Abstract
Background:
Characteristics of patients admitted to intensive care units with respiratory failure (RF) and undergoing mechanical ventilation (MV) have been described for particular indications and diseases, but there are few studies in the general Intensive Care Unit (ICU) population and even lesser from developing countries.
Objective:
This study aims to study clinical characteristics, outcomes, and factors affecting outcomes in adult patients with RF on MV admitted to ICU.
Methods:
A retrospective study of medical records of all patients admitted to ICU between January 1, 2015, and March 31, 2016. Patients receiving MV for more than 6 h were included in the study. Patients younger than 12 years were excluded. Data were recorded of all patients receiving MV during this period regarding demographics, indications for MV, type and characteristics of ventilation, concomitant complications and treatment, and outcomes. Data were recorded at the initiation of MV and daily all throughout the course of MV. The main outcome measure was all-cause mortality at the end of ICU stay.
Results:
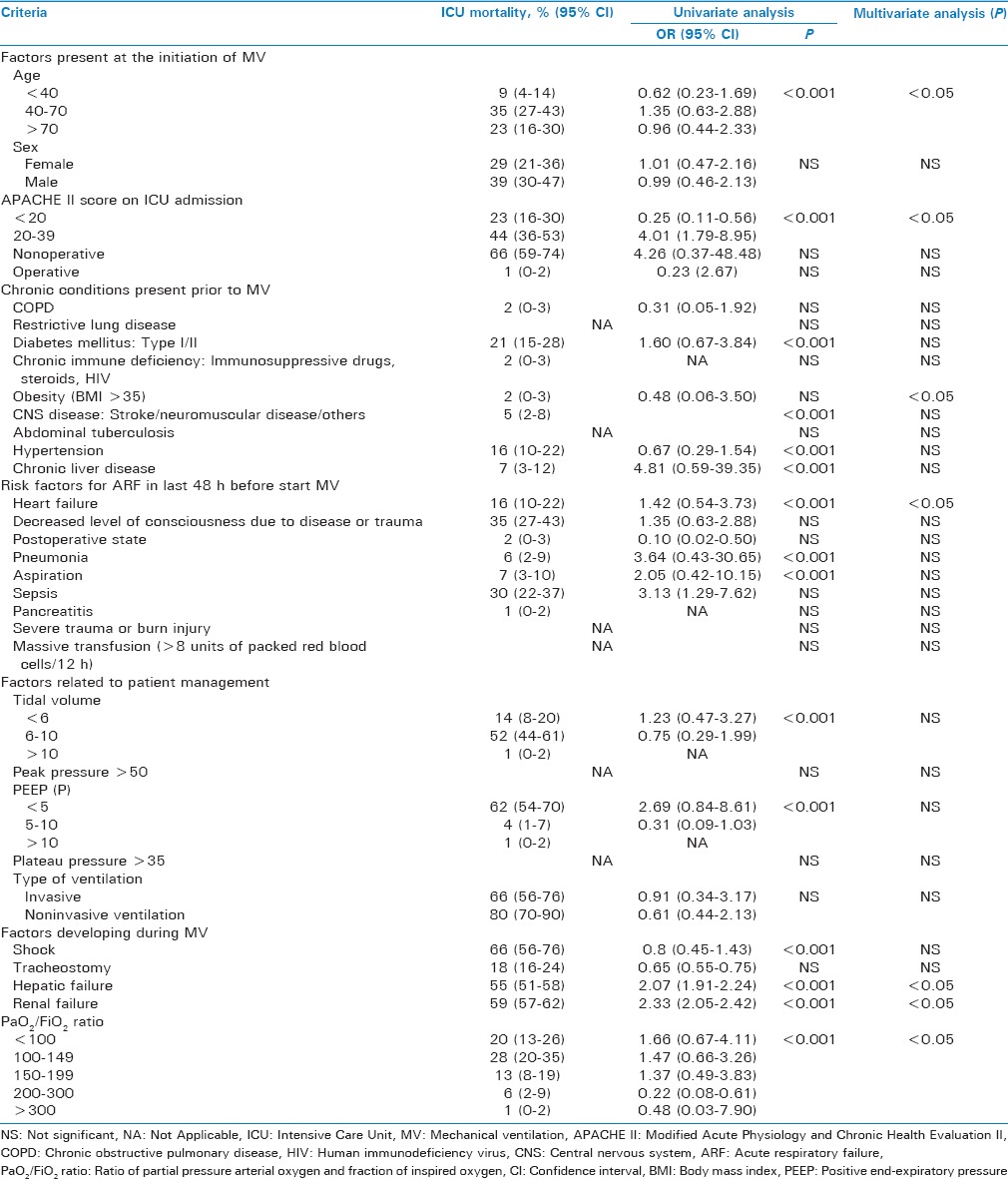
Of the 500 patients admitted to the ICU during the period of the study, a total of 122 patients received MV (and were included in study) for mean (standard deviation [SD]) duration of 4 (3.4) days. The mean (SD) stay in ICU and hospital was 4.49 (3.52) and 6.4 (3.6), respectively. Overall mortality for the unselected general ICU patients on MV was 67.21% while that for ARDS patients was 76.1%. The main factors independently associated with increased mortality were (i) pre-MV factors: age, Apache II scores, heart failure (odds ratio [OR], 1.42; 95% confidence interval [CI], 0.54–3.73; P < 0.001); (ii) patient management factors: positive end-expiratory pressure (OR, 2.69; 95% CI, 0.84–8.61; P < 0.001); (iii) Factors occurring over the course of MV: PaO2/FiO2 ratio < 100 (OR, 1.66; 95% CI, 0.67–4.11; P < 0.001) and development of renal failure (OR, 2.33; 95% CI, 2.05–2.42; P < 0.001) and hepatic failure (OR, 2.07; 95% CI, 1.91–2.24; P < 0.001) after initiation of MV.
Conclusions:
Outcomes of patients undergoing MV are dependent on various factors (including patient demographics, nature of associated morbidity, characteristics of the MV received, and conditions developing over course of MV) and these factors may be present before or develop after initiation of MV.
Key Words: Acute respiratory failure, critical illness, Intensive Care Unit, mechanical ventilation, noninvasive ventilation
INTRODUCTION
Mechanical ventilation (MV) is used quite frequently in the intensive care unit (ICU), for the treatment of patients with respiratory failure (RF), with its utilization increasing in recent years.[1,2] More patients get admitted to ICU for respiratory support than any other indication. Data regarding patients admitted for specific disease and then needing MV is available.