Abstract
Introduction:
Laparoscopic management of giant hydatid cyst has limitations such as spillage, poor control, difficulties in suctioning the contents through special ports which are not easily available, difficulty in the obliteration of residual cavity and recurrence. We describe single-incision trocar-less endoscopic (SITE) technique which simplifies enucleation and management of residual cavity.
Method:
Inclusion criteria for these cases were patients having single uncomplicated giant hydatid cyst >5 cm present at the surface of the liver and palpable on clinical examination. The cysts which were <5 cm, multiple, deep-seated and impalpable were excluded from the study.
Technique:
An incision of 1 cm is marked over the site of the maximum bulge and deepened to open peritoneum, cyst is held with two stay sutures, injection of scolicidal agent and aspiration is done and suction of the cyst content is done. After suction of the contents, 5 mm telescope is inserted, and the cyst cavity is inspected, clearance and cyst procedure is done.
Results:
In 6 years, 62 cases of giant hydatid cyst fulfilling the inclusion criteria and were taken for SITE technique. SITE was successful in all patients and none needed a conversion. Twenty-nine (46.77%) underwent omentopexy and three (4.83%) underwent SITE capitonnage. There was post-operative biliary leak in one (0.016%) patient who underwent capitonnage, which was managed by prolonged drainage which resolved in 10 days. Mean operative duration was 52 min (30 min to 85 min). Mean follow-up was for 18 months (12–36 months). One (0.016%) patient had cyst recurrence.
Discussion:
SITE has advantages of endoscopic clearance and does not require special ports which are expensive, technically difficult to use and often unavailable. It allows controlled handling, effective suction and easier management of bile communication. SITE can be a preferred procedure for endoscopic management of giant liver hydatid cysts.
Conclusion:
SITE management of giant liver hydatid cyst seems to be a reliable treatment modality as it is minimally invasive, efficient, easy to perform and effective.
Keywords: Children, hydatid cyst, laparoscopy, liver, single incision
INTRODUCTION
Laparoscopic management of liver hydatid cysts is becoming a standard approach and has advantages of the minimal incision, faster recovery and complete clearance of cavity under endovision. Giant liver hydatid cysts are rare and reported in literature as case reports but are common in certain regions of the world.[1,2] Management of giant hydatid cyst presents unique set of challenges such as spill-free enucleation of cysts which are under pressure and difficult evacuation of large thick endocysts through small sized ports.[3,4] The management of residual cavity with omentopexy or capitonnage further complicates the procedure in laparoscopy in giant hydatid cysts.[5,6] The giant cyst was defined as cysts of such a size and location resulting to a palpable mass.[7] Therefore, either laparoscopy is complicated by spillage, residual and recurrent disease or open surgery is preferred in the management of these giant hydatid cysts.[8,9] We describe a single-incision trocar-less endoscopic (SITE) technique which simplifies the enucleation and management of residual cavity along with having all the advantages of laparoscopy.
MATERIALS AND METHODS
This study was conducted from March 2011 to February 2017. Inclusion criteria for these cases were patients having single uncomplicated giant hydatid cyst measuring >5 cm present at the surface of the liver and palpable on clinical examination. Hydatid cyst <5 cm was excluded and was managed with Percutaneous Aspiration, Instillation and Reaspiration (PAIR) technique and medical management. The cysts which are multiple in number, deep-seated and impalpable were excluded for the present technique and are managed with conventional laparoscopy. All the selected patients received albendazole treatment for 15 days before surgery as per guidelines.[10] Patients underwent IgE levels preoperatively. The site, size, content and extent of the cyst are identified by preoperative computed tomography.
Technique
Patients are taken under general anaesthesia and point of the maximum bulge is marked intraoperatively. An incision of 1 cm is marked over the site of the bulge and deepened to open peritoneum with the assistance of computed tomography images [Figure 1]. The liver cyst is identified by the white area bulging at the incision. The cyst is held with two stay sutures of 4-0 calibre. Spillage is avoided using deeper bites and keeping a fine suction on. A 16 Fr intravenous cannula is inserted into the cyst and aspiration of fluid is done. Through the same cannula, instillation of the scolicidal agent (10% povidone-iodine solution is our preference) and reaspiration is done. The decompression of the cyst and pulling the stay sutures allows the delivery of part of the cyst at the incision site. The cyst is opened, and suction of the cyst content is done by open wide bore suction cannula [Figure 2]. The small sized sponge holding or Babcock's forceps aids in cyst enucleation which is easily done similar to open surgery. After suction of the contents, 5 mm telescope is inserted, and the cyst cavity is inspected for any residual content or biliary leak [Figure 3]. The daughter cysts are sucked out by putting a laparoscopy/open suction cannula by the side of the telescope, and irrigation and complete clearance of the cyst is done conveniently. No port placement or gas insufflation is needed as cysts as non-collapsible. If a biliary staining is found, then capitonnage is performed with 3-0 polyglactin-910, for which procedure is converted into three-port laparoscopic surgery for endosuturing. If there is no biliary contamination, the omentum is delivered out through the incision and omentopexy is performed. The incision is closed in the standard manner over the drain which is taken out through the umbilical scar. We routinely place a 10 Fr drain in the cavity which is removed after 48 h if there is no drainage. Local bupivacaine infiltration is done, and postoperative feeds are allowed the same day. The patients were followed up for 1–6 years.
