Abstract
Hyaluronic acid plays a role in controlling inflammatory airway processes and mucociliary clearance, and it is also involved in tissue healing and remodelling. Some studies have tested the effectiveness of topically administered hyaluronic acid in patients with upper airway diseases with positive preliminary results. This article describes the use of topically administered hyaluronic acid in patients with otolaryngological disorders. Pertinent studies published between January 2000 and October 2016 were selected by means of a MEDLINE search using the following terms: ‘hyaluronic acid’ and ‘otolaryngology’, ‘otitis’, ‘pharyngitis’, ‘tonsillitis’, ‘rhinitis’, ‘rhinosinusitis’ and ‘nose’. Twelve of the 19 initially identified papers were selected, corresponding to 902 patients as a whole. There is some evidence that topically administered hyaluronic acid is effective or moderately effective in different otolaryngological conditions, as it improves the global subjective and clinical status of patients with inflammation of the nasopharyngeal and oto-tubaric complex, those with rhinitis or rhinosinusitis and those who have undergone nasal and sinonasal surgery. However, these findings should be viewed cautiously as they are based on a limited number of studies, some of which were probably under-powered because of their small patient samples.
Keywords: adenoiditis, hyaluronic acid, otitis media, rhinitis, rhinosinusitis
Introduction
Hyaluronic acid (HA) is a high-molecular-weight (HMW) and ubiquitously endogenous non-sulphated glycosaminoglycan that acts as a component of many extra-cellular matrices and organic fluids. It can be found in connective tissue, respiratory epithelia, nasal and tracheobronchial mucosa, airway secretions and gland serous cells.
HA acts as a lubricant of airway surfaces, and it is involved in tissue healing and remodelling and modulates inflammatory responses.1 It also plays a role in regulating vascular tone and mucous gland secretion,2 and it has been reported that HA can exert in vitro anti-infective and anti-biofilm effects by preventing bacterial adhesion.3
HA is widely used in various branches of medicine, including orthopaedics, otolaryngology, aesthetic medicine and plastic surgery, gastroenterology, paediatric dentistry and pneumology,4,5 and new topical formulations have been developed in order to deliver it to the upper airways by means of a nebulised, micronised nasal douche. A number of studies have shown the effectiveness and safety of topically administered HA in adults and children with upper airway tract infections or inflammation, and in those who have undergone nasal surgery.1,2,6–17 This review describes the use of topically administered HA in patients with otolaryngological disorders.
Methods
Pertinent studies published between January 2000 and October 2016 were selected by Sara Torretta on November 2016 by means of a MEDLINE search (accessed via PubMed) using the following terms: ‘hyaluronic acid’ and ‘otolaryngology’, ‘otitis’, ‘pharyngitis’, ‘tonsillitis’, ‘rhinitis’, ‘rhinosinusitis’ and ‘nose’.
We only considered English language papers describing randomised and controlled trials (RCTs) involving otherwise healthy children or adults with a single and well-defined otolaryngological condition (e.g. inflammation of the nasopharyngeal and oto-tubaric complex; rhinitis and rhinosinusitis; previous nasal and sinonasal surgery) undergoing treatment with topically administered HA that had been published in peer-reviewed journals. When the full text of a paper was not available on line, an e-mailed request was sent to the corresponding author; if there was no answer, the paper was excluded, as were any studies of invasive HA administration or its use in the form of nasal packing or dressing. The reference lists were subsequently reviewed in order to ensure that all of the selected papers were truly relevant and identify any possibly overlooked and pertinent papers.
Results
Twelve of the 20 initially identified papers were included in this review, corresponding to 902 patients (Figure 1). Three papers were performed exclusively on paediatric patients, while the remaining ones on adult patients. Table 1 shows their main results and Table 2 summarises the evidence gathered regarding the efficacy of topically administered HA in the previously defined conditions.
Figure 1.
