Due to the prevalence of low-dose computed tomography (LDCT) screening, the detection rate of lung cancer presenting as multiple ground-glass opacities (GGOs) is increasing. In statements from the Fleischner Society and the International Association for the Study of Lung Cancer (IASLC) Staging and Prognostic Factors Committee, GGOs are considered as multiple primary lung cancers and at the early stage of tumorigenesis.1 2 Accumulating evidence supports the notion that metastasis in human cancer can occur at an early stage of disease progression. Whether multiple GGOs may represent intrapulmonary metastases remains unclear. In two patients with multiple GGOs, we found that two of the multiple GGOs in each patient shared somatic mutations based on exome sequencing, indicative of intrapulmonary metastasis. This finding, for the first time to our knowledge, shows that metastasis can occur among GGOs, even pure GGOs.
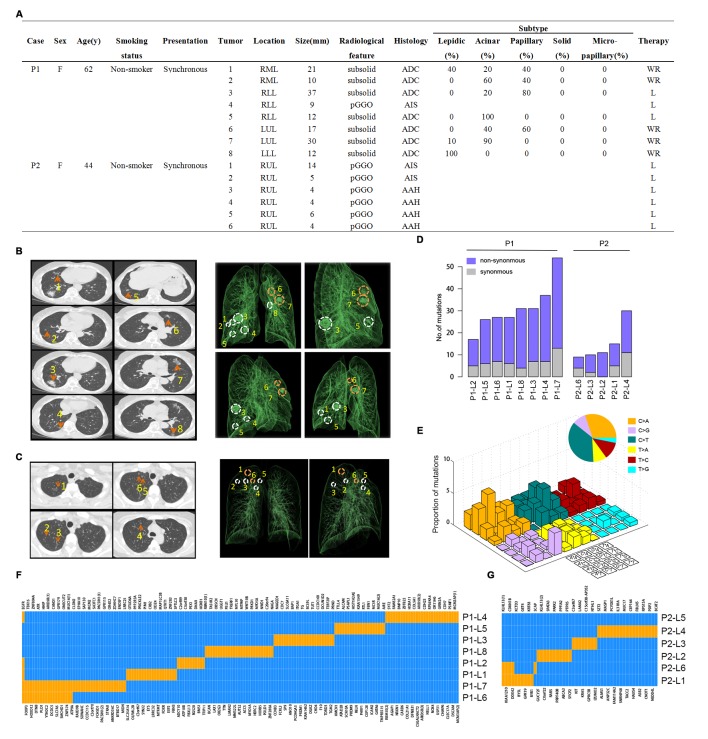
The two patients (P1 and P2) were both non-smokers. Detailed clinicopathological characteristics are summarised in (figure 1A). P1 was a 62-year-old woman who presented with nine GGOs including two in the right middle lobe (RML), three in the right lower lobe (RLL), three in the left upper lobe (LUL) and one in the left lower lobe (LLL) (figure 1B). She underwent RLL lobectomy and RML wedge resection in January 2015. The five resected nodules were all diagnosed as lung adenocarcinomas. Four months later she underwent LUL and LLL wedge resections. Three of the four resected nodules were diagnosed as lung adenocarcinomas. All eight malignant lesions were pathological T1–T2 tumours without lymphovascular invasion (online supplementary figure 1). No lymph node metastasis was detected. P2 was a 44-year-old woman who presented with eight GGOs including six in the right upper lobe (RUL) and two in the LUL (figure 1C). Radiologically, all of the eight lesions were pure GGOs <15 mm (range 4–14 mm). She only underwent RUL lobectomy and six nodules were removed. All six lesions were adenocarcinoma in situ or atypical adenomatous hyperplasia (online supplementary figure 2).
Figure 1.
Radiological features and whole-exome sequencing of the two patients. (A) Clinicopathological characteristics. RML, right middle lobe; RLL, right lower lobe; LUL, left upper lobe; LLL, left lower lobe; RUL, right upper lobe; pGGO, pure ground-glass opacities; ADC, adenocarcinoma; AIS, adenocarcinoma in situ; AAH, atypical adenomatous hyperplasia; WR, wedge resection; L, lobectomy; (B) Left: chest CT scans obtained with 1 mm thick sections of patient 1 (P1) with eight scattered GGOs (orange arrows) in the bilateral lung. Right: reconstructed lung 3D images of P1. Circles denote the spatial locations of the lesions and orange circles indicate metastatic lesions. (C) Left: CT scans obtained with 1 mm thick sections of patient 2 (P2) with six scattered GGOs (orange arrows) in her right upper lobe. All six lesions are pure GGOs of very small size. Right: reconstructed 3D images of P2. Circles denote the spatial locations of the lesions and orange circles indicate metastatic lesions. (D) Number of somatic mutations identified in each lesion of the two patients. Lesion name is in form of ‘Patient ID + lesion number’. For example, P1-L1 stands for the number 1 lesion of patient 1. (E) Mutational signature of P1 based on all somatic mutations detected in this patient. (F) Regional distribution of non-synonymous somatic mutations among the eight lesions of P1. Each column represents a single mutation site. Blue represents wild type while orange represents mutation in a certain site of a certain gene. (G) Regional distribution of somatic mutations among the six lesions of P2. Each column represents a single mutation site. Blue represents wild type while orange represents mutation in a certain site of a certain gene.
