Abstract
Multiple sclerosis is a disabling and progressive neurological disease that has significant negative effects on health-related quality of life. This exploratory efficacy study examined the effects of Healing Light Guided Imagery (HLGI), a novel variant of guided imagery, compared with a wait-list control in patients with relapsing-remitting multiple sclerosis. Changes in the Beck Depression Inventory, Fatigue Severity Scale, and Multiple Sclerosis Quality of Life instrument (physical and mental components) were compared between groups. Patients who completed HLGI (N = 9) showed significant reductions in depressed mood (P < .05) and fatigue (P < .01) and showed significant gains in physical (P = .01) and mental (P < .01) quality of life compared with journaling (N = 8). Our results suggest that HLGI can improve self-reported physical and mental well-being in patients with relapsing-remitting multiple sclerosis. Further research is needed to study the effectiveness of this therapy, as well as its mind-body mechanisms of action.
Keywords: multiple sclerosis, guided imagery, depression, fatigue, quality of life
Multiple sclerosis (MS) is a disabling and progressive neurological disease that affects approximately 400 000 people in the United States.1,2 MS has a significant negative effect on health-related quality of life, including in domains of emotional, functional, physical, social, and spiritual well-being.3,4 In a survey of more than 11 000 individuals with MS conducted by the MS Foundation, 57% of patients reported having tried at least one complementary and alternative medicine modality (now commonly called integrative medicine when incorporating complementary and alternative medicine practices into mainstream medical practice).5 Other studies suggest higher rates (67%) of use of such practices by MS patients.6,7 MS patients often seek out mind-body therapies, and studies indicate benefits including improved quality of life and physical functioning and moderation of common MS symptoms such as fatigue.6,8–12 Recent reviews focusing on potential benefits of mindfulness meditation, for example, suggest an association between meditation practice and lower risk of depression and improved quality of life in people with MS.9,13–15 Given known associations between measures of MS disease activity and stressful life events, and the moderating effect of stress management programs on these measures of disease activity,16,17 it is been postulated that integrative therapies mediate benefits through the reduction of autonomic arousal and stress.18,19
Among integrative modalities, Guided Imagery (GI) is considered a “relaxation modality” by the National Center for Complementary and Integrative Health, because it can profoundly activate the body’s natural relaxation response as characterized by slower breathing and lower blood pressure as well as increased feelings of well-being.20 A critical review of the literature by Trakhtenberg21 suggested that GI can influence the immune system.21 There is increasing interest in the literature on the efficacy of GI as part of a broader biobehavioral model for disability and depression, which includes its use in the management of inflammatory diseases.22–24 Given the potential immune-mediating effects of GI via changes in the hypothalamic-pituitary-adrenal axis,24–26 there is a rational foundation for the use of GI in the treatment of immune mediated disorders such as MS to therapeutically modulate immune responses.21,27 Important indirect effects of GI also include adherence to other positive lifestyle activities and medication recommendations.28,29
A recent trial in clinical groups examining the effectiveness of GI as compared with usual care on fibromyalgia symptoms demonstrated that patients assigned to GI showed significant decreases in fatigue, pain, and depression.30 Studies on GI effects in breast cancer patients suggest improvements in depression and immune function.23,31
Despite the promise of the literature suggesting such benefits of GI, few studies have explored the potential benefits of GI in MS. GI and affirmations are believed to stimulate a light self-hypnotic state that has the potential to provide a healing modality to accompany current MS treatment. In a prior quasi-experimental trial comparing the effects of self-hypnosis training with relaxation on pain in 22 MS patients, Jensen et al32 reported reductions in pain and pain interference associated with self-hypnosis.
The current study examined a novel GI modality, Healing Light Guided Imagery (HLGI). HLGI was developed by an MS patient specifically for MS patients and their symptoms. Unlike hypnosis scripts developed by generalized hypnotherapy practitioners who seek to treat a broad range of conditions using several combinations of scripts available from published sources, HLGI was developed specifically to treat the concerns related to an MS diagnosis. In addition to the relaxation component, the therapeutic use of GI includes using active visualization or directed imagery for changing behavior and the use of receptive imagery to help relieve symptoms and improve mood.
The purpose of this exploratory efficacy study therefore was to examine the potential of HLGI to enhance self-reported quality of life. We hypothesized that HLGI, as compared to an active wait-list control, would improve symptoms of depression and fatigue and improve self-reported quality of life.
