Abstract
Untreated cavities can have far-reaching negative consequences for people’s ability to eat, speak, and learn. By adolescence, 27 percent of low-income children in the United States will have untreated cavities. School-based sealant programs typically provide dental sealants (a protective coating that adheres to the surface of molars) at little or no cost to students attending schools in areas with low socioeconomic status. These programs have been shown to increase the number of students receiving sealants and to prevent cavities. We analyzed the cost-effectiveness of school sealant programs using data (from school programs in fourteen states between 2013 and 2014) on children’s cavity risk, including the effects of untreated cavities on a child’s quality of life. We found that providing sealants in school programs to 1,000 children would prevent 485 fillings and 1.59 disability-adjusted life-years. School-based sealant programs saved society money and remained cost-effective across a wide range of reasonable values.
Almost 27 percent of US children living in poverty have untreated cavities.1 If left untreated, cavities can lead to pain; infection; and problems with eating, speaking, and learning.2 Recent evidence continues to show that children with unmet dental needs miss more school days and have lower grades than children with no unmet needs.3–5 About 90 percent of cavities in children’s permanent teeth occur on the chewing surfaces of molars (posterior teeth),6 where dental sealants are commonly applied.
Dental sealants are coatings applied to the chewing surfaces of molars to prevent cavities. Increasing the prevalence of sealants is a national health goal,7 and performance measures endorsed by the National Quality Forum aim to increase this prevalence among children at high risk for cavities.8 Sealants prevent 81 percent of potential cavities two years after placement, and despite evidence that they remain protective at nine years after placement,9 they are not used enough among low-income children.10 Recent national data indicate that only 38 percent of that population receive sealants, compared to 47 percent of higher-income children.11
When sealants are applied in schools attended by low-income children, more children at high risk for cavities receive the preventive treatment. School sealant programs typically use portable dental equipment to deliver sealants in schools at little or no cost to students.12 The Community Preventive Services Task Force recommends these programs based on strong evidence of sealants’ effectiveness and because the programs increase the prevalence of sealants among schoolchildren.12 The task force is an independent, unpaid, nonfederal panel of public health and prevention experts; their recommendations for use of community preventive services, programs, and policies are based on systematic reviews to determine program effectiveness. Although it has recommended school-based sealant programs since 2002,13 many eligible US schools still have no program. In 2013 only fifteen states had programs in more than half of schools where most students participated in the free/reduced-cost meal program—the indicator used to identify low-income populations of children.14
After the task force determines that a program is effective, a systematic review of economic viability is typically conducted. The 2015 economic review included four economic models15–18 of school-based sealant programs’ cost-effectiveness, where cost-effectiveness was defined as the ratio of net cost to gained health or quality of life. Net costs equaled program costs minus the averted treatment costs that resulted from fewer cavities. Programs were cost-saving (net cost was negative) in two studies.15,17 Another three studies explored claims data19–21 to see whether sealants provided to Medicaid-enrolled children in any setting were cost-saving: One found cost savings for all children,19 one found cost savings for children with at least two other filled molars,20 and one found no cost savings. None of these studies included the impact of cavities’ remaining untreated in their estimates of averted treatment costs or outcome measures. Because school-based sealant programs typically target children who do not receive regular dental care, it is likely that some cavities will remain untreated and result in toothaches and lower quality of life. We conducted an additional analysis for the task force that included the effect of untreated cavities on school sealant program cost-effectiveness. (That analysis will not be published or posted elsewhere.)
In this article we estimate cavity risk using actual data from children participating in school-based sealant programs. We believe that this is the first analysis to estimate net cost for a school-based program to prevent a disability-adjusted life-year (DALY) through the use of dental sealants. Since DALYs are a measure commonly used to evaluate other interventions to improve children’s health and quality of life, this allows our results to be compared to results for other interventions.
Study Data And Methods
We estimated the net costs and increased quality of life derived from sealing a child’s four permanent first molars. Based on a societal perspective, we modeled a school-based program that targets children for sealant placement soon after the first molars erupt into the mouth (typically between ages six and seven)22 but does not maintain sealants by reapplication. We limited our analysis to four years because the evidence for sealant effectiveness is strongest over that period,9 but we considered a nine-year period in the sensitivity analysis. We assumed that the only permanent teeth at risk for cavities are first molars; thus, measures of annual cavity incidence (the probability that a child will develop a cavity in at least one permanent tooth) and annual cavity increment (the number of teeth with new cavities per child) would include first molars only. We also assumed that the annual first-molar cavity attack rate (the probability that a healthy, permanent first molar develops a cavity) was the same for each first molar and did not change over time. Justification for each of these assumptions is provided in the online Appendix.23
We followed the recent recommendations of the Second Panel on Cost-effectiveness in Health and Medicine24 to calculate the net cost per averted DALY (a year in which normal activities are limited, owing to disease, injury, or disability; DALY values range from 0 [perfect health] to 1 [death]). Net cost—the numerator of the cost-effectiveness ratio—equaled sealant program resource costs minus filling costs and lost productivity that would occur in the absence of sealants. Averted DALYs—the denominator—equaled the number of years a child would have painful untreated cavities multiplied by the associated loss in health or well-being that sealants would prevent.