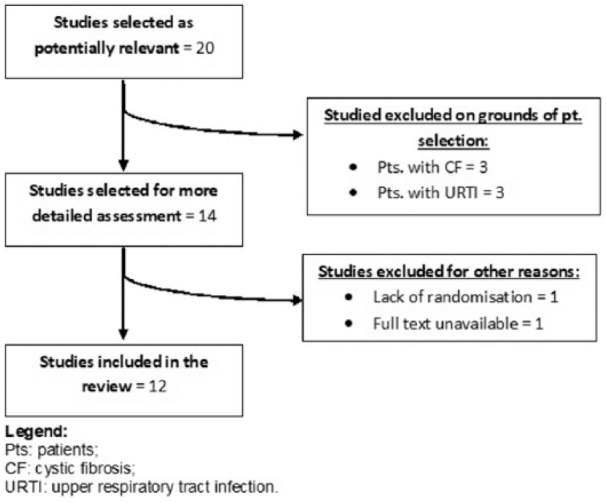
Flow chart of article selection.
Table 1.
Results of the included studies. .
| Topic | Authors | No. of pts. | Mean age ± SD (years) | Disease | Treatment | Results |
|---|---|---|---|---|---|---|
| Inflammation of the nasopharyngeal and oto-tubaric district | Varricchio et al.8 | 51 | 5.9 ± 2.1 | Acute bacterial rhinopharyngitis | Nebulised thiamphenicol + SH + xylitol 5% versus nebulised thiamphenicol + ISS | Thiamphenicol + SH had a significantly greater effect on subjective symptoms, and nasal neutrophilic and bacterial counts than thiamphenicol + ISS |
| Torretta et al.9 | 103 | 63.3 ± 18.2 months | Chronic adenoiditis with RAOM and OME | Nebulised SH + ISS versus nebulised ISS | SH significantly reduced the mean number of all AOM episodes and AOM episodes without spontaneous tympanic membrane perforation, and significantly improved all endoscopic findings. ISS did not reduce the number of AOM episodes and significantly improved only 3/10 endoscopic findings | |
| Torretta et al.10 | 116 | 62.9 ± 17.9 months | OME and/or RAOM with chronic adenoiditis | Nebulised SH + ISS versus nebulised ISS | SH significantly reduced the number of children with impaired otoscopy and tympanometry, conductive hearing loss, and moderate hearing impairment, and significantly improved the mean auditory threshold. No improvement was found in the ISS group | |
| Rhinitis and rhinosinusitis | Gelardi et al.7 | 78 | 21–63 (range) | Allergic and non-allergic rhinitis | Nebulised SH + ISS + intranasal mometasone spray + oral desloratadine versus nebulised ISS + mometasone intranasal spray + oral desloratadine | SH was significantly more effective than ISS in improving rhinorrhoea and sneezing, and reducing nasal exudate |
| Casale et al.13 | 39 | 30–63 (range) | Chronic rhinosinusitis | Nebulised SH + ISS versus nebulised ISS | SH significantly improved symptom scores and endoscopic findings; no change was observed in the ISS group | |
| Cassandro et al.17 | 80 | 38.6 ± 13.1 (NIS) 34.8 ± 17.7 (ICS) 38.7 ± 13.1 (NSH) 38.8 ± 13.3 (ICS + NSH) |
CRSwNP | Nebulised ISS (NIS) versus intranasal mometasone spray (ICS) versus nebulised SH + ISS (NSH) versus intranasal mometasone spray + nebulised SH + ISS (ICS + NSH) | Nasal symptoms, endoscopic and, radiological scores, rhinomanometry, and saccharine clearance test significantly improved in the NSH, ICS and ICS + NSH groups during treatment. In comparison with NIS, NSH, ICS and ICS + NSH led to significant improvements in all scores during and after treatment, and significantly reduced the use of oral steroids | |
| Gelardi et al.12 | 89 | 36.3 ± 7.1 | Allergic, non-allergic rhinitis, and mixed rhinitis | Intranasal ointment containing LHT versus nasal lavage with ISS | The active treatment significantly improved symptoms and endoscopic features, and reduced the number of inflammatory nasal cells | |
