Abstract
Background
The etiopathology of multiple sclerosis (MS) is believed to include genetic and environmental factors. Human leukocyte antigen (HLA) alleles, in particular, are associated with disease susceptibility, whereas Epstein Barr Virus (EBV) infection has long been suspected to play a role in disease pathogenesis. The aim of the present study is to evaluate correlations between HLA alleles and EBV infection in MS.
Methods
HLA alleles, EBV viral load (VL) and serum anti-EBV antibody titers were evaluated in EBV-seropositive MS patients (N = 117) and age- and sex-matched healthy controls (HC; N = 89).
Results
Significantly higher DNA viral loads (p = 0.048) and EBNA-1 antibody titer (p = 0.0004) were seen in MS compared to HC. EBV VL was higher in HLA-B*07+ (p = 0.02) and HLA-DRB1*15+ (p = 0.02) MS patients, whereas it was lower in HLA-A*02+ (p = 0.04) subjects. EBV VL was highest in HLA-A*02−/B*07+/DRB1*15+ patients and lowest in HLA-A*A02+/B*07−/DRB1*15− individuals (p < 0.0001). HLA-B*07 resulted the most associated allele to EBV VL after multiple regression analysis considering altogether the three alleles, (p = 0.0001). No differences were observed in anti-EBV antibody titers in relationship with HLA distribution.
Conclusions
Host HLA-B*07 allele influence EBV VL in MS. As HLA-class I molecules present antigens to T lymphocytes and initiate immune response against viruses, these results could support a role for EBV in MS.
Electronic supplementary material
The online version of this article (10.1186/s12967-018-1450-6) contains supplementary material, which is available to authorized users.
Keywords: Epstein-Barr virus, HLA-class I alleles, HLA-A*02, HLA-B*07, Multiple sclerosis, Immunogenetics
Background
Multiple sclerosis (MS), a chronic inflammatory disease of the central nervous system (CNS), is the most common cause of neurological disability in adults, and it affects over 2.5 million people worldwide [1]. The etiopathogenesis of the disease is still unclear and is believed to include both environmental and genetic factors, whose interplay leads to chronic activation of immune cells and neuronal damage. The major human leukocyte antigens (HLA) locus (6p21.3), in particular, was identified as the chromosomal region most strongly linked to MS [2], and a number of epidemiological studies identified HLA alleles that correlate with an increased risk of developing MS and that can influence disease progression in patients. Notably, the realization that different HLA alleles play a role in MS led to the understanding that this disease is, above all, an antigen-specific autoimmune disease [3]. To date, HLA-DRB1*15 is the strongest risk factor for the development of MS [4]. HLA-DRB1*15 is nevertheless not the only HLA allele related to MS: HLA-B*07+ patients are characterized by higher disease burdens and by a more evident degree of brain atrophy [5]. The presence of the HLA-A*02 allele, on the other hand, seems to be a protective factor against MS [6] and, in patients with the disease, it results in a more favorable clinical course, with a slower progression and a lower disease burden [7].
Amongst environmental factors, chronic viral infections, including those supported by Epstein Barr virus (EBV), are suspected to be involved in the initiation of MS [8]. EBV (also called human herpesvirus 4, HHV-4) is a ubiquitous human virus with a double stranded DNA genome (172 kbp long) wrapped in a protein capsid belonging to the Herpesviridae family, Gammaherpesvirinae subfamily, Lymphocryptovirus genus [9]. The virus is a worldwide pathogen and is persistently harbored by almost all adults regardless of health or geographic location. In western countries, with high standard of living, primary EBV infection occurs commonly in adolescence, and might cause infectious mononucleosis (IM) in a minority of cases. EBV replicates in oropharyngeal epithelial cells during primary disease and subsequently establishes a latent infection in circulating B lymphocytes.
IM and elevated titers of antibodies against EBV nuclear antigens (EBNA) have been associated to an increased risk to develop MS and, on the other hand, lack of EBV infection correlates with a lower risk to develop the disease [8]. Other epidemiologic results suggesting a role for EBV in the pathogenesis of MS include the observations that EBV-infected B cells and plasma cells accumulate in the brain of MS patients [10] and a strong EBV specific cell-mediated immune responses are seen in these patients [11, 12].
Moreover, evidences of EBV DNA or transcripts in brain or cerebrospinal fluid of MS individuals remains controversial [13], as reported by some papers [10, 14], but not confirmed by other authors [15–17].
Confliting results are reported on possible correlations between HLA alleles, EBV infection, and MS [18, 19]. Thus, an interaction between HLA-class I alleles and reactivity to EBV-related epitopes was recently shown, suggesting that the mechanism through which HLA genes influence the risk of developing MS may involve EBV-specific immune responses [18, 20]. Other data showed that HLA-B*7 allele is associated with increased EBV-specific Ab titers, higher disability scores, and a more compromised MRI pattern in MS patients [21]. We verified if correlations could be established between protective/risk HLA-class I alleles and EBV-specific parameters in MS; results suggest that this is indeed the case.
Methods
Study population and specimens
A total of 206 individuals were enrolled in the study: 117 of them (mean age: 44.7 ± 12.6 years) were patients with a diagnosis of MS according to revised McDonald criteria [22]; these patients are followed by the Multiple Sclerosis Unit of the Don C. Gnocchi Foundation, IRCCS S. Maria Nascente in Milan, Italy, and by the MS Centers of the PROGEMUS Consortium, coordinated at the University of Piemonte Orientale. The remaining 89 individuals (mean age: 44.8 ± 10.8 years) were age- and sex-matched healthy controls (HC), who donate blood at the same institutions. HC and MS patients were selected in order to obtain comparable distribution of HLA-B*07, -A*02 and -DRB1*15 frequency.
