Abstract
Background
Cardiovascular (CV) outcome trials in type 2 diabetes (T2D) have underrepresented patients with chronic kidney disease (CKD), leading to uncertainty regarding their kidney efficacy and safety. The CARMELINA® trial aims to evaluate the effects of linagliptin, a DPP-4 inhibitor, on both CV and kidney outcomes in a study population enriched for cardio-renal risk.
Methods
CARMELINA® is a randomized, double-blind, placebo-controlled clinical trial conducted in 27 countries in T2D patients at high risk of CV and/or kidney events. Participants with evidence of CKD with or without CV disease and HbA1c 6.5–10.0% (48–86 mmol/mol) were randomized 1:1 to receive linagliptin once daily or matching placebo, added to standard of care adjusted according to local guidelines. The primary outcome is time to first occurrence of CV death, non-fatal myocardial infarction, or non-fatal stroke. The key secondary outcome is a composite of time to first sustained occurrence of end-stage kidney disease, ≥ 40% decrease in estimated glomerular filtration rate (eGFR) from baseline, or renal death. CV and kidney events are prospectively adjudicated by independent, blinded clinical event committees. CARMELINA® was designed to continue until at least 611 participants had confirmed primary outcome events. Assuming a hazard ratio of 1.0, this provides 90% power to demonstrate non-inferiority of linagliptin versus placebo within the pre-specified non-inferiority margin of 1.3 at a one-sided α-level of 2.5%. If non-inferiority of linagliptin for the primary outcome is demonstrated, then its superiority for both the primary outcome and the key secondary outcome will be investigated with a sequentially rejective multiple test procedure.
Results
Between July 2013 and August 2016, 6980 patients were randomized and took ≥ 1 dose of study drug (40.6, 33.1, 16.9, and 9.4% from Europe, South America, North America, and Asia, respectively). At baseline, mean ± SD age was 65.8 ± 9.1 years, HbA1c 7.9 ± 1.0%, BMI 31.3 ± 5.3 kg/m2, and eGFR 55 ± 25 mL/min/1.73 m2. A total of 5148 patients (73.8%) had prevalent kidney disease (defined as eGFR < 60 mL/min/1.73 m2 or macroalbuminuria [albumin-to-creatinine ratio > 300 mg/g]) and 3990 patients (57.2%) had established CV disease with increased albuminuria; these characteristics were not mutually exclusive. Microalbuminuria (n = 2896 [41.5%]) and macroalbuminuria (n = 2691 [38.6%]) were common.
Conclusions
CARMELINA® will add important information regarding the CV and kidney disease clinical profile of linagliptin by including an understudied, vulnerable cohort of patients with T2D at highest cardio-renal risk.
Trial registration ClinicalTrials.gov identifier—NCT01897532; registered July 9, 2013
Electronic supplementary material
The online version of this article (10.1186/s12933-018-0682-3) contains supplementary material, which is available to authorized users.
Keywords: Diabetes mellitus, type 2; Cardiovascular diseases; Diabetic nephropathies; Dipeptidyl-peptidase IV inhibitors; Linagliptin; Clinical trial, phase IV; Research design; Treatment outcome
Background
People with type 2 diabetes (T2D) are at increased risk for both cardiovascular (CV) disease and microvascular complications such as chronic kidney disease (CKD) and kidney failure. In 2008, concerns about adverse CV events associated with the peroxisome proliferator-activated receptor agonists rosiglitazone [1] and muraglitazar [2] were among the issues that led the US Food and Drug Administration (FDA) and European Medicines Agency (EMA) to mandate that novel glucose-lowering drugs for treatment of T2D demonstrate CV safety [3–5]. The CV outcome trials conducted in response to this guidance over the past decade have consequently focused on T2D patients at high risk for CV complications [6–16]. In contrast, evaluation of novel glucose-lowering drugs in individuals at high risk of adverse kidney outcomes has been sparse and relatively neglected.
Approximately 50% of patients with T2D globally also have some evidence of CKD [17], which is associated with significantly increased risk of progression to end-stage kidney disease (ESKD) and premature mortality (Fig. 1). CKD is also one of the strongest risk factors for CV events [18]. A 2016 summit convened by the International Society of Nephrology concluded that a concerted effort is required to increase the quantity and quality of clinical trials investigating CKD [19]; however, there are notable challenges involved in conducting such studies [20]. The paucity of clinical trials specifically designed to evaluate kidney-related efficacy and safety outcomes with glucose-lowering drugs represents an important gap in knowledge to support informed treatment decision-making in patients with T2D at high risk for kidney complications.
Fig. 1.
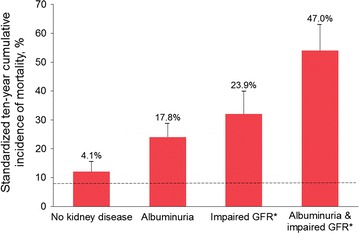
10-year mortality in T2D by kidney disease manifestation in the United States. The dashed line indicates mortality in persons without diabetes or kidney disease (the reference group, 7.7%). The numbers above bars indicate excess mortality above the reference group. Error bars indicate upper limits of the 95% confidence intervals. Republished with permission of the American Society of Nephrology from Afkarian et al. [21]; permission conveyed through Copyright Clearance Center, Inc. *Impaired GFR was defined as GFR ≤ 60 mL/min/1.73 m2. GFR glomerular filtration rate, T2D type 2 diabetes
Dipeptidyl peptidase-4 (DPP-4) inhibitors are now established as oral glucose-lowering drugs with little intrinsic risk of causing hypoglycemia or weight gain [22]. The DPP-4 inhibitors evaluated to date in CV outcomes studies (saxagliptin, alogliptin, sitagliptin) have demonstrated CV safety with regard to atherosclerotic CV disease outcomes, with neutral effects on major adverse CV events compared with placebo [6–8]. However, the incidence of hospitalization for heart failure was statistically increased in the SAVOR-TIMI 53 trial of saxagliptin versus placebo [6] and numerically increased in the EXAMINE trial of alogliptin versus placebo [23]; whereas no effect on the incidence of heart failure hospitalization was observed in the TECOS trial of sitagliptin versus placebo [24]. These observations have prompted FDA product label warnings in the US for all members of the DPP-4 inhibitor class.
Linagliptin is a DPP-4 inhibitor that is excreted predominantly by non-renal pathways, unlike most other members of this drug class, and thus can be prescribed to patients with T2D at a single dose irrespective of kidney function [25, 26]. In pooled analyses of clinical trials designed to evaluate glycemic efficacy and tolerability over the short term (typically 12–24 weeks), linagliptin was not associated with an increase in either CV [27] or kidney risk [28] in patients with T2D, but was associated with a significant reduction in clinically relevant kidney disease endpoints [28].
The CV and kidney clinical profile of linagliptin is being comprehensively evaluated in the CArdiovascular safety and Renal Microvascular outcomE study with LINAgliptin (CARMELINA®) trial. Uniquely among the outcomes studies of glucose-lowering drugs initiated to date, the CARMELINA® trial was designed to recruit patients with T2D at high risk of both CV and kidney complications who had evidence of compromised kidney function with or without CV disease. We report here the study design and methods of CARMELINA® alongside the pooled baseline clinical characteristics of the patients in this trial.
Methods
Study design
The CARMELINA® study is a multi-national, randomized, double-blind, placebo-controlled clinical trial conducted in 27 countries (ClinicalTrials.gov identifier: NCT01897532) (Fig. 2). CARMELINA® is an event-driven trial designed to assess the impact of linagliptin versus placebo on CV and kidney outcomes in a population of patients with T2D enriched for both macrovascular and kidney microvascular risk. The study is designed to run until at least 611 participants have had an adjudicated primary-outcome event. The study protocol was approved by institutional review boards, independent ethics committees and competent authorities according to national and international regulations. CARMELINA® was conducted in accordance with the ICH Harmonised Tripartite Guideline for Good Clinical Practice. All participants provided written informed consent prior to entering the study.
Fig. 2.
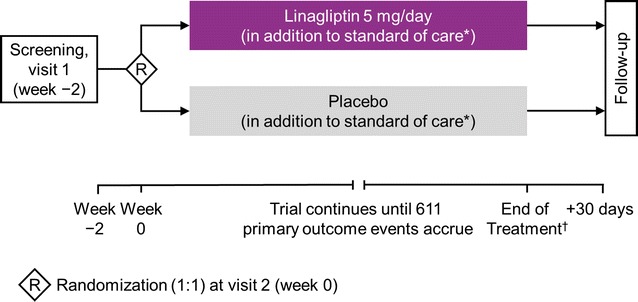
Design of the CARMELINA® trial. *Additional glucose-lowering therapy may be given on top of study medication if HbA1c > 7.5%; investigators are encouraged to treat all other CV risk factors in accordance with local or regional standards of care. †Participants who stop study drug early are observed until study end (not just until 30 days after the end of treatment with study drug). CV cardiovascular, HbA1c glycated hemoglobin A1c
Participants
Patients with T2D aged ≥ 18 years with glycated hemoglobin A1c (HbA1c) 6.5–10.0% (48–86 mmol/mol) and body-mass index (BMI) ≤ 45 kg/m2 were eligible for inclusion. Participants had to be at high risk of vascular events based on established history of CV disease, and/or the presence of markers of CKD (Table 1). Participants could be either drug-naïve or receiving any glucose-lowering therapy except glucagon-like peptide (GLP)-1 receptor agonists, DPP-4 inhibitors and/or sodium-glucose co-transporter 2 (SGLT2) inhibitors. Those individuals already receiving glucose-lowering therapy had to be on the same dose for at least 8 weeks prior to randomization.