[3,4] However, data regarding MV in general ICU patients, especially in general ICU Indian patients, is still sparse. Moreover, newer modes of MV are now available, each claiming to be better and have found some clinical acceptability. However, data regarding their utilization in real-life ICU situations are not available.[5,6] We undertook a study to understand the clinical characteristics of patients, indications, modes, and characteristics of MV used and outcomes (all-cause mortality in ICU) of patients admitted to the tertiary ICU of our hospital in Western India. India being a vast and diverse country, standards of care across the country may vary, and patterns of care might be different in other parts of the country.
METHODS
WE conducted a retrospective analysis of medical records of all patients admitted to the ICU of our hospital located in western India. The study was approved by the institutional ethics committee. As it was a retrospective study of records, need for consent was waived.
Inclusion criteria
All patients initiated on MV and requiring MV for more than 6 h, during their stay in ICU were included.
Exclusion criteria
Patients <18 years of age were excluded from the study.
Data collection
The following data were collected from the medical records of the patients.
Demographic data: (i) age, (ii) gender, (iii) underlying disease and diagnosis on admission, (iv) Modified Acute Physiology and Chronic Health Evaluation (APACHE) II score, (v) date of initiation of MV, (vi) mode of airway access-intubation (orotracheal or nasotracheal), face mask or tracheostomy, (vii) length of stay in ICU and in hospital in days, (viii) length of MV in days and (ix) outcomes (all-cause mortality in ICU)
Indications for the initiation of MV were classified into one of the following: (i) Acute exacerbation of previous chronic RF (acute on chronic renal failure [CRF])-patients suffering from obstructive, restrictive, or mixed obstructive and restrictive disease of the lung now presenting with exacerbation due to infective, bronchospastic, or an acute event, (ii) Acute RF (ARF)-patients without any previous respiratory disease, now requiring MV for RF, (iii) Coma-unconscious patients requiring endotracheal intubation for airway protection and MV, and (iv) Neuromuscular disease (NMD). In the presence of more than one indication for MV, the one thought to be more important was recorded
The modality of ventilation (invasive or noninvasive [NIV]), mode of ventilator (Assist control, pressure controlled ventilation, pressure support ventilation) and ventilator settings at the time of initiation of MV were noted along with hemodynamic parameters, arterial blood gas analysis (ABG) at that time. The following were assessed daily throughout the duration of MV and were recorded if present: changeover from NIV to invasive ventilation following endotracheal (orotracheal or nasotracheal) intubation, mode of ventilator, ventilator settings, hemodynamic parameters, ABG, acute respiratory distress syndrome (ARDS), ventilator-associated pneumonia, sepsis, acute renal or hepatic failure, and coagulopathy. The concomitant treatment (vasopressors, neuromuscular blockers, sedatives) was also noted.