All costs were reported in 2014 US dollars and converted where necessary with the US city average Consumer Price Index.24 All costs were estimated from the societal perspective and discounted at a 3 percent annual rate. Health outcomes were discounted on the premise that people value good health immediately rather than later.25 All costs and outcomes were estimated per child, not per tooth.
PARAMETERS USED IN THE MODEL
Further details on how each of the parameters described below was derived are provided in the Appendix. Information on the base value, distribution, and data source for all parameters is provided in Exhibits A1–A6 in the Appendix.23
▸ FIRST-MOLAR CAVITY ATTACK RATE
To estimate the annual risk that a sound, unsealed permanent first molar developed a cavity, we used deidentified data for children participating in school-based sealant programs in fourteen states between 2013 and 2014 (see Appendix Exhibit A1).23 These data were collected for program evaluation under Centers for Disease Control and Prevention Cooperative Agreement No. 5U58DP001480-05, with the intent to improve public health practice. Almost all programs served schools where more than half of students participated in the free/reduced-cost meal program (eligibility based on family income of 185 percent or less of the federal poverty level). The annual first-molar cavity attack rate, 0.078, was used to estimate annual cavity incidence and annual cavity increment. Details on the derivation of first-molar cavity attack rate, and on the calculation of cavity incidence and increment per child, are in Appendix I.A.23
Increasing sealant prevalence among low-income children could save society money and decrease toothaches.
▸ PROBABILITY THAT CAVITY REMAINS UNTREATED
We used published estimates of the probability that a child with an urgent dental problem (primarily cavity-related) would not visit the dentist for that problem.26
▸ SCHOOL-SEALANT EFFECTIVENESS
We estimated sealant effectiveness at one, two, three, and four years after placement, and we assumed that sealant effectiveness decreased each year. We adjusted sealant effectiveness for different follow-up times from the 2013 Cochrane Review9 downward such that overall four-year effectiveness would be 50 percent, the same estimate as in the Community Preventive Services Task Force’s systematic effectiveness review.12The percentage reduction in incidence and increment due to sealants was 68.5 percent at one year, 57.9 percent at two years, 40.1 percent at three years, and 25.8 percent at four years. Because a child’s molars might not all be sealant-eligible (a molar may have a cavity, be filled, or not be erupted), we also examined the cost-effectiveness of a scenario where only three first molars were sealed, assuming the cost per child would not decrease. Finally, we estimated cost-effectiveness using a nine-year time horizon and 60 percent effectiveness (consistent with estimated effectiveness from the Cochrane Review).9
▸ PROBABILITY OF TOOTHACHE IN CHILD WITH UNTREATED CAVITY
Using estimates from national survey data on the ratio of the percentage of children ages 6–17 in 2007 with a reported toothache within the past six months (12.0 percent)27 to the percentage of children ages 5–19 in 2005–08 with at least one untreated cavity (16.6 percent),28 we estimated a 0.721 probability that a child with at least one untreated cavity would experience pain.
▸ LOSS IN HEALTH OR WELL-BEING CAUSED BY TOOTHACHE
To measure the loss in health or well-being from having a toothache for one year, we used DALY data from the World Health Organization’s Global Burden of Disease study in 2010, which includes the effect of illness (in this case, toothache from untreated cavities) on lost quality of life.29 This value was 0.012.
▸ SCHOOL-BASED SEALANT PROGRAM RESOURCE COSTS
We used information on resource costs from the four US studies included in the task force’s systematic economic review.18,30–32 For the base model, we excluded two studies; one18 took about twice as long to deliver sealants, and another32 sealed almost three times as many teeth compared to current practice.33 Base-case resource cost per child was $63.33, and when all studies were included in a sensitivity analysis, cost per child was $80.33.
▸ COST PER FILLING
To estimate resource costs needed to fill a tooth, we first used national survey data on the frequency and cost of typical molar fillings.34,35 We multiplied the average cost of $173.98 by the proportion of dental charges typically covered by insurance, using the assumption that insurers could negotiate the competitive price. A filling cost of $139.18 was used in the base analysis, and the average Medicaid fee, $64.17, was used in a sensitivity analysis.
