Abstract
OBJECTIVE
To describe our experience with the circle nephrostomy tube (NT) (Cook Medical), a drainage system uniquely designed for use after multiple-access percutaneous nephrolithotomy (PNL).
METHODS
A retrospective review of 1317 consecutive patients undergoing 1599 PNLs at IU Health Methodist Hospital was performed. All multiple access cases utilizing circle NTs were reviewed and analyzed. The method of insertion of circle NT was demonstrated.
RESULTS
A total of 1843 accesses were obtained in 1599 renal units (RUs): 380 upper pole, 129 interpolar, and 1334 lower pole. Multiple accesses in this series were required in 282 RUs (17.6%). Following multiple-access PNL, circle NTs, Cope loop, and reentry Malecot NTs were inserted in 91 RUs (32.3%), 208 RUs (73.8%), and 31 RUs (11%), respectively. None of the patients who had circle NT experienced clogging, dislodgement, or obstruction of the tube. The cost of circle, Cope loop, and Malecot NTs are 121.73 USD, 95.20 USD, and 81 USD, respectively.
CONCLUSION
Circle NTs are easy to insert, secure, cost-effective compared with inserting two NTs. Circle NTs provide excellent drainage and facilitate secondary procedures.
Percutaneous nephrolithotomy (PNL) is the preferred approach for managing large and complex kidney stones.1 A percutaneous approach allows complete stone removal even in the largest of stones through one or more accesses and obviates open stone removal. Indications for PNL include conditions such as staghorn calculi, lower pole stones, calyceal diverticular calculi, ectopic kidneys with stones, failure of ureteroscopy or lithotripsy, or stone removal, with planned concurrent procedures such as antegrade endopyelotomy. Multiple access is sometimes necessary to achieve complete stone clearance.2
Post-procedural nephrostomy tube (NT) placement is generally recommended for drainage, as well as for maintaining access in the event a secondary stone procedure is necessary. The choice of NT placement after PNL varies widely by provider,3–5 and there has been a recent trend to minimize NT use or abandoning it altogether.6–8 However, a tubeless approach is applicable only in select straightforward cases9 and not when multiple-access tracts are made, as such complex cases have a higher potential for morbidity, bleeding, obstruction, and need for secondary procedures.10
As previously reported by Kim et al, NTs available are Cope loop, reentry Malecot catheters (Boston Scientific Corp., Natick, MA), Foley catheters, and circle NT.2 At our institution, it is our custom to leave the smallest NT for a single-puncture PNL and the circle NT for multiple-access PNL. Despite perceived advantages in terms of security, drainage, comfort, and cost, there are few reports on the use of circle NT in the medical literature.11 Herein we describe and demonstrate the use of the circle NT (Cook Medical, Bloomington, IN) following complex PNL.
METHODS
After an institutional review board approval, a retrospective review of 1317 consecutive patients who had 1599 PNLs done by multiple surgeons at IU Health Methodist Hospital from January 2003 to June 2014 was performed. Cases with renal units (RU) treated with multiple accesses were reviewed and analyzed. Demographic data, number and location of accesses, NTs used, and complications were recorded. All accesses were obtained by the urologist whereby access to the desired calyx is obtained using an 18-gauge diamond-tipped needle utilizing a fluoroscopic triangulation technique.12 A Boston Scientific NephroMax balloon is then used to dilate the tract and place a 30F Amplatz sheath. Rigid nephroscopy is performed and an ultrasonic lithotrite is utilized for stone fragmentation. Once stone material accessible to rigid instruments is removed, the flexible nephroscope is used to assess the remainder of the kidney. If a substantial amount of stone (>2 cm) remains in a location not otherwise accessible to rigid instruments, additional access is obtained. In cases needing only a single access, a 10F Cope loop NT is placed and a 5-French open-ended ureteral catheter is left down the ureter to help secure access.13 Antegrade double J ureteral stents are not used unless concomitant ureteric or ureteropelvic junction pathology is encountered.