There were no institutional protocols for the initiation of MV or for weaning from MV, and they were done as per the clinical judgement of the treating physician and intensivist, in accordance with accepted international guidelines for the same.
Statistical analysis: all categorical data were displayed as numbers and percentages. Continuous data were presented as mean ± standard deviation and median, as appropriate. Statistical analysis was performed using the Statistical package for social sciences (SPSS Windows version 16, Chicago IL., USA). The primary outcome measure was all-cause mortality during the stay in ICU. The variables were grouped in three categories: (i) pre-MV factors, (ii) patient management factors, and (iii) occurrences over the course of MV. For the univariate analysis, factor frequency was compared by Chi-square test, and adjusted odds ratios (OR) along with 95% confidence intervals (CIs) were calculated. Groups were formed depending on the reason for initiation of MV and they were compared using 1 way analysis of variance (ANOVA) for continuous variables. A multivariate analysis was performed, using a conditional logistic regression model and a forward stepwise selection method to correct for colinearity, to estimate the simultaneous effects of multiple variables on ICU mortality. The criterion for entering variables in the multivariate analysis was P < 0.10 in the univariate analysis.
RESULTS
Five hundred patients were admitted to the ICU during the study period of January 1, 2015, and March 31, 2016. Of these, 130 patients (26%) received MV for more than 6 h. 8 of these patients were excluded as their records were unavailable. Hence, 122 patients were included in the study. All these patients were studied during their entire period of MV. Demographic characteristics, reason for initiation of MV and causes for acute RF are listed in Table 1. The duration of MV, length of stay in ICU, and length of stay in hospital and outcomes of the studied patients are listed in Table 2. The modes of ventilator and monitored variables are listed in Table 3 according to the reasons (indications) for the initiation of MV. Figure 1 shows the modes of ventilator in the whole group of studied patients over time. Trials of weaning were performed with T-piece trial in 43 (89.6%) patients and continuous positive airway pressure was used in 5 (10.4%) patients. One patient required reintubation after extubation. Six patients underwent tracheostomy (4 in the ARF group and 2 in non-ARF group). Mortality in patients undergoing tracheostomy was 66.66%.
Table 1.
Characteristics of patients on Intensive Care Unit admission (n=122)
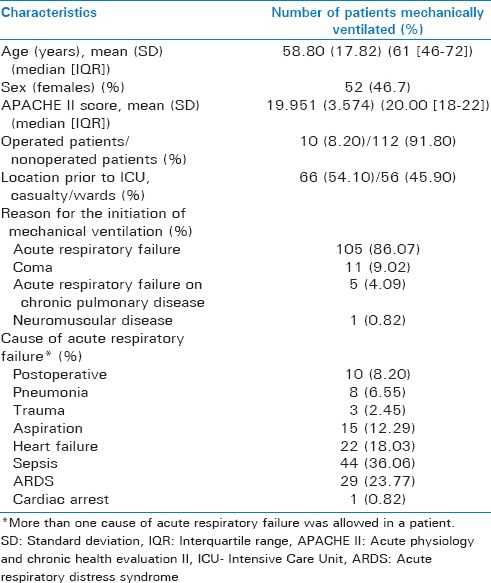
Table 2.
Duration of mechanical ventilation, length of stay in Intensive Care Unit, length of stay in hospital and outcomes in studied patients
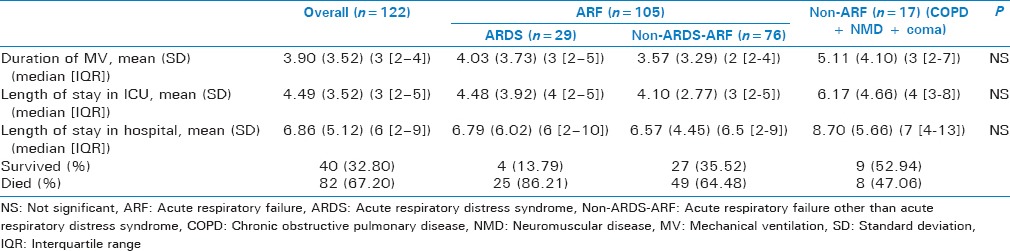
Table 3.