Table 1.
CARMELINA® inclusion criteria
| High risk of vascular events (I and/or II) | ||
| I. | Albuminuria (UACR ≥ 30 mg/g or ≥ 30 μg albumin/min or ≥ 30 mg albumin/24 h in two out of three unrelated spot urine or timed samples in the 24 months prior to randomization) and previous macrovascular disease, defined as one or more of the following | |
| (a) | Confirmed history of myocardial infarction (> 2 months prior to screening) | |
| (b) | Advanced coronary artery disease, defined by any one of the following | |
| ≥ 50% narrowing of the luminal diameter in 2 or more major coronary arteries (left anterior descending, circumflex, right coronary artery) by coronary angiography, MRI angiography or CT angiography | ||
| Left main stem coronary artery with ≥ 50% narrowing of the luminal diameter by coronary angiography, MRI angiography or CT angiography | ||
| Prior percutaneous or surgical revascularization of ≥ 2 major coronary arteries ≥ 2 months prior to screening | ||
| The combination of prior percutaneous or surgical revascularization of 1 major coronary artery ≥ 2 months prior to screening, and ≥ 50% narrowing of the luminal diameter by coronary angiography, MRI angiography or CT angiography of at least 1 additional major coronary artery | ||
| (c) | High-risk single-vessel coronary artery disease, defined as the presence of ≥ 50% narrowing of the luminal diameter of one major coronary artery by coronary angiography, MRI angiography or CT angiography in patients not revascularized and at least one of the following | |
| A positive non-invasive stress test, confirmed by either | ||
| A positive ECG exercise tolerance test in patients without left bundle branch block, Wolff–Parkinson–White syndrome, left ventricular hypertrophy with repolarization abnormality, or paced ventricular rhythm, atrial fibrillation in case of abnormal ST-T segments | ||
| A positive stress echocardiogram showing induced regional systolic wall motion abnormalities | ||
| A positive nuclear myocardial perfusion imaging stress test showing stress-induced reversible perfusion abnormality | ||
| A positive cardiac stress perfusion MRI showing a stress-induced perfusion defect | ||
| Patient discharged from hospital with a documented diagnosis of unstable angina pectoris between 2 and 12 months prior to screening | ||
| (d) | History of ischemic or hemorrhagic stroke (> 3 months prior to screening) | |
| (e) | Presence of carotid artery disease (symptomatic or not) documented by either | |
| Imaging techniques with at least one lesion estimated to be ≥ 50% narrowing of the luminal diameter | ||
| Prior percutaneous or surgical carotid revascularization | ||
| (f) | Presence of peripheral artery disease documented by either | |
| Previous limb angioplasty, stenting or bypass surgery | ||
| Previous limb or foot amputation due to macrocirculatory insufficiency | ||
| Angiographic evidence of peripheral artery stenosis ≥ 50% narrowing of the luminal diameter in at least one limb (definition of peripheral artery: common iliac artery, internal iliac artery, external iliac artery, femoral artery, popliteal artery) | ||
| II | Impaired renal function with/without CV comorbidities | |
| eGFR (MDRD) of 15 to < 45 mL/min/1.73 m2 at screening | ||
| eGFR (MDRD) ≥ 45 to 75 mL/min/1.73 m2 at screening with UACR > 200 mg/g or > 200 μg albumin/min or > 200 mg albumin/24 h in two out of three unrelated spot urine or timed samples in the 24 months prior to randomization | ||
CT computed tomography, CV cardiovascular, ECG electrocardiogram, eGFR estimated glomerular filtration rate, MDRD Modification of Diet in Renal Disease study equation, MRI magnetic resonance imaging, UACR, urinary albumin-to-creatinine ratio
Individuals who had had an acute coronary syndrome in the 2 months prior to screening were ineligible, as were those who had had a stroke or transient ischemic attack in the 3 months before screening, and those who were scheduled to have percutaneous coronary intervention (PCI) or coronary artery bypass graft surgery (CABG) or had had PCI and/or CABG in the 2 months before screening. Also excluded were individuals with ESKD, defined as an estimated glomerular filtration rate (eGFR) by the Modification of Diet in Renal Disease study equation (MDRD) of < 15 mL/min/1.73 m2 and/or the receipt of maintenance dialysis. Premenopausal women who were pregnant, nursing, or not practicing birth control were also excluded, as were individuals with active liver disease or impaired hepatic function (serum levels of alanine aminotransferase, aspartate aminotransferase or alkaline phosphatase equal to or greater than three times the upper limit of normal [≥ 3× ULN]), and those with prior or planned bariatric surgery. The full inclusion and exclusion criteria are shown in Additional file 1.
Randomization, investigational product administration and follow-up
Eligible individuals were randomized 1:1 via an interactive telephone/web-based system to receive once-daily oral treatment with linagliptin 5 mg (the licensed dose) or matching placebo in a double-blind manner (Fig. 2). Treatment assignment was determined by computer-generated random sequence with stratification by geographical region. Following randomization, participants were instructed to return to the clinic for check-up after 12 weeks and then every 24 weeks until study end. Assessments included checks for adverse events and outcome events, physical examinations, vital signs, laboratory parameters, and 12-lead electrocardiograms (ECGs).
The use of additional medication for optimizing glycemic control according to local standard of care was encouraged throughout the trial independent of study treatment assignment, and included any approved glucose-lowering drugs except DPP-4 inhibitors, GLP-1 receptor agonists, and SGLT2 inhibitors. Dosing was required to adhere to local labelling and be in accordance with local/international guidelines. Intensification of glycemic control was advised for participants with fasting plasma glucose > 180 mg/dL (> 10.0 mmol/L) (confirmed by at least two measurements on different days) and those with HbA1c > 7.5% (> 58 mmol/mol). Investigators were also encouraged to treat all other CV risk factors (e.g. dyslipidemia, hypertension, albuminuria, smoking) in accordance with optimal local or regional guidelines and standards of care. Ultimately, changes in medication were at the discretion of the investigator and/or treating clinician.
Outcomes and adjudication
The primary outcome is the time to the first occurrence of CV death, non-fatal myocardial infarction (MI) or non-fatal stroke—the so-called 3-point major adverse CV events (3P-MACE) composite outcome. The adoption of 3P-MACE as the primary outcome resulted from a study protocol amendment in 2016 from the original primary outcome of 4P-MACE (3P-MACE plus hospitalization for unstable angina). Although no longer a component of the primary composite, hospitalization for unstable angina continued to be an adjudicated endpoint. This amendment was made by the CARMELINA® steering committee based on emerging evidence from other CV outcomes studies accumulated since study start indicating that 3P-MACE is the more suitable primary outcome for studies of glucose-lowering medications [29] and, accordingly, is now preferred by the FDA as a CV outcome over the 4P-MACE composite outcome [30]. This change aligns CARMELINA® with other recent and ongoing studies of novel glucose-lowering drugs [29]. The steering committee had neither access to unblinded data nor input from the independent data monitoring committee when making this amendment, and the study remained fully blinded to the steering committee, sponsor, trial team, investigators and participants during these deliberations.
The key secondary outcome is a kidney composite of time to first occurrence of sustained ESKD, renal death (adjudicated death due to kidney disease), or a sustained decrease of ≥ 40% in eGFR from baseline. This kidney composite outcome had been amended in 2016 to lower the threshold for sustained eGFR decrease from ≥ 50 to ≥ 40%. This amendment was made on the basis of evolving clinical evidence and multi-disciplinary workshops convened by the US National Kidney Foundation and the FDA, where it was concluded that there is strong evidence for a sustained decline of ≥ 40% in eGFR being an appropriate outcome for clinical trials seeking to identify evidence of kidney protection [31, 32]. Furthermore, both the FDA and the EMA have acknowledged that a ≥ 40% decline in eGFR is a suitable outcome in kidney outcome studies to improve trial efficiency [32, 33]. The original key secondary composite outcome (time to first occurrence of ESKD, renal death, or a sustained decrease of ≥ 50% in eGFR from baseline) will be evaluated as a tertiary endpoint.
Further tertiary outcomes include the following, among others: 4P-MACE, CV death, fatal or non-fatal MI, fatal or non-fatal stroke, hospitalization for unstable angina, stent thrombosis, transient ischemic attack, all-cause mortality, and renal death. Additional kidney-related endpoints include transition in albuminuria class or CKD stage from baseline as well as eGFR slope analyses. Glucose-related outcomes include change from baseline in levels of HbA1c and fasting plasma glucose.
All CV and cerebrovascular events are prospectively ascertained and centrally adjudicated by an independent and blinded external clinical event committee, as recommended by the FDA [3]. Some heterogeneity in the risk of heart failure has been observed in previous outcome trials of DPP-4 inhibitors. In CARMELINA®, hospitalization for heart failure is prospectively evaluated. All reported events of hospitalization for heart failure are independently adjudicated under blinded conditions by a central committee based on pre-defined criteria. Hospitalization for heart failure is another pre-defined tertiary outcome in the protocol—both on its own and as a composite with CV death, consistent with contemporary best practice in heart failure trials. Separate independent and blinded clinical event committees adjudicate kidney and pancreatic events.
Identification of potential outcome events sent for adjudication based on investigator reports was supplemented using a search of the trial database for events based on Standardised Medical Dictionary for Regulatory Activities (MedDRA) Queries and other events defined in the adjudication charters to trigger adjudication committee review. Furthermore, all deaths were sent for adjudication. Additionally, a periodic, blinded pharmacovigilance review of all other (non-trigger) events was performed.