▸ PRODUCTIVITY LOSSES
Productivity losses for a parent taking a child to the dentist for a filling were estimated to be $21.34. We made the conservative assumption that a child with untreated first molar cavities would require one dental visit regardless of how many molars were affected. We estimated net costs (numerator of cost-effectiveness ratio) without productivity losses in a sensitivity analysis.
ANALYSIS
We estimated the cost-effectiveness of school-based sealant programs under base-case assumptions, using the alternative parameter values discussed above. We also examined which model inputs had the largest impact on cost-effectiveness and the impact on our findings from allowing simultaneous variation of both first-molar cavity attack rate and program cost. Finally, we conducted a probabilistic sensitivity analysis (allowing all parameters to vary simultaneously) to estimate 95% confidence intervals for outcomes of interest. Further details are provided in Appendix section I.23
We used two criteria to determine whether a school sealant program offered good value: whether a program was cost-saving (if the net cost was negative) and whether a program was cost-effective (if the net cost per averted DALY was less than the 2014 US gross domestic product per capita, $54,639).
LIMITATIONS
This study had the following limitations. First, our estimates of averted treatment costs and productivity losses were conservative; we limited treatment options to a basic filling and did not include travel costs associated with a dental visit (such as for fuel) or future treatment costs and productivity losses associated with maintaining or replacing a filling. Second, we may have overestimated the loss in quality of life associated with untreated first molar cavities if the impact of these teeth produced no additional discomfort in the presence of other teeth with untreated cavities. Finally, our comparison group was children not receiving sealants, as opposed to children in a school without a sealant program, and thus our analysis did not account for the additional costs and benefits that would occur if some of the schoolchildren had received sealants in a dental office after the program delivered sealants.
Study Results
Under base-case assumptions, net costs were negative: School sealant program costs per child were $8.43 (95%CI: $6.14, $10.72) less than the money they saved in treatment and productivity costs (Exhibit 1). Providing sealants in school programs to 1,000 children would prevent toothaches for a year in 133 children (95%CI: 130, 135), 485 fillings (95%CI: 473, 497), and 1.59 DALYs (95%CI: 1.53, 1.65). Using the higher estimate of school program costs, which included studies inconsistent with current program practices or costs, resulted in positive net costs of $8.57 per child and a net cost per averted DALY of $5,678. If Medicaid fees represented the actual cost of resources to fill a tooth, then net cost per child increased to $27.98, and cost per averted DALY increased to $18,541. If a child had only three first molars eligible for sealants, the net cost per child was $9.17, and cost per averted DALY was $7,293. Using a nine-year effectiveness estimate of 61 percent increased cost savings to $23.22 per child and averted 2.11 DALYs. School sealant programs remained cost-saving even if productivity losses were $0.
EXHIBIT 1.
Net cost per averted DALY per child for different parameter values and assumptions in a school sealant program
| Parameter value used in analysis | Averted treatment and productivity costsa |
Net costa | Averted years with toothachea |
Averted fillingsa |
Averted DALYsb |
Net cost per averted DALY |
|---|---|---|---|---|---|---|
| Base case ($63.33 per child) | $71.76 | −$ 8.43 | 0.133 | 0.485 | 0.002 | —c |
| SSP cost of $80.33 per child | 71.76 | 8.57 | 0.133 | 0.485 | 0.002 | $ 5,678 |
| Cost per filling for Medicaid ($64.17) | 35.35 | 27.98 | 0.133 | 0.485 | 0.002 | 18,541 |
| Sealed 3 teeth rather than 4d | 54.16 | 9.17 | 0.111 | 0.364 | 0.001 | 7,293 |
| Nine-year sealant effectiveness | 86.55 | −23.22 | 0.176 | 0.580 | 0.002 | —c |
| Without productivity losses ($0) | 67.56 | −4.23 | 0.133 | 0.485 | 0.002 | —c |
SOURCE Authors’ analysis of multiple data sources, listed in Appendix Exhibit A6 (see Note 23 in text). NOTES Net cost is program costs minus the averted treatment costs that resulted from fewer cavities. DALY is disability-adjusted life-year. SSP is school sealant program.
Discounted at 3 percent.
Values in text reported per 1000 children differ from value in exhibit due to rounding to 3 decimal points.
Not reported if net cost is negative.
SSP cost per child does not decrease if the program seals only three teeth.