| Nasal and nasosinusal surgery | Casale et al.14 | 57 | 19–78 (range) | Pts. who had undergone radiofrequency turbinoplasty | Nebulised SH + ISS versus nasal irrigation with ISS | SH was significantly more effective than ISS in improving symptoms 1 and 2 weeks after treatment, and significantly reduced nasal crusting |
| Macchi et al.1 | 46 | 37 ± 14 (SH) 40 ± 15 (ISS) |
Pts. who had undergone FESS for rhino-sinusal remodelling | Nebulised SH + ISS versus nebulised ISS | SH significantly improved nasal dyspnoea, ciliary motility and nasal secretions, and significantly decreased endonasal mycetes in comparison with ISS | |
| Gelardi et al.2 | 36 | 47 ± 14 (SH) 47 ± 14 (ISS) |
Pts. who had undergone FESS because of CRSwNP | Nebulised SH + ISS versus nebulised ISS | SH significantly improved mucociliary clearance, rhinorrhoea, nasal obstruction and nasal exudate in comparison with ISS | |
| Cantone et al.16 | 124 | 41.4 ± 2.4 (SH) 42.4 ± 1.4 (ISS) |
Pts. who had undergone FESS because of CRSwNP | Nebulised SH + ISS versus nebulised ISS | SH significantly improved symptoms, and endoscopic, SNOT-22 and SF-36 scores in comparison with ISS | |
| Gelardi et al.11 | 83 | 46.4 ± 6.2 | Pts. who had undergone FESS because of CRSwNP, CRSwithoutNP, and for purposes of septoplasty and turbinoplasty | Intranasal ointment containing LHT versus nasal lavage with ISS | LTH significantly improved symptoms and endoscopic features, and reduced inflammatory nasal cells in comparison with controls |
No.: number; Pts: patients; SD: standard deviation; SH: sodium hyaluronate; ISS: isotonic saline solution; ICS: intranasal corticoid steroid; RAOM: recurrent acute otitis media; OME: otitis media with effusion; AOM: acute otitis media; FESS: functional endoscopic sinus surgery; CRSwNP: chronic rhinosinusitis with nasal polyps; SNOT-22: 22-item Sino-Nasal Outcome Test; SF-36: Italian Short Form-36; LHT: lysine hyaluronate, thymine, and sodium chloride.
NIS: nebulised isotonic saline solution; NSH: nebulised sodium hyaluronate plus isotonic saline solution
Table 2.
Overall efficacy of topically administered, according to any otolaryngological condition.
| Topic | Overall efficacy |
|---|---|
| RAOM with or without OME | Moderately effective in prevent AOM episodes |
| Nasopharyngeal inflammation | Effective |
| Chronic rhinosinusitis | Moderately effective |
| CRSwNP | Moderately effective with concomitant ICS |
| Allergic and non-allergic rhinitis | Moderately effective with concomitant ICS |
| Nasal and nasosinusal surgery | Effective |
RAOM: recurrent acute otitis media; OME: otitis media with effusion; AOM: acute otitis media; CRSwNP: chronic rhinosinusitis with nasal polyps; ICS: intranasal corticoid steroid.