Figure 1.

Site of incision marked with the assistance of computed tomography imaging
Figure 2.

Cyst wall held with stay sutures, after isolation it is opened and cyst evacuation done with suction cannula
Figure 3.
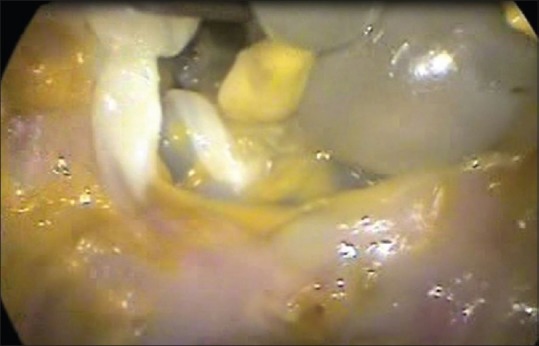
Telescope inserted in the cyst without a trocar and residual daughter cysts/membranes being cleared by suction cannula under vision
RESULTS
Over the study period, we had 92 cases of liver hydatid, of which 20 (21.73%) underwent conventional laparoscopic management for deep seated/multiple impalpable liver cysts, 7 (7.6%) had very small cysts and were treated medically and 3 (3.26%) underwent PAIR technique. Only 43 (46.73%) patients had positive IgE status which is a striking finding in the present clinical setup.
Sixty-two cases (67.39%) were giant hydatid cyst fulfilling the inclusion criteria and were taken for SITE technique. Twelve (19.35%) of these cases had associated impalpable splenic cysts and were managed with spleen-preserving laparoscopic enucleation by three-port laparoscopy and SITE was done for the giant liver cyst in the same sitting. Intraoperative spillage was seen in 1 (0.016%) patient who had a relatively smaller cyst, which could not be delivered out in the wound but the spill was cleaned with betadine 10%. Twelve (19.35%) patients had multiple daughter cysts, four (6.45%) had infected hydatid cysts and three (4.83) had biliary communication. SITE was successful in all patients and none needed a conversion to open. Twenty-nine (46.77%) underwent omentopexy and three (4.83%) underwent SITE capitonnage. There was post-operative biliary leak in 1 (0.016%) patient who underwent capitonnage, which was managed by prolonged drainage which resolved in 10 days. Mean operative duration was 52 min (30–85 min). Mean follow-up was for 18 months (12–36 months). One (0.016%) patient had cyst recurrence, which was a 5 cm × 5 cm fluid-filled cyst and was further managed with conventional laparoscopic redo surgery.
DISCUSSION
The principle of hydatid cyst management is to eliminate the parasite from the body and prevent recurrence of the disease. Surgery has been the mainstay of therapy for large cysts due to risks of rupture and infection.[11] Routine interventions done in the management of hydatid cyst are PAIR, laparoscopy and open surgery.[12]
Treatment of hydatid cyst more than 5 cm size is challenging, and open or laparoscopic surgery is the mainstay of management.[11] Laparoscopy eliminates the disadvantages of a large surgical incision and shortens the hospital stay markedly. It allows better access to multiple cysts and unusual locations which are otherwise difficult to handle with open surgery. The limitations of laparoscopy include a higher risk of intraperitoneal spillage due to poor control as routine laparoscopic suction devices are not very effective in the evacuation of the cyst content.[3,4,8,13] Hence, there may be suboptimal evacuation of the particulate contents of the cyst, the daughter cysts and laminated membrane predisposing to higher chance of recurrence.[9]
There are various innovations in the form of suction devices to enable controlled suction of contents without spillage.[9,10] An aspirator-grinder apparatus was developed by Acarli.[9] Special trocar-cannula system – the Palanivelu hydatid system is described which enables removal of endocyst without excision of the entire cyst.[4,10,11] These devices are not easily available and are very often ineffective. There are several disadvantages of various hydatid systems including the risk for leakage around the puncture site (because of the high pressure in the cyst), frequent blockage of the puncture needle by intracystic particles (necessitating withdrawal and causing further leakage), difficulty in evacuating the particulate contents (daughter cysts and laminated membrane), large size of trocars for children, cost and availability.[3]
Hydatid cyst patients present late in India, and consequently, the cyst size is large; therefore. giant hydatid is relatively common.[2,3] Although laparoscopy is increasingly being used for hydatid cyst management, the literature on laparoscopic treatment of giant hydatid disease of the liver is scarce.[5,9,11] Management of giant hydatid cyst presents the unique set of challenges in laparoscopic management and has limitations of spillage due to poor control, difficulties of suctioning the cyst contents through limited sized ports, recurrence and technical difficulty in the obliteration of residual cavity with omentopexy or capitonnage.[5,12]
Authors have developed a SITE technique for giant hydatid cysts which is easily reproducible, cosmetic, can be done by conventional instruments, avoids intraperitoneal spillage, allows complete evacuation and simplifies surgical management of residual cavity. This can become preferred technique in giant hydatid cases where the open surgery will entail a large incision and conventional laparoscopy will involve suboptimal outcome. This technique combines the advantage of open surgery as well as minimal access surgery and therefore is cost effective and can be easily be adopted in developing countries where the disease burden of hydatid is enormous.[10] Very few reports describe single-incision laparoscopy for hydatid cysts in children and recommend the use of expensive ports.[14] The technique described by the authors has all advantages of single-incision laparoscopy and is a trocar-less technique. Additional advantage is to be able to visualise cyst-biliary communications and effectively deal with them. As with any technique, there are few limitations of this technique such as the inability to handle deep-seated impalpable hydatid cysts which are otherwise easier to handle with the conventional laparoscopic approach and an obvious scar which is not at umbilicus albeit small.