Safety is assessed based on all reported adverse events (including serious adverse events and adverse events of special interest), physical examinations, vital signs, laboratory parameters, and 12-lead ECGs. Hypoglycemia was defined as documented blood glucose ≤ 70 mg/dL (≤ 3.9 mmol/L) with the exception of severe hypoglycemia, which was defined as any episode requiring third-party assistance. Incidence and event rates will be analyzed for hypoglycemia ≤ 70 mg/dL (≤ 3.9 mmol/L) and < 54 mg/dL (< 3.0 mmol/L) or severe hypoglycemia. Adverse events pre-specified as being of special interest were hypersensitivity reactions, skin lesions, kidney adverse events including acute kidney injury, pancreatitis, pancreatic cancer, benign thyroid neoplasms, thyroid cancer and hepatic events. A periodic review of all lipase values ≥ 3× ULN not reported as adverse events was performed.
Study oversight and organization
The CARMELINA® trial was sponsored by Boehringer Ingelheim, the manufacturer of linagliptin, and Eli Lilly and Company. CARMELINA® was designed jointly by independent academic investigators and sponsor-employed scientists and physicians with relevant clinical and methodological expertise, who together comprise the steering committee. The steering committee, led by the academic investigators, supervised the conduct of the trial, and an independent data monitoring committee regularly reviewed safety data, on the basis of which it recommended the trial to continue or terminate early according to a pre-specified charter. Independent contract research organizations were involved in interactive response technology for randomization, analyses of ECGs, blinded event adjudication, central laboratory analyses, and operational implementation of the trial.
Statistical analysis
The primary null hypothesis was that treatment with linagliptin would be inferior by a hazard ratio of ≥ 1.3 compared with placebo as assessed by the time to first occurrence of any of the 3P-MACE (primary endpoint) events. Rejection of the null hypothesis will be evaluated by the upper limit of the two-sided 95% confidence interval (CI) for the hazard ratio, as required by FDA guidance [3]. The test of the primary outcome for non-inferiority is the first of the following two-step testing strategy in which superiority tests will only be performed if the first test is statistically significant: (i) non-inferiority test of the primary outcome; (ii) superiority tests of (a) the primary outcome and (b) the key secondary composite kidney outcome, with a sequentially rejective multiple test procedure (Fig. 3).
Fig. 3.
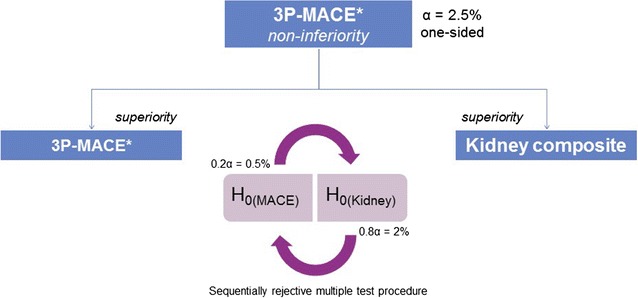
Statistical testing for the primary and secondary endpoints. For the final analysis, the first hypothesis (non-inferiority of the primary endpoint [3P-MACE]) will be tested at the one-sided alpha-level of 2.5%. In case of significance, the null hypothesis (H0) is rejected in a confirmatory sense and the next set of hypotheses (two separate hypothesis tests) will be tested: (a) test of the primary endpoint for superiority and (b) test of the composite renal endpoint for superiority. To adjust for multiplicity, a sequentially rejective multiple test procedure will be applied. Both one-sided hypotheses H0(Sup1) and H0(Sup2) will be tested separately, at the initial alpha-levels of ×0.2 alpha for the primary endpoint and ×0.8 alpha for the composite renal endpoint, respectively. If both null hypotheses cannot be rejected at these initial alpha-levels, the procedure stops and for neither endpoint can superiority be declared. After having shown superiority for one of these endpoints, the used alpha can be shuffled to the other test: If H0(Sup2) is rejected at the alpha-level of ×0.8 alpha, then H0(Sup1) can be tested at the full alpha-level of 2.5% (one-sided). If H0(Sup1) is rejected at the alpha-level of ×0.2 alpha, then H0(Sup2) can be tested at the full alpha-level of 2.5% (one-sided). *Cardiovascular death, non-fatal myocardial infarction, or non-fatal stroke. H0 null hypothesis, 3P-MACE 3-point major adverse cardiovascular events
A total of 611 primary (3P-MACE) events provides 90% power to demonstrate non-inferiority of linagliptin versus placebo at the overall one-sided α-level of 2.5% if the hazard ratio is 1.0. The sample size and event estimates were based on the primary hypothesis.
If non-inferiority has been demonstrated, then superiority with regard to the primary outcome will be tested. Assuming 611 patients with an event and a hazard rate for linagliptin at any time 20% less than the risk for placebo, then the resulting power to demonstrate superiority at the final analysis is 79% for a test at the α-level of 2.5%.
Assuming 432 patients with a composite kidney outcome, an annualized event rate of 2.5% in the placebo group and a hazard rate for linagliptin of 0.75, then the resulting power to demonstrate superiority for the key secondary outcome at the final analysis is 85% if the test can be performed at the α-level of 2.5%.
The primary and key secondary outcomes will be analyzed using the treated set (all patients treated with at least one dose of study drug) with treatment assignment at randomization and including all adjudication-confirmed events that occur until study end. The primary and key secondary endpoints will be analyzed using a Cox proportional hazards regression model of time to the first event, with randomized treatment and geographical region as factors.
Sensitivity analyses will be conducted on the per-protocol set, which excludes patients with important protocol violations such as incorrect study drug taken; the on-treatment set with a minimum treatment duration of 30 days; and the treated set with censoring at 30 days after last dose of study drug (treated set + 30). For these analyses, events will be considered that have occurred no later than 30 days after last intake of study drug. An additional analysis will only include outcome events until last study drug intake (treated set + 0).
The primary and key secondary outcomes will also be analyzed in patient subgroups based on several baseline characteristics, including but not limited to the following: geographical region, age, sex, blood pressure, insulin use, eGFR < 60 mL/min/1.73 m2, and prevalent kidney disease (eGFR < 60 mL/min/1.73 m2 or urinary albumin-to-creatinine ratio [UACR] > 300 mg/g).
Safety will be evaluated in the treated set using descriptive statistical analyses of adverse events, as well as changes in clinical and laboratory parameters.
The data will be analyzed by the contract research organization in charge of study conduct, the sponsor, and the statistics group at the Duke Clinical Research Institute (Durham, NC, USA) who will conduct an independent statistical analysis.
Results
Recruitment of participants for the CARMELINA® study began in July 2013 and was completed in August 2016. A total of 12,280 individuals were screened and 6991 were randomized at 407 clinics in 27 countries. Of these, 6980 participants received at least one dose of study drug. Europe provided the largest number of participants (n = 2833 [40.6%]), followed by South America (n = 2310 [33.1%]), North America (n = 1180 [16.9%]) and Asia (n = 657 [9.4%]).
Pooled baseline characteristics of the participants are shown in Table 2. Participants had mean age, HbA1c, and BMI of 65.8 years, 7.9% and 31.3 kg/m2, respectively, with mean duration of diabetes of 14.7 years (Table 2). The majority were male (63%), white (80%) and had eGFR < 60 mL/min/1.73 m2 (62%). Mean eGFR was 54.6 mL/min/1.73 m2, and 1063 (15%) participants had severe renal impairment (eGFR < 30 and > 15 mL/min/1.73 m2). Median UACR was 162 mg/g (25th–75th percentile: 44–727 mg/g); 1390 participants (20%) were normoalbuminuric (UACR < 30 mg/g), while the majority had either microalbuminuria (UACR 30 − 300 mg/g; n = 2896 [41.5%]) or macroalbuminuria (UACR > 300 mg/g; n = 2691 [39%]). Mean systolic and diastolic blood pressure were 141 and 78 mmHg, respectively, and 95% of participants (6637) were taking antihypertensive medication. Angiotensin-converting enzyme (ACE) inhibitors or angiotensin-receptor blockers were being taken by 81% of the trial population, while 53% were taking diuretics.
Table 2.