Ventilator modes and monitored variables on days 1, 3 and 7 in studied patients according to reasons (indications) for initiation of mechanical ventilation
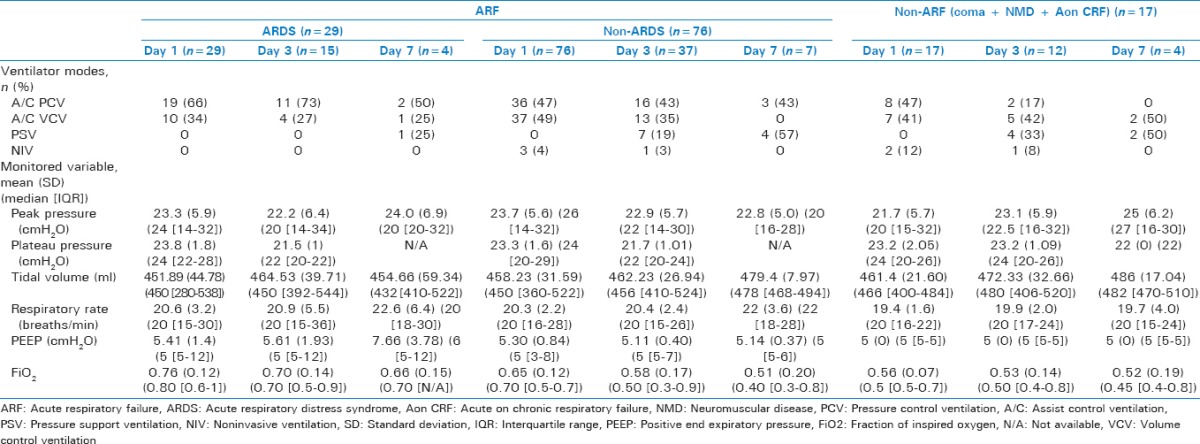
Figure 1.
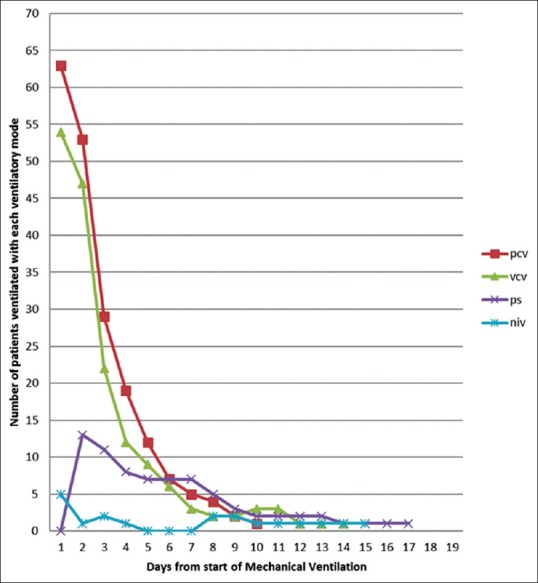
Ventilator modes used per day during course of mechanical ventilation. PCV: Pressure control ventilation, VCV: Assist control ventilation, PS: Pressure support ventilation, NIV: Noninvasive ventilation
Univariate and multivariate analysis of factors associated with ICU mortality is shown in Table 4. The following factors were independently associated with an increased mortality: age, APACHE II scores on ICU admission, heart failure, obesity (body mass index >35), level of positive-end expiratory pressure (PEEP), ratio of partial pressure arterial oxygen and fraction of inspired oxygen (PaO2/FiO2 ratio) <100 and development of renal or hepatic failure after initiation of MV.
Table 4.
Factors associated with Intensive Care Unit mortality in respiratory failure patients on mechanical ventilation-univariate and multivariate analysis
DISCUSSION
RF requiring MV is one of the most frequent indications for admission to ICU and may have been the very reason for the initiation of ICUs in hospitals. There has been an increase in the use of MV in patients admitted to ICUs, and MV is improving the outcomes in some diseases. Data regarding the mortality of patients initiated on MV is important as it allows for better conveying the outcome to patient's family. Outcomes of MV for patients with particular disease (e.g., chronic obstructive pulmonary disease [COPD], ARDS) have been addressed by investigators.[3,4] In addition, there is considerable literature on survival rates of patients with ARF from Western countries.[7,8,9] There is a rather lack of “real world” data from Indian ICUs, especially among general ICU patients with RF requiring MV. We present real-world data from our ICU in Western India.
