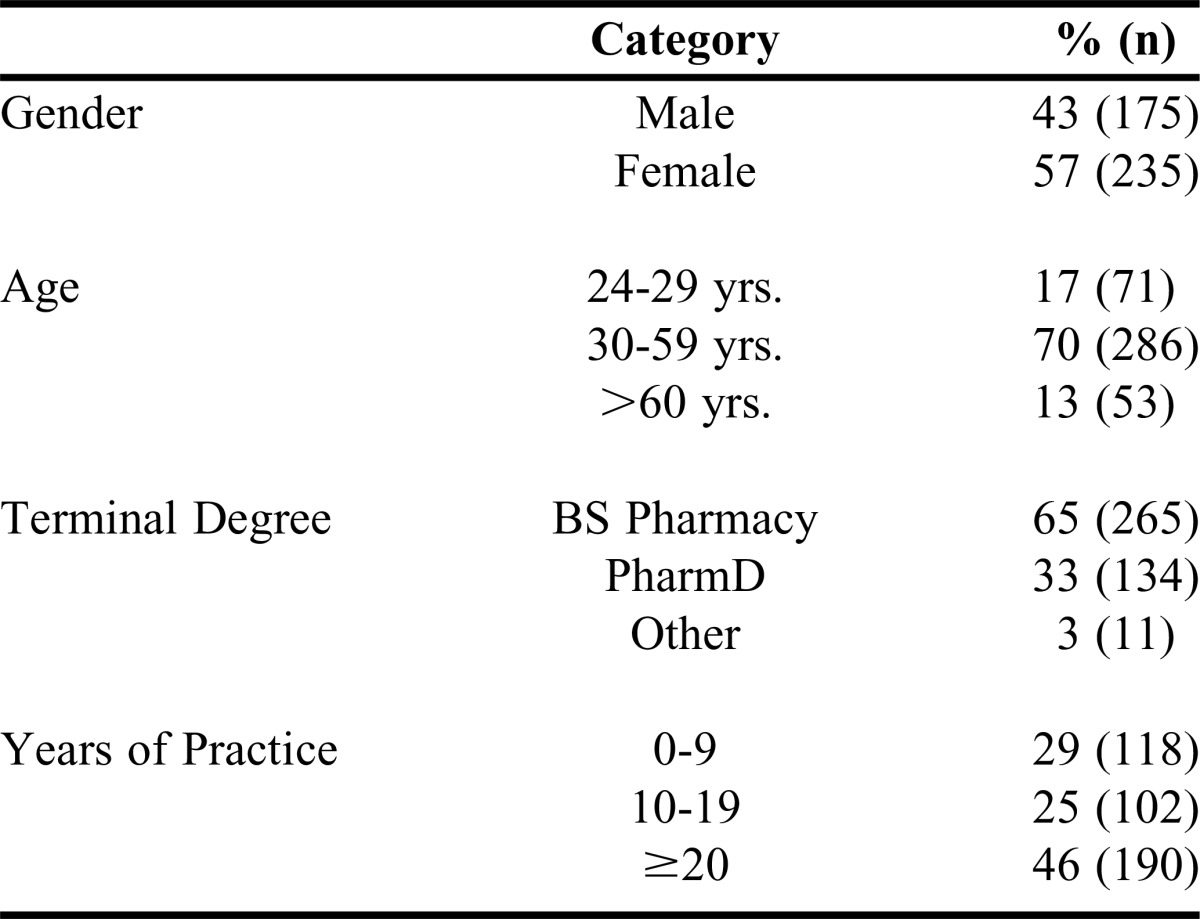
Table 2.
Responses of Community Pharmacists Who Self-Reported with Poor/Limited (PL) vs Basic/Advanced (BA) Understanding of Celiac Disease (N=379)a
When asked to select which statements best define celiac disease, the responses from both the PL and BA group demonstrated similar poor knowledge. Only 27% of pharmacists in the two study groups correctly selected both statements “it is an autoimmune disease” and “it is a chronic lifelong disease.” The survey asked the pharmacists to identify which ingredients patients with celiac disease must avoid ingesting. The BA group (62%) showed a higher proportion of correct responses compared to the PL group (39%) (p <.001).
When asked if pharmacists had a role in identifying celiac disease, 95% (n=353) of all respondents to this question agreed that pharmacists have a role in identifying the disease. Only 41.69% of all pharmacists correctly identified all the signs and symptoms of untreated celiac disease from the list provided (ie, chronic fatigue, skin rash, weight loss, abdominal pain and diarrhea). The least identified potential sign or symptom among all respondents was skin rash. The pharmacists in the BA group (49%) demonstrated increased knowledge (p<.001) compared to those in the PL group (31%).