Baseline characteristics
| Total (n = 6980) | |
|---|---|
| Age, years | 65.8 ± 9.1 |
| Male, n (%) | 4390 (62.9) |
| Race, n (%) | |
| White | 5595 (80.2) |
| Asian | 641 (9.2) |
| Black/African American | 411 (5.9) |
| Othera | 333 (4.8) |
| Region, n (%) | |
| Europe | 2833 (40.6) |
| South America | 2310 (33.1) |
| North America | 1180 (16.9) |
| Asia | 657 (9.4) |
| Smoking status, n (%) | |
| Never smoker | 3753 (53.8) |
| Ex-smoker | 2507 (35.9) |
| Current smoker | 713 (10.2) |
| Missing | 7 (0.1) |
| eGFR (MDRD), mL/min/1.73 m2 | 54.6 ± 25.0 |
| eGFR (MDRD), n (%) | |
| ≥ 90 mL/min/1.73 m2 | 728 (10.4) |
| ≥ 60 to < 90 mL/min/1.73 m2 | 1903 (27.3) |
| ≥ 45 to < 60 mL/min/1.73 m2 | 1349 (19.3) |
| ≥ 30 to < 45 mL/min/1.73 m2 | 1937 (27.8) |
| < 30 mL/min/1.73 m2 | 1063 (15.2) |
| UACR, mg/g, median (25th–75th percentile) | 162 (44–727)c |
| UACR, n (%) [mg/g] | |
| < 30 | 1390 (19.9) |
| 30–300 | 2896 (41.5) |
| > 300 | 2691 (38.6) |
| Missing | 3 (0.0) |
| BMI, kg/m2 | 31.3 ± 5.3d |
| HbA1c, % | 7.9 ± 1.0 |
| Fasting plasma glucose, mmol/Lb (mg/dL) | 8.4 ± 3.4 (151.8 ± 61.7)e |
| Diabetes duration, years | 14.7 ± 9.5 |
| Systolic blood pressure, mmHg | 140.5 ± 17.9 |
| Diastolic blood pressure, mmHg | 77.8 ± 10.5 |
| Total cholesterol, mmol/L (mg/dL) | 4.5 ± 1.3 (172 ± 48)f |
| LDL cholesterol, mmol/L (mg/dL) | 2.4 ± 1.0 (91 ± 40)g |
| HDL cholesterol, mmol/L (mg/dL) | 1.2 ± 0.3 (45 ± 13)h |
| Triglycerides, mmol/L (mg/dL) | 2.1 ± 1.5 (188 ± 133)f |
| Glucose-lowering therapy, n (%) | 6802 (97.4) |
| Metformin | 3823 (54.8) |
| Sulfonylurea | 2434 (34.9) |
| Insulin | 4039 (57.9) |
| Antihypertensives, n (%) | 6637 (95.1) |
| ACE inhibitors or ARBs | 5655 (81.0) |
| β-blockers | 4144 (59.4) |
| Diuretics | 3711 (53.2) |
| Calcium antagonists | 2870 (41.1) |
| Platelet aggregation inhibitors (excluding heparin), n (%) | 4764 (68.3) |
| Statins, n (%) | 5010 (71.8) |
Data are mean ± SD unless otherwise specified, and may change slightly when the trial is completed
ACE angiotensin-converting enzyme, ARB angiotensin-receptor blocker, BMI body-mass index, eGFR estimated glomerular filtration rate, HbA1c glycated hemoglobin A1c, HDL high-density lipoprotein, LDL low-density lipoprotein, MDRD Modification of Diet in Renal Disease study equation, UACR urinary albumin-to-creatinine ratio
aAmerican Indian/Alaska Native or Native Hawaiian/other Pacific Islander, b calculated by multiplying mg/dL values by 0.0555 [34], c n = 6977, d n = 6975, e n = 6915; f n = 6749, g n = 6744, h n = 6748
Mean levels of low-density lipoprotein cholesterol, high-density lipoprotein cholesterol and triglycerides were 2.4 mmol/L (91 mg/dL), 1.2 mmol/L (45 mg/dL), and 2.1 mmol/L (188 mg/dL), respectively. A total of 5010 (72%) and 4764 (68%) participants were taking statins and platelet aggregation inhibitors (excluding heparin), respectively. Almost all participants (n = 6802 [97%]) were taking glucose-lowering medication at baseline. Over half (n = 4039 [58%]) were taking insulin, while metformin was the most frequently used oral drug (n = 3823, [55%]) (Table 2).
The majority of patients from the overall trial population (5148 [74%]), had prevalent kidney disease at baseline, defined as eGFR < 60 mL/min/1.73 m2 or UACR ≥ 300 mg/g, while 3990 (57%) had established CV disease with elevated UACR (≥ 30 mg/g) and 2268 (32.5%) had both conditions (Fig. 4). Baseline characteristics for patients with prevalent kidney disease are shown in Table 3, while Additional files 2 and 3 show baseline characteristics for those with established CV disease and those with both prevalent kidney disease and established CV disease.
Fig. 4.
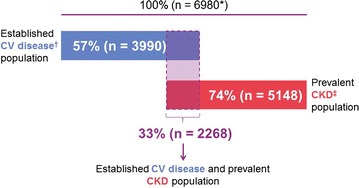
Proportion of patients included in the CARMELINA® trial with established CV disease, prevalent kidney disease, or both. *110 patients without established CV disease had eGFR ≥ 60 mL/min/1.73 m2 and UACR ≤ 300 mg/g. †Defined as albuminuria (UACR ≥ 30 mg/g or ≥ 30 μg albumin/min or ≥ 30 mg albumin/24 h) and prevalent macrovascular disease (≥ 1 of the following: confirmed history of myocardial infarction; advanced coronary artery disease; high-risk single-vessel coronary artery disease; history of ischemic or hemorrhagic stroke; presence of carotid artery disease; presence of peripheral artery disease). ‡Defined as eGFR < 60 mL/min/1.73 m2 or macroalbuminuria (UACR > 300 mg/g). CKD chronic kidney disease, CV cardiovascular, eGFR estimated glomerular filtration rate, UACR urinary albumin-to-creatinine ratio
Table 3.
Baseline characteristics by prevalent kidney disease at baseline
| Prevalent CKDa (n = 5148) | No prevalent CKD (n = 1832) | |
|---|---|---|
| Age, years | 66.8 ± 9.0 | 62.9 ± 8.8 |
| Male, n (%) | 3114 (60.5) | 1276 (69.7) |
| Race, n (%) | ||
| White | 4042 (78.5) | 1553 (84.8) |
| Asian | 508 (9.9) | 133 (7.3) |
| Black/African American | 349 (6.8) | 62 (3.4) |
| Otherb | 249 (4.8) | 84 (4.6) |
| Region, n (%) | ||
| Europe | 1997 (38.8) | 836 (45.6) |
| South America | 1658 (32.2) | 652 (35.6) |
| North America | 984 (19.1) | 196 (10.7) |
| Asia | 509 (9.9) | 148 (8.1) |
| Smoking status, n (%) | ||
| Never smoker | 2821 (54.8) | 932 (50.9) |
| Ex-smoker | 1861 (36.1) | 646 (35.3) |
| Current smoker | 461 (9.0) | 252 (13.8) |
| Missing | 5 (0.1) | 2 (0.1) |
| eGFR (MDRD), mL/min/1.73 m2 | 44.6 ± 19.2 | 82.6 ± 16.9 |
| eGFR (MDRD), n (%) | ||
| ≥ 90 mL/min/1.73 m2 | 179 (3.5) | 549 (30.0) |
| ≥ 60 to < 90 mL/min/1.73 m2 | 620 (12.0) | 1283 (70.0) |
| ≥ 45 to < 60 mL/min/1.73 m2 | 1349 (26.2) | 0 |
| ≥ 30 to < 45 mL/min/1.73 m2 | 1937 (37.6) | 0 |
| < 30 mL/min/1.73 m2 | 1063 (20.6) | 0 |
| UACR, mg/g, median (25th–75th percentile) | 336 (60–1126)d | 70 (27–138)j |
| UACR, n (%) [mg/g] | ||
| < 30 | 907 (17.6) | 483 (26.4) |
| 30–300 | 1548 (30.1) | 1348 (73.6) |
| > 300 | 2691 (52.3) | 0 |
| BMI, kg/m2 | 31.4 ± 5.4e | 31.0 ± 5.1 |
| HbA1c, % | 7.9 ± 1.0 | 8.0 ± 1.0 |
| Fasting plasma glucose, mmol/Lc (mg/dL) | 8.3 ± 2.6 (150.1 ± 47.5)f | 8.7 ± 5.0 (156.5 ± 90.3)k |
| Diabetes duration, years | 15.9 ± 9.6 | 11.6 ± 8.4 |
| Systolic blood pressure, mmHg | 141.7 ± 18.5 | 137.2 ± 15.3 |
| Diastolic blood pressure, mmHg | 77.5 ± 10.8 | 78.8 ± 9.5 |
| Total cholesterol, mmol/L (mg/dL) | 4.5 ± 1.3 (173 ± 50)g | 4.4 ± 1.2 (168 ± 44)l |
| LDL cholesterol, mmol/L (mg/dL) | 2.4 ± 1.1 (92 ± 40)h | 2.3 ± 1.0 (90 ± 37)m |
| HDL cholesterol, mmol/L (mg/dL) | 1.2 ± 0.3 (45 ± 13)i | 1.1 ± 0.3 (44 ± 12)l |
| Triglycerides, mmol/L (mg/dL) | 2.2 ± 1.5 (191 ± 136)g | 2.0 ± 1.4 (181 ± 125)l |
| Glucose-lowering therapy, n (%) | 5013 (97.4) | 1789 (97.7) |
| Metformin | 2350 (45.6) | 1473 (80.4) |
| Sulfonylurea | 1653 (32.1) | 781 (42.6) |
| Insulin | 3294 (64.0) | 745 (40.7) |
| Antihypertensives, n (%) | 4946 (96.1) | 1691 (92.3) |
| ACE inhibitors or ARBs | 4183 (81.3) | 1472 (80.3) |
| β-blockers | 3043 (59.1) | 1101 (60.1) |
| Diuretics | 3032 (58.9) | 679 (37.1) |
| Calcium antagonists | 2313 (44.9) | 557 (30.4) |
| Platelet aggregation inhibitors (excluding heparin), n (%) | 3365 (65.4) | 1399 (76.4) |
| Statins, n (%) | 3708 (72.0) | 1302 (71.1) |
Data are mean ± SD unless otherwise specified, and may change slightly when the trial is completed
ACE angiotensin-converting enzyme, ARB angiotensin-receptor blocker, BMI body-mass index, CKD chronic kidney disease, eGFR estimated glomerular filtration rate, HbA1c glycated hemoglobin A1c, HDL high-density lipoprotein, LDL low-density lipoprotein, MDRD Modification of Diet in Renal Disease study equation, UACR urinary albumin-to-creatinine ratio
aDefined as eGFR < 60 mL/min/1.73 m2 or macroalbuminuria (UACR > 300 mg/g), b American Indian/Alaska Native or Native Hawaiian/other Pacific Islander, c calculated by multiplying mg/dL values by 0.0555 [34], d n = 5146, e n = 5143, f n = 5097, g n = 4971, h n = 4967, i n = 4970, j n = 1831, k n = 1818, l n = 1778, m n = 1777
Approximately 71% of CARMELINA® participants are considered at high risk (n = 1902 [27.2%]) or very high risk (n = 3033 [43.5%]) for adverse kidney events, on the basis of their eGFR and albuminuria status at baseline according to risk stratification by Kidney Disease: Improving Global Outcomes (KDIGO) foundation standards (Fig. 5).