Methods
Patients and Procedures
Participants were a convenience sample recruited through study flyers distributed to local and UC San Diego MS clinics and organizations. The ad sought volunteers for a study on “complementary and alternative techniques for improving quality of life in patients with Relapsing-Remitting Multiple Sclerosis (RRMS).” Potential participants underwent a phone screening where the study was further described, and age, sex, diagnosis, and duration of disease were collected. Inclusion criteria included if participants were between 18 and 70 years old, had a current medical diagnosis of RRMS, agreed they were able to read and write in English, and were available for 1 hour weekly at home or at the University of California San Diego School of Medicine.
Ethical Approval
The UC San Diego Institutional Review Board approved the study and all study participants provided written informed consent prior to participation.
Assessments
Screening assessments included the Beck Depression Inventory–II (BDI-II) and the Fatigue Severity Scale (FSS), which were administered over the phone. BDI-II is a measure of mood based on criteria found in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition for depressive disorders33 and is a strong predictor of cognitive performance in MS patients.34 FSS is a measure of fatigue that differentiates MS patients from controls and is sensitive to changes in fatigue over time. As measured by the FSS, fatigue is largely independent of self-reported symptoms of depression.35
Potential participants were excluded for severe depression (score of 31 or higher on the BDI) and/or very high levels of fatigue that might interfere with intervention adherence (greater than an average of 6 on the FSS).
Intervention assessments included the BDI-II, FSS, and the Multiple Sclerosis Quality of Life instrument (MS-QOL-54) which were completed at their intake session and again the end of the 10-week intervention. MS-QOL-54 is a multidimensional health-related quality of life measure that combines both generic and MS-specific items into a single instrument. This 54-item instrument generates 12 subscales along with 2 summary scores, and 2 additional single-item measures; we studied the physical health and mental health composite scores. The MSQOL-54 shows good test-retest reliability and good intraclass correlation coefficients (.66-.96.).36
For this population, the Cronbach α reliability coefficients for the BDI-II and FSS and the physical and mental health MS-QOL-54 instruments were .367, .841, .857, and .736, respectively.
All assessment questionnaires were scored by an experimenter with intervention masked.
Interventions
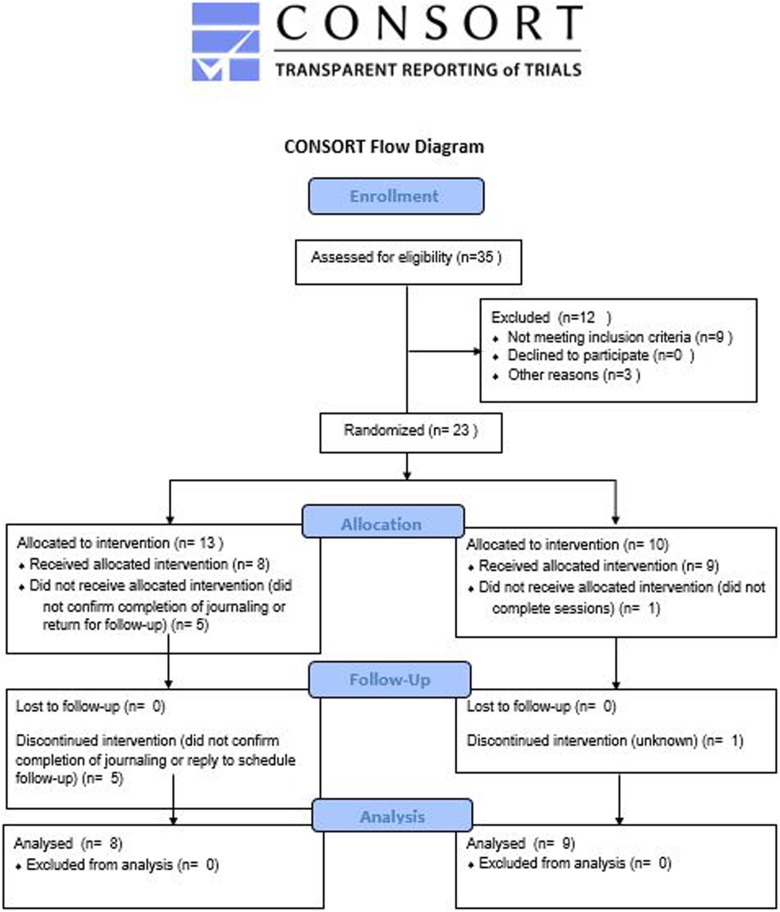
Patients who met inclusion criteria were invited to enroll in the study and were put in contact with the study coordinator. Study enrollment occurred in person at the University of California San Diego School of Medicine. A study coordinator who was not involved in phone screening conducted the informed consent process and assigned participants to the study arms. Twenty-three individuals were enrolled into the study (Figure 1). Participants were assigned alternately (1:1) to the 2 study arms; 10 hours of HLGI or 10 hours of positive journaling (control condition). If enrolled patients dropped out of the study, we enrolled new patients in order to achieve our intended sample size.