CONCLUSION
SITE management of liver hydatid cyst seems to be a reliable treatment modality as it is minimally invasive, efficient, easy to perform and effective. Authors believe that this treatment modality should be taken as a preference for giant hydatid cyst management.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Gole S, Gole G, Satyanarayana V. Unusual presentation of hydatid cyst: A case series with review of literature. Internet J Parasit Dis. 2013;6:1–11. [Google Scholar]
- 2.Pukar MM, Pukar SM. Giant solitary hydatid cyst of spleen – A case report. Int J Surg Case Rep. 2013;4:435–7. doi: 10.1016/j.ijscr.2012.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hemmati SH. How to build a simple and safe laparoscopic hydatid evaluation system. JSLS. 2014;18 doi: 10.4293/JSLS.2014.00314. pii: e201400314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Palanivelu C, Senthilkumar R, Jani K, Rajan PS, Sendhilkumar K, Parthasarthi R, et al. Palanivelu hydatid system for safe and efficacious laparoscopic management of hepatic hydatid disease. Surg Endosc. 2006;20:1909–13. doi: 10.1007/s00464-005-0274-7. [DOI] [PubMed] [Google Scholar]
- 5.Acarli K. Controversies in the laparoscopic treatment of hepatic hydatid disease. HPB (Oxford) 2004;6:213–21. doi: 10.1080/13651820410024003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rihani HR, Nabulsi B, Yiadat AA, Al-Jareh BR. Laparoscopic approach to liver hydatid is it safe? JRMS. 2005;12:69–71. [Google Scholar]
- 7.Aghajanzadeh M, Aghajanzadeh G, Ebrahimi H, Jahromi SK, Maafi AA, Massahnia S. One stage operation for five giant hydatid cysts of both lungs and liver in a 20-year-old female. Tanaffos. 2012;11:52–4. [PMC free article] [PubMed] [Google Scholar]
- 8.Ali FM. Laparoscopic versus open management of hydatid cyst. World J Laparosc Surg. 2011;4:7–11. [Google Scholar]
- 9.Yagmur Y, Akbulut S, Gümüs S, Babür M, Can MA. Laparoscopic management of hydatid cyst of the liver. S Afr J Surg. 2016;54:14–17. [PubMed] [Google Scholar]
- 10.Vuitton DA, Millon L, Gottstein B, Giraudoux P. Proceedings of the international symposium. Parasite. 2014;21:28. [Google Scholar]
- 11.Sahin DA, Kusaslan R, Sahin O, Dilek ON. Huge hydatid cysts that arise from the liver, growing exophytically. Can J Surg. 2007;50:301–3. [PMC free article] [PubMed] [Google Scholar]
- 12.Vennarecci G, Manfredelli S, Guglielmo N, Laurenzi A, Goletti D, Ettorre GM. Major liver resection for recurrent hydatid cyst of the liver after suboptimal treatment. Updates Surg. 2016;68:179–84. doi: 10.1007/s13304-016-0368-x. [DOI] [PubMed] [Google Scholar]
- 13.Chowbey PK, Shah S, Khullar R, Sharma A, Soni V, Baijal M, et al. Minimal access surgery for hydatid cyst disease: Laparoscopic, thoracoscopic, and retroperitoneoscopic approach. J Laparoendosc Adv Surg Tech A. 2003;13:159–65. doi: 10.1089/109264203766207672. [DOI] [PubMed] [Google Scholar]
- 14.Karabicak I, Yuruker S, Seren DT, Kesicioglu T, Cinar H, Ozen N. Single incision laparoscopic surgery for hepatic hydatid disease. Report of a case. Ann Ital Chir. 2013;84:451–3. [PubMed] [Google Scholar]