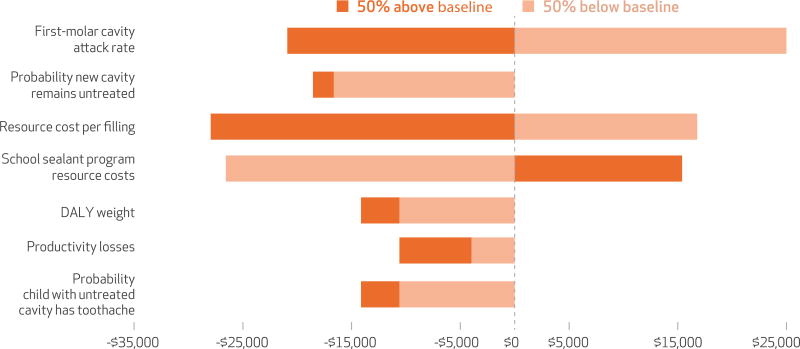
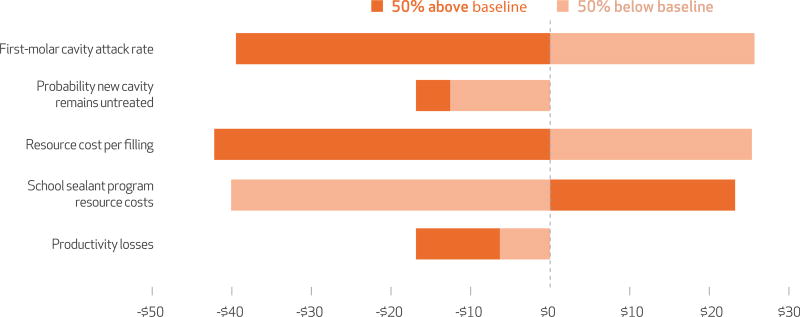
A one-way sensitivity analysis examined the impact of allowing parameters to vary from 50 percent above and 50 percent below their base value. For example, when we varied the first-molar cavity attack rate, the cost per averted DALY ranged from −$20,907 to $27,868, and net cost ranged from −$39 to $26. The parameters with the largest influence on estimated cost-effectiveness (cost per averted DALY) and on net costs were the first-molar cavity attack rate, resource cost per filling, and sealant program resource costs (Exhibits 2 and 3).
EXHIBIT 2. Effect on net cost per averted DALY from varying parameters between 50 percent below and 50 percent above baseline value.
SOURCE Authors’ sensitivity analysis, based on data sources in Appendix Exhibit A6. NOTES Net costs are program costs minus the averted treatment costs that resulted from fewer cavities. DALY is disability-adjusted life-year.
EXHIBIT 3. Effect on net cost from varying parameters between 50 percent below and 50 percent above baseline value.
SOURCE Authors’ sensitivity analysis, based on data sources in Appendix Exhibit A6. NOTE Net costs are program costs minus the averted treatment costs that resulted from fewer cavities.
The two-way sensitivity analysis, which measured how changes in program cost and cavity risk affected changes in cost-effectiveness, indicated that school sealant programs were cost-effective across the full range of school program costs per child if the annual first-molar attack rate was 0.05 or higher (Exhibit 4). If sealant program cost per child was $40 or less, programs were cost-saving when the annual first-molar attack rate was 0.04 or higher, and cost-effective when that probability was 0.02 or higher (Exhibit 4). If program cost per child were $80 or less, the program would be cost-effective when the annual first-molar attack rate was 0.04 or higher.
EXHIBIT 4.
Impact of simultaneously varying school sealant program cost and first-molar cavity attack rate on cost-effectiveness (net cost per averted DALY)
| Annual first-molar cavity attack rate |
School sealant program cost | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| $30 | $40 | $50 | $60 | $70 | $80 | $90 | $100 | $110 | |
| 0.01 | $67,723 | $101,628 | $135,534 | $169,439 | $203,344 | $237,250 | $271,155 | $305,060 | $338,966 |
| 0.02 | $18,345a | $26,237a | $54,272a | $72,235 | $90,199 | $108,162 | $126,126 | $144,089 | $162,053 |
| 0.03 | $890a | $13,563a | $26,237a | $38,910a | $51,584a | $64,257 | $76,931 | $89,604 | $102,278 |
| 0.04 | CS | $1,439a | $11,485a | $21,531a | $31,578a | $41,624a | $51,670a | $61,716 | $71,762 |
| 0.05 | CS | CS | $2,031a | $10,515a | $18,998a | $27,482a | $35,965a | $44,449a | $52,932a |
| 0.06 | CS | CS | CS | $2,666a | $10,119a | $17,572a | $25,025a | $32,478a | $39,931a |
| 0.07 | CS | CS | CS | CS | $3,346a | $10,072a | $16,798a | $23,524a | $30,251a |
| 0.08 | CS | CS | CS | CS | CS | $4,070a | $10,259a | $16,448a | $22,637a |
| 0.09 | CS | CS | CS | CS | CS | CS | $4,841a | $10,619a | $16,397a |
| 0.10 | CS | CS | CS | CS | CS | CS | $203a | $5,658a | $11,113a |
| 0.11 | CS | CS | CS | CS | CS | CS | CS | $1,327a | $6,522a |
| 0.12 | CS | CS | CS | CS | CS | CS | CS | CS | $2,450a |
SOURCE Authors’ probabilistic sensitivity analysis, based on data sources in Appendix Exhibit A6 (see Note 23 in text). NOTES 2014 US gross domestic product per capita was $54,639. Net cost is program costs minus the averted treatment costs that resulted from fewer cavities. CS is cost saving (meaning that net cost is negative). DALY is disability-adjusted life-year.