Figure 1.
CONSORT (Consolidated Standards of Reporting Trials) diagram.
Patients in the HLGI condition participated in 10 HLGI sessions, which were conducted by a qualified practitioner. Eight of the sessions involved active HLGI; the first and final sessions were intake and completion sessions with little or no active treatment. HLGI followed a common sequence for each participant (see Appendixes A and B) but was highly individualized depending on patients’ responses.
Journaling was chosen as an active wait-list control activity. Patients in the journaling condition were instructed to write at home for 1 hour a week for 10 weeks. Participants were provided with a positive journaling prompt each week. Participants returned their journals to the study investigators at the end of the 10 weeks. Several participants completed the journaling verbally (audio recording) rather than by hand due to pain or limited hand mobility. As part of enrollment, patients were told that those assigned to journaling would receive HLGI following the study, if they so choose.
Data Analysis
This was an exploratory study to examine the effects of HLGI as compared to a wait-list control in patients with RRMS. The purpose was to examine potential effectiveness and, if the findings were significant and promising, to generate data for a subsequent effectiveness trial based on a power analysis using data from this study. Data were analyzed by t tests, 1-way analysis of variance (ANOVA), and 2-way (group × time) repeated-measures ANOVAs (SPSS Version 24). Per examination of box plots and skewness and kurtosis values, data were found to be normally distributed. We report effect sizes in the form of the partial η2 statistic and 95% confidence intervals (CIs).
Results
Nine participants completed HLGI and 8 completed positive journaling. Five participants dropped out (or fell out of contact) in the journaling condition and 1 in the HLGI condition (38% and 10%, respectively). Mean enrollment scores did not differ between participants who completed versus those who did not complete the study for the BDI II (completed M = 8.2, dropped M = 11.6, t(20) = 0.90, P = .38), FSS (completed M = 38.7, dropped M = 48.0, t(20) = 1.22, P = .24), MS-QOL-54 physical composite (completed M = 53.3, dropped M = 49.0, t(19) = 0.47, P = .64), or MS-QOL-54 mental composite (completed M = 69.8, dropped M = 64.3, t(19) = 0.61, P = .55).
Patients ranged in age from 33 to 69 years (mean = 50.8 years, SD = 11.5). Disease duration was 1 to 32 years (mean = 12.1 years, SD = 10.2). There were no significant group differences in age, gender distribution, disease duration or screening scores for depressed mood or fatigue (Table 1).
Table 1.
Relapsing-Remitting Multiple Sclerosis Patient Characteristics According to Group.a
| Variable | Healing Light Guided Imagery | Wait-List Journaling |
|---|---|---|
| Age (years) | 49.1 (10.4) | 52.7 (13.2) |
| Disease duration (years) | 13.2 (9.8) | 10.7 (11.3) |
| Screening Beck Depression Inventory II | 10.5 (9.01) | 5.4 (5.6) |
| Screening Fatigue Severity Scale | 41.9 (12.7) | 38.2 (14.6) |
aData are presented as mean ± standard deviation; no significant differences.
