Abstract
Background:
Catheter - associated urinary tract infection (CAUTI) remains a critical threat for patients in intensive care unit especially in traumatic brain injury patients with low Glasgow coma score (GCS). Almost all patients in ICU receive antibiotic either prophylactic or therapeutic based on local antibiogram of particular ICU or hospital. For prophylaxis, systemic antibiotics are used. It will be helpful to avoid systemic side effects by introducing antibiotics locally through bladder irrigation. The indwelling urinary catheter is an essential part of modern medical care.
Aims and Objectives:
The primary objective was to study the effect of Neomycin and Polymyxin sulphate solution for bladder wash on CAUTI in traumatic brain injury patients. The secondary objectives was to study the various organisms causing CAUTI and their antibiotic sensitivity and resistance pattern.
Materials and Methods:
This was a prospective randomized controlled study performed on 100 patients who met the inclusion criteria at the trauma intensive care unit of Banaras Hindu University between September and February 2016. The patients were randomized into two groups – one was the study group which received Neomycin and Polymyxin Sulphate solution bladder wash, while the other was the control group that received Normal saline bladder wash. Urine samples were collected at certain days and sent for culture and sensitivity.
Results:
There was significant reduction in the incidence of CAUTI in neomycin/polymyxin test group in comparison to normal saline irrigated control group. Out of 50 patients in test group 8 patients and in control group 26 patients was identified as CAUTI positive and they were statistically significant. In our study pseudomonas aeruginosa (51%) was the commonest isolated pathogen.
Conclusions:
Neomycin and Polymyxin Sulphate bladder wash was effective in preventing CAUTI. It can thus decrease the antibiotic usage thereby preventing the emergence of antibiotic resistance.
Key Words: Catheter-associated urinary tract infection, neomycin and polymyxin sulfate bladder irrigation, traumatic brain injury
INTRODUCTION
Catheter associated urinary tract infection (CAUTI) remains a critical threat for patients in Intensive Care Unit (ICU), especially in traumatic brain injury patients with low Glasgow coma score (GCS). Almost all patients in ICU receive antibiotic either prophylactic or therapeutic based on local antibiogram of particular ICU or hospital. However, prophylaxis of urinary tract infection (UTI) with systemic antibiotics or sporadic antibiotic treatment of asymptomatic bacteriuria should be avoided because these interventions have little effect on prevention of symptomatic UTI and may increases colonization with antimicrobial-resistant bacteria.[1,2,3,4,5,6] Nosocomial infections such as CAUTI and ventilator associated pneumonia (VAP) are the most common. CAUTI comprising more than 40% of all institutionally acquired infections.[7,8,9,10,11] The systemic antibiotic used for prophylaxis of CAUTI have side effects which are further deleterious on various organ system in critically ill compromised patients.
It will be helpful to avoid systemic side effects of antibiotics using it locally through bladder irrigation. The indwelling urinary catheter is a routine part of ICU care, especially in patient of low GCS for urine output monitoring. Neomycin-polymyxin combination is bactericidal and active in vitro against Enterobacteriaceae, Pseudomonas aeruginosa, and Staphylococcus aureus, but it is not active against Serratia marcescens, streptococci, and enterococci. Neomycin-Polymyxin when irrigated to the bladder are poorly absorbed systemically and less likely to produce toxic side effects and resistant bacteria. We performed an extensive review of literature which did not reveal any study done on the effectiveness of Neomycin-Polymyxin combination bladder wash in traumatic brain injury patients admitted to ICU. We hypothesized that neomycin-polymyxin bladder wash reduces the incidence of CAUTI and resistant bacteria.
The primary objective was to study the effect of Neomycin and Polymyxin sulphate solution for bladder wash on CAUTI in traumatic brain injury patients. The secondary objectives was to study the various organisms causing CAUTI and their antibiotic sensitivity and resistance pattern.
