Abstract
Here, we report a case of repeated laparoscopic resection of extra-regional lymph node metastases in a patient after laparoscopic surgery for rectal cancer. A 72-year-old woman was diagnosed with upper rectal cancer and underwent laparoscopic low anterior resection and D3 dissection. The pathological stage was considered as T3, N2b, M0, Stage IIIC. Six months after the operation, positron emission tomography-computed tomography (PET-CT) showed fluorodeoxyglucose (FDG) accumulation in the infra-renal para-aortic lymph nodes (PALNs). Systemic chemotherapy was administered; however, chemotherapy was discontinued due to hemoptysis related to her pulmonary disease. Therefore, we performed laparoscopic PALN resection. Pathologically, one lymph node was diagnosed with a metastasis. Three months after the second operation, PET-CT identified FDG accumulation in the left lateral pelvic lymph nodes (LPLNs) and a PALN. Laparoscopic LPLN dissection and PALN resection through minilaparotomy were performed. Pathologically, lymph node metastases were diagnosed in both fields. Sixteen months after the 3rd operation, there is no recurrence.
Keywords: Laparoscopic surgery, lateral pelvic lymph node metastasis, para-aortic lymph node metastasis, rectal cancer
INTRODUCTION
An isolated para-aortic lymph node (PALN) recurrence after curative resection for colorectal cancer is a rare type of recurrence with an incidence of 1%–1.2%.[1,2] PALN metastases are frequently associated with other distant metastases. In patients with isolated extra-regional lymph node recurrence, there is no standardised treatment.
Here, we report a case of repeated laparoscopic resection of extra-regional lymph node metastases in a patient who underwent laparoscopic radical resection for rectal cancer.
CASE REPORT
A 72-year-old women with upper rectal cancer underwent laparoscopic low anterior resection and D3 lymph node dissection.[3] The pathological diagnosis was a moderately differentiated adenocarcinoma, and the final stage was pT3, N2b, M0 and pStage IIIC (TNM classification). Post-operative adjuvant chemotherapy with capecitabine and oxaliplatin regimen was administered. Six months after the operation, her serum carcinoembryonic antigen level was elevated and positron emission tomography-computed tomography (PET-CT) revealed the accumulation of fluorodeoxyglucose (FDG) in the infrarenal PALN, located around the dorsal side of the inferior mesenteric artery root [Figure 1]. We changed to systemic chemotherapy with 5-fluorouracil, leucovorin and oxaliplatin plus panitumumab regimen; however, the chemotherapy was discontinued due to hemoptysis related to her pulmonary non-tuberculous mycobacterial infection. Therefore, we decided to conduct surgical treatment and performed laparoscopic PALN resection 13 months after the first operation.
Figure 1.
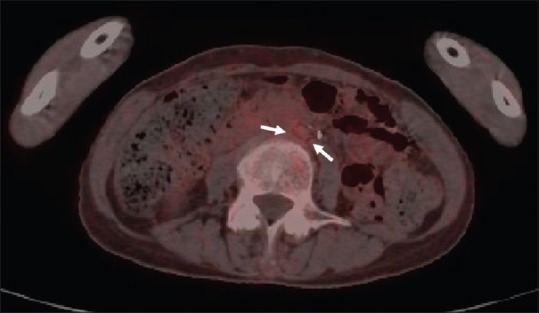
Positron emission tomography-computed tomography revealed the accumulation of fluorodeoxyglucose in the infra-renal para-aortic lymph nodes (arrows)
Procedure of the second operation and clinical course
Under general anaesthesia, we placed five ports the same as the first operation. The anterolateral side of the abdominal aorta and left common iliac artery were dissected using laparoscopic coagulating shears. The left ureter was dissected and retracted to the ipsilateral abdominal wall with the Teflon tape to clarify the lateral margin and avoid urinary injury. The PALN specimens were dissected upwards to preserve the inferior mesenteric vein [Figure 2a]. Finally, the specimens were cranially ligated with clips below the renal vein [Figure 2b]. Pathologically, one lymph node out of 13 harvested PALNs was diagnosed as metastasis. The patient was discharged on post-operative day 14 without complications.
Figure 2.
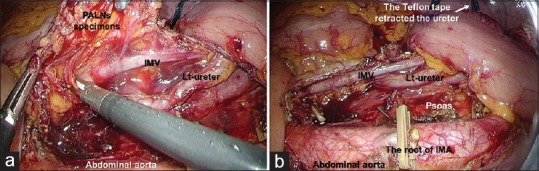
(a) Operative finding during PALN resection the resected specimens included PALNs are dissected the upwards to keep the IMV. IMV: Inferior mesenteric vein, PALN: Para-aortic lymph node. (b) Operative finding after PALN resection Psoas: Psoas muscle
Three months after the second operation, PET-CT showed FDG accumulation in the right lateral pelvic lymph nodes (LPLNs) and in a PALN. We diagnosed lymph node metastases in both fields. Five months after the second operation, we planned a surgical resection of the right LPLNs and the PALN.
Procedure on the third operation and clinical course
Five ports were placed in total the same as the previous two operations. During dissection of the right LPLN field, the right ureter was retracted to the contralateral abdominal wall to keep the hypogastric nerve, plexus and prehypogastric nerve fascia to the medial side. Dissection for the right LPLNs metastases was laparoscopically performed [Figure 3a]. However, the PALN was resected through minilaparotomy because the PALN in the aortocaval area was hardly adherent to the inferior vena cava [Figure 3b]. Pathologically, five lymph nodes out of 17 LPLNs and one PALN were diagnosed with metastases. The post-operative course was uneventful and the patient was discharged on post-operative day 9. Sixteen months after the 3rd operation, there is no recurrence.