In our study, survival in patients with RF who require MV for more than 6 h was 32.8% and mortality was 67.2%, which depended on many factors, some present before the initiation of MV and others developing during the course of management of the patient and on complications occurring during this time. The reported mortality among patients requiring MV for RF of different etiologies ranges from 30% to 45% in developed countries and up to 74% in third world countries.[7,8,9,10,11,12,13,14,15,16,17]
A good number of studies have reported the effects of age on mortality of MV patients. At least six prospective cohort studies have found age to be independently associated with hospital mortality.[8,9,10,18,19,20,21] Esteban et al. have shown mortality in patients with MV is independently associated with age and they have divided these patients in 3 age groups (<40 years, 40–70 years, and more than 70 years), each having different prognostic value.[10] Our study shows mortality to be much lower in the <40 years age group. Mortality in the over 70 year's age group patients is not any worse than those in the 40–70 years age group. Hence, elderly patients should not be denied MV on the sole criterion of age. Mortality in elderly patients with RF on MV ranges from 38% to 99% in reported literature.[8,9,10,18,19,20,21] Ely et al. reported hospital mortality of 38.1%[19] among patients older than 75 years while Esteban et al. reported mortality rate of 36% in these patients.[10] Physicians and caregivers may struggle with the decision of initiating MV in elderly patients, but we found no evidence to support this decision.
In most studies, men account for more than 50% of patients receiving MV.[5,9,10,20] Kollef et al. found mortality to be greater among female patients compared to male patients despite being similarly ill and having similar organ system dysfunctions.[20] Other studies, however, could not find such or other relationship of gender with mortality in patients of RF undergoing MV.[8,22] In our study, there was no association of gender with mortality in patients of RF undergoing MV.
The reason for initiation of MV definitely influences the outcomes of these patients. Various studies have found increased mortality in patients of RF who were initiated on MV due to coma, ARDS or sepsis and reduced mortality in patients initiated on MV due to postoperative state.[10,20,22] In our study, heart failure, pneumonia, aspiration as a reason for the initiation of MV increased mortality in the univariate analysis but not the multivariate analysis. Patients with ARDS on MV have higher mortality rates ranging from 30% to 62% in various studies.[18,23,24,25] Even our mortality was 86% in such patients. Mortality in ARDS patients depends on associated organ failure and type of ARDS (early or late).[18,23,24,25,26,27]
Doctors and caregivers of patients with chronic respiratory diseases requiring MV for acute decompensation may hesitate to start invasive MV due to bad prognosis and increased duration of MV in these patients. However, patients in the non-ARF group (patients with RF due to Acute on CRF, NMD or coma) did not have increased mortality in our study (though the number of patients is small). These results are similar to other studies.[3,10,19,28] These patients should not be denied invasive MV, when required.
Mortality prognostication scores (APACHE, simplified acute physiology score) have good sensitivity and specificity in predicting outcomes of patients admitted in ICU. Among ICU patients requiring MV, studies have shown APACHE II score to be independently associated with mortality.[29,30,31] This correlation has been demonstrated in general ICU patients as well as patients requiring MV due to specific indications (COPD patients requiring invasive MV,[29] Severe community-acquired pneumonia requiring MV [31]). Even our study demonstrates correlation of APACHE II score with mortality in univariate and multivariate analysis, with higher mortality in patients with higher scores. However, in one study of patients requiring MV due to acute cardiogenic pulmonary edema, APACHE II score did not predict mortality.[32] The link between APACHE II score and mortality may be easy to understand as patients with higher scores will be more severely ill and hence more likely to die.