A non-contrast computed tomography scan is routinely obtained the morning after surgery to assess for any residual fragments or complications. If there are any residual stones, a secondary procedure is performed. Once deemed stone-free, a nephrostogram is routinely performed to assess for adequate antegrade drainage. If the ureter is patent, the NT is removed.
Technique of Insertion
In the case of multiple-access PNL, a circle NT (Cook Medical) is commonly utilized (Supplementary Video S1). The circle NT consists of a silicon circle nephrostomy catheter, 30-cm polyvinyl chloride connecting tube, and a Y connector. Circle NTs come in 4 different sizes, 14–20F, and have 2 radio-opaque markers to facilitate proper positioning inside the kidney (Fig. 1).
Figure 1.
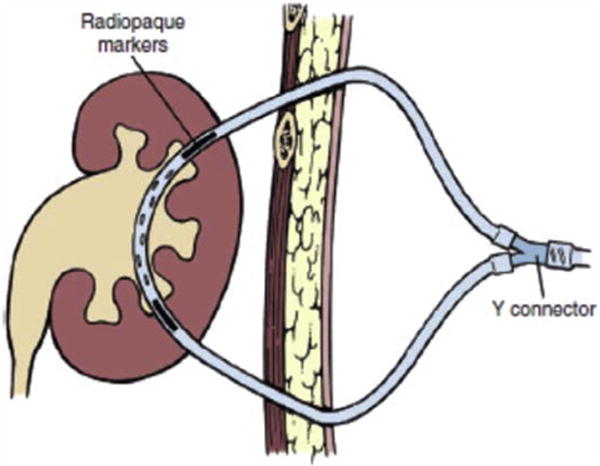
Circle nephrostomy tube (Campbell-Walsh Urology. 10th ed. Philadelphia, Saunders [an imprint of Elsevier Science], Chapter 47, p. 1344, 2012). (Color version available online.)
After obtaining additional access, a 0.035 zip wire is passed into the collecting system and identified by the flexible nephroscope. A 5F flexible grasper is utilized to pull the wire through the initial access (Fig. 2A). Once through and through access is obtained, the zip wire is exchanged for a stiffer working wire. Dilatation and utilization of the additional access are performed as described above.
Figure 2.
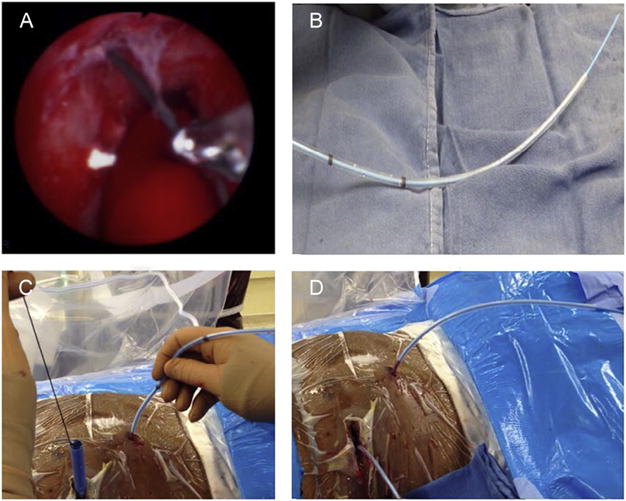
(A) Identifying the zip wire and gaining through and through access; (B) preparing the circle nephrostomy tube; (C) push and pull maneuver; and (D) both ends of the tube through both access. (Color version available online.)
Prior to placement, the circle NT is prepared on the back table by inserting an 8F coaxial dilator through its lumen (Fig. 2B). This is facilitated if the circle NT is wet first. The tube is then passed over the working wire from either direction (Fig. 2C). Hemostats are placed on both ends of the wire at the end of the 8F coaxial dilator to facilitate passing of the tube, and a push-pull maneuver is then used to pass the tube from one point of access to the other. Once both ends of the tubes can be seen emerging from the skin, the Amplatz sheaths, working wire, and the coaxial dilator are removed (Fig. 2D). The tube is then positioned within the kidney using the radio-opaque markers and fluoroscopic guidance. Contrast is injected to confirm proper positioning (Fig. 3A,B). The silicon tubing is cut to the desired length and attached to the Y connector and the drainage bag (Fig. 3C). The tube is then secured to the skin using 2-0 silk suture (Fig. 3D).