MATERIAL AND METHODS
After institutional ethical approval and written informed consent, 100 patient of traumatic brain injury, aged 20–65 years, admitted to trauma intensive care were included in this prospective randomized study between September 2015 and February 2016. All patient that catheterized within 24 hours were included in our study and on meeting the inclusion criteria they were randomly divided into two groups of 50 each: Group I: Received bladder washes with normal saline and Group II: To receive bladder washes with neomycin and polymyxin sulfate solution. Patient with history of pregnancy, immunocompromized patients (AIDS, chemotherapy), diabetes, recurrent UTI, renal insufficiency, use of antibiotics within the previous 7 days and catheter removed before the 3rd day were excluded from the study.
Sampling technique
Urine samples was collected after 24 h of admission and transported immediately for culture in microbiology laboratory according to hospital protocol. Urine culture sensitivity was performed on days 3, 7, and then weekly until the removal of catheter or discharge. We made our diagnosis of CAUTI based on findings of bacteriuria, along with an elevated white blood cell count on a urinalysis examination, but in our study, the diagnosis of CAUTI was only made when the urine culture shows 105 colony-forming units/mL of urine from a catheterized patient. Urine samples were taken from the distal end of the catheter after disinfection with 70% ethyl alcohol.
Bladder irrigation
Under strict aseptic and antiseptic precaution the irrigation procedure involved disconnecting the catheter tubing, attaching a syringe containing 30 mL of irrigant, and pushing the plunger of the syringe to instil the solution into the bladder through the foleys catheter where it remained for 20 min. The syringe was disconnected, and the catheter was reconnected to the tubing of the bag. Both test and control group, patients were subjected to bladder wash twice daily. Both groups received standard catheter care including perineal care; the only difference was the bladder wash.
Statistical analysis
A prospective sample size calculation indicated that 45 patients were required in each group to have a 80% power to detect a 25% difference at an type I (α) error of 0.05 for finding CAUTI in patient undergoing with or without bladder wash and assuming a drop out of 5%, fifty patients was included in each study group. Statistical analysis was performed using Microsoft ® Excel ® 2016 (Redmond, WA, U.S.A) and SPSS version 10.0 (SPSS Inc., Chicago, Illinois, USA). Range and median was used for all continuous variables having nonnormal distribution (age and duration of catheterization) and the two groups was compared using Mann–Whitney U-test. For continuous variables having normal distribution, data was summarized using mean ± standard deviation, and the groups was compared using independent t-test. Frequency and percentage was used for all categorical variables and the groups were compared using Pearson's Chi-square test with Yates correction and Fisher's exact test. A probability of <0.05 was considered as statistically significant.
RESULTS
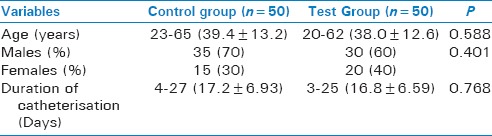
The incidence of CAUTI in our ICU is ranging from 20% to 60%. All head injury patient admitted to trauma ICU were catheterized according to protocol. All patients admitted during the study period were screened for eligibility with a target of 100 patients. In our study the demographic variables was comparable in both control and test group in respect to age, Sex and duration of catheterisation and was statistically insignificant.(p>0.05) [Table 1].
Table 1.