Inflammation of the nasopharyngeal and oto-tubaric district
Two RCTs9,10 have investigated the efficacy of topically administered HA in children with chronic adenoiditis and middle ear diseases, including recurrent acute otitis media (RAOM) and otitis media with effusion (OME). In the first, Torretta et al.9 documented a significant reduction in the mean number of all episodes of acute otitis media (AOM; 0.8 ± 0.4 episodes/month), and in the mean number of AOM episodes without spontaneous tympanic membrane perforation (0.6 ± 0.3 episodes/month) in 54 patients receiving HA (9 mg of sodium hyaluronate (SH) diluted in 3 mL of isotonic saline solution, administered once daily for 15 days a month for three consecutive months), whereas there was no reduction in the 49 children receiving isotonic saline solution alone. HA proved to be effective in improving all of the assessed endoscopic outcomes (the degree of adenoidal hypertrophy, the presence of turbinate hypertrophy, nasal secretion, nasal mucosal dyschromia or swelling and obstruction of the Eustachian tube orifice), only a few of which were improved into the control group. The second study showed that the same therapeutic protocol reduced the mean number of patients with impaired otoscopy and tympanometry, conductive hearing loss and moderate hearing impairment, and globally improved the mean auditory threshold of 58 children with OME and/or RAOM and chronic adenoiditis, whereas no significant improvement was observed in children receiving isotonic saline solution alone.10
In addition, Varricchio et al.8 found that the efficacy of topical antibiotic therapy with 125 of thiamphenicol could be improved by adding 4 mL of SH 0.2% plus xylitol 5%, as shown by the greater improvement on symptom perception and nasal neutrophilic and bacterial counts in 51 children with acute bacterial rhinopharyngitis
Rhinitis and rhinosinusitis
Two studies published by Gelardi et al.7,12 assessed the effectiveness of two compounds containing HA in patients with allergic and non-allergic rhinitis. In the first,7 nebulised SH 9 mg diluted in 3 mL of isotonic saline solution plus mometasone furoate nasal spray 100 µg/day and oral desloratadine 5 mg (39 patients) was compared with 6 mL of nebulised isotonic saline solution plus mometasone furoate nasal spray 100 µg/day and oral desloratadine 5 mg (39 patients). It was found that in comparison with the controls, the patients in the treatment group had a significantly lower number of nasal neutrophils as assessed by means of nasal cytology; they also experienced a significant improvement in nasal symptoms (sneezing, rhinorrhoea and nasal congestion) and showed a reduction in endoscopic evidence of nasal exudate. In the second, an intranasal ointment containing lysine hyaluronate, thymine and sodium chloride (LHT) was used in 48 patients with allergic, non-allergic and mixed rhinitis,12 in addition to intranasal mometasone furoate 100 µg/day and oral rupatadine fumarate. It was found that intranasal LHT significantly reduced the number of patients with subjective symptoms, the number of inflammatory intranasal cells and the endoscopic features of nasal impairment in comparison with baseline, and in comparison with the control treatment (intranasal isotonic saline solution plus intranasal corticosteroid and oral antihistamine).
Topically administered HA has also been successfully used to treat chronic rhinosinusitis with or without nasal polyps:13,17 Cassandro et al.17 conducted an open-label trial involving 80 patients with chronic rhinosinusitis with nasal polyposis and found a significant improvement in nasal symptoms, endoscopic appearance, radiological score, rhinomanometry and saccharine clearance in those receiving mometasone furoate nasal spray 400 µg/day with or without nebulised SH 9 mg diluted in 2 mL of isotonic saline solution in comparison with baseline, and in comparison with patients receiving nebulised isotonic saline solution alone. Moreover, the patients in the treatment groups resorted to oral steroid consumption less frequently than the controls. Casale et al.13 found that nebulised HA (SH 3 mL dissolved in 2 mL of isotonic saline solution) significantly reduced ostiomeatal oedema and secretion and improved the quality of life of 21 adults with chronic rhinosinusitis and nasal polyposis, whereas no change was observed in 18 patients receiving nebulised isotonic saline solution alone.
Nasal and sinonasal surgery
We found five RCTs assessing the effect of topically administered HA after nasal or sinonasal surgery,1,2,11,14,16 four of which involved patients who had undergone functional endoscopic sinus surgery (FESS)1,2,11,16 and one patients who had undergone turbinoplasty.14 The trials conducted by Macchi et al.,1 Gelardi et al.2 and Cantone et al.16 compared the effects of nebulised SH 9 mg diluted in isotonic saline solution with those of nebulised isotonic saline solution alone in patients who had undergone FESS because of chronic rhinosinusitis with nasal polyposis and for the purpose of rhino-sinusal remodelling. Of the 202 patients in the three trials, 104 received topically administered SH and 98 received nebulised isotonic saline solution. All three studies showed that SH had a positive clinical effect on subjective and objective parameters, including symptom scores evaluated by means of visual analogue scales and standardised SNOT-22 (22-item Sino-Nasal Outcome Test) and SF-36 (Italian Short Form-36) questionnaires, endoscopic appearance and cytological measures. In particular, it was reported that the patients receiving nebulised SH experienced a significantly greater improvement in nasal dyspnoea, impaired nasal secretion and ciliary motility, and a reduction in the presence of nasal mycetes and biofilm.1
Cantone et al.16 compared topically administered SH with nebulised isotonic saline solution in a double-blind trial involving 124 patients and found that in comparison with the controls, SH significantly improved the patients’ post-operative quality of life not only in terms of sinonasal status, but also in terms of general health as assessed on the basis of physical functioning, social/emotional role functioning, bodily pain, vitality and mental health.