Figure 3.
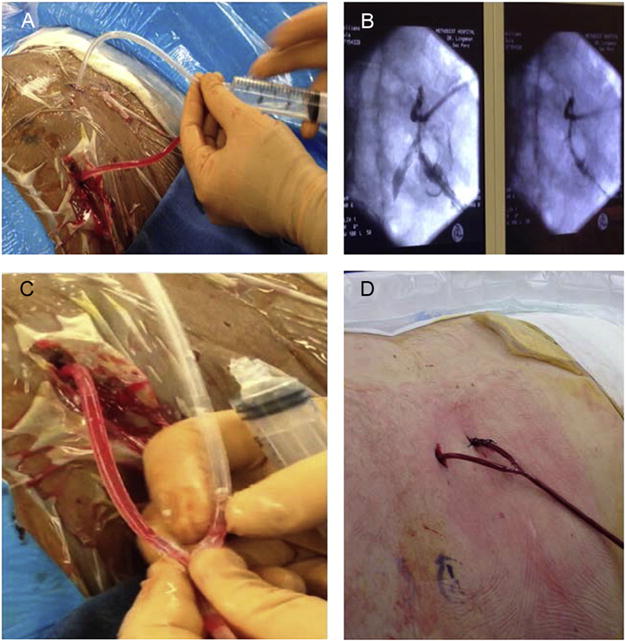
(A) Injection of contrast material; (B) positioning of the nephrostomy tube within the kidney; (C) attaching the Y connector to both ends of the tubes; and (D) securing the tube to the skin. (Color version available online.)
Gaining Access for a Secondary Procedure Through the Circle NT
The 2 ends of the pre-placed circle NT are cut (Fig. 4A), and a straight moveable core wire is advanced through one end of the NT while the other end is concomitantly pulled. Fluoroscopy is usually not required for this maneuver. Both access sites can then be utilized as needed (Fig. 4B,C).
Figure 4.
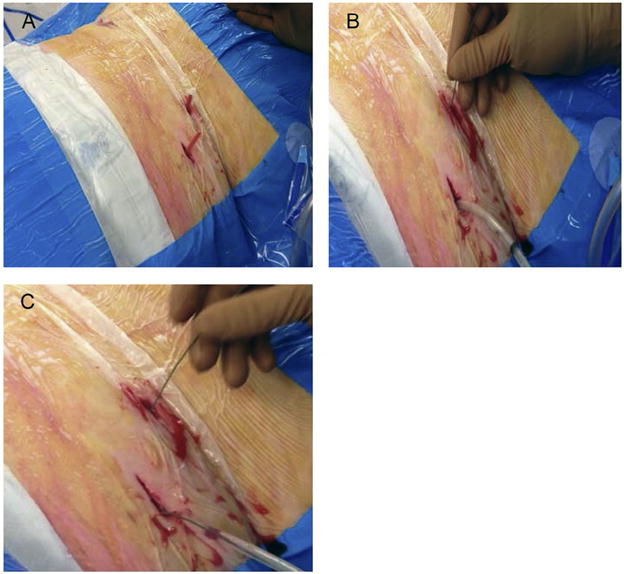
(A) Preparing the nephrostomy tube for the secondary procedure by cutting both ends to the appropriate length; (B) soft tip wire is advanced through one end of the tube; and (C) push and pull maneuver until the wire is through and through. (Color version available online.)