Cost-effective.
Discussion
We found that under base-case assumptions, school dental sealant programs were cost-saving. Providing sealants in school programs to 1,000 children would prevent toothaches for a year in 133 children and 1.59 DALYs.
For this analysis we used actual data on the first-molar cavity attack rate for children participating in school sealant programs in fourteen states. A recent analysis of National Health and Nutrition Examination Survey (NHANES) data from 2011–14 suggests that the children in our analysis had only a slightly higher first-molar cavity attack rate than the average US child with family income sufficiently low to make children eligible for the free/reduced-cost meal program.11 The analysis of NHANES data found that the mean first-molar cavity increment among children ages 7–11 who had no sealants was 0.82, corresponding to an annual first-molar cavity attack rate of 0.073. The analysis further found that sealant prevalence among these poor children is low; more than 60 percent of children, ages 6–11, had not received the preventive benefits of dental sealants. Increasing sealant prevalence among low-income children could save society money and decrease toothaches and their sequelae.
The economic systematic review we conducted for the Community Preventive Services Task Force located no existing analyses of school sealant programs’ cost-effectiveness. Among the four economic models in the task force review, only one U.S. study included averted treatment costs and productivity losses in net cost calculations.17 That model also found school sealant programs to be cost-saving. In addition, we estimated the median annual benefit of sealants for the task force review from six studies that included economic models of school sealant programs or clinically delivered sealants and analyses of Medicaid claims data. For four of these studies, which were calculated from the payer perspective, we estimated annual productivity losses and added that to the annual benefit. Based on the findings of those six studies, the task force reported that the median annual benefit of sealing a tooth was $6.29.36 The corresponding value in our analysis was $4.82 (annualized, per tooth estimate of averted treatment and productivity costs per child). The higher benefit in the Task Force review was likely attributable to studies having higher annual first-molar cavity attack rates (range: 4.9 percent, 13.2 percent; mean: 8.9 percent).
Estimated school sealant resource costs per child used in our analysis were also conservative. The task force review estimated school sealant program resource costs both per tooth and per child. For this analysis we used findings on resource cost per child for US studies because data on cost per tooth were available for only three US programs compared to nine for cost per child. As a result, our cost per child, $63.33, was higher than the cost of $46.66 if the cost per tooth, $11.64, in the task force review were multiplied by 4.
The task force effectiveness review12 also noted that for many children, school-based sealant programs may increase access to restorative dental services through early identification of cavities and referral of children to needed dental services. Baseline screening data from school sealant programs in the fourteen states included in this analysis suggest that, compared to the general child population, school-based programs are indeed serving children who are not only at high risk for cavities but who are also unlikely to use clinical dental services; 33 percent of participating children had at least one cavity needing treatment in a permanent or primary tooth. This value is about 60 percent higher than the national average of 20 percent.37 In the absence of access to restorative care, prevention becomes even more critical to long-term dental health.
A recent survey of state oral health programs found that although a steady stream of financing was critical to the sustainability of school sealant programs, a variety of financing approaches were used.38 Both the Health Resources and Services Administration and the Centers for Disease Control and Prevention fund school sealant programs through competitive grants or cooperative agreements, and almost all sealant programs bill Medicaid for services delivered to enrolled children. Some programs can exist almost solely on Medicaid billing if reimbursements cover their costs.38
The systematic review of economic evaluations of school sealant programs undertaken for the Community Preventive Services Task Force found wide variation in reported cost per program.12 Because labor accounts for about two-thirds of program costs,12 reducing labor time per child or cost per labor unit would lower program costs. State policies can determine which category of licensed dental professionals (dentists, hygienists, or therapists) can place sealants and assess a child’s need for sealants. Programs in states that require a dentist to be present during at least one of these activities have higher hourly labor costs and also may use more labor time per child. For example, when a dentist is required only for assessment, children may be called back for sealant placement by other dental professionals. Although this approach minimizes the dentist’s time on site, assessing and placing sealants in more than one visit results in higher costs for infection control and labor. One study found that this extra step increased costs by 18–29 percent depending on program size.17
Under almost all tested scenarios, school-based sealant programs met the cost-effectiveness threshold.