thoraxjnl-2017-210169supp001.pdf (558KB, pdf)
We performed exome sequencing of 14 tumour samples (eight from P1 and six from P2) and matched blood samples as germline comparators. On average, we obtained 68x exome coverage depth (online supplementary table 1) and found a total of 172 and 49 non-synonymous mutations in P1 and P2, respectively (48 and 20 synonymous mutations, respectively) (online supplementary table 2). The mutation number of each lesion ranged from 9 to 54 (no somatic mutation was detected in P2-L5) (figure 1D). Among the non-synonymous mutations detected in P1, putative driver mutations in cancer-associated genes like EGFR, BAP1, RBM10 and ARID5B were identified. Further, we found that the C to A transversion and C to T transition were predominant among the six substitution subtypes. The prevalent C to A transversion exhibited notable transcriptional strand bias (figure 1E), which is potentially associated with tobacco exposure. In P2 we found that the average mutational number of the lesions was lower than in P1, probably because GGOs in P2 were at an earlier stage of disease progression.
We then investigated the regional distribution of somatic mutations in each case. In P1 we found that five lesions shared a single mutation in EGFR (p.L858R) (figure 1F). Given that this mutation has been widely recognised as a recurrent mutation in lung adenocarcinoma, we considered it as the result of convergent evolution rather than inheritance from a common ancestor. Unexpectedly, lesions P1-L6 and P1-L7, which displayed different major histological subtypes (P1-L6, 40% acinar + 60% papillary; P1-L7, 10% lepidic + 90% acinar) and therefore tend to be considered as separate primaries from the view of histological assessment, shared nineteen non-synonymous and seven synonymous mutations, excluding the EGFR p.L858R variant (online supplementary figure 3). Almost all the shared mutations occurred in rarely reported genes, which could hardly be explained as the results of convergent evolution. Taken together, these findings indicate that the two GGOs of P1, both located in the lingular segment of LUL (figure 1B), originated from a common ancestor. Regarding the formation of P1-L6 and P1-L7, in order to distinguish field cancerisation from intrapulmonary metastasis, we performed exome sequencing on a neighbouring normal lung tissue (P1-NT) between these two GGOs. As a result, we did not find any signs of field cancerisation since no somatic mutation was detected in P1-NT. More surprisingly, a similar circumstance was observed in P2. Lesions P2-L1 and P2-L6 were radiologically judged as pure GGOs and both were located in the apical segment of RUL. We unexpectedly found that the two lesions shared four non-synonymous and four synonymous mutations (figure 1G and online supplementary figure 3). Meanwhile, no somatic mutation was found in the neighbouring normal tissue (P2-NT). Taken together, our observations indicate that intrapulmonary metastasis occurred among GGOs.
On the other hand, in P1 six out of eight lesions had no shared mutation excluding the EGFR (p.L858R) mutation (figure 1F). Therefore these six GGOs, as expected, were from independent clonal origins. Taken together, the eight lesions in P1 showed that multicentric tumours and intrapulmonary metastatic lesions co-existed in the same patient. A similar scenario was seen in P2 (figure 1G). The co-existence of multicentric tumours and metastatic lesions in the same patient, especially at the early stage of disease, may challenge the treatment decision and prognostic evaluation of certain patients.
In the current study, we investigated the clonal relationship of multiple GGOs from two patients based on exome sequencing data. We found a relatively low mutational burden in GGOs compared with the results of TCGA lung adenocarcinoma sequencing study. This may reflect the fact that GGOs are at an early stage of carcinogenesis. However, we cannot rule out the possibility that a low mutational burden may be due to insufficient tumour purity and exome coverage. Regarding the enrichment of C to A transversions in P1, it is closely associated with tobacco smoking. Although P1 was described as a non-smoker, we speculate she was suffering from secondhand smoking. The prevalence of C to T transition is possibly caused by formalin embedding. Meanwhile, we identified an EGFR (p.L858R) mutation in this patient, which seems to contradict the fact of tobacco exposure. However, it has been reported that, among patients with EGFR mutations in the white population, about 40% are former or current smokers.3 On the other hand, in Asian patients with a smoking history of >50 pack-years, the EGFR mutation rate is 31.4%.4 Therefore, smoking history or secondhand smoking history is not exclusive to EGFR mutation.