Of all respondents (61.21%), regardless of study group, chose the incorrect responses stating that they recommended a change in diet to people suspected with celiac disease before the diagnosis was confirmed. More pharmacists in the PL group 47% (n=72 of 154) compared to the BA group 33% (n=75 of 225) reported never recommending a change in diet to those suspected to have the disease before the diagnosis was confirmed (p=.008). Nearly all respondents (98%) included maintaining a gluten-free diet as an effective way of treating celiac disease in their responses. However, only 71% of the respondents correctly indicated maintaining a gluten-free diet alone as the effective treatment of celiac disease. Approximately one-fourth, 22.30%, of all pharmacists who responded to this question included “celiac disease-specific medications” in their response as an effective way to treat this disorder. Among the two study groups, only 13% of respondents correctly selected both endoscopy with biopsy and response to changes in diet or these two factors along with serological testing as ways to confirm celiac disease in a patient.
When asked to identify complications most likely encountered by patients with celiac disease who do not follow a gluten-free diet compared to the general population, only 3% of participants in both groups correctly selected all the listed complications: cancer, chronic diarrhea, damage to the intestine, decreased medication absorption and nutritional deficiencies. Cancer was included by only 30% of the participants in their response to this question.
Approximately three-fifths of all respondents accurately recognized that there are no federal regulations requiring manufacturers to designate a prescription (59.47%) or non-prescription medication (56.84%) as gluten-free. Within the study groups, pharmacists in the BA group demonstrated better knowledge than those in the PL group regarding federal regulations requiring manufacturers to designate prescription and non-prescription medications as gluten-free (p=.032, p=.007 respectively). Fifty-two percent (n=116) of respondents in the BA group correctly selected natural flavoring and/or starch of unknown origin as excipients in non-prescription and prescription medications that may be a problem for patients with celiac disease if ingested. Comparatively, only 38% of pharmacists in the PL group where able to correctly identify the excipients that may pose a problem (p=.011).
When asked how they would check if a medication contains gluten, the three top responses selected by all respondents included contact the manufacturer, check the package insert or look at the bottle labeling. Among all respondents, approximately 46% stated all three. There was no significant difference between the studied groups (BA 54%, PL 47% respectively p=.153). A participant was correct if they did not include “refer the patient to their doctor” and/or “ask the patient to check on their own” in their response (Table 2). Less than 3% of participants in the study groups included these two choices. There was no significant difference among the groups (p=.12).
There was also no significant difference between the study groups in response to the definition, diagnosis, incidence, prevalence or effective treatment of celiac disease. Over 90% of all respondents correctly recognized that the frequency with which patients are diagnosed with celiac has increased in the past year. In contrast, only 35% of respondents correctly recognized that celiac disease occurs in approximately 1 in every 100 Americans. Fifty-eight percent of all respondents correctly indicated that celiac disease occurs more frequently among females. In the open-ended portion of the survey, many pharmacists expressed an interest in continuing education programs specific to celiac disease and the correct responses to the survey questions.
DISCUSSION
While many pharmacists were able to recognize the most common facts pertaining to celiac disease, the study demonstrated that there is a need for additional education and training regardless of the pharmacists’ self-reported level of understanding about the disease. Participants who self-reported their understanding of the disease to be basic or advanced did, overall, perform better in correct responses to our assessment questions. Although the BA group performed better than the PL group, numerous times less than 50% of the BA group was able to correctly respond to survey questions about the disease, its impact on patients and the care they should receive.
Less than half (49.33%) of the participants in the BA group were able to identify the potential signs and symptoms of the disease despite the majority (94.72%) of all participants agreeing pharmacists have a role in identifying the disease. Nearly all of the pharmacists (97.13%) did include the most common complications associated with the disease included in this survey; however, only 3% of the participants were able to identify all correct potential conditions associated with untreated celiac disease. Cancer, which is a known and potential consequence of improperly treated or undiagnosed celiac disease, was selected by only one-third of respondents to this question. There was no significant differences between the two groups (PL 2%, BA 4%, p=.263). Both groups showed poor knowledge in this area which indicates a need for further education. Being aware of all the potential complications of untreated celiac disease may help pharmacists realize the importance of identifying and avoiding the ingestion of gluten from any source.
Regardless of the self-reported understanding, the majority (73.09%) of respondents were not able to identify the comprehensive definition of the disease or its prevalence. The majority (86.84%) of all respondents were able to specify some of the key signs and symptoms of celiac disease including abdominal pain and diarrhea. However, less than half (39.47%) were able to correctly identify all the correct signs and symptoms of the disease included in this survey. This may compromise the effective care the pharmacist could provide to these patients, both in screening for undiagnosed patients who have the disease or assisting patients post-diagnosis.