Fig. 5.
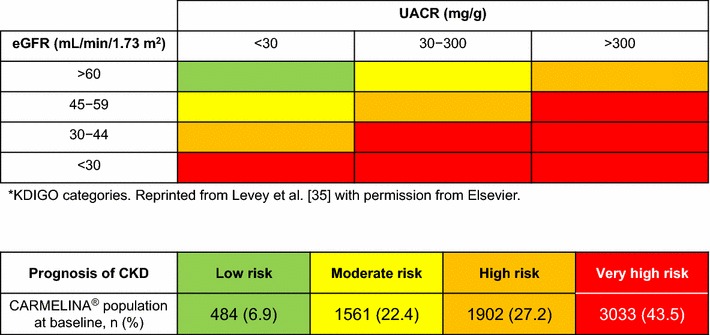
Prognosis of CKD in the CARMELINA® trial population by eGFR and albuminuria categories.*CKD chronic kidney disease, eGFR estimated glomerular filtration rate, KDIGO Kidney Disease: Improving Global Outcomes, UACR urinary albumin-to-creatinine ratio
Discussion
The CARMELINA® trial comprises 6991 patients with T2D randomized to daily oral treatment with the DPP-4 inhibitor linagliptin or placebo on top of standard care. Baseline characteristics of the treated set (n = 6980) delineate a population with long-standing T2D and a substantial burden of both CV and kidney disease. As intended, this will enable assessment of whether linagliptin is non-inferior—and, if so, superior—to placebo for CV and renal outcomes in individuals with T2D at very high vascular risk.
A pooled analysis of 19 randomized clinical trials of linagliptin involving 9459 individuals found no increased risk for major adverse CV events [27]. However, this analysis was limited by the short duration of drug exposure, inclusion of participants at relatively low CV risk, the small number of CV events for analysis, and the fact that these trials were not designed to assess either CV or renal safety. In hypothesis-generating, mechanistic clinical studies, linagliptin did not alter macrovascular function, but showed potential to improve microvascular function [36, 37], reduced early atherosclerotic vascular wall inflammation [38] and appeared to improve arterial stiffness [39].
In the last decade, a multitude of CV outcomes trials of glucose-lowering drugs have been initiated [29]. The trials completed to date have shown discordant results. The studies of empagliflozin, an SGLT2 inhibitor, and liraglutide, a GLP-1 receptor agonist, observed statistically significant reductions in CV mortality of 38% (hazard ratio, 0.62 [95% CI 0.49–0.77]) [9] and 22% (hazard ratio, 0.78 [95% CI 0.66–0.93]) [11], respectively. The outcomes trial of the SGLT2 inhibitor canagliflozin found a significant reduction in CV events (hazard ratio, 0.86 [95% CI 0.75–0.97) [13]. The GLP-1 receptor agonist semaglutide was shown to be non-inferior to placebo in CV safety (hazard ratio, 0.74, 95% CI 0.58–0.95) [12], while another two GLP-1 receptor agonists (lixisenatide [10] and once-weekly exenatide [15]) have demonstrated CV safety but no significant reduction in CV events. The three DPP-4 inhibitors studied to date (saxagliptin [6], alogliptin [7], sitagliptin [8]) have demonstrated neutral effects on atherosclerotic CV disease. However, a significantly increased risk of hospitalization for heart failure with saxagliptin was observed in the SAVOR-TIMI 53 study [6]. It remains to be determined whether this reflects a class effect of DPP-4 inhibitors, as a numerical (but non-significant) increase in hospitalization for heart failure was also seen in the EXAMINE study of alogliptin [23] but not in the TECOS study of sitagliptin [24]. Recent observational studies have suggested that individuals treated with DPP-4 inhibitors may have a lower risk for CV disease (including events of heart failure) than those treated with either a non-sulfonylurea insulin secretagogue or insulin [40], and that the risk of heart failure with linagliptin is not increased compared with sulfonylureas [41]. The CARMELINA® study will thoroughly explore heart failure-related outcomes with linagliptin, as it includes hospitalization for heart failure as an adjudicated and pre-specified outcome and is proactively capturing information related to heart failure.
The CV outcomes data provided by CARMELINA® will also complement the results from the ongoing CAROLINA® study of linagliptin (ClinicalTrials.gov identifier: NCT01243424) [42]. CAROLINA® is designed to evaluate the CV outcomes of linagliptin as a second-line treatment added to metformin. CAROLINA® is comparing linagliptin with an active compound, the sulfonylurea glimepiride, rather than placebo, and with this unique design represents the only active-controlled, double-blind, multinational CV outcome study to date in patients with T2D. Furthermore, by design, the participants in CAROLINA® have lower overall CV and renal risk, earlier stage of T2D disease (median duration 6.2 years), and better glycemic control (mean baseline HbA1c 7.2%) [42] than those in the CARMELINA® study. The results from CAROLINA® will help inform decision-making for second-line treatment of early T2D and may answer a long-standing question regarding the CV safety of sulfonylureas.
In addition to CV safety, CARMELINA® was also designed and powered to evaluate renal outcomes of linagliptin treatment in an alpha-controlled manner—a notable feature compared to CV outcomes studies of other glucose-lowering drugs. Accordingly, the proportion of participants with overt kidney disease (defined as eGFR < 60 mL/min/1.73 m2 or macroalbuminuria [74%]) or reduced kidney function (eGFR < 60 mL/min/1.73 m2 [62%]) is substantially higher in CARMELINA® than in other CV outcomes studies of oral glucose-lowering drugs in T2D (9.3–29.1%) [6–12, 43, 44] (Fig. 6). CARMELINA® also includes a large number of individuals with very low eGFR (< 30 mL/min/1.73 m2) (n = 1063 [15%]) and/or elevated levels of albuminuria (n = 5587 [80%]) (Additional file 4).
Fig. 6.
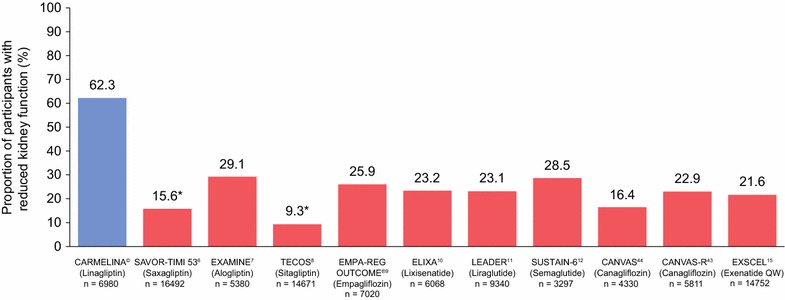
Proportion of patients with reduced kidney function at baseline (eGFR < 60 mL/min/1.73 m2) in CARMELINA® compared to previously reported CV outcome trials of non-insulin glucose-lowering drugs for T2D. *eGFR < 50 mL/min/1.73 m2. CV cardiovascular, eGFR estimated glomerular filtration rate, QW once weekly, T2D type 2 diabetes
No new pharmacotherapy for diabetic kidney disease has been licensed since the early 2000s when the angiotensin-receptor blockers losartan and irbesartan demonstrated efficacy in this indication [45]. Hypothesis-generating evidence has suggested that DPP-4 inhibitors may have specific renal effects independent of their glucose-lowering properties [46]. A pooled analysis of 13 randomized controlled studies found that linagliptin treatment was associated with a significant 16% reduction in the risk for clinically relevant adverse renal events (hazard ratio 0.84, 95% CI 0.72–0.97; P = 0.02) [28]. Additional data from pooled analyses of the linagliptin development program [47] and exploratory data from SAVOR-TIMI 53 and TECOS [48, 49] suggested that DPP-4 inhibitors could lower albuminuria in patients with T2D. This hypothesis was, however, not supported by the MARLINA-T2D™ study of linagliptin, which was the first randomized clinical study prospectively designed to investigate the effects of a DPP-4 inhibitor on albuminuria [50]. In MARLINA-T2D™, linagliptin elicited a placebo-adjusted, non-significant 6% reduction in albuminuria (95% CI − 15.0 to 3.0; P = 0.1954) after 24 weeks of treatment in individuals with T2D and early diabetic kidney disease who had residual albuminuria despite receiving ACE inhibitors or angiotensin-receptor blockers [50]. Since previous clinical evidence for renal effects of DPP-4 inhibitors has mainly emerged from patient populations at earlier stages of kidney disease, CARMELINA® will answer an important question whether DPP-4 inhibition with linagliptin may have the potential to alter renal disease progression at more advanced stages of the renal continuum. Respective experimental evidence to support such a hypothesis has emerged from recent preclinical studies showing that linagliptin exerted anti-fibrotic, anti-inflammatory and anti-oxidant renal effects in animal models of diabetic kidney disease that—if translated to human disease—would be more likely to manifest as long-term disease-modifying renal effects than to elicit short-term changes in albuminuria [51–54].