Gelardi et al.11 recently published a paper describing an open-label trial of intranasal LHT ointment involving 83 patients who had undergone FESS, septoplasty and turbinoplasty and found that in comparison with isotonic saline solution nasal lavage, the treatment significantly reduced symptom severity and improved endoscopic and nasal cytological features.
Casale et al.14 studied the effect of nebulised HA (SH 3 mL dissolved in 2 mL of isotonic saline solution) in 22 patients who had undergone radiofrequency surgery because of chronic inferior turbinate hypertrophy and found that in comparison with 35 patients receiving nasal irrigation with isotonic saline solution, the patients in the treatment group experienced a significant post-operative improvement in nasal respiration as assessed by means of subjective scores and the reduction in nasal crusting.
Discussion
The few published studies of topically administered HA in patients with otolaryngological disorders suggest that it is effective as ancillary treatment in children with recurrent or chronic middle ear inflammation and chronic adenoiditis, in adult patients with rhinitis or chronic rhinosinusitis, and in those who have undergone sinonasal surgery.1,2,6–17 Nebulised HA seems to act positively on the endoscopic appearance of the sinonasal and nasopharyngeal district, as shown by the significant reduction in nasal exudate and inflammatory cells, and the improvements in mucociliary clearance, microbiological status and nasal respiratory patency. This leads to a decrease in the number of AOM episodes and a global improvement in audiological outcomes and the otoscopic appearance of the tympanic membrane in otitis-prone children, and the better control of respiratory symptoms and inflammatory events in patients with recurrent or chronic nasal or sinonasal disease.
Some of the reviewed RCTs show that topically administered HA can significantly improve sinus ostial patency and reduce the presence of nasal crusting and secretions, thus allowing a prompt mucosal recovery and greater comfort in patients who have undergone FESS or turbinoplasty.1,2,11,14,16 This is probably due to its positive effect on the healing process and mucosal trophism. Our review also indicates that nebulised HA is safe as it was well-tolerated and no untoward effects were reported.
In conclusion, despite there are some evidences that topically administered HA improves the global subjective and clinical status of patients with different upper airway disorders, these findings should be viewed cautiously as they are based on a limited number of studies (including only three involving children), some of which were probably under-powered because of their small patient samples. Therefore, further research should be performed in order to confirm the effectiveness of topical administered HA in such patients, to define the better therapeutic protocols (way of administration and dosage) and to selectively test its effectiveness in the paediatric age.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
ORCID iD: Sara Torretta  https://orcid.org/0000-0002-8461-6042
https://orcid.org/0000-0002-8461-6042
References
- 1. Macchi A, Terranova P, Digilio E, et al. (2013) Hyaluronan plus saline nasal washes in the treatment of rhino-sinusal symptoms in patients undergoing functional endoscopic sinus surgery for rhino-sinusal remodeling. International Journal of Immunopathology and Pharmacology 26: 137–145. [DOI] [PubMed] [Google Scholar]
- 2. Gelardi M, Guglielmi AV, De Candia N, et al. (2013) Effect of sodium hyaluronate on mucociliary clearance after functional endoscopic sinus surgery. European Annals of Allergy and Clinical Immunology 45: 103–108. [PubMed] [Google Scholar]