All individuals were EBV-seropositive. The study conformed to the ethical principles of the Declaration of Helsinki; all subjects gave informed and written consent according to a protocol approved by the local ethics committee of the centers.
Whole blood and serum samples were collected from all the individuals enrolled in the study. Whole blood was utilized for DNA extraction, whereas serum samples, obtained by centrifugation for 10 min at 1800g at room temperature, were aliquoted into sterile cryovials and stored at − 20 °C.
DNA extraction
Genomic DNA was extracted from whole blood using standard phenol/chloroform procedure. DNA amount for each sample was determined by measuring the optical density at 260 nm wavelengths. DNA samples were stored at − 20 °C until use.
HLA genotyping
The molecular genotyping of HLA-class I (HLA-A: 18 alleles and HLA-B: 38 alleles) and HLA-class II polymorphisms (HLA-DRB1: 18 alleles) was performed as previously described [23, 24].
ELISA analysis
EBV seropositivity was measured in serum using commercial enzyme immunoassays (BEIA EBV EBNA-1 IgG Quant, Technogenetics, Milan, Italy, and EBV viral capsid antigen (VCA) IgG ELISA, IBL International, Hamburg, Germany), according to the manufacturer instructions.
EBNA-1-specific Ab (U/ml) were considered positive if > 180 U/ml, or negative if < 150 U/ml. Samples in grey zone (between 150 and 180 U/ml) were re-tested using the same immunoassay, and if repeatedly resulted in the grey zone, they was excluded from the analysis.
VCA-specific Ab (U/ml) were considered positive if > 22 U/ml, or negative if < 8 U/ml. Samples in grey zone (between 8 and 22 U/ml) were re-tested using the same immunoassay, and if repeatedly resulted in the grey zone, they was excluded from the analysis.
Cytomegalovirus (CMV) seropositivity was measured in serum using commercial enzyme immunoassay (CMV IgG ELISA, IBL International), according to the manufacturer instructions.
CMV IgG-specific Ab (U/ml) were considered positive if > 12 U/ml, or negative if < 8 U/ml. Samples in grey zone (between 8 and 12 U/ml) were re-tested using the same immunoassay, and if repeatedly resulted in the grey zone, they was excluded from the analysis.
EBV and CMV DNA viral load
500 ng of genomic DNA was used as the template for quantitative evaluation by quantitative PCR (qPCR) using the ABI Prism 7000 sequence detection system (Applied Biosystems, Foster City, CA, US), and following a previously described protocol [25]. For EBV, the sequences of primers and probes were designed by Applied Biosystems on EBNA-LP region, whereas for CMV, primers CMVF (5′-CGCTCACATGCAAGAGTTAATCTTT), CMVR (5′AACTCGGTAAGTCTGTTGACATGTATG) and probe CMVP (FAM-CTCTATCTGACATACACAAGTAAATCCACGTCCCA-TAMRA) were selected from the UL123 gene using the Primer Express version 2.0.0 software. The EBNA-LP region is rich of variable copy numbers of a repeat domain: although the primers/probes were optimized by a commercial company, an effect on the results can’t be categorically exclude. EBV and CMV viral load was measured on a single occasion in each patient; each sample was tested in triplicate. Negative controls, as well as serial dilutions (from 104 to 10 copies/μl for both EBV and CMV) of commercially available viral genomes (Advanced Biotechnologies Inc., Columbia, MD, USA), were included in each run. For both EBV and CMV the detection limit of this specific qPCR assay was 2.1 copies/μg DNA.
Statistical analysis
Normally distributed data were summarized as mean and standard deviation (SD), or standard error mean (SEM), and comparison among groups were analyzed by ANOVA test and Student t test. Not-normally distributed data were summarized as median and interquartile range (IQR: 25th and 75th percentile), and comparisons were analyzed by Kruskal–Wallis test and Mann–Whitney U test, as appropriate. Multiple regression analysis was performed to verify the possible association between viral data and genetic parameters. Qualitative data were compared using Fisher’s exact test.
Results
Clinical characterization of study subjects
Clinical characteristics of the individuals enrolled in the study are shown in Table 1. Demographic analysis showed that age and sex were not different when MS patients and HC were compared. Among MS patients, 77 were affected by relapsing–remitting disease (RR-MS) in a phase of disease stability, whereas 40 had a diagnosis of progressive MS (P-MS, 15 with primary form and 25 with secondary form). As per definition, the expanded disability status scale (EDSS) score was significantly higher in P-MS (6.1 ± 2.1) than in RR-MS (2.9 ± 1.6, p < 0.0001). Within the MS group of patients the age at disease onset was significantly lower in RR-MS compared to P-MS (p = 0.04), but the disease duration was comparable (data not shown).
Table 1.