Demographic variables
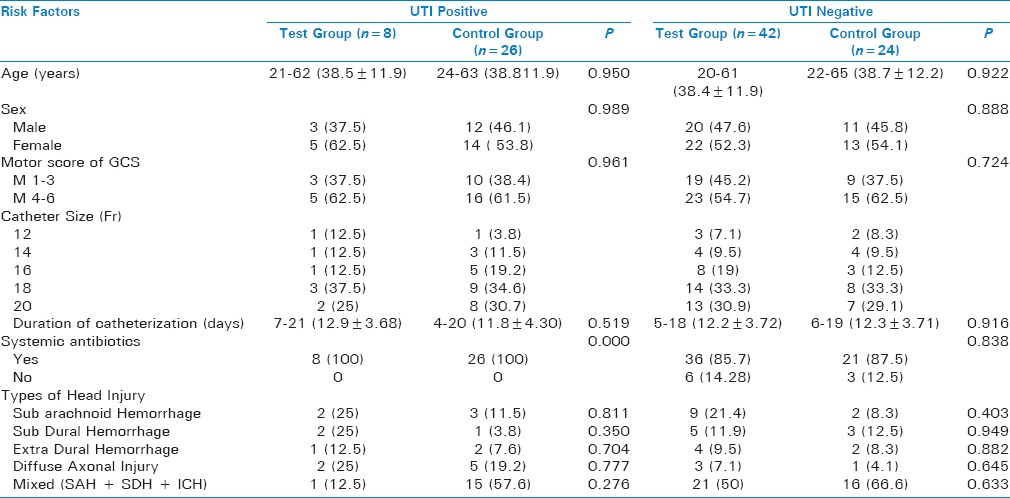
There was a significant reduction in the incidence of CAUTI in neomycin/polymyxin test group in comparison to normal saline irrigated control group. In our study on comparing several risks factors like Motor score of GCS, Foley's Catheter size (Fr), Use of systemic antibiotics and types of Head injury in both UTI positive (Test and Control) groups and UTI negative (Test and Control) groups we observed no statistical significant difference.(p> 0.05) (Table 2). On comparing among total of fifty patients in test group (UTI positive and UTI negative) only 8 and in control group(UTI positive and UTI Negative) only 26 patients was CAUTI positive and statistically significant difference exists between two group [Table 2].
Table 2.
Risk factors for catheter.associated urinary tract infection (n=100)
P. aeruginosa was the most common organism responsible for 51% of CAUTI followed by Escherichia coli and Klebsiella [Figure 1]. Isolated organisms were universally sensitive to polymyxin. Other antibiotics sensitivity was piperacillin-tazobactam, amikacin, and cefeperazone-salbactum All organisms including multidrug resistant was sensitive to polymyxin. Few isolated organism was sensitive to polymyxin only.
Figure 1.
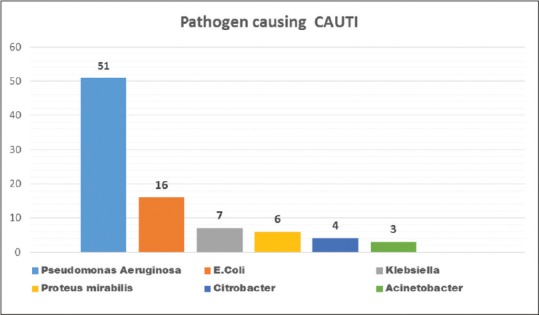
Pathogens causing catheter associated urinary tract infection
DISCUSSION
As far as our literature search is concern this is the first study which compared the effect of neomycin-polymyxin sulfate solution for bladder wash, especially in patient of traumatic brain injury admitted to ICU. An efficiency of bladder irrigation using various different solutions have been studied in the past in an attempt to reduce the incidence of CAUTI, majority of the investigators found it to be a time-consuming and costly procedure that did not have an impact on CAUTI.[12,13,14,15,16] In contrast, this study revealed that neomycin-polymyxin sulfate solution bladder wash is effective in preventing CAUTI. In previous studies, the incidence of CAUTI ranged from 11.0% to 73.3%.[16,17] Neomycin and polymyxin are the only antimicrobial agents sold commercially in the United States as a urinary bladder irrigant. This combination is bactericidal and active in vitro against several members of the Enterobacteriaceae, P. aeruginosa, and S. aureus, but it is not active against S. marcescens, streptococci, and enterococci. The fact that these antibiotics are poorly absorbed systemically in the absence of compromised renal function makes this solution potentially less likely to generate resistant bacteria or induce toxic side effects than other agents. However, both of these agents are known to produce toxic effects when administered systemically, especially ototoxicity and nephrotoxicity. However, study by Puri et al. concluded that the risk was significantly higher for females, elderly patients, critically ill patients, and those on prolonged catheterization.