In the recently published consensus of the Fleischner Society and IASLC Staging and Prognostic Factors Committee, multiple GGOs are described as multiple primary lung cancers and usually at a very early stage. Nevertheless, studies regarding the clonal relationship of multifocal lung cancer have seldom focused on GGOs. Based on the shared mutations, especially those occurring in rarely reported genes, we identified lesions with a common clonal origin in two cases and provided genetic evidence supporting early intrapulmonary metastasis among GGOs for the first time.
With the emergence of the concept of tumour spread through air spaces, a new metastasis model of lung cancer has been gradually accepted.5 6 Accumulative evidence from clinical, radiological and pathological observations supports the possibility of aerogenic metastasis in lung cancer. In our study, two GGOs from each patient were considered as metastatic lesions. These lesions may stem from aerogenic metastasis, since no evidence of lymphovascular invasion was observed in either patient. If multiple GGOs can metastasize through aerogenous spread, it may have implications for tumour staging and management. For patients with metastatic GGOs, wedge resection may not be enough and segmentectomy or lobectomy may be more suitable.
Whether metastasis among GGOs influences the prognosis remains to be explored. In clinical practice, patients with GGOs are usually associated with a good prognosis. However, there are also exceptions and a few patients with GGOs have a poor prognosis. In a prospective trial of limited resection of GGOs <2 cm with adequate margins, about 15% of patients experienced a late recurrence near the surgical margin within the 10-year follow-up period.7 Whether this situation is associated with the fact that metastasis exists among GGOs warrants further investigation.
Due to limitations such as moderate exome coverage in the current study, the conclusions that can be made are limited. For example, we cannot rule out the possibility that these clonally unrelated GGOs may be identified as clonally related under a higher exome coverage depth. However, we believe the observation that clonally related GGOs exist is of significant interest to the community.
Acknowledgments
We thank all the patients for their participation in this study. We thank Yiqing Du at Peking University People’s Hospital, Zhanghua Chen and Zhe Su at Biodynamic Optical Imaging Center (BIOPIC) for useful discussion.
Footnotes
RL, XL, RX and FY contributed equally.
Contributors: RL: prepared manuscript and performed bioinformatic analysis. XL and FY: prepared manuscript and collected samples. RX, YL and WW: performed experiments. SW: collected samples. DS and KS: pathological assessment. KC: prepared manuscript and figures. FB and JW: designed the project.
Funding: This work was supported by the National High Technology Research and Development Program of China (863 Program, 2015AA020403), the National Key Research and Development Program(2016YFC0900100), the Beijing Municipal Science & Technology Commission (No. Z141100000214013) and the Recruitment Program of Global Youth Experts (to FB).
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: This study was approved by the institutional review board (IRB) of both Peking University People’s Hospital and Peking University.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Sequence data have been deposited in the NCBI Sequence Read Archive under accession number SRP080783
References
- 1. Naidich DP, Bankier AA, MacMahon H, et al. . Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the fleischner society. Radiology 2013;266:304–17. 10.1148/radiol.12120628 [DOI] [PubMed] [Google Scholar]
- 2. Detterbeck FC, Marom EM, Arenberg DA, et al. . The IASLC lung cancer staging project: background data and proposals for the application of TNM staging rules to lung cancer presenting as multiple nodules with ground glass or lepidic features or a pneumonic type of involvement in the forthcoming eighth edition of the TNM classification. J Thorac Oncol 2016;11:666–80. 10.1016/j.jtho.2015.12.113 [DOI] [PubMed] [Google Scholar]
- 3. D’Angelo SP, Pietanza MC, Johnson ML, et al. . Incidence of EGFR exon 19 deletions and L858R in tumor specimens from men and cigarette smokers with lung adenocarcinomas. J Clin Oncol 2011;29:2066–70. 10.1200/JCO.2010.32.6181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shi Y, Au JS, Thongprasert S, et al. . A prospective, molecular epidemiology study of EGFR mutations in Asian patients with advanced non-small-cell lung cancer of adenocarcinoma histology (PIONEER). J Thorac Oncol 2014;9:154–62. 10.1097/JTO.0000000000000033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kadota K, Nitadori J, Sima CS, et al. . Tumor spread through air spaces is an important pattern of invasion and impacts the frequency and location of recurrences after limited resection for small stage I lung adenocarcinomas. J Thorac Oncol 2015;10:806–14. 10.1097/JTO.0000000000000486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gaikwad A, Souza CA, Inacio JR, et al. . Aerogenous metastases: a potential game changer in the diagnosis and management of primary lung adenocarcinoma. AJR Am J Roentgenol 2014;203:W570–82. 10.2214/AJR.13.12088 [DOI] [PubMed] [Google Scholar]
- 7. Nakao M, Yoshida J, Goto K, et al. . Long-term outcomes of 50 cases of limited-resection trial for pulmonary ground-glass opacity nodules. J Thorac Oncol 2012;7:1563–6. 10.1097/JTO.0b013e3182641b5c [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
thoraxjnl-2017-210169supp001.pdf (558KB, pdf)