Demographic, clinical and genetic characteristics of the individuals enrolled in the study
| Healthy controls (HC) | Multiple sclerosis patients (MS) | Relapsing–remitting MS patients (RR-MS) | Progressive MS patients (P-MS) | |
|---|---|---|---|---|
| N | 89 | 117 | 77 | 40 |
| Gender (M:F) | 43:46 | 48:69 | 32:45 | 16:24 |
| Age (years) | 44.8 ± 10.8 | 44.7 ± 12.6 | 42.1 ± 9.5 | 50.8 ± 10.2 |
| EDSS | – | 3.8 ± 2.2 | 2.9 ± 1.6 | 6.1 ± 2.1* |
| HLA-A*02 carriers (%) | 64 | 62 | 66 | 60 |
| HLA-B*07 carriers (%) | 69 | 60 | 61 | 57 |
| HLA-DRB1*15 carriers (%) | 68 | 64 | 63 | 68 |
Data are expressed as mean ± standard deviation
EDSS Expanded Disability Status Scale
* p < 0.0001 vs. RR-MS
EBV seropositivity and viral load
All the 206 individuals included in the study were IgG EBNA-1 and VCA seropositive. The EBNA-1 antibody titer was significantly higher in MS (1009.23; 782.79–1383.37 U/ml) compared to HC (782.55; 627.82–910.95 U/ml; p < 0.0001). This difference remained significant when MS patients were split in RR-MS (p = 0.0008 vs. HC) and in P-MS (p = 0.03 vs. HC). IgG EBNA-1 Ab titers were comparable in RR-MS and P-MS patients (Table 2).
Table 2.
EBV and CMV seroprevalence and antibodies titers in MS patients and controls
| Healthy controls (HC) | Multiple sclerosis patients (MS) | Relapsing–remitting MS patients (RR-MS) | Progressive MS patients (P-MS) | |
|---|---|---|---|---|
| EBV seroprevalence (%) | 100 | 100 | 100 | 100 |
| EBNA-1 IgG (U/ml) | 782.55 (627.82–910.95) | 1009.23* (782.79–1383.37) | 1139.00* (782.70–1452.15) | 937.29** (828.82–1191.21) |
| VCA Ab (U/ml) | 375.54 (144.77–625.19) | 969.07** (511.62–1340.41) | 1146.45** (560.95–1407.95) | 885.15 (277.02–1050.24) |
| CMV seroprevalence (%) | 64.3 | 70.2 | 69.7 | 71.2 |
| CMV IgG (U/ml) | 58.40 (38.15–84.47) | 83.40 (46.33–119.56) | 80.87 (46.78–124.58) | 86.68 (55.04–112.95) |
Data are expressed as medians and (interquartile range)
EBV Epstein-Barr Virus, CMV cytomegalovirus, EBNA1 EBV nuclear antigen 1, VCA viral capsid antigen, IgG immunoglobulin G, VL viral load
* p < 0.0001 vs. HC
** p < 0.05 vs. HC
The VCA antibody titer was significantly higher in MS (969.07; 511.62–1340.41 U/ml) compared to HC (375.54; 144.77–625.19 U/ml; p = 0.02). When MS patients were split in RR-MS and in P-MS, this difference remained significant between RR-MS and HC (p = 0.01), whereas no significant differences were observed between P-MS and HC, and between RR-MS and P-MS (Table 2).
EBV DNA was significantly more frequently detected in MS patients (54/117; 46.1%) compared to HC (25/89; 28.1%) (p = 0.009). Moreover, although the median is the same in MS and HC group (2.0 copies/μg), the overall EBV DNA viral load is significantly increased in MS patients (IQR: 2.00–37.50 copies/μg) than HC (IQR: 2.00–2.36 copies/μg) (p = 0.006) (Fig. 1).
Fig. 1.
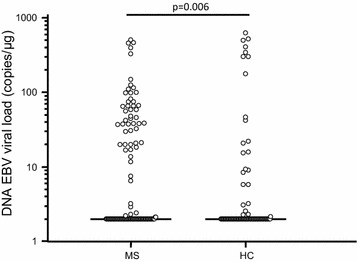
EBV viral load in blood of multiple sclerosis patients and healthy controls
Finally, no differences were detected when either EBV DNA or viral loads were compared between RR-MS (EBV DNA positivity: 48%; EBV viral load: 2.0; 2.0–39.3 copies/μg) and P-MS (EBV DNA positivity: 43%; EBV viral load: 2.0; 2.0–28.9 copies/μg) patients. As previously indicated, all the individuals enrolled in the study were EBV seropositive; some of them, nevertheless, had an undetectable EBV viral load. An arbitrary value < 2 copies/μg (i.e. the limit detection of the assay) was assigned to these samples for the analysis of association with HLA genotyping. No correlation was observed between EBV viral load and EBV or VCA Ab titers, either considering the enrolled subject altogether, either considering the enrolled individuals as a group or splitting them in MS and HC (see Additional file 1: Figure S1).
CMV seropositivity and viral load
The 70.2% of MS and the 64.3% of HC were CMV IgG seropositive. The antibody titer was similar in the two groups (MS: 83.40; 46.33–119.56 U/ml; HC: 58.40; 38.15–84.47 U/ml) (Table 2), and no differences were observed also splitting the patients in RR-MS and P-MS. The CMV viral load was not detectable in blood in all the enrolled subjects but in one healthy control (VL: 65.75 copies/μg).