RESULTS
Of the 1317 patients studied, a total of 1843 accesses were obtained in 1599 RUs: 380 upper pole, 129 interpolar, and 1334 lower pole. Multiple accesses were performed in 282 RUs (17.6%), with a total of 573 additional accesses. Of these additional accesses, 175, 66, and 332 accesses were placed in the upper pole, interpolar, and lower pole, respectively.
Following multiple-access PNL, every RU was left with at least 1 NT. A total of 330 NTs were placed in the additional 573 accesses: 70 NTs in the upper pole, 48 interpolar, and 303 in the lower pole. Circle NTs, Cope loop, and reentry Malecot catheter were placed in 91, 208, and 31 RUs, respectively. Eighty-four patients with circle NTs required secondary percutaneous procedures. The average body mass index in the circle NT cohort was 38.9.
The overall transfusion rate was 3.49% in multiple accesses cases compared with 2.5% in single access cases (P = 1). The use of circle NT had no influence on the risk of hemorrhage. The postoperative hemoglobin was 10.9 for both circle NT and any other NT (P = .9). No complications were attributed to the insertion of the circle NT. There was no difference in infections, complications, or readmission rates among the various NTs. None of these patients experienced clogging, dislodgement, or obstruction of the tube.
The costs of circle, Cope loop, and reentry Malecot are 121.73 USD, 95.20 USD, and 81 USD, respectively. Despite being more expensive than any other single NT, the circle NT is cheaper when considering placing an NT in each access.
DISCUSSION
It is well accepted that PNL is the gold standard management for renal stones larger than 2 cm. The decision and choice to leave a NT after surgery, however, remains controversial.1–6 Despite the innovation in terms of NT design over the years since the introduction of PNL in 1976,14 very few publications have addressed NT selection postoperatively.2,11
We believe that the circle NT offers an optimal choice of drainage after multiple-access PNL. Besides the demonstrated cost savings of using a singular drainage tube rather than combining 2 separate alternative NTs, we believe the circle NT has several other unique advantages as well.
There were no instances of tube dislodgment when this device was used. This is due to the through and through nature of the tube design whereby each end is secured externally, creating a loop within the kidney. Tube security is an important factor to consider when choosing an appropriate NT, as rates of dislodgment can vary between 1% and 30%.15,16 Bayne et al reported body mass index as a sole determinant of NT dislodgment, with a rate of 6%. However, the choices of NTs were only Malecot, Cope loop, and Foley, without mentioning the circle NT as a secure option.17
Another benefit of the circle NT is that it is available in a variety of sizes. Large-diameter NTs have been proven to cause more pain, discomfort, and need for analgesics.7,8,18 As reported by Pietrow et al,7 Maheshwari et al,8 and Liatsikos et al,18 there is a relationship between the size of NT and pain. However, no circle NT was studied in these series. NT sizes have evolved from initial sizes of 24–28F to smaller sized tubes of 8.5–10F.2,6,10,19–21 Circle NT comes in sizes of 14–20F, and although these are slightly larger than some alternative NTs we believe that the relatively larger size is sometimes necessary, especially for complicated cases where maximal drainage is warranted and secondary procedures are often needed. Furthermore, the soft silicon material of the circle NT differs from the traditional harder material of a Cope loop or Malecot. Although no formal pain assessments have been performed to date, it is our anecdotal experience that patients rarely complain of significant discomfort when such tubes are utilized.
The tubeless PNL technique has gained popularity since its introduction in the late 1990s.22 However, it should only be used in selected patients, excluding patients with intraoperative bleeding, questionable residual stones, multiple-access PNL, chronic kidney disease, and supracostal approaches.23,24
At our institution, in multiple-access PNL, each RU gets at least 1 NT. For combined upper pole and either lower pole or interpolar access, if complete stone clearance has been achieved, a 10F Cope loop is inserted through one access, whereas the upper pole access is left tubeless to minimize the pain from inserting the tube between the ribs. In our series, 105 out of 175 (60%) upper poles accessed in multiple access cases have been left tubeless. The use of circle NT for multiple-access PNL is performed if there is a possible need for a secondary procedure, risk of dislodgement of the tube especially in patients with high body mass index, or if there is unusual intraoperative bleeding that warrants maximal drainage. None of the patients who had circle NT experienced clogging or obstruction of the tube, likely due to the presence of multiple side holes which allow maximal drainage.