Conclusions
The CARMELINA® trial is designed to assess CV and kidney outcomes of the DPP-4 inhibitor linagliptin versus placebo when added to standard care in individuals with T2D and established CV and/or kidney complications. Compared with the spectrum of CV outcome trials conducted in patients with T2D to date, CARMELINA® has the highest number of individuals with prevalent kidney disease, including a large proportion of patients with severe kidney impairment and/or elevated albuminuria. These individuals are at a very high CV risk, face limited glucose-lowering treatment options, and have been largely underrepresented in previous CV outcomes trials in T2D. CARMELINA® will thus enable assessment of the inherent effects of linagliptin on CV and kidney events in a vulnerable population at high cardio-renal risk. Results are expected in 2018.
Additional files
Additional file 1. Full inclusion and exclusion criteria for CARMELINA®.
Additional file 2. Baseline characteristics by established CV disease at baseline in CARMELINA® participants.
Additional file 3. Baseline characteristics by established CV disease and prevalent kidney disease at baseline in CARMELINA® participants.
Additional file 4. CARMELINA® baseline characteristics versus TECOS and SAVOR-TIMI 53.
Authors’ contributions
All authors participated in design of the study, and collection and interpretation of data. JR, VP, DKM, JT, and MvE were involved in developing the initial draft of the manuscript and all subsequent revisions, and approved the final version. JHA, MEC, NM, MJP, RDT, CW, BZ, DB, EP, MM, UCB, and HJW reviewed the initial draft and all subsequent revisions. All authors read and approved the final manuscript.
Acknowledgements
The authors thank the individuals who participated in this study. Medical writing assistance, supported financially by Boehringer Ingelheim, was provided by Giles Brooke, Ph.D., CMPP, of Envision Scientific Solutions during the preparation of this manuscript.
Competing interests
JR has served on scientific advisory boards and received honoraria or consulting fees from Eli Lilly, Sanofi, Novo Nordisk, Janssen, AstraZeneca, Boehringer Ingelheim and Intarcia; he has also received grants/research support from Merck, Pfizer, Sanofi, Novo Nordisk, Bristol-Myers Squibb, Eli Lilly, GlaxoSmithKline, Genentech, Janssen, Lexicon, Boehringer Ingelheim and Intarcia. VP consults for AbbVie, Astellas, Bristol-Myers Squibb, Boehringer Ingelheim, Eli Lilly, GlaxoSmithKline, Janssen, Novartis, Retrophin, and Astra Zeneca; has received lecture fees or grant support from Baxter, Boehringer Ingelheim, Merck and Pfizer; and his institution has held clinical trial contracts with AbbVie, Roche, Janssen, Servier and Novartis. JHA has received institutional research grants from Bristol-Myers Squibb, Boehringer Ingelheim, CSL Behring, National Institutes of Health, Regado Biosciences, Sanofi, Tenax Therapeutics, Vivus Pharmaceuticals; consulting fees from Bristol-Myers Squibb, Portola Pharmaceuticals, Somahlution; and honoraria from Bristol-Myers Squibb, Portola Pharmaceuticals, Somahlution. MEC has received fees for advisory services to Boehringer Ingelheim. NM has served as a consultant to AstraZeneca, Amgen, Bayer, Bristol-Myers Squibb, Boehringer Ingelheim, Merck, Novo Nordisk, Roche, and Sanofi and has received grant support from Merck and Boehringer Ingelheim; he has served as a speaker for AstraZeneca, Amgen, Bayer, Bristol-Myers Squibb, Boehringer Ingelheim, Lilly, Merck, Mitsubishi Tanabe Pharma Corporation, Novartis, Novo Nordisk, Pfizer, Roche, and Sanofi. MJP has no competing interests. RT is a consultant to Amgen, Boehringer Ingelheim, ZS Pharma, Relypsa, Novo Nordisk, Reata, AstraZeneca and receives grant support from the NIH. CW has received grants from the European Foundation for the Study of Diabetes (EFSD), personal fees from Boehringer Ingelheim (steering committee membership, lecturing), and personal fees from Janssen (data safety monitoring board membership). BZ has received grant support from Boehringer Ingelheim, AstraZeneca and Novo Nordisk; and consulting fees from AstraZeneca, Boehringer Ingelheim, Eli Lilly, Janssen, Merck, Novo Nordisk, and Sanofi Aventis. DB, EP, MM, JTG, UCB, MvE are employees of Boehringer Ingelheim, the manufacturer of linagliptin. HJW was an employee of Boehringer Ingelheim at the time of the study. DKM has received support for clinical trial leadership from Novo Nordisk, AstraZeneca, Boehringer Ingelheim, Merck & Co., Lexicon, GlaxoSmithKline, Janssen, Lexicon, Sanofi Aventis and Eli Lilly and consultancy fees from Novo Nordisk, Sanofi-Aventis, Janssen, Boehringer Ingelheim, AstraZeneca, Eli Lilly and Merck & Co.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Ethics approval and consent to participate
The study protocol was approved by the respective Institutional Review Boards, Independent Ethics Committees and Competent Authorities according to national and international regulations. CARMELINA® is being conducted in accordance with the ICH Harmonised Tripartite Guideline for Good Clinical Practice. All participants provided written informed consent prior to entering the study.
Funding
This study was sponsored by the Boehringer Ingelheim & Eli Lilly and Company Diabetes Alliance. The authors employed by the sponsor were involved in study design, data collection, review and analysis.
Prior publication
Data from this study have previously been presented at the American Diabetes Association 77th Scientific Sessions, June 9–13, 2017, San Diego, CA, USA and the 53rd Annual Meeting of the European Association for the Study of Diabetes, Lisbon, Portugal, 11–15 September 2017.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- 3P-MACE
3-point major adverse cardiovascular events
- 4P-MACE
4-point major adverse cardiovascular events
- ACE
angiotensin-converting enzyme
- ARB
angiotensin-receptor blocker
- BMI
body-mass index
- CABG
coronary artery bypass graft surgery
- CANVAS
CANagliflozin cardioVascular Assessment Study
- CANVAS-R
CANVAS-Renal
- CARMELINA®
CArdiovascular safety and Renal Microvascular outcomE study with LINAgliptin
- CAROLINA®
CARdiovascular Outcome Study of LINAgliptin versus Glimepiride in Patients with Type 2 Diabetes
- CI
confidence interval
- CKD
chronic kidney disease
- CT
computed tomography
- CV
cardiovascular
- CVD
cardiovascular disease
- DPP-4
dipeptidyl peptidase-4
- ECG
electrocardiogram
- eGFR
estimated glomerular filtration rate
- ELIXA
Evaluation of Lixisenatide in Acute Coronary Syndrome
- EMA
European Medicines Agency
- EMPA-REG OUTCOME
EMPAgliflozin Removal of Excess Glucose: Cardiovascular OUTCOME Event Trial in Type 2 Diabetes Mellitus Patients
- ESKD
end-stage kidney disease
- EXAMINE
Examination of Cardiovascular Outcomes with Alogliptin versus Standard of Care
- EXSCEL
Exenatide Study of Cardiovascular Event Lowering
- FDA
US Food and Drug Administration
- GLP-1
glucagon-like peptide-1
- HbA1c
glycated hemoglobin A1c
- HDL
high-density lipoprotein
- KDIGO
Kidney Disease: Improving Global Outcomes
- LDL
low-density lipoprotein
- LEADER
Liraglutide Effect and Action in Diabetes: Evaluation of Cardiovascular Outcome Results
- MARLINA-T2D™
Efficacy, Safety & Modification of Albuminuria in Type 2 Diabetes Subjects With Renal Disease With LINAgliptin
- MDRD
Modification of Diet in Renal Disease study equation
- MI
myocardial infarction
- MRI
magnetic resonance imaging
- PCI
percutaneous coronary intervention
- P-gp
P-glycoprotein
- UACR
urinary albumin-to-creatinine ratio
- SAVOR-TIMI 53
Saxagliptin Assessment of Vascular Outcomes Recorded in Patients with Diabetes Mellitus-Thrombolysis in Myocardial Infarction 53
- SGLT2
sodium-glucose cotransporter 2
- SUSTAIN-6
Trial to Evaluate Cardiovascular and Other Long-term Outcomes with Semaglutide in Subjects with Type 2 Diabetes
- T2D
type 2 diabetes
- TECOS
Trial Evaluating Cardiovascular Outcomes with Sitagliptin
- UACR
urinary albumin-to-creatinine ratio
- ULN
upper limit of normal
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s12933-018-0682-3) contains supplementary material, which is available to authorized users.
Contributor Information
Julio Rosenstock, Email: juliorosenstock@dallasdiabetes.com.
Vlado Perkovic, Email: VPerkovic@georgeinstitute.org.au.
John H. Alexander, Email: john.h.alexander@duke.edu
Mark E. Cooper, Email: mark.cooper@monash.edu
Nikolaus Marx, Email: nmarx@ukaachen.de.
Michael J. Pencina, Email: michal.pencina@duke.edu
Robert D. Toto, Email: Robert.Toto@UTSouthwestern.edu
Christoph Wanner, Email: Wanner_C@ukw.de.
Bernard Zinman, Email: zinman@lunenfeld.ca.
David Baanstra, Email: david.baanstra@boehringer-ingelheim.com.
Egon Pfarr, Email: egon.pfarr@boehringer-ingelheim.com.
Michaela Mattheus, Email: michaela.mattheus@outlook.de.
Uli C. Broedl, Email: uli.broedl@boehringer-ingelheim.com
Hans-Juergen Woerle, Email: j.woerle@me.com.
Jyothis T. George, Email: jyothis.george@boehringer-ingelheim.com
Maximilian von Eynatten, Email: maximilian.von_eynatten@boehringer-ingelheim.com.