Children must return a signed consent form to receive sealants from a school program. Thus, low consent rates could pose a potential barrier to low-income children’s receipt of sealants. A focus group of dental directors and managers of oral health programs from federally qualified health centers that provide dental services in schools noted that some of their programs had low participation (below 50 percent) because of failure to return consent forms.39 Low consent rates may be associated with low oral health literacy. Studies indicate that low sealant prevalence is associated with low health literacy40 or low parental education, a predictor of health literacy.41 Policies aimed at increasing oral health literacy among low-income caregivers could increase the number of high-risk children receiving sealants. School staff and teachers, who can also influence children’s participation in sealant programs, may also be unaware of the benefits of sealants. A telephone survey of consumers in 2009 found that over half of respondents could not correctly identify the purpose of dental sealants.42
Conclusion
We found that under almost all tested scenarios, school-based sealant programs met the cost-effectiveness threshold. Threshold values, though widely used, have been criticized because, on their own, they do not provide sufficient information to rank the relative values of local interventions.42 For a community, the best combination of health interventions will depend on local conditions, including prevalence of various diseases/conditions and the relative costs and benefits of implementing different interventions. Combining the threshold with our sensitivity analyses provides decision makers with useful information with which to compare investing in school-based sealant programs to other competing alternatives.
Supplementary Material
Acknowledgments
The authors thank Barbara Gooch for her review and suggestions for this article. The findings and conclusions in this report are the work of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Contributor Information
Susan Griffin, Division of Oral Health, Centers for Disease Control and Prevention (CDC), in Atlanta, Georgia.
Shillpa Naavaal, Virginia Commonwealth University, in Richmond.
Christina Scherrer, Department of Systems and Industrial Engineering at Kennesaw State University, in Georgia.
Paul M. Griffin, School of Industrial and Systems Engineering, Georgia Institute of Technology, in Atlanta.
Kate Harris, Center for Surveillance, Epidemiology, and Laboratory Services at the CDC.
Sajal Chattopadhyay, Center for Surveillance, Epidemiology, and Laboratory Services at the CDC.
NOTES
- 1.Dye BA, Tan S, Smith V, Lewis BG, Barker LK, Thornton-Evans G, et al. Trends in oral health status: United States, 1988–1994 and 1999–2004. Vital Health Stat 11. 2007;(248):1–92. [PubMed] [Google Scholar]
- 2.Department of Health and Human Services. Oral health in America: a report of the surgeon general. Rockville (MD): DHHS; 2000. [Google Scholar]
- 3.Agaku IT, Olutola BG, Adisa AO, Obadan EM, Vardavas CI. Association between unmet dental needs and school absenteeism because of illness or injury among U.S. school children and adolescents aged 6–17 years, 2011–2012. Prev Med. 2015;72:83–8. doi: 10.1016/j.ypmed.2014.12.037. [DOI] [PubMed] [Google Scholar]
- 4.Seirawan H, Faust S, Mulligan R. The impact of oral health on the academic performance of disadvantaged children. Am J Public Health. 2012;102(9):1729–34. doi: 10.2105/AJPH.2011.300478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jackson SL, Vann WF, Jr, Kotch JB, Pahel BT, Lee JY. Impact of poor oral health on children’s school attendance and performance. Am J Public Health. 2011;101(10):1900–6. doi: 10.2105/AJPH.2010.200915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gooch BF, Griffin SO, Gray SK, Kohn WG, Rozier RG, Siegal M, et al. Preventing dental caries through school-based sealant programs: updated recommendations and reviews of evidence. J Am Dent Assoc. 2009;140(11):1356–65. doi: 10.14219/jada.archive.2009.0070. [DOI] [PubMed] [Google Scholar]
- 7.HealthyPeople.gov. Topics and objectives: oral health [Internet] Washington (DC): Department of Health and Human Services; [cited 2016 Oct 31]. Available from: http://www.healthypeople.gov/2020/topics-objectives/topic/oral-health. [Google Scholar]