HLA genotyping and EBV
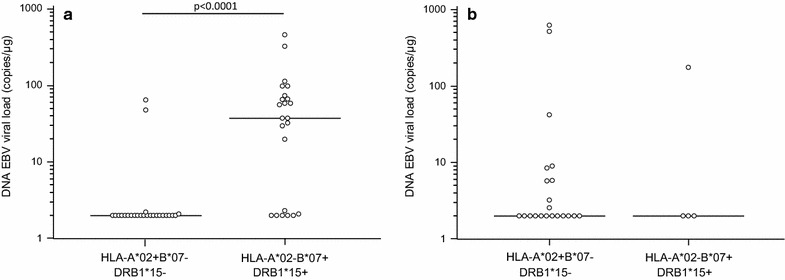
HLA-A, -B, and -DRB1 genotyping was performed in all the enrolled subjects and genetic patterns were evaluated in relationship with EBV parameters. The HLA frequencies are summarized in Table 1. Results showed that a significantly higher EBV viral load could be detected in MS subjects carrying the HLA-B*07 allele (non-protective allele) (HLA-B*07+) (N = 47/117) (37.54; 2.0–74.25 copies/µg) compared to those not carrying this allele (HLA-B*07−) (N = 70/117) (2.0; 2.0–2.0 copies/μg; p < 0.0001) (Fig. 2a). Similarly, MS patients carrying the HLA-DRB1*15 allele (risk allele) (HLA-DRB1*15+) (N = 42/117) had higher EBV viral load (11.7; 2.0–58.3 copies/µg) than those not carrying this allele (HLA-DRB1*15−) (N = 75/117) (2.0; 2.0–21.1 copies/µg) (Fig. 3a) (p = 0.02).
Fig. 2.
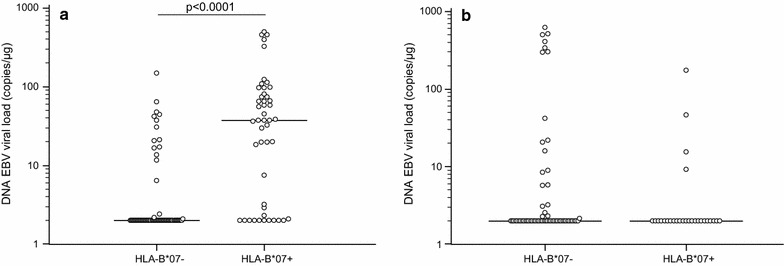
EBV viral load in blood of multiple sclerosis patients (a) and healthy controls (b) carrying HLA-B*07 allele
Fig. 3.
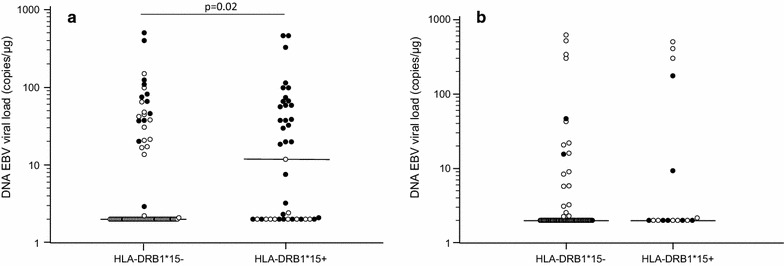
EBV viral load in blood of multiple sclerosis patients (a) and healthy controls (b) carrying HLA-DRB1*15 (c) allele
Conversely, a significantly lower EBV viral load was observed in MS patients expressing the HLA-A*02 antigen (HLA-A*02+) (N = 44/117) (2.0; 2.0–2.1 copies/µg), which is suggested to be a protective factor in MS, compared to those without the allele (HLA-A*02−) (N = 73/117) (2.9; 2.00–37.65 copies/µg; p = 0.01) (Fig. 4a). EBV viral load was next evaluated in MS patients in relationship with the different distribution pattern of HLA-A*02, -B*07 and -DRB1*15 alleles. Results showed that the highest EBV viral load (37.5; 2.1–72.1 copies/µg) was detected in HLA-B*07+/HLA-DRB1*15+/HLA-A*02− (least favorable HLA combination) patients (N = 23); conversely, the 25 HLA-B*07−/HLA-DRB1*15−/HLA-A*A02+ patients were characterized by the lowest EBV viral load (2.0; 2.0–2.0 copies/µg) (p < 0.0001) (Fig. 5a).
Fig. 4.
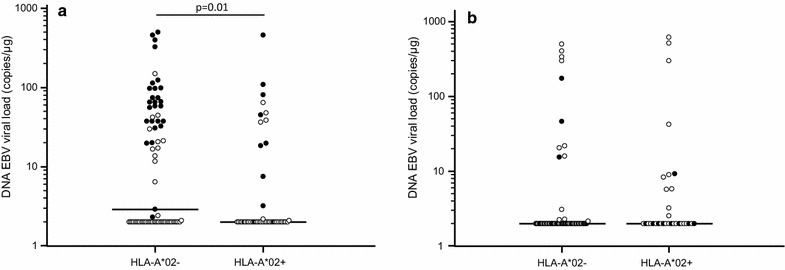
EBV viral load in blood of multiple sclerosis patients (a) and healthy controls (b) carrying HLA-A*02. Black dots represent subjects carrying HLA-B*07 allele
Fig. 5.
EBV viral load in blood of multiple sclerosis patients (a) and of healthy controls (b) in relationship with the co-segregation of HLA-A*02, -B*07 and -DRB1*15 alleles
Moreover, a multiple regression analysis where EBV viral load was computed as dependent variable and HLA-B*07, -A*02 and –DRB1*15 alleles as independent variables, confirmed only the association of HLA-B*07 with high EBV viral load (p = 0.0001). These data suggest that the risk effects of the HLA-B*07 allele are stronger than the “protective” ones attributed to the HLA-A*02 allele and than the “risk” ones attributed to the HLA-DRB1*15 allele. Notably, the relationship between HLA alleles and viral parameters was exclusively seen in MS patient as no such effects could be observed in the 89 HC (Figs. 2, 3, 4 and 5b).