Darren K. McGuire, Email: Darren.McGuire@UTSouthwestern.edu
References
- 1.Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med. 2007;356(24):2457–2471. doi: 10.1056/NEJMoa072761. [DOI] [PubMed] [Google Scholar]
- 2.Nissen SE, Wolski K, Topol EJ. Effect of muraglitazar on death and major adverse cardiovascular events in patients with type 2 diabetes mellitus. JAMA. 2005;294(20):2581–2586. doi: 10.1001/jama.294.20.joc50147. [DOI] [PubMed] [Google Scholar]
- 3.Center for Drug Evaluation and Research. Guidance for industry. Diabetes mellitus—evaluating cardiovascular risk in new antidiabetic therapies to treat type 2 diabetes. Silver Spring, MD, U.S. Food and Drug Administration; 2008. http://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm071627.pdf. Accessed 10 July 2017.
- 4.Committee for Medicinal Products for Human Use (CHMP). Guideline on clinical investigation of medicinal products in the treatment or prevention of diabetes mellitus. London. European Medicines Agency; 2012. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2012/06/WC500129256.pdf. Accessed 10 July 2017.
- 5.Smith RJ, Goldfine AB, Hiatt WR. Evaluating the cardiovascular safety of new medications for type 2 diabetes: time to reassess? Diabetes Care. 2016;39(5):738–742. doi: 10.2337/dc15-2237. [DOI] [PubMed] [Google Scholar]
- 6.Scirica BM, Bhatt DL, Braunwald E, Steg PG, Davidson J, Hirshberg B, Ohman P, Frederich R, Wiviott SD, Hoffman EB, et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med. 2013;369(14):1317–1326. doi: 10.1056/NEJMoa1307684. [DOI] [PubMed] [Google Scholar]
- 7.White WB, Cannon CP, Heller SR, Nissen SE, Bergenstal RM, Bakris GL, Perez AT, Fleck PR, Mehta CR, Kupfer S, et al. Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N Engl J Med. 2013;369(14):1327–1335. doi: 10.1056/NEJMoa1305889. [DOI] [PubMed] [Google Scholar]
- 8.Green JB, Bethel MA, Armstrong PW, Buse JB, Engel SS, Garg J, Josse R, Kaufman KD, Koglin J, Korn S, et al. Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015;373(3):232–242. doi: 10.1056/NEJMoa1501352. [DOI] [PubMed] [Google Scholar]
- 9.Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–2128. doi: 10.1056/NEJMoa1504720. [DOI] [PubMed] [Google Scholar]
- 10.Pfeffer MA, Claggett B, Diaz R, Dickstein K, Gerstein HC, Kober LV, Lawson FC, Ping L, Wei X, Lewis EF, et al. Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. N Engl J Med. 2015;373(23):2247–2257. doi: 10.1056/NEJMoa1509225. [DOI] [PubMed] [Google Scholar]
- 11.Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JF, Nauck MA, Nissen SE, Pocock S, Poulter NR, Ravn LS, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375(4):311–322. doi: 10.1056/NEJMoa1603827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jodar E, Leiter LA, Lingvay I, Rosenstock J, Seufert J, Warren ML, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375(19):1834–1844. doi: 10.1056/NEJMoa1607141. [DOI] [PubMed] [Google Scholar]
- 13.Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, Shaw W, Law G, Desai M, Matthews DR. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–657. doi: 10.1056/NEJMoa1611925. [DOI] [PubMed] [Google Scholar]
- 14.Marso SP, McGuire DK, Zinman B, Poulter NR, Emerson SS, Pieber TR, Pratley RE, Haahr PM, Lange M, Brown-Frandsen K, et al. Efficacy and safety of degludec versus glargine in type 2 diabetes. N Engl J Med. 2017;377(8):723–732. doi: 10.1056/NEJMoa1615692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Holman RR, Bethel MA, Mentz RJ, Thompson VP, Lokhnygina Y, Buse JB, Chan JC, Choi J, Gustavson SM, Iqbal N, et al. Effects of once-weekly exenatide on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2017;377(13):1228–1239. doi: 10.1056/NEJMoa1612917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vaccaro O, Masulli M, Nicolucci A, Bonora E, Del Prato S, Maggioni AP, Rivellese AA, Squatrito S, Giorda CB, Sesti G, et al. Effects on the incidence of cardiovascular events of the addition of pioglitazone versus sulfonylureas in patients with type 2 diabetes inadequately controlled with metformin (TOSCAIT): a randomised, multicentre trial. Lancet Diabetes Endocrinol. 2017;5(11):887–897. doi: 10.1016/S2213-8587(17)30317-0. [DOI] [PubMed] [Google Scholar]
- 17.Thomas MC, Cooper ME, Zimmet P. Changing epidemiology of type 2 diabetes mellitus and associated chronic kidney disease. Nat Rev Nephrol. 2016;12(2):73–81. doi: 10.1038/nrneph.2015.173. [DOI] [PubMed] [Google Scholar]
- 18.Gansevoort RT, Correa-Rotter R, Hemmelgarn BR, Jafar TH, Heerspink HJ, Mann JF, Matsushita K, Wen CP. Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet. 2013;382(9889):339–352. doi: 10.1016/S0140-6736(13)60595-4. [DOI] [PubMed] [Google Scholar]
- 19.Levin A, Tonelli M, Bonventre J, Coresh J, Donner JA, Fogo AB, Fox CS, Gansevoort RT, Heerspink HJL, Jardine M, et al. Global kidney health 2017 and beyond: a roadmap for closing gaps in care, research, and policy. Lancet. 2017;390(10105):1888–1917. doi: 10.1016/S0140-6736(17)30788-2. [DOI] [PubMed] [Google Scholar]
- 20.Baigent C, Herrington WG, Coresh J, Landray MJ, Levin A, Perkovic V, Pfeffer MA, Rossing P, Walsh M, Wanner C, et al. Challenges in conducting clinical trials in nephrology: conclusions from a Kidney Disease-Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2017;92(2):297–305. doi: 10.1016/j.kint.2017.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Afkarian M, et al. Kidney disease and increased mortality risk in type 2 diabetes. J Am Soc Nephrol. 2013;24:302–308. doi: 10.1681/ASN.2012070718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cahn A, Cernea S, Raz I. An update on DPP-4 inhibitors in the management of type 2 diabetes. Expert Opin Emerg Drugs. 2016;21(4):409–419. doi: 10.1080/14728214.2016.1257608. [DOI] [PubMed] [Google Scholar]
- 23.Zannad F, Cannon CP, Cushman WC, Bakris GL, Menon V, Perez AT, Fleck PR, Mehta CR, Kupfer S, Wilson C, et al. Heart failure and mortality outcomes in patients with type 2 diabetes taking alogliptin versus placebo in EXAMINE: a multicentre, randomised, double-blind trial. Lancet. 2015;385(9982):2067–2076. doi: 10.1016/S0140-6736(14)62225-X. [DOI] [PubMed] [Google Scholar]
- 24.McGuire DK, Van de Werf F, Armstrong PW, Standl E, Koglin J, Green JB, Bethel MA, Cornel JH, Lopes RD, Halvorsen S, et al. Association between sitagliptin use and heart failure hospitalization and related outcomes in type 2 diabetes mellitus: secondary analysis of a randomized clinical trial. JAMA Cardiol. 2016;1(2):126–135. doi: 10.1001/jamacardio.2016.0103. [DOI] [PubMed] [Google Scholar]
- 25.Blech S, Ludwig-Schwellinger E, Grafe-Mody EU, Withopf B, Wagner K. The metabolism and disposition of the oral dipeptidyl peptidase-4 inhibitor, linagliptin, in humans. Drug Metab Dispos. 2010;38(4):667–678. doi: 10.1124/dmd.109.031476. [DOI] [PubMed] [Google Scholar]
- 26.Graefe-Mody U, Friedrich C, Port A, Ring A, Retlich S, Heise T, Halabi A, Woerle HJ. Effect of renal impairment on the pharmacokinetics of the dipeptidyl peptidase-4 inhibitor linagliptin(*) Diabetes Obes Metab. 2011;13(10):939–946. doi: 10.1111/j.1463-1326.2011.01458.x. [DOI] [PubMed] [Google Scholar]
- 27.Rosenstock J, Marx N, Neubacher D, Seck T, Patel S, Woerle HJ, Johansen OE. Cardiovascular safety of linagliptin in type 2 diabetes: a comprehensive patient-level pooled analysis of prospectively adjudicated cardiovascular events. Cardiovasc Diabetol. 2015;14:57. doi: 10.1186/s12933-015-0215-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cooper ME, Perkovic V, McGill JB, Groop PH, Wanner C, Rosenstock J, Hehnke U, Woerle HJ, von Eynatten M. Kidney disease end points in a pooled analysis of individual patient-level data from a large clinical trials program of the dipeptidyl peptidase 4 inhibitor linagliptin in type 2 diabetes. Am J Kidney Dis. 2015;66(3):441–449. doi: 10.1053/j.ajkd.2015.03.024. [DOI] [PubMed] [Google Scholar]
- 29.Marx N, McGuire DK, Perkovic V, Woerle HJ, Broedl UC, von Eynatten M, George JT, Rosenstock J. Composite primary end points in cardiovascular outcomes trials involving type 2 diabetes patients: should unstable angina be included in the primary end point? Diabetes Care. 2017;40(9):1144–1151. doi: 10.2337/dc17-0068. [DOI] [PubMed] [Google Scholar]
- 30.Center for Drug Evaluation and Research. Meeting expectations to exclude a CV risk margin of 1.3. In: Application number: 204042Orig1s000 summary review. 2013, p. 20. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2013/204042Orig1s000SumR.pdf. Accessed 24 Oct 2017.