- 8.National Quality Forum. Oral health performance measurement: environmental scan, gap analysis, and measure topics prioritization—technical report. Washington (DC): NQF; 2012. [Google Scholar]
- 9.Ahovuo-Saloranta A, Forss H, Walsh T, Hiiri A, Nordblad A, Makela M, et al. Sealants for preventing dental decay in the permanent teeth. Cochrane Database Syst Rev. 2013;3 doi: 10.1002/14651858.CD001830.pub4. CD001830. [DOI] [PubMed] [Google Scholar]
- 10.Beauchamp J, Caufield PW, Crall JJ, Donly K, Feigal R, Gooch B, et al. Evidence-based clinical recommendations for the use of pit-and-fissure sealants: a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2008;139(3):257–68. doi: 10.14219/jada.archive.2008.0155. [DOI] [PubMed] [Google Scholar]
- 11.Griffin SO, Wei L, Gooch BF. Changes in dental sealant and untreated tooth decay prevalence and the estimated impact of increasing school-based sealant program coverage. MMWR Morb Mortal Wkly Rep. 2016 doi: 10.15585/mmwr.mm6541e1. Forthcoming. [DOI] [PubMed] [Google Scholar]
- 12.Community Guide. Dental caries (cavities): school-based dental sealant delivery programs [Internet] Atlanta (GA): Community Preventive Services Task Force; [cited 2016 Oct 31]. Available from: https://www.thecommunityguide.org/findings/dental-caries-cavities-school-based-dental-sealant-delivery-programs. [Google Scholar]
- 13.Truman BI, Gooch BF, Sulemana I, Gift HC, Horowitz AM, Evans CA, et al. Reviews of evidence on interventions to prevent dental caries, oral and pharyngeal cancers, and sports-related craniofacial injuries. Am J Prev Med. 2002;23(1 Suppl):21–54. doi: 10.1016/s0749-3797(02)00449-x. [DOI] [PubMed] [Google Scholar]
- 14.Pew Center on the States. Falling short: most states lag on dental sealants [Internet] Washington (DC): The Center; 2013. Jan, [cited 2016 Oct 31]. Available from: http://www.pewtrusts.org/~/media/legacy/uploadedfiles/pcs_assets/2013/Pewdentalsealantsreportpdf.pdf. [Google Scholar]
- 15.Bertrand E, Mallis M, Bui NM, Reinharz D. Cost-effectiveness simulation of a universal publicly funded sealants application program. J Public Health Dent. 2011;71(1):38–45. doi: 10.1111/j.1752-7325.2010.00200.x. [DOI] [PubMed] [Google Scholar]
- 16.Marino R, Fajardo J, Morgan M. Cost-effectiveness models for dental caries prevention programmes among Chilean schoolchildren. Community Dent Health. 2012;29(4):302–8. [PubMed] [Google Scholar]
- 17.Scherrer CR, Griffin PM, Swann JL. Public health sealant delivery programs: optimal delivery and the cost of practice acts. Med Decis Making. 2007;27(6):762–71. doi: 10.1177/0272989X07302134. [DOI] [PubMed] [Google Scholar]
- 18.Werner CW, Pereira AC, Eklund SA. Cost-effectiveness study of a school-based sealant program. ASDC J Dent Child. 2000;67(2):93–7. 82. [PubMed] [Google Scholar]
- 19.Dasanayake AP, Li Y, Kirk K, Bronstein J, Childers NK. Restorative cost savings related to dental sealants in Alabama Medicaid children. Pediatr Dent. 2003;25(6):572–6. [PubMed] [Google Scholar]
- 20.Weintraub JA, Stearns SC, Rozier RG, Huang CC. Treatment outcomes and costs of dental sealants among children enrolled in Medicaid. Am J Public Health. 2001;91(11):1877–81. doi: 10.2105/ajph.91.11.1877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bhuridej P, Kuthy RA, Flach SD, Heller KE, Dawson DV, Kanellis MJ, et al. Four-year cost-utility analyses of sealed and nonsealed first permanent molars in Iowa Medicaid-enrolled children. J Public Health Dent. 2007;67(4):191–8. doi: 10.1111/j.1752-7325.2007.00025.x. [DOI] [PubMed] [Google Scholar]
- 22.For the dental patient. Tooth eruption: the permanent teeth. J Am Dent Assoc. 2006;137(1):127. doi: 10.14219/jada.archive.2006.0031. [DOI] [PubMed] [Google Scholar]
- 23.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 24.Bureau of Labor Statistics. Databases, tables, and calculators by subject: inflation and prices [Internet] Washington (DC): BLS; [cited 2016 Oct 31]. Available from: http://www.bls.gov/data/#prices. [Google Scholar]
- 25.Sanders GD, Neumann PJ, Basu A, Brock DW, Feeny D, Krahn M, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: Second Panel on Cost-Effectiveness in Health and Medicine. JAMA. 2016;316(10):1093–103. doi: 10.1001/jama.2016.12195. [DOI] [PubMed] [Google Scholar]