Splitting MS patients between RR-MS and P-MS, results regarding the association between EBV viral load was significantly higher in RR-MS expressing the HLA-B*07 antigen (37.5; 2.1–74.0 copies/µg) than those not carrying this allele (2.0; 2.0–4.7 copies/µg; p < 0.0001). EBV viral load was significantly increased as well in P-MS carrying -B*07 (37.5; 15.6–97.79 copies/µg) compared to P-MS patients who did not carry this allele (2.0; 2.0–2.0 copies/µg; p < 0.0001). Regarding the others alleles, results were confirmed for DRB1*15 in P-MS patients (p = 0.009) (Fig. 6). Notably, comparable EBV viral load characterized RR-MS and P-MS expressing the same HLA molecules.
Fig. 6.
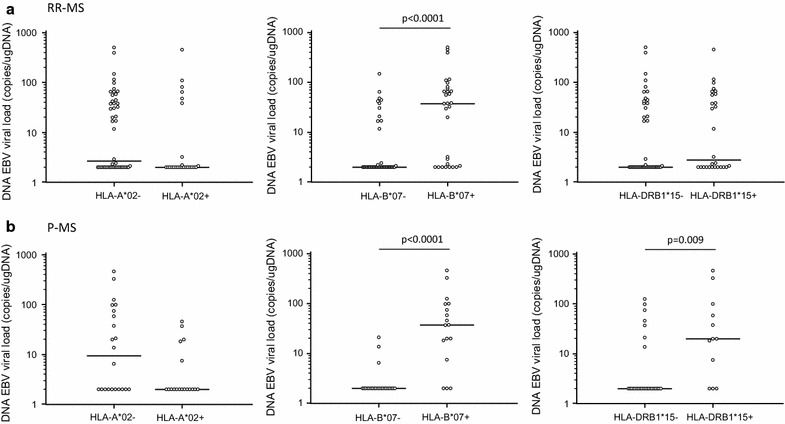
EBV viral load in blood of RR-MS (a) and P-MS (b) carrying HLA-A*02, -B*07 and -DRB1*15 alleles
Finally, no relationships were found between HLA distribution and EBV-specific antibody titers, either considering the enrolled individuals as a group or splitting them in MS and HC.
Discussion
The etiology of MS is still unknown, but it is widely accepted that interactions between environmental and genetic factors shape the susceptibility to this multifactorial disease. Thus, whereas the correlation between certain HLA alleles and disease susceptibility has been definitely established, the possible association between EBV infection and MS has been repeatedly suggested but is still in need of convincing and definitive conclusions.
Herein we initially analyzed EBV infection parameters in a MS study population; our results confirmed previous data indicating that higher anti-EBNA-1 IgG serum titers are present in MS patients compared to HC [8, 26]. We also observed that, in MS patients compared to controls: (1) EBV DNA in blood is more frequently detected, and (2) EBV viral loads are significantly increased, although these viral loads are not comparable to those seen in EBV-associated malignancies [27]. These data confirm previously published results [28, 29], even if not all authors confirm such findings [30, 31], and could be the consequence of increased rates of EBV replication, more frequent reactivations, or of higher frequencies of circulating EBV-infected B lymphocytes [32]. However, it is important to note that, because in our experiments DNA was extracted from whole blood, viral DNA originating from B cells could not be discriminated from that originating from virions.
No relations were observed between EBV-specific antibody titers and EBV viral load in the study population. These results are partially in agreement with recent results indicating that, whereas VCA-specific Ab titers do correlate with EBV viral load, EBNA-1-specific Ab do not [33]; analyses on wider cohorts of individuals will be needed to clarify this aspect.
Having covered the virological side, we next analyzed whether polymorphisms in the HLA region known to modulate MS susceptibility [34] and its progression could associate with virologic parameters. Several lines of evidence indicate the presence of possible interactions between EBV infection-associated parameters, usually EBNA-1 antibody titers, and HLA profiles in MS; these evidences are nevertheless not unequivocal [18–21, 35, 36]. Whereas in our cohort we did not observe any correlations between anti-EBV antibody titers and HLA antigens, possibly because of the small number of individuals analyzed, clear correlations emerged between HLA alleles and EBV viral loads. Thus, results showed that patients carrying the MS risk allele B*07 (HLA-B*07+) in the presence of the risk allele DRB1*15 and in the absence of the protective allele A*02 (HLA-B*07+/DRB1*15+/A*02−) were characterized by the presence of the highest EBV viral loads. These findings were confirmed by the observation that the lowest EBV viral loads were seen in MS patients showing the opposite HLA profile (HLA-B*07−/DRB1*15−/A*02+). The same trend remained when HLA-B*07, DRB1*15 and HLA-A*02 alleles were analyzed singularly. To note, analyzing the effects of HLA alleles altogether by multiple regression analysis, HLA-B*07 allele appears to have the strongest role on EBV DNA viral load. It is noteworthy that HLA-B*07 belongs to the same HLA haplotype carrying the HLA-DRB1*15 allele, whose association with MS susceptibility is well-established. Recently, a role of B*07 in EBV infection in MS patients has been proposed [12]. It is also important to observe that these correlations disappeared when the analyses were performed in healthy controls.
Conclusions
Merging the virologic and the genetic results presented herein allows the speculation that the increased blood viral loads seen in our patients are the consequence of a suboptimal control of EBV replication/reactivation by HLA-B*07+ restricted CD8+ T cell. Notably, HLA-B*07 antigen was recently shown to only weakly present viral epitopes to cytotoxic T lymphocytes [11]. This would allow more frequent EBV lytic replication/reactivation and the infection of an ampler pool of naïve B lymphocytes.