Figure 3.
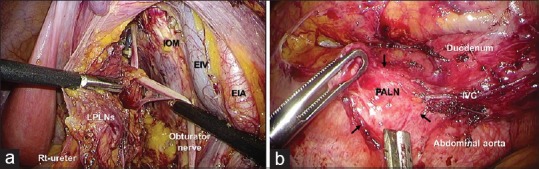
(a) LPLN dissection EIA: External iliac artery, EIV: External iliac vein, IOM: Internal obturator muscle, LPLN: Lateral pelvic lymph node. (b) PALN resection A PALN in the aortocaval area was hardly adherent to the inferior vena cava (arrows). Finally, the PALN was resected via mini-laparotomy. IVC: Inferior vena cava, PALN: Para-aortic lymph node
DISCUSSION
Isolated PALN recurrence after curative resection for colorectal cancer is a rare type of recurrence with an incidence of 1%–1.2%.[1,2] PALN metastases are frequently associated with other distant metastases. In patients with isolated extra-regional lymph node recurrence, treatment has not been standardised. The surgical management of isolated extra-regional lymph node metastasis, including PALN, remains controversial. However, some studies have recently suggested that surgical treatment for metachronous isolated PALN metastasis below the renal vessel may have contributed to better outcomes compared to patients without surgical treatment.[1,2]
Laparoscopic surgery has been widely employed for colorectal cancer treatment. Lately, the laparoscopic approach has been used for more complicated procedures in patients with colorectal cancer, such as multivisceral resection and LPLN dissection in advanced colorectal cancer and intersphincteric resection in very low rectal cancer.[4,5] In selected patients with synchronous or metachronous isolated PALN metastases, it has been reported to be a feasible and safe laparoscopic procedure.[6,7]
In the western countries, LPLN is considered to be an extra-regional lymph node and therefore LPLN metastasis is defined as systemic disease. However, in the 2014 Japanese Society for Cancer and Rectum Guideline for treatment of colorectal cancer,[3] LPLN is considered to be a regional lymph node in patients with lower rectal cancer. After performing LPLN dissection for locally advanced lower rectal cancer, it is expected that 5-year survival improves by 8%–9%. Lately, laparoscopic LPLN dissection has been introduced.[4] After PALN resection, recurrences occur in approximately 70% of cases and multiple organ recurrence occurs in 60%. Moreover, the most commonly affected sites are the PALNs and repeated PALN resection has previously been performed in only one out of 16 patients after PALN resection.[2]
We conclude that laparoscopic PALN resection and LPLN dissection in patients with isolated extra-regional lymph node recurrences of colorectal cancer can be a feasible and safe approach in selected patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Min BS, Kim NK, Sohn SK, Cho CH, Lee KY, Baik SH, et al. Isolated paraaortic lymph-node recurrence after the curative resection of colorectal carcinoma. J Surg Oncol. 2008;97:136–40. doi: 10.1002/jso.20926. [DOI] [PubMed] [Google Scholar]
- 2.Choi PW, Kim HC, Kim AY, Jung SH, Yu CS, Kim JC. Extensive lymphadenectomy in colorectal cancer with isolated paraaortic lymph node metastasis below the level of renal vessels. J Surg Oncol. 2010;101:66–71. doi: 10.1002/jso.21421. [DOI] [PubMed] [Google Scholar]
- 3.Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2014 for treatment of colorectal cancer. Int J Clin Oncol. 2015;20:207–39. doi: 10.1007/s10147-015-0801-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Furuhata T, Okita K, Nishidate T, Ito T, Yamaguchi H, Ueki T, et al. Clinical feasibility of laparoscopic lateral pelvic lymph node dissection following total mesorectal excision for advanced rectal cancer. Surg Today. 2015;45:310–4. doi: 10.1007/s00595-014-0906-4. [DOI] [PubMed] [Google Scholar]
- 5.Fujii S, Yamamoto S, Ito M, Yamaguchi S, Sakamoto K, Kinugasa Y, et al. Short-term outcomes of laparoscopic intersphincteric resection from a phase II trial to evaluate laparoscopic surgery for stage 0/I rectal cancer: Japan Society of Laparoscopic Colorectal Surgery Lap RC. Surg Ensdosc. 2012;26:3067–76. doi: 10.1007/s00464-012-2317-1. [DOI] [PubMed] [Google Scholar]
- 6.Song SH, Park SY, Park JS, Kim HJ, Yang CS, Choi GS, et al. Laparoscopic para-aortic lymph node dissection for patients with primary colorectal cancer and clinically suspected para-aortic lymph nodes. Ann Surg Treat Res. 2016;90:29–35. doi: 10.4174/astr.2016.90.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liang JT. Surgical techniques of laparoscopic peritonectomy plus paraaortic lymph node dissection for the treatment of patients with positive lymph node metastasis and peritoneal seeding from rectosigmoid cancer. Surg Endosc. 2012;26:2383–7. doi: 10.1007/s00464-012-2163-1. [DOI] [PubMed] [Google Scholar]