- 3. Drago L, Cappelletti L, De Vecchi E, et al. (2014) Antiadhesive and antibiofilm activity of hyaluronic acid against bacteria responsible for respiratory tract infections. Acta Pathologica, Microbiologica, et Immunologica Scandinavica 122: 1013–1019. [DOI] [PubMed] [Google Scholar]
- 4. Gutowski KA. (2016) Hyaluronic acid fillers: Science and clinical uses. Clinics in Plastic Surgery 43: 489–496. [DOI] [PubMed] [Google Scholar]
- 5. D’Ercole S, Nanussi A, Tieri M, et al. (2015) Hyaluronic acid-based medical device and oral disorders: Can it be used in paediatric dentistry? Journal of Biological Regulators and Homeostatic Agents 29: 999–1005. [PubMed] [Google Scholar]
- 6. Macchi A, Castelnuovo P, Terranova P, et al. (2013) Effects of sodium hyaluronate in children with recurrent upper respiratory tract infections: Results of a randomised controlled study. International Journal of Immunopathology and Pharmacology 26: 127–135. [DOI] [PubMed] [Google Scholar]
- 7. Gelardi M, Iannuzzi L, Quaranta N. (2013) Intranasal sodium hyaluronate on the nasal cytology of patients with allergic and nonallergic rhinitis. International Forum of Allergy & Rhinology 3: 807–813. [DOI] [PubMed] [Google Scholar]
- 8. Varricchio A, Capasso M, Avvisati F, et al. (2014) Inhaled hyaluronic acid as ancillary treatment in children with bacterial acute rhinopharyngitis. Journal of Biological Regulators and Homeostatic Agents 28: 537–543. [PubMed] [Google Scholar]
- 9. Torretta S, Marchisio P, Rinaldi V, et al. (2016) Endoscopic and clinical benefits of hyaluronic acid in children with chronic adenoiditis and middle ear disease. European Archives of Oto-Rhino-Laryngology 274: 1423–1429. [DOI] [PubMed] [Google Scholar]
- 10. Torretta S, Marchisio P, Rinaldi V, et al. (2016) Topical administration of hyaluronic acid in children with recurrent or chronic middle ear inflammations. International Journal of Immunopathology and Pharmacology 29: 438–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gelardi M, Taliente S, Fiorella ML, et al. (2016) Intranasal T-LysYal® as adjunctive therapy for patients after functional endoscopic sinus surgery. Journal of Biological Regulators and Homeostatic Agents 30: 277–284. [PubMed] [Google Scholar]
- 12. Gelardi M, Taliente S, Fiorella ML, et al. (2016) Ancillary therapy of intranasal T-LysYal® for patients with allergic, non-allergic, and mixed rhinitis. Journal of Biological Regulators and Homeostatic Agents 30: 255–262. [PubMed] [Google Scholar]
- 13. Casale M, Sabatino L, Frari V, et al. (2014) The potential role of hyaluronan in minimizing symptoms and preventing exacerbations of chronic rhinosinusitis. American Journal of Rhinology & Allergy 28: 345–348. [DOI] [PubMed] [Google Scholar]
- 14. Casale M, Ciglia G, Frari V, et al. (2013) The potential role of hyaluronic acid in postoperative radiofrequency surgery for chronic inferior turbinate hypertrophy. American Journal of Rhinology & Allergy 27: 234–236. [DOI] [PubMed] [Google Scholar]
- 15. Montella S, Cantone E, Maglione M, et al. (2016) Sodium hyaluronate improves quality of life and nasal endoscopy features in preschool children with upper respiratory tract infections. Journal of Biological Regulators and Homeostatic Agents 30: 303–308. [PubMed] [Google Scholar]
- 16. Cantone E, Castagna G, Sicignano S, et al. (2014) Impact of intranasal sodium hyaluronate on the short-term quality of life of patients undergoing functional endoscopic sinus surgery for chronic rhinosinusitis. International Forum of Allergy & Rhinology 4: 484–487. [DOI] [PubMed] [Google Scholar]
- 17. Cassandro E, Chiarella G, Cavaliere M, et al. (2015) Hyaluronan in the treatment of chronic rhinosinusitis with nasal polyposis. Indian Journal of Otolaryngology and Head and Neck Surgery 67: 299–307. [DOI] [PMC free article] [PubMed] [Google Scholar]