[18] This study showed only severity of the disease (low motor score of GCS) as a statistically significant risk factor. This might be since a lower GCS corresponds to the severity of tissue injury, where there is hyper metabolism and increased protein catabolism, which eventually leads to decreased immunity that makes the person more susceptible to infections. However, the present study did not show any influence of sex, age, catheter size, duration of catheterization, and systemic use of antibiotics. This might be due to the small sample size and inclusion of long-term catheterized patient's only pathogenic organisms responsible for CAUTI and their antibiotic sensitivity pattern vary with time. In a study, Jha et al. found that most common organisms responsible for CAUTI were E. coli (49%), S. aureus (23%), Proteus spp.(3.6%), Klebsiella (9.71%), Pseudomonas (0.8%), and Citrobacter (2.8%).[19] Where as in the present study, Pseudomonas (51%), E. coli (17%), Proteus spp., Citrobacter, Klebsiella, and Acinetobacter (8% each) were the most common. Similarly, antibiotic resistance pattern also varied. In their study, Taneja et al. found the highest frequency of antibiotic resistance was for ciprofloxacin (68.6%) followed by netilmicin (60.7%), ceftazidime (58.8%), imipenem (43.7%), amikacin (43.1%), and piperacillin (39.2%).[20] In the present study, the pattern of antibiotic resistance was ceftazidime, imipenem, ciprofloxacin, and meropenem but universally sensitive to polymyxin. In this study, we have shown that neomycin-polymyxin sulfate solution bladder wash is very effective in preventing CAUTI. Thus it can be included in the routine catheter care, especially if catheterization is needed for more than 5 days. It is easy to implement and cost effective.
Limitations
Our studies have three main limitations. First, we did not study the effect on mortality, ICU stay and ventilatory days. Second, we did not send the culture before catheterization. Third due to small sample size and single center study our result may vary from other studies.
CONCLUSION
This study showed that twice daily bladder wash with the neomycin-polymyxin solution is effective in the prevention of CAUTI. It can be incorporated as a routine practice in long-term catheterized traumatic brain injury patients admitted to ICU.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Written informed consent for publication obtained from each patients relatives enrolled in this study. Presented at 23rd Annual Conference of Indian Society of Critical Care Medicine (CRITICARE 2017) held at Kochi, Kerala, India.
REFERENCES
- 1.Sandock DS, Gothe BG, Bodner DR. Trimethoprim-sulfamethoxazole prophylaxis against urinary tract infection in the chronic spinal cord injury patient. Paraplegia. 1995;33:156–60. doi: 10.1038/sc.1995.34. [DOI] [PubMed] [Google Scholar]
- 2.Waites KB, Canupp KC, DeVivo MJ. Eradication of urinary tract infection following spinal cord injury. Paraplegia. 1993;31:645–52. doi: 10.1038/sc.1993.104. [DOI] [PubMed] [Google Scholar]
- 3.Waites KB, Canupp KC, Brookings ES, DeVivo MJ. Effect of oral ciprofloxacin on bacterial flora of perineum, urethra, and lower urinary tract in men with spinal cord injury. J Spinal Cord Med. 1999;22:192–8. doi: 10.1080/10790268.1999.11719569. [DOI] [PubMed] [Google Scholar]
- 4.Biering-Sørensen F, Høiby N, Nordenbo A, Ravnborg M, Bruun B, Rahm V. Ciprofloxacin as prophylaxis for urinary tract infection: Prospective, randomized, cross-over, placebo controlled study in patients with spinal cord lesion. J Urol. 1994;151:105–8. doi: 10.1016/s0022-5347(17)34882-6. [DOI] [PubMed] [Google Scholar]