- 26.Naavaal S, Barker LK, Griffin SO. The effect of health and dental insurance on US children’s dental care utilization for urgent and non-urgent dental problems—2008. J Public Health Dent. 2016 Sep 10; doi: 10.1111/jphd.12171. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lewis C, Stout J. Toothache in US children. Arch Pediatr Adolesc Med. 2010;164(11):1059–63. doi: 10.1001/archpediatrics.2010.206. [DOI] [PubMed] [Google Scholar]
- 28.Dye BA, Li X, Beltran-Aguilar ED. Selected oral health indicators in the United States, 2005–2008. NCHS Data Brief. 2012;(96):1–8. [PubMed] [Google Scholar]
- 29.Marcenes W, Kassebaum NJ, Bernabe E, Flaxman A, Naghavi M, Lopez A, et al. Global burden of oral conditions in 1990–2010: a systematic analysis. J Dent Res. 2013;92(7):592–7. doi: 10.1177/0022034513490168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Calderone JJ, Mueller LA. The cost of sealant application in a state dental disease prevention program. J Public Health Dent. 1983;43(3):249–54. doi: 10.1111/j.1752-7325.1983.tb01916.x. [DOI] [PubMed] [Google Scholar]
- 31.Garcia AI. Caries incidence and costs of prevention programs. J Public Health Dent. 1989;49(5 Spec No):259–71. doi: 10.1111/j.1752-7325.1989.tb02084.x. [DOI] [PubMed] [Google Scholar]
- 32.Klein SP, Bohannan HM, Bell RM, Disney JA, Foch CB, Graves RC. The cost and effectiveness of school-based preventive dental care. Am J Public Health. 1985;75(4):382–91. doi: 10.2105/ajph.75.4.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Association of State and Territorial Dental Directors. Best practice approach: school-based dental sealant programs [Internet] Reno (NV): ASTDD; [originally published 2003 Jun 16; updated 2015 Mar]. Available from: http://www.astdd.org/docs/bpar-selants-update-03-2015.pdf. [Google Scholar]
- 34.American Dental Association. 2000 Survey of Dental Practice. Chicago (IL): ADA; 2002. [Google Scholar]
- 35.American Dental Association. Dental fees: results from the 2013 Survey of Dental Fees. Chicago (IL): ADA; 2014. [Google Scholar]
- 36.Griffin SO, Naavaal S, Scherrer CR, Patel M, Chattopadhyay S. Evaluation of school-based dental sealant programs: an updated Community Guide Systematic Economic Review. Am J Prev Med. 2016 doi: 10.1016/j.amepre.2016.10.004. Forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dye BA, Thornton-Evans G, Li X, Iafolla TJ. Dental caries and sealant prevalence in children and adolescents in the United States, 2011–2012. NCHS Data Brief. 2015;(191):1–8. [PubMed] [Google Scholar]
- 38.Children’s Dental Health Project. Dental sealants: proven to prevent tooth decay: a look at issues impacting the delivery of state and local school-based sealant programs [Internet] Washington (DC): CDHP; 2014. May, [cited 2016 Oct 31]. Available for download from: https://www.cdhp.org/resources/314-dental-sealants-proven-to-prevent-tooth-decay. [Google Scholar]
- 39.National Network for Oral Health Access. Survey of School-Based Oral Health Programs Operated by Health Centers: descriptive findings [Internet] Denver (CO): NNOHA; 2014. Jul, [cited 2016 Oct 31]. Available from: http://www.nnoha.org/nnoha-content/uploads/2014/07/SBHC-Report-FINAL_2014-07-28.pdf. [Google Scholar]
- 40.Mejia GC, Weintraub JA, Cheng NF, Grossman W, Han PZ, Phipps KR, et al. Language and literacy relate to lack of children’s dental sealant use. Community Dent Oral Epidemiol. 2011;39(4):318–24. doi: 10.1111/j.1600-0528.2010.00599.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Al Agili DE, Griffin SO. Effect of family income on the relationship between parental education and sealant prevalence, National Health and Nutrition Examination Survey, 2005–2010. Prev Chron Dis. 2015;12:E138. doi: 10.5888/pcd12.150037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Junge ML, Corley T, Orgain L, Betancourt M, Barker LK. Factors associated with sealant and fluoridation knowledge—Health Styles 2009; Presentation at: International Association of Dental Research 89th General Session and Exhibition of the IADR; San Diego, CA. March 16–19, 2011. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.