The relation of PEEP with mortality has been studied in patients on MV, especially in patients with ARDS. A meta-analysis has shown that high PEEP has a small but significant mortality benefit in ARDS patients, with another systematic review and meta-analysis supporting its use even in unselected group of MV patients.[33,34]
PaO2/FiO2 ratio, an indication of pulmonary failure, when severe (PaO2/FiO2 ratio <100) increases risk of mortality in our study and even in studies conducted by Esteban et al. (general ICU patients),[10] Sloane et al. (ARDS patients),[35] Navarrete-Navarro et al. (ARDS patients),[27] and Knaus et al. (ARDS patients).[36] Some studies failed to show any association between PaO2/FiO2 ratio and mortality.[8,25,37]
In these patients with RF on MV, additional organ failure (renal, hepatic) during the period of MV was independently associated with mortality. Patients with sepsis presenting with single organ system failure have mortality from 14% to 40% while those two organ system failure have mortality from 20% to 76%, 3 organ system failures have mortality from 30% to 90%, and 4 or more organ system failures have mortality of 100%.[38] Thus, additional organ system failure would be associated with increased mortality in patients with RF.
The strength of our study was that it is a real-world study including all adults patients who underwent MV in our ICU and these patients were followed up everyday with monitoring of data throughout the course of MV.
The limitations of our study were: i) single-center study, ii) limited number of patients, and iii) lack of external validity.
CONCLUSIONS
Outcomes of patients undergoing MV are multifactorial dependent, and these factors may be present before MV initiation as well as develop after onset of MV. In “real world” adult ICU patients undergoing MV in our ICU in Western India, outcomes (all cause ICU mortality) are determined by age, APACHE score on ICU admission, presence of heart failure, and obesity before initiation of MV, severity of RF (as determined by PaO2/FiO2 ratio), and subsequent additional organ failure. Additional prospective, randomized multicenter trials in Indian ICU setting will lend additional clarity to these findings.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank (i) Dr. Rachana Rhayakar for assistance with data collection, and (ii) Dr. Harshal T. Pandve, Associate Professor, Department of Community Medicine, S. K. N. Medical College, Pune, Maharashtra, India, and Tejashree Kulkarni, S. K. N. Medical College, Pune, Maharashtra, India, and Aditi Deshpande, from Amaze Stats, Pune for help with statistical analysis of the data.
REFERENCES
- 1.Stefan MS, Shieh MS, Pekow PS, Rothberg MB, Steingrub JS, Lagu T, et al. Epidemiology and outcomes of acute respiratory failure in the United States, 2001 to 2009: A national survey. J Hosp Med. 2013;8:76–82. doi: 10.1002/jhm.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mehta AB, Syeda SN, Wiener RS, Walkey AJ. Epidemiological trends in invasive mechanical ventilation in the United States: A population-based study. J Crit Care. 2015;30:1217–21. doi: 10.1016/j.jcrc.2015.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seneff MG, Wagner DP, Wagner RP, Zimmerman JE, Knaus WA. Hospital and 1-year survival of patients admitted to Intensive Care Units with acute exacerbation of chronic obstructive pulmonary disease. JAMA. 1995;274:1852–7. [PubMed] [Google Scholar]
- 4.Acute Respiratory Distress Syndrome Network. Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301–8. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 5.Esteban A, Alía I, Ibañez J, Benito S, Tobin MJ. Modes of mechanical ventilation and weaning. A national survey of Spanish hospitals. The Spanish Lung Failure Collaborative Group. Chest. 1994;106:1188–93. doi: 10.1378/chest.106.4.1188. [DOI] [PubMed] [Google Scholar]