Gaining access for a secondary procedure is easy and quick with circle NT. Feeding a soft tip wire from one end to another is a simple, risk-free procedure, uses little or no flouroscopy, utilizes both tracts, and saves times when compared with gaining access through multiple tubes.
This study is not devoid of limitations. It is retrospective in nature, although the data are collected in a prospective fashion to minimize bias. As this study spans a 12-year period, differences in patients, experience of surgeon, and techniques may exist. Despite these limitations, this study is the first to focus on circle NT and the method of its insertion.
In summary, circle NT offers a cost-effective, secure, and reliable method of drainage and reaccess after multiple-access PNL.
CONCLUSION
Circle NTs are easy to insert as demonstrated, and provide secure access and optimal drainage. Circle NTs come in a variety of sizes (14–20F), facilitate secondary procedures, and are cost-effective when compared with inserting 2 Cope loops or reentry Malecot.
Supplementary Material
APPENDIX
Supplementary Data
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.urology.2017.01.012.
Footnotes
Financial Disclosure: The authors declare that they have no relevant financial interests.
References
- 1.Preminger GM, Assimos DG, Lingeman JE, et al. Chapter 1: AUA guideline on management of staghorn calculi: diagnosis and treatment recommendations. J Urol. 2005;173:1991–2000. doi: 10.1097/01.ju.0000161171.67806.2a. [DOI] [PubMed] [Google Scholar]
- 2.Kim SC, Tinmouth WW, Kuo RL, et al. Using and choosing a nephrostomy tube after percutaneous nephrolithotomy for large or complex stone disease: a treatment strategy. J Endourol. 2005;19:348–352. doi: 10.1089/end.2005.19.348. [DOI] [PubMed] [Google Scholar]
- 3.Agrawal MS, Agarwal M. Percutaneous nephrolithotomy: large tube, small tube, tubeless, or totally tubeless? Indian J Urol. 2013;29:219–224. doi: 10.4103/0970-1591.117285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agrawal MS, Agrawal M. Are multiple nephrostomy tubes necessary after multitract percutaneous nephrolithotomy? A randomized comparison of single versus multiple nephrostomy tubes. J Endourol. 2009;23:1831–1834. doi: 10.1089/end.2008.0452. [DOI] [PubMed] [Google Scholar]
- 5.Resorlu B, Kara C, Sahin E, et al. Comparison of nephrostomy drainage types following percutaneous nephrolithotomy requiring multiple tracts: single tube versus multiple tubes versus tubeless. Urol Int. 2011;87:23–27. doi: 10.1159/000324264. [DOI] [PubMed] [Google Scholar]
- 6.Segura JW, Patterson DE, LeRoy AJ, et al. Percutaneous removal of kidney stones: review of 1,000 cases. J Urol. 1985;134:1077–1081. doi: 10.1016/s0022-5347(17)47633-6. [DOI] [PubMed] [Google Scholar]
- 7.Pietrow PK, Auge BK, Lallas CD, et al. Pain after percutaneous nephrolithotomy: impact of nephrostomy tube size. J Endourol. 2003;17:411–414. doi: 10.1089/089277903767923218. [DOI] [PubMed] [Google Scholar]
- 8.Maheshwari PN, Andankar MG, Bansal M. Nephrostomy tube after percutaneous nephrolithotomy: large-bore or pigtail catheter? J Endourol. 2000;14:735–737. doi: 10.1089/end.2000.14.735. discussion 737–738. [DOI] [PubMed] [Google Scholar]