The suboptimal control of EBV replication/reactivation observed in HLA-B*07+ MS subjects may have had an impact on disease severity, but interestingly, no differences in EBV viral load were observed between HLA-B*07+ restricted RR- and P-MS patients. Finally, it could be expected that the frequency and/or the potency of EBV-specific cytotoxic T cell would be different in MS patients expressing (or lacking) the different HLA alleles analyzed in this study. We are currently enrolling patients and controls selected according to their HLA profiles to verify this hypothesis. Interestingly, these results are in line with several analyses performed in other diseases in which the etiologic role of EBV is suspected, or has been definitely confirmed. Thus, the presence of the HLA-A*02 allele was shown to be protective in nasopharyngeal carcinoma and in Hodgkin’s lymphomas [37, 38]. Taken together results herein reinforce the hypothesis that the role of HLA-class I antigens in the pathogenesis of MS could be at least partially mediated by their ability to control EBV infection and persistence.
Additional file
Additional file 1: Figure S1.Correlation between DNA EBV viral load and EBV Ab titers in study population. Correlation between DNA EBV viral load and Ab EBNA-1 titers (A) or Ab VCA titers (B) in study population.
Authors’ contributions
Conceived and designed experiments: SA, RM, FG, MC. Recruited patients and collected clinical data: ML, DC, MR; Performed the virological experiments: SA, AH; Performed genetic experiments: CA, MZ, ND, SD; Performed analysis: SA, RM, FG; Wrote the paper: SA, RM, FG, MC. All authors read and approved the final manuscript.
Acknowledgements
The authors thank all the subjects enrolled in the study; we are particularly grateful to Mrs. Franca Mazzali, Mrs. Raffaella De Pedrina, Mrs. Rosaria Trovato and all the nurses of Multiple Sclerosis Unit and of Day Hospital of IRCCS S. Maria Nascente for taking care of our patients.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
Available under request.
Consent for publication
The participant gave informed consent before taking part in this study.
Ethics approval and consent to participate
Samples use in this study was approved by the ethics committees of Don C. Gnocchi Foundation, IRCCS S. Maria Nascente in Milan, Italy, and of the MS Centers of the PROGEMUS Consortium.
Funding
This work was supported by 2015–2016 Ricerca Corrente (Italian Ministry of Health).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- Ab
antibody
- ANOVA
analysis of variance
- CMV
cytomegalovirus
- CNS
central nervous system
- DNA
deoxyribonucleic acid
- EBNA-1
EBV nuclear antigens
- EBV
Epstein Barr-virus
- EDSS
Expanded Disability Status Scale
- HC
healthy controls
- HHV-4
human herpesvirus 4
- HLA
human leukocyte antigen
- IgG
immunoglobulin G
- IM
infectious mononucleosis
- IQR
interquartile range
- MRI
magnetic resonance imaging
- MS
multiple sclerosis
- P-MS
progressive MS
- RR-MS
relapsing-remitting MS
- SD
standard deviation
- SEM
standard error mean
- VCA
viral capsid antigen
- VL
viral load
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s12967-018-1450-6) contains supplementary material, which is available to authorized users.
Contributor Information
Simone Agostini, Phone: +39 0250330412, Email: sagostini@dongnocchi.it.
Roberta Mancuso, Email: rmancuso@dongnocchi.it.
Franca R. Guerini, Email: fguerini@dongnocchi.it
Sandra D’Alfonso, Email: sandra.dalfonso@med.uniupo.it.
Cristina Agliardi, Email: cagliardi@dongnocchi.it.
Ambra Hernis, Email: ahernis@dongnocchi.it.
Milena Zanzottera, Email: mzanzottera@dongnocchi.it.
Nadia Barizzone, Email: nadia.barizzone@med.uniupo.it.
Maurizio A. Leone, Email: m.leone@operapadrepio.it
Domenico Caputo, Email: dcaputo@dongnocchi.it.
Marco Rovaris, Email: mrovaris@dongnocchi.it.
Mario Clerici, Email: mario.clerici@unimi.it.