- 6.Singh PM, Borle A, Trikha A. Newer nonconventional modes of mechanical ventilation. J Emerg Trauma Shock. 2014;7:222–7. doi: 10.4103/0974-2700.136869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vasilyev S, Schaap RN, Mortensen JD. Hospital survival rates of patients with acute respiratory failure in modern respiratory intensive care units. An international, multicenter, prospective survey. Chest. 1995;107:1083–8. doi: 10.1378/chest.107.4.1083. [DOI] [PubMed] [Google Scholar]
- 8.Luhr OR, Antonsen K, Karlsson M, Aardal S, Thorsteinsson A, Frostell CG, et al. The ARF Study Group. Incidence and mortality after acute respiratory failure and acute respiratory distress syndrome in Sweden, Denmark, and Iceland. Am J Respir Crit Care Med. 1999;159:1849–61. doi: 10.1164/ajrccm.159.6.9808136. [DOI] [PubMed] [Google Scholar]
- 9.Behrendt CE. Acute respiratory failure in the United States: Incidence and 31-day survival. Chest. 2000;118:1100–5. doi: 10.1378/chest.118.4.1100. [DOI] [PubMed] [Google Scholar]
- 10.Esteban A, Anzueto A, Frutos F, Alía I, Brochard L, Stewart TE, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: A 28-day international study. JAMA. 2002;287:345–55. doi: 10.1001/jama.287.3.345. [DOI] [PubMed] [Google Scholar]
- 11.Tomicic V, Espinoza M, Andresen M, Molina J, Calvo M, Ugarte H, et al. Characteristics and factors associated with mortality in patients receiving mechanical ventilation: First Chilean multicenter study. Rev Med Chil. 2008;136:959–67. [PubMed] [Google Scholar]
- 12.Vincent JL, Akça S, De Mendonça A, Haji-Michael P, Sprung C, Moreno R, et al. The epidemiology of acute respiratory failure in critically ill patients. Chest. 2002;121:1602–9. doi: 10.1378/chest.121.5.1602. [DOI] [PubMed] [Google Scholar]
- 13.Lewandowski K, Metz J, Deutschmann C, Preiss H, Kuhlen R, Artigas A, et al. Incidence, severity, and mortality of acute respiratory failure in Berlin, Germany. Am J Respir Crit Care Med. 1995;151:1121–5. doi: 10.1164/ajrccm.151.4.7697241. [DOI] [PubMed] [Google Scholar]
- 14.Linko R, Okkonen M, Pettilä V, Perttilä J, Parviainen I, Ruokonen E, et al. Acute respiratory failure in Intensive Care Units. FINNALI: A prospective cohort study. Intensive Care Med. 2009;35:1352–61. doi: 10.1007/s00134-009-1519-z. [DOI] [PubMed] [Google Scholar]
- 15.Franca SA, Toufen C, Jr, Hovnanian AL, Albuquerque AL, Borges ER, Pizzo VR, et al. The epidemiology of acute respiratory failure in hospitalized patients: A Brazilian prospective cohort study. J Crit Care. 2011;26:330.e1–8. doi: 10.1016/j.jcrc.2010.10.010. [DOI] [PubMed] [Google Scholar]
- 16.Sinclair JR, Watters DA, Davison M. Outcome of mechanical ventilation in Central Africa. Ann R Coll Surg Engl. 1988;70:76–9. [PMC free article] [PubMed] [Google Scholar]
- 17.Okafor UV. Challenges in critical care services in Sub-Saharan Africa: Perspectives from Nigeria. Indian J Crit Care Med. 2009;13:25–7. doi: 10.4103/0972-5229.53112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zilberberg MD, Epstein SK. Acute lung injury in the medical ICU: Comorbid conditions, age, etiology, and hospital outcome. Am J Respir Crit Care Med. 1998;157:1159–64. doi: 10.1164/ajrccm.157.4.9704088. [DOI] [PubMed] [Google Scholar]
- 19.Ely EW, Evans GW, Haponik EF. Mechanical ventilation in a cohort of elderly patients admitted to an Intensive Care Unit. Ann Intern Med. 1999;131:96–104. doi: 10.7326/0003-4819-131-2-199907200-00004. [DOI] [PubMed] [Google Scholar]
- 20.Kollef MH, O'Brien JD, Silver P. The impact of gender on outcome from mechanical ventilation. Chest. 1997;111:434–41. doi: 10.1378/chest.111.2.434. [DOI] [PubMed] [Google Scholar]
- 21.Steiner T, Mendoza G, De Georgia M, Schellinger P, Holle R, Hacke W. Prognosis of stroke patients requiring mechanical ventilation in a neurological critical care unit. Stroke. 1997;28:711–5. doi: 10.1161/01.str.28.4.711. [DOI] [PubMed] [Google Scholar]
- 22.Epstein SK, Vuong V. Lack of influence of gender on outcomes of mechanically ventilated medical ICU patients. Chest. 1999;116:732–9. doi: 10.1378/chest.116.3.732. [DOI] [PubMed] [Google Scholar]