- 9.Monga M. Percutaneous nephrolithotomy: leave a tube! J Endourol. 2008;22:1863–1864. doi: 10.1089/end.2008.9789. discussion 1871. [DOI] [PubMed] [Google Scholar]
- 10.Shah HN, Sodha HS, Khandkar AA, et al. A randomized trial evaluating type of nephrostomy drainage after percutaneous nephrolithotomy: small bore v tubeless. J Endourol. 2008;22:1433–1439. doi: 10.1089/end.2007.0350. [DOI] [PubMed] [Google Scholar]
- 11.Paul EM, Marcovich R, Lee BR, et al. Choosing the ideal nephrostomy tube. BJU Int. 2003;92:672–677. doi: 10.1046/j.1464-410x.2003.04454.x. [DOI] [PubMed] [Google Scholar]
- 12.Miller NL, Matlaga BR, Lingeman JE. Techniques for fluoroscopic percutaneous renal access. J Urol. 2007;178:15–23. doi: 10.1016/j.juro.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 13.Kim SC, Kuo RL, Lingeman JE. Percutaneous nephrolithotomy: an update. Curr Opin Urol. 2003;13:235–241. doi: 10.1097/00042307-200305000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Fernström I, Johansson B. Percutaneous pyelolithotomy. A new extraction technique. Scand J Urol Nephrol. 1976;10:257–259. doi: 10.1080/21681805.1976.11882084. [DOI] [PubMed] [Google Scholar]
- 15.Saad WEA, Virdee S, Davies MG, et al. Inadvertent discontinuation of percutaneous nephrostomy catheters in adult native kidneys: incidence and percutaneous management. J Vasc Interv Radiol. 2006;17:1457–1464. doi: 10.1097/01-RVI.0000235703.68819.8C. [DOI] [PubMed] [Google Scholar]
- 16.Mahaffey KG, Bolton DM, Stoller ML. Urologist directed percutaneous nephrostomy tube placement. J Urol. 1994;152:1973–1976. doi: 10.1016/s0022-5347(17)32282-6. [DOI] [PubMed] [Google Scholar]
- 17.Bayne D, Taylor ER, Hampson L, et al. Determinants of nephrostomy tube dislodgment after percutaneous nephrolithotomy. J Endourol. 2015;29:289–292. doi: 10.1089/end.2014.0387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liatsikos EN, Hom D, Dinlenc CZ, et al. Tail stent versus re-entry tube: a randomized comparison after percutaneous stone extraction. Urology. 2002;59:15–19. doi: 10.1016/s0090-4295(01)01475-3. [DOI] [PubMed] [Google Scholar]
- 19.White EC, Smith AD. Percutaneous stone extraction from 200 patients. J Urol. 1984;132:437–438. doi: 10.1016/s0022-5347(17)49683-2. [DOI] [PubMed] [Google Scholar]
- 20.Goldwasser B, Weinerth JL, Carson CC, et al. Factors affecting the success rate of percutaneous nephrolithotripsy and the incidence of retained fragments. J Urol. 1986;136:358–360. doi: 10.1016/s0022-5347(17)44868-3. [DOI] [PubMed] [Google Scholar]
- 21.Clayman RV, Surya V, Miller RP, et al. Percutaneous nephrolithotomy: extraction of renal and ureteral calculi from 100 patients. J Urol. 1984;131:868–871. doi: 10.1016/s0022-5347(17)50686-2. [DOI] [PubMed] [Google Scholar]
- 22.Bellman GC, Davidoff R, Candela J, et al. Tubeless percutaneous renal surgery. J Urol. 1997;157:1578–1582. [PubMed] [Google Scholar]
- 23.Goh M, Wolf JS. Almost totally tubeless percutaneous nephrolithotomy: further evolution of the technique. J Endourol. 1999;13:177–180. doi: 10.1089/end.1999.13.177. [DOI] [PubMed] [Google Scholar]
- 24.Shoma AM, Elshal AM. Nephrostomy tube placement after percutaneous nephrolithotomy: critical evaluation through a prospective randomized study. Urology. 2012;79:771–776. doi: 10.1016/j.urology.2011.09.042. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