- 5.Pedersen SS, Hørbov S, Biering-Sørensen F, Høiby N. Peroral treatment with ciprofloxacin of patients with spinal cord lesion and bacteriuria caused by multiply resistant bacteria. Paraplegia. 1990;28:41–7. doi: 10.1038/sc.1990.5. [DOI] [PubMed] [Google Scholar]
- 6.Stannard AJ, Sharples SJ, Norman PM, Tillotson GS. Ciprofloxacin therapy of urinary tract infections in paraplegic and tetraplegic patients: A bacteriological assessment. J Antimicrob Chemother. 1990;26(Suppl F):13–8. doi: 10.1093/jac/26.suppl_f.13. [DOI] [PubMed] [Google Scholar]
- 7.Schaeffer AJ. Catheter-associated bacteriuria. Urol Clin North Am. 1986;13:735–47. [PubMed] [Google Scholar]
- 8.Stamm WE. Catheter-associated urinary tract infections: Epidemiology, pathogenesis, and prevention. Am J Med. 1991;91:65S–71S. doi: 10.1016/0002-9343(91)90345-x. [DOI] [PubMed] [Google Scholar]
- 9.Burke JP, Riley DK. Nosocomial urinary tract infection. In: Mayhall CG, editor. Hospital Epidemiology and Infection Control. Baltimore: Williams and Wilkins; 1996. pp. 139–53. [Google Scholar]
- 10.Warren JW. Catheter-associated urinary tract infections. Infect Dis Clin North Am. 1997;11:60922. doi: 10.1016/s0891-5520(05)70376-7. [DOI] [PubMed] [Google Scholar]
- 11.Kunin CM. Urinary Tract Infections: Detection, Prevention and Management. 5th ed. Baltimore: Williams and Wilkins; 1997. Care of the urinary catheter; pp. 227–99. [Google Scholar]
- 12.Dudley MN, Barriere SL. Antimicrobial irrigations in the prevention and treatment of catheter-related urinary tract infections. Am J Hosp Pharm. 1981;38:59–65. [PubMed] [Google Scholar]
- 13.van den Broek PJ, Daha TJ, Mouton RP. Bladder irrigation with povidone-iodine in prevention of urinary-tract infections associated with intermittent urethral catheterisation. Lancet. 1985;1:563–5. doi: 10.1016/s0140-6736(85)91217-6. [DOI] [PubMed] [Google Scholar]
- 14.Muncie HL, Jr, Hoopes JM, Damron DJ, Tenney JH, Warren JW. Once-daily irrigation of long-term urethral catheters with normal saline. Lack of benefit. Arch Intern Med. 1989;149:441–3. [PubMed] [Google Scholar]
- 15.Elliott TS, Reid L, Rao GG, Rigby RC, Woodhouse K. Bladder irrigation or irritation? Br J Urol. 1989;64:391–4. doi: 10.1111/j.1464-410x.1989.tb06049.x. [DOI] [PubMed] [Google Scholar]
- 16.Schneeberger PM, Vreede RW, Bogdanowicz JF, van Dijk WC. A randomized study on the effect of bladder irrigation with povidone-iodine before removal of an indwelling catheter. J Hosp Infect. 1992;21:223–9. doi: 10.1016/0195-6701(92)90079-2. [DOI] [PubMed] [Google Scholar]
- 17.Stamm AM, Coutinho MS. Urinary tract infection associated with indwelling bladder catheter: Incidence and risk factors. Rev Assoc Med Bras. 1999;45:27–33. doi: 10.1590/s0104-42301999000100007. [DOI] [PubMed] [Google Scholar]
- 18.Puri J, Mishra B, Mal A, Murthy NS, Thakur A, Dogra V, et al. Catheter associated urinary tract infections in neurology and neurosurgical units. J Infect. 2002;44:171–5. doi: 10.1053/jinf.2002.0968. [DOI] [PubMed] [Google Scholar]
- 19.Jha N, Bapat SK. A study of sensitivity and resistance of pathogenic microorganisms causing UTI in Kathmandu valley. Kathmandu Univ Med J (KUMJ) 2005;3:123–9. [PubMed] [Google Scholar]
- 20.Taneja N, Meharwal SK, Sharma SK, Sharma M. Significance and characterisation of pseudomonads from urinary tract specimens. J Commun Dis. 2004;36:27–34. [PubMed] [Google Scholar]