It is concerning that only 39% of all respondents in both groups studied said they never recommended a change in diet to people suspected to have celiac disease before the diagnosis was confirmed. Interestingly, according to survey responses more pharmacists in the BA group stated they would recommend a diet change before a diagnosis was made compared to the PL group. After providing some fundamental patient information on the disease or its diagnosis, suspected patients should be encouraged to seek appropriate follow-up before implementing a gluten-free diet or self-treating their symptoms. Starting a gluten-free diet prior to a confirmed diagnosis is not recommended as this may cause false negative diagnostic test results. A false negative result may delay or prevent an accurate diagnosis from being made and will predispose the patient to disease-related complications and other illnesses.
Sixty percent of respondents were aware that (at the time of this study) there are no federal regulations requiring manufacturers to designate a prescription or non-prescription medication as gluten-free. While both checking the package insert and/or looking at the bottle labeling would be correct in trying to identify if a medication contains gluten, these two actions alone may not be sufficient. Additionally, not all pharmacists surveyed were able to correctly identify all excipients in prescription and over-the-counter medications may be a problem for patients with celiac disease if ingested. Contacting the manufacturer may be the best way to obtain the needed information.
It is interesting that although there are no drugs currently on the market that are approved by the FDA with the specific indication to treat celiac disease at this time, almost a quarter of respondents included, “celiac disease-specific medications” in their response as an effective way to treat this disorder, further identifying a continuing education opportunity.
Due to their high degree of accessibility and the level of trust bestowed upon them, community pharmacists are in an ideal position to identify and refer suspected celiac disease patients for early medical attention for a proper diagnosis. Community pharmacists should consider discussing celiac disease with patients seeking or purchasing products for the treatment of chronic gastrointestinal symptoms or presenting with signs and symptoms of the disorder. Pharmacists are also in an ideal position to help patients already diagnosed identify and avoid harmful ingredients found in both prescription and over-the-counter medications and products.
Due to the increasing importance of celiac disease and other forms of gluten intolerance, pharmacy schools should determine to what degree information about this important autoimmune disease, and how the pharmacist can assist patients with this disorder, is included in their curriculum. The 2016 American College of Clinical Pharmacy Pharmacotherapy Didactic Curriculum Toolkit now includes celiac disease as a suggested topic to be covered in the curriculum. Celiac disease is listed as a tier 3 competency-based tier. Compared to tier 1 and 2, a tier 3 item is assigned less emphasis in developing a curriculum.16 However, celiac disease was not included at all in the previous 2009 toolkit.17 One can conclude there is an increasing need for knowledge in the treatment and management of celiac disease than in the past. Since celiac disease is an autoimmune disease that affects the small intestine and results in nutritional deficiencies as well as other systemic manifestations and these patients are often encountered in an ambulatory care or community pharmacy setting, discussions about celiac disease could be included in many areas of the pharmacy curriculum including courses focusing on immunology, gastroenterology, ambulatory care and/or community pharmacy practice. This study identified a knowledge gap among practicing community pharmacists on this autoimmune disease. The results of this study may serve to support the need for development in this area within the curriculum. This study also may serve to determine objectives for specific continuing education programs on celiac disease.
Although pharmacists are not directly involved in the diagnosis of the disease, it would be beneficial if they understood how a patient is diagnosed to enable them to provide more effective patient education. It is generally agreed that the diagnosis of celiac disease depends on three main factors, positive celiac panel blood test, positive small bowel biopsy and remission of symptoms on a gluten-free diet after testing is complete.11
To optimize care for patients with celiac disease, a pharmacist’s actual knowledge of the disease should surpass poor or basic levels, regardless of their perceived knowledge. Through further training and education on this disorder, we would expect community pharmacists to be capable to identify 100% of the correct responses to the survey as well as feel confident in assisting patients with the disease.
The results of this study are specific to only one geographic division within one chain pharmacy. Further studies are needed examining a larger group of pharmacists’ understanding of celiac disease. The authors recognize comprehensive pilot testing of survey questions was not performed. However, the study is exploratory in nature, and was reviewed by selected individuals in the field. We adopted a conservative approach to assess the comprehensive understanding of pharmacist knowledge regarding the disease or measures to cope with the disease. All respondents had to answer correctly on all items based on the literature and expert opinions to be considered correct. We believe this is an important factor to ensure patient safety would not be compromised even if it seems to be a stringent criterion to assess a pharmacist’s knowledge.
CONCLUSION
Celiac disease is a common chronic autoimmune disease that is often overlooked or misdiagnosed. The results of this study suggest that although pharmacists in the BA group performed better than those in the PL group, pharmacists surveyed would benefit from, and expressed an interest in, receiving additional education about this disorder. The four main areas in need of additional education identified in this study are in the etiology and diagnosis of the disease, complications of untreated celiac disease and the role that the pharmacist may play in the management of celiac disease. Practicing pharmacists may therefore benefit from continuing professional education coursework designed to enhance their knowledge about this chronic disorder and how they can best assist patients suspected of having celiac disease or who have been diagnosed with this disorder.