References
- 1.Compston A, Coles A. Multiple sclerosis. Lancet. 2008;372:1502–1517. doi: 10.1016/S0140-6736(08)61620-7. [DOI] [PubMed] [Google Scholar]
- 2.GAMES; Transatlantic multiple sclerosis genetics cooperative A meta-analysis of whole genome linkage screens in multiple sclerosis. J Neuroimmunol. 2003;143:39–46. doi: 10.1016/j.jneuroim.2003.08.009. [DOI] [PubMed] [Google Scholar]
- 3.Jersild C, Svejgaard A, Fog T. HL-A antigens and multiple sclerosis. Lancet. 1972;1:1240–1241. doi: 10.1016/S0140-6736(72)90962-2. [DOI] [PubMed] [Google Scholar]
- 4.Nolan D, Castley M, Tschochner M, James I, Qiu W, Sayer D, et al. Contributions of vitamin D response elements and HLA promoters to multiple sclerosis risk. Neurology. 2012;79:538–546. doi: 10.1212/WNL.0b013e318263c407. [DOI] [PubMed] [Google Scholar]
- 5.Zivadinov R, Uxa L, Zacchi T, Nasuelli D, Ukmar M, Furlan C, et al. HLA genotypes and disease severity assessed by magnetic resonance imaging findings in patients with multiple sclerosis. J Neurol. 2003;250:1099–1106. doi: 10.1007/s00415-003-0164-7. [DOI] [PubMed] [Google Scholar]
- 6.Moutsianas L, Jostins L, Beecham AH, Dilthey AT, Xifar DK, Ban M, et al. Class II HLA interactions modulate genetic risk for multiple sclerosis. Nat Genet. 2015;47:1107–1113. doi: 10.1038/ng.3395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brynedal B, Duvefelt K, Jonasdottir G, Roos IM, Akesson E, Palmgren J, et al. HLA-A confers an HLA-DRB1 independent influence on the risk of multiple sclerosis. PLoS ONE. 2007;2:e664. doi: 10.1371/journal.pone.0000664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ascherio A, Munger KL. Environmental risk factors for multiple sclerosis. Part I: the role of infection. Ann Neurol. 2007;61:288–299. doi: 10.1002/ana.21117. [DOI] [PubMed] [Google Scholar]
- 9.Young LS, Rickinson AB. Epstein-Barr virus: 40 years on. Nat Rev Cancer. 2004;4:757–768. doi: 10.1038/nrc1452. [DOI] [PubMed] [Google Scholar]
- 10.Serafini B, Severa M, Columba-Cabezas S, Rosicarelli B, Veroni C, Chiappetta C, et al. Epstein-Barr virus latent infection and BAFF expression in B cells in the multiple sclerosis brain: implications for viral persistence and intrathecal B-cell activation. J Neuropathol Exp Neurol. 2010;69:677–693. doi: 10.1097/NEN.0b013e3181e332ec. [DOI] [PubMed] [Google Scholar]
- 11.Hollsberg P, Hansen HJ, Haahr S. Altered CD8+ T cell responses to selected Epstein-Barr virus immunodominant epitopes in patients with multiple sclerosis. Clin Exp Immunol. 2003;132:137–143. doi: 10.1046/j.1365-2249.2003.02114.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jilek S, Schluep M, Harari A, Canales M, Lysandropoulos A, Zekeridou A, et al. HLA-B7-restricted EBV-specific CD8+ T cells are dysregulated in multiple sclerosis. J Immunol. 2012;188:4671–4680. doi: 10.4049/jimmunol.1103100. [DOI] [PubMed] [Google Scholar]
- 13.Lassmann H, Niedobitek G, Aloisi F, Middeldorp JM, NeuroproMiSe EBV Working Group Epstein-Barr virus in the multiple sclerosis brain: a controversial issue-report on a focused workshop held in the Centre for Brain Research of the Medical University of Vienna, Austria. Brain. 2011;134:2772–2786. doi: 10.1093/brain/awr197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Serafini B, Rosicarelli B, Franciotta D, Magliozzi R, Reynolds R, Cinque P, et al. Dysregulated Epstein-Barr virus infection in the multiple sclerosis brain. J Exp Med. 2007;204:2899–2912. doi: 10.1084/jem.20071030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alvarez-Lafuente R, Garcia-Montojo M, De Las Heras V, Dominguez-Mozo MI, Bartolome M, Benito-Martin MS, et al. Herpesviruses and human endogenous retroviral sequences in the cerebrospinal fluid of multiple sclerosis patients. Mult Scler. 2008;14:595–601. doi: 10.1177/1352458507086425. [DOI] [PubMed] [Google Scholar]
- 16.Willis SN, Stadelmann C, Rodig SJ, Caron T, Gattenloehner S, Mallozzi SS, et al. Epstein-Barr virus infection is not a characteristic feature of multiple sclerosis brain. Brain. 2009;132:3318–3328. doi: 10.1093/brain/awp200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sargsyan SA, Shearer AJ, Ritchie AM, Burgoon MP, Anderson S, Hemmer B, et al. Absence of Epstein-Barr virus in the brain and CSF of patients with multiple sclerosis. Neurology. 2010;74:1127–1135. doi: 10.1212/WNL.0b013e3181d865a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xiao D, Ye X, Zhang N, Ou M, Guo C, Zhang B, et al. A meta-analysis of interaction between Epstein-Barr virus and HLA-DRB1*1501 on risk of multiple sclerosis. Sci Rep. 2015;5:18083. doi: 10.1038/srep18083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.De Jager PL, Simon KC, Munger KL, Rioux JD, Hafler DA, Ascherio A. Integrating risk factors: HLA-DRB1*1501 and Epstein-Barr virus in multiple sclerosis. Neurology. 2008;70:1113–1118. doi: 10.1212/01.wnl.0000294325.63006.f8. [DOI] [PubMed] [Google Scholar]
- 20.Sundqvist E, Sundstrom P, Linden M, Hedstrom AK, Aloisi F, Hillert J, et al. Epstein-Barr virus and multiple sclerosis: interaction with HLA. Genes Immun. 2012;13:14–20. doi: 10.1038/gene.2011.42. [DOI] [PubMed] [Google Scholar]