- 31.Levey AS, Inker LA, Matsushita K, Greene T, Willis K, Lewis E, de Zeeuw D, Cheung AK, Coresh J. GFR decline as an end point for clinical trials in CKD: a scientific workshop sponsored by the National Kidney Foundation and the US Food and Drug Administration. Am J Kidney Dis. 2014;64(6):821–835. doi: 10.1053/j.ajkd.2014.07.030. [DOI] [PubMed] [Google Scholar]
- 32.Thompson A, Lawrence J, Stockbridge N. GFR decline as an end point in trials of CKD: a viewpoint from the FDA. Am J Kidney Dis. 2014;64(6):836–837. doi: 10.1053/j.ajkd.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 33.Mol PG, Maciulaitis R, Vetter T. GFR decline as an end point for clinical trials in CKD: a view from Europe. Am J Kidney Dis. 2014;64(6):838–840. doi: 10.1053/j.ajkd.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 34.SI Conversion Calculator. American medical association manual of style: a guide for authors and editors. 10th ed. Oxford: Oxford UP. http://www.amamanualofstyle.com/page/si-conversion-calculator. Accessed 22 Jan 2018.
- 35.Levey AS, de Jong PE, Coresh J, El Nahas M, Astor BC, Matsushita K, Gansevoort RT, Kasiske BL, Eckardt KU. The definition, classification, and prognosis of chronic kidney disease: a KDIGO controversies conference report. Kidney Int. 2011;80(1):17–28. doi: 10.1038/ki.2010.483. [DOI] [PubMed] [Google Scholar]
- 36.Jax T, Stirban A, Terjung A, Esmaeili H, Berk A, Thiemann S, Chilton R, von Eynatten M, Marx N. A randomised, active- and placebo-controlled, three-period crossover trial to investigate short-term effects of the dipeptidyl peptidase-4 inhibitor linagliptin on macro- and microvascular endothelial function in type 2 diabetes. Cardiovasc Diabetol. 2017;16(1):13. doi: 10.1186/s12933-016-0493-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baltzis D, Dushay JR, Loader J, Wu J, Greenman RL, Roustit M, Veves A. Effect of linagliptin on vascular function: a randomized, placebo-controlled study. J Clin Endocrinol Metab. 2016;101(11):4205–4213. doi: 10.1210/jc.2016-2655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.de Boer SA, Heerspink HJ, Lefrandt JD, Hovinga-de Boer MC, van Roon AM, Juarez Orozco LE, Glaudemans AW, Kamphuisen PW, Slart RH, Mulder DJ. Effect of linagliptin on arterial (18)F-fluorodeoxyglucose positron emission tomography uptake: a randomized controlled trial (RELEASE) J Am Coll Cardiol. 2017;69(8):1097–1098. doi: 10.1016/j.jacc.2016.12.018. [DOI] [PubMed] [Google Scholar]
- 39.de Boer SA, Heerspink HJL, Juarez Orozco LE, van Roon AM, Kamphuisen PW, Smit AJ, Slart R, Lefrandt JD, Mulder DJ. Effect of linagliptin on pulse wave velocity in early type 2 diabetes: a randomized, double-blind, controlled 26-week trial (RELEASE) Diabetes Obes Metab. 2017;19(8):1147–1154. doi: 10.1111/dom.12925. [DOI] [PubMed] [Google Scholar]
- 40.Ou HT, Chang KC, Li CY, Wu JS. Risks of cardiovascular diseases associated with dipeptidyl peptidase-4 inhibitors and other antidiabetic drugs in patients with type 2 diabetes: a nation-wide longitudinal study. Cardiovasc Diabetol. 2016;15:41. doi: 10.1186/s12933-016-0350-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim YG, Yoon D, Park S, Han SJ, Kim DJ, Lee KW, Park RW, Kim HJ. Dipeptidyl peptidase-4 inhibitors and risk of heart failure in patients with type 2 diabetes mellitus: a population-based cohort study. Circ Heart Fail. 2017;10(9):e003957. doi: 10.1161/CIRCHEARTFAILURE.117.003957. [DOI] [PubMed] [Google Scholar]
- 42.Marx N, Rosenstock J, Kahn SE, Zinman B, Kastelein JJ, Lachin JM, Espeland MA, Bluhmki E, Mattheus M, Ryckaert B, et al. Design and baseline characteristics of the CARdiovascular Outcome Trial of LINAgliptin Versus Glimepiride in Type 2 Diabetes (CAROLINA(R)) Diab Vasc Dis Res. 2015;12(3):164–174. doi: 10.1177/1479164115570301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Neal B, Perkovic V, Matthews DR, Mahaffey KW, Fulcher G, Meininger G, Erondu N, Desai M, Shaw W, Vercruysse F, et al. Rationale, design and baseline characteristics of the CANagliflozin cardioVascular Assessment Study-Renal (CANVAS-R): a randomized, placebo-controlled trial. Diabetes Obes Metab. 2017;19(3):387–393. doi: 10.1111/dom.12829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Neal B, Perkovic V, de Zeeuw D, Mahaffey KW, Fulcher G, Stein P, Desai M, Shaw W, Jiang J, Vercruysse F, et al. Rationale, design, and baseline characteristics of the Canagliflozin Cardiovascular Assessment Study (CANVAS)—a randomized placebo-controlled trial. Am Heart J. 2013;166(2):217–223. doi: 10.1016/j.ahj.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 45.Wanner C. EMPA-REG OUTCOME: the nephrologist’s point of view. Am J Cardiol. 2017;120(1S):S59–S67. doi: 10.1016/j.amjcard.2017.05.012. [DOI] [PubMed] [Google Scholar]
- 46.Shi S, Koya D, Kanasaki K. Dipeptidyl peptidase-4 and kidney fibrosis in diabetes. Fibrogenesis Tissue Repair. 2016;9:1. doi: 10.1186/s13069-016-0038-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Groop PH, Cooper ME, Perkovic V, Emser A, Woerle HJ, von Eynatten M. Linagliptin lowers albuminuria on top of recommended standard treatment in patients with type 2 diabetes and renal dysfunction. Diabetes Care. 2013;36(11):3460–3468. doi: 10.2337/dc13-0323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cornel JH, Bakris GL, Stevens SR, Alvarsson M, Bax WA, Chuang LM, Engel SS, Lopes RD, McGuire DK, Riefflin A, et al. Effect of sitagliptin on kidney function and respective cardiovascular outcomes in type 2 diabetes: outcomes from TECOS. Diabetes Care. 2016;39(12):2304–2310. doi: 10.2337/dc16-1415. [DOI] [PubMed] [Google Scholar]
- 49.Mosenzon O, Leibowitz G, Bhatt DL, Cahn A, Hirshberg B, Wei C, Im K, Rozenberg A, Yanuv I, Stahre C, et al. Effect of saxagliptin on renal outcomes in the SAVOR-TIMI 53 trial. Diabetes Care. 2017;40(1):69–76. doi: 10.2337/dc16-0621. [DOI] [PubMed] [Google Scholar]
- 50.Groop PH, Cooper ME, Perkovic V, Hocher B, Kanasaki K, Haneda M, Schernthaner G, Sharma K, Stanton RC, Toto R, et al. Linagliptin and its effects on hyperglycaemia and albuminuria in patients with type 2 diabetes and renal dysfunction: the randomized MARLINA-T2D trial. Diabetes Obes Metab. 2017;19(11):1610–1619. doi: 10.1111/dom.13041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tsuprykov O, Ando R, Reichetzeder C, von Websky K, Antonenko V, Sharkovska Y, Chaykovska L, Rahnenfuhrer J, Hasan AA, Tammen H, et al. The dipeptidyl peptidase inhibitor linagliptin and the angiotensin II receptor blocker telmisartan show renal benefit by different pathways in rats with 5/6 nephrectomy. Kidney Int. 2016;89(5):1049–1061. doi: 10.1016/j.kint.2016.01.016. [DOI] [PubMed] [Google Scholar]
- 52.Gangadharan Komala M, Gross S, Zaky A, Pollock C, Panchapakesan U. Linagliptin limits high glucose induced conversion of latent to active TGFss through interaction with CIM6PR and limits renal tubulointerstitial fibronectin. PLoS ONE. 2015;10(10):e0141143. doi: 10.1371/journal.pone.0141143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shi S, Srivastava SP, Kanasaki M, He J, Kitada M, Nagai T, Nitta K, Takagi S, Kanasaki K, Koya D. Interactions of DPP-4 and integrin beta1 influences endothelial-to-mesenchymal transition. Kidney Int. 2015;88(3):479–489. doi: 10.1038/ki.2015.103. [DOI] [PubMed] [Google Scholar]
- 54.Kanasaki K, Shi S, Kanasaki M, He J, Nagai T, Nakamura Y, Ishigaki Y, Kitada M, Srivastava SP, Koya D. Linagliptin-mediated DPP-4 inhibition ameliorates kidney fibrosis in streptozotocin-induced diabetic mice by inhibiting endothelial-to-mesenchymal transition in a therapeutic regimen. Diabetes. 2014;63(6):2120–2131. doi: 10.2337/db13-1029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Full inclusion and exclusion criteria for CARMELINA®.
Additional file 2. Baseline characteristics by established CV disease at baseline in CARMELINA® participants.
Additional file 3. Baseline characteristics by established CV disease and prevalent kidney disease at baseline in CARMELINA® participants.
Additional file 4. CARMELINA® baseline characteristics versus TECOS and SAVOR-TIMI 53.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.