ACKNOWLEDGMENTS
The authors would like to acknowledge the following members of St John’s University for their contributions to the study. Anthony Marziliano, the Department of Assessment, for his assistance with Survey Monkey; Tazruba Kabir, PharmD, for her assistance in researching survey questions as a student pharmacist; Dr. Somnath Pal, professor of Pharmacy Administration and Health Sciences for his initial input in the data analysis.
REFERENCES
- 1.Green PH. Mortality in celiac disease, intestinal inflammation, and gluten sensitivity. JAMA. 2009;302(11):1225–1226. doi: 10.1001/jama.281.24.2344. [DOI] [PubMed] [Google Scholar]
- 2.Chiu JG, Shin Y, Patel PN, Mangione RA. Gluten content of barium sulfate suspensions used for barium swallows in patients with celiac disease. Radiol Technol. 2014;86(1):11–16. [PubMed] [Google Scholar]
- 3.Mangione RA, Patel PN. Caring for patients with celiac disease: the role of the pharmacist. J Am Pharm Assoc. 2008;48(5):e125–135. doi: 10.1331/JAPhA.2008.08014. [DOI] [PubMed] [Google Scholar]
- 4.Honesty/Ethics in Professions. http://www.gallup.com/poll/200057/americans-rate-healthcare-providers-high-honesty-ethics.aspx . Accessed February 21, 2017.
- 5.Cardwell TB, Bean R. 2011 Pharmacist provides telephone-based medication reconciliation and education to recently discharged patients, leading to fewer readmissions. Agency for Healthcare Research and Quality; 2011.
- 6.Arnold ME, Buys L, Fullas F. Impact of pharmacist intervention in conjunction with outpatient physician follow-up visits after hospital discharge on readmission rate. Am J Health Syst Pharm. 2015;72(11 Suppl 1):S36–S42. doi: 10.2146/sp150011. [DOI] [PubMed] [Google Scholar]
- 7.Kalista T, Lemay V, Cohen L. Postdischarge community pharmacist-provided home services for patients after hospitalization for heart failure. J Am Pharm Assoc (2003) 2015;55(4):438–442. doi: 10.1331/JAPhA.2015.14235. [DOI] [PubMed] [Google Scholar]
- 8.Cheema E, Sutcliffe P, Singer DRJ. The impact of interventions by pharmacists in community pharmacies on control of hypertension: a systematic review and meta-analysis of randomized control trails. Br J Clin Pharmcol. 2014;78(6):1238–1247. doi: 10.1111/bcp.12452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Santschi V, Chiolero A, Colosimo AL, et al. Improving blood pressure control through pharmacists interventions: a meta-analysis of randomized control trails. J Am Heart Assoc. 2014;3:e000718. doi: 10.1161/JAHA.113.000718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nemerovski CW, Young M, Mariani N, Bugdalski-Stutrud C, Moser LR. Project ImPACT: hypertension outcomes of a pharmacist-provided hypertension service. Innov Pharm. 2013;4(3) Article 126. [Google Scholar]
- 11.Celiac Support Association. Celiac disease facts. https://www.csaceliacs.org/celiacdiseasefacts.jsp. Accessed June 24, 2016.
- 12.National Foundation for Celiac Awareness. Celiac disease: fast facts. http://www.celiaccentral.org/celiac-disease/facts-and-figures. Accessed September 29, 2014.
- 13.National Foundation for Celiac Awareness and the American Society of Health-System Pharmacists. What is celiac disease? http://www.celiaccentral.org/SiteData/docs/NFCA%20Glute/09662d869bb02629/NFCA%20Gluten%20in%20Medications%20Guide.pdf. September 29, 2014.
- 14.Mangione RA, Patel PN. Pharmaceutical care of celiac disease. US Pharm. 2011;36(12):30–33. [Google Scholar]
- 15.Petkewicz K, Hines E, Wilhelm M. Helping patients manage celiac disease. CE Drug Store News. http://www.cedrugstorenews.com/userapp/lessons/lesson_view_ui.cfm?lessonuid=0401-0000-11-006-H01-P. Accessed September 29, 2014.
- 16.Schwinghammer TL, Crannage AJ, Boyce EG, et al. The 2016 ACCP Pharmacotherapy Didactic Curriculum Toolkit. Pharmacotherapy. 2016;36:e189–e194. doi: 10.1002/phar.1846. https://www.accp.com/docs/positions/misc/Toolkit_final.pdf Accessed June 8, 2017. [DOI] [PubMed] [Google Scholar]
- 17.Slain D, Wong-Berringer A, Blake B, et al. American College of Clinical Pharmacy. Pharmacotherapy Didactic Curriculum Toolkit 2009. https://www.accp.com/docs/positions/misc/PharmacotherapyToolkit.pdf Accessed June 8, 2017.