- 21.Zivadinov R, Weinstock-Guttman B, Zorzon M, Uxa L, Serafin M, Bosco A, et al. Gene-environment interactions between HLA B7/A2, EBV antibodies are associated with MRI injury in multiple sclerosis. J Neuroimmunol. 2009;209:123–130. doi: 10.1016/j.jneuroim.2009.01.023. [DOI] [PubMed] [Google Scholar]
- 22.Polman CH, Reingold SC, Banwell B, Clanet M, Cohen JA, Filippi M, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011;69:292–302. doi: 10.1002/ana.22366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agliardi C, Guerini FR, Saresella M, Caputo D, Leone MA, Zanzottera M, et al. Vitamin D receptor (VDR) gene SNPs influence VDR expression and modulate protection from multiple sclerosis in HLA-DRB1*15-positive individuals. Brain Behav Immun. 2011;25:1460–1467. doi: 10.1016/j.bbi.2011.05.015. [DOI] [PubMed] [Google Scholar]
- 24.Barizzone N, Zara I, Sorosina M, Lupoli S, Porcu E, Pitzalis M, et al. The burden of multiple sclerosis variants in continental Italians and Sardinians. Mult Scler J. 2015;21:1385–1395. doi: 10.1177/1352458515596599. [DOI] [PubMed] [Google Scholar]
- 25.Mancuso R, Hernis A, Cavarretta R, Caputo D, Calabrese E, Nemni R, et al. Detection of vital DNA sequence in the cerebrospinal fluid of patients with multiple sclerosis. J Med Virol. 2010;82:1051–1057. doi: 10.1002/jmv.21764. [DOI] [PubMed] [Google Scholar]
- 26.Farrell RA, Antony D, Wall GR, Clark DA, Fisniku L, Swanton J, et al. Humoral immune response to EBV in multiple sclerosis is associated with disease activity on MRI. Neurology. 2009;73:32–38. doi: 10.1212/WNL.0b013e3181aa29fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hohaus S, Santnagelo R, Giachelia M, Massini G, Cuccaro A, Martini M, et al. The viral load of Epstein-Barr virus (EBV) DNA in peripheral blood predicts for biological and clinical characteristics in Hodgkin lymphoma. Clin Cancer Res. 2011;17:2885–2892. doi: 10.1158/1078-0432.CCR-10-3327. [DOI] [PubMed] [Google Scholar]
- 28.Ben Fredj N, Rotola A, Nefz F, Chebei S, Rizzo R, Caselli E, et al. Identification of human herpesviruses 1–8 in Tunisian multiple sclerosis patients and healthy blood donors. J Neurovirol. 2012;18:12–19. doi: 10.1007/s13365-011-0056-z. [DOI] [PubMed] [Google Scholar]
- 29.Lucas RM, Taylor BV. Epstein-Barr virus infection: a smoking gun for multiple sclerosis? Neurology. 2012;79:1310–1311. doi: 10.1212/WNL.0b013e31826c1baf. [DOI] [PubMed] [Google Scholar]
- 30.Lindsey JW, Hatfield LM, Crawford MP, Patel S. Quantitative PCR for Epstein-Barr virus DNA and RNA in multiple sclerosis. Mult Scler. 2009;15:153–158. doi: 10.1177/1352458508097920. [DOI] [PubMed] [Google Scholar]
- 31.Cocuzza CE, Piazza F, Musumeci R, Oggioni D, Andreoni S, Gardinetti M, et al. Quantitative detection of Epstein-Barr virus DNA in cerebrospinal fluid and blood samples of patients with relapsing-remitting multiple sclerosis. PLoS ONE. 2014;9:e94497. doi: 10.1371/journal.pone.0094497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maurmann S, Fricke L, Wagner HJ, Schlenke P, Hennig H, Steinhoff J, et al. Molecular parameters for precise diagnosis of asymptomatic Epstein-Barr virus reactivation in healthy carriers. J Clin Microbiol. 2003;41:5419–5428. doi: 10.1128/JCM.41.12.5419-5428.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pender MP, Csurhes PA, Burrows JM, Burrows SR. Defective T-cell control of Epstein-Barr virus infection in multiple sclerosis. Clin Transl Immunology. 2017;6:e126. doi: 10.1038/cti.2016.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.International Multiple Sclerosis Genetics C. Wellcome Trust Case Control C. Sawcer S, Hellenthal G, Pirinen M, Spencer CC, et al. Genetic risk and a primary role for cell-mediated immune mechanisms in multiple sclerosis. Nature. 2011;476:214–219. doi: 10.1038/nature10251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nielsen TR, Rostgaard K, Askling J, Steffensen R, Oturai A, Jersild C, et al. Effects of infectious mononucleosis and HLA-DRB1*15 in multiple sclerosis. Mult Scler. 2009;15:431–436. doi: 10.1177/1352458508100037. [DOI] [PubMed] [Google Scholar]
- 36.Sundstrom P, Nystrom L, Jidell E, Hallmans G. EBNA-1 reactivity and HLA DRB1*1501 as statistically independent risk factors for multiple sclerosis: a case-control study. Mult Scler. 2008;14:1120–1122. doi: 10.1177/1352458508092353. [DOI] [PubMed] [Google Scholar]
- 37.Hjalgrim H, Rostgaard K, Johnson PC, Lake A, Shield L, Little AM, et al. HLA-A alleles and infectious mononucleosis suggest a critical role for cytotoxic T-cell response in EBV-related Hodgkin lymphoma. Proc Natl Acad Sci USA. 2010;107:6400–6405. doi: 10.1073/pnas.0915054107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huang X, Kushekhar K, Nolte I, Kooistra W, Visser L, Bouwman I, et al. HLA associations in classical Hodgkin lymphoma: EBV status matters. PLoS ONE. 2012;7:e39986. doi: 10.1371/journal.pone.0039986. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Figure S1.Correlation between DNA EBV viral load and EBV Ab titers in study population. Correlation between DNA EBV viral load and Ab EBNA-1 titers (A) or Ab VCA titers (B) in study population.
Data Availability Statement
Available under request.