- 23.Roupie E, Lepage E, Wysocki M, Fagon JY, Chastre J, Dreyfuss D, et al. Prevalence, etiologies and outcome of the acute respiratory distress syndrome among hypoxemic ventilated patients. SRLF Collaborative Group on Mechanical Ventilation. Société de Réanimation de Langue Française. Intensive Care Med. 1999;25:920, 9. doi: 10.1007/s001340050983. [DOI] [PubMed] [Google Scholar]
- 24.Suchyta MR, Clemmer TP, Elliott CG, Orme JF, Jr, Weaver LK. The adult respiratory distress syndrome. A report of survival and modifying factors. Chest. 1992;101:1074, 9. doi: 10.1378/chest.101.4.1074. [DOI] [PubMed] [Google Scholar]
- 25.Doyle RL, Szaflarski N, Modin GW, Wiener-Kronish JP, Matthay MA. Identification of patients with acute lung injury. Predictors of mortality. Am J Respir Crit Care Med. 1995;152(6 Pt 1):1818–24. doi: 10.1164/ajrccm.152.6.8520742. [DOI] [PubMed] [Google Scholar]
- 26.Valta P, Uusaro A, Nunes S, Ruokonen E, Takala J. Acute respiratory distress syndrome: Frequency, clinical course, and costs of care. Crit Care Med. 1999;27:2367–74. doi: 10.1097/00003246-199911000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Navarrete-Navarro P, Ruiz-Bailén M, Rivera-Fernández R, Guerrero-López F, Pola-Gallego-de-Guzmán MD, Vázquez-Mata G. Acute respiratory distress syndrome in trauma patients: ICU mortality and prediction factors. Intensive Care Med. 2000;26:1624–9. doi: 10.1007/s001340000683. [DOI] [PubMed] [Google Scholar]
- 28.Nevins ML, Epstein SK. Predictors of outcome for patients with COPD requiring invasive mechanical ventilation. Chest. 2001;119:1840–9. doi: 10.1378/chest.119.6.1840. [DOI] [PubMed] [Google Scholar]
- 29.Liu H, Zhang TT, Ye J. Analysis of risk factors for hospital mortality in patients with chronic obstructive pulmonary diseases requiring invasive mechanical ventilation. Chin Med J (Engl) 2007;120:287–93. [PubMed] [Google Scholar]
- 30.Matic I, Titlic M, Dikanovic M, Jurjevic M, Jukic I, Tonkic A. Effects of APACHE II score on mechanical ventilation; prediction and outcome. Acta Anaesthesiol Belg. 2007;58:177–83. [PubMed] [Google Scholar]
- 31.Aydogdu M, Ozyilmaz E, Aksoy H, Gürsel G, Ekim N. Mortality prediction in community-acquired pneumonia requiring mechanical ventilation; values of pneumonia and Intensive Care Unit severity scores. Tuberk Toraks. 2010;58:25–34. [PubMed] [Google Scholar]
- 32.Fedullo AJ, Swinburne AJ, Wahl GW, Bixby K. Acute cardiogenic pulmonary edema treated with mechanical ventilation. Factors determining in-hospital mortality. Chest. 1991;99:1220–6. doi: 10.1378/chest.99.5.1220. [DOI] [PubMed] [Google Scholar]
- 33.Oba Y, Thameem DM, Zaza T. High levels of PEEP may improve survival in acute respiratory distress syndrome: A meta-analysis. Respir Med. 2009;103:1174–81. doi: 10.1016/j.rmed.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 34.Phoenix SI, Paravastu S, Columb M, Vincent JL, Nirmalan M. Does a higher positive end expiratory pressure decrease mortality in acute respiratory distress syndrome? A systematic review and meta-analysis. Anesthesiology. 2009;110:1098–105. doi: 10.1097/ALN.0b013e31819fae06. [DOI] [PubMed] [Google Scholar]
- 35.Sloane PJ, Gee MH, Gottlieb JE, Albertine KH, Peters SP, Burns JR, et al. A multicenter registry of patients with acute respiratory distress syndrome. Physiology and outcome. Am Rev Respir Dis. 1992;146:419–26. doi: 10.1164/ajrccm/146.2.419. [DOI] [PubMed] [Google Scholar]
- 36.Knaus WA, Sun X, Hakim RB, Wagner DP. Evaluation of definitions for adult respiratory distress syndrome. Am J Respir Crit Care Med. 1994;150:311–7. doi: 10.1164/ajrccm.150.2.8049808. [DOI] [PubMed] [Google Scholar]
- 37.Jiménez P, Torres A, Roca J, Cobos A, Rodriguez-Roisin R. Arterial oxygenation does not predict the outcome of patients with acute respiratory failure needing mechanical ventilation. Eur Respir J. 1994;7:730–5. doi: 10.1183/09031936.94.07040730. [DOI] [PubMed] [Google Scholar]
- 38.Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: Analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–10. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]