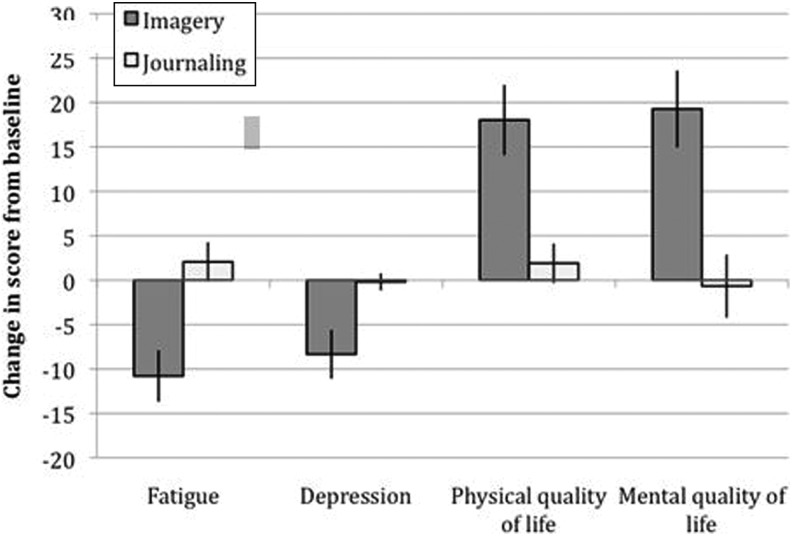
Separate 2-way (group × time) repeated-measures ANOVAs showed that HLGI led to significant improvements in each of the 4 study outcomes (Figure 2). HLGI led to a 75% decrease (95% CI, 4.18-11.7) in depressed mood scores (vs a 15% decrease with journaling (95% CI, 1.68-5.44), F(1, 8.3) = 5.9, P = .04, partial η2 = 0.34), and a 24% decrease in fatigue scores (95% CI, 27.6-43.1) (vs a 6% increase with journaling (95% CI, 27.6-43.1), F(1, 15.3) = 11.1, P = .004, partial η2 = 0.35). Regarding quality of life, HLGI led to a 38% increase in physical quality of life scores (95% CI, 43.3-64.3) (vs a 3% increase with journaling (95% CI, 53.5-74.6), F(1, 14.2) = 8.7, P = .01, partial η2 = 0.38), and a 30% increase in mental quality of life (95% CI, 60.4-80.0) (vs 0% change with journaling (95% CI, 71.1-87.5), F(1, 14.4) = 9.8, P = .007, partial η2 = 0.41).
Figure 2.
Change in scores of multiple sclerosis (MS) patients from before to after Healing Light Guided Imagery (HLGI) or positive journaling for outcome measures fatigue (Fatigue Severity Scale), depressed mood (Beck Depression Inventory II), and MS physical and mental quality of life (MS-QOL-54 domain scores). HLGI was associated with reductions in depression (P < .05) and fatigue (P < .01), and increases in physical (P = .01) and mental (P < .01) quality of life. Error bars display standard error of the mean.
Discussion
Guided imagery is a mind-body modality that has demonstrated benefits for stress, depression, and possibly inflammatory diseases.20,21 The current exploratory study tested a variant of GI called “Healing Light Guided Imagery” (HLGI) and MS patients showed improvements in depression, fatigue, and physical and mental quality of life following practice. All 4 planned outcome measures suggested clinically relevant effects with strong effect sizes that require confirmation in larger controlled studies. These effects were obtained after 10 hours of once-a-week treatment, suggesting that HLGI may be a fruitful relaxation technique to explore for individuals with RRMS. While relaxation, in and by itself, is a benefit to individuals with MS, we find additional benefits of changes in depressed mood and fatigue as well as improvements in the client’s physical and mental quality of life.
The effects of HLGI are consistent with the broader literature on the efficacy of GI for illnesses associated with pain, depression and chronic disability.30 Although in this efficacy study we did not evaluate potential mechanisms of action of HLGI, studies on other GI modalities suggest the practices support relaxation and beneficial changes in hypothalamic-pituitary-adrenal axis activation,24–26 which might be supporting the effects we’ve observed. While it is common for studies of mind-body and relaxation techniques to apply a generalized script or procedure to each individual, HLGI was administered in an individualized manner. While this allowed us to learn less about potential mechanisms involved in HLGI, we believe it is a demonstration of the strength of mind-body interventions in their natural state, that is, as typically individually practiced in the complementary and alternative medicine community.
There are several limitations of this efficacy study, including the modest sample size and a higher drop-out rate in the active wait-list group, which could have led to bias in the results. While patients in the journaling group had been offered HLGI following completion of the study, this did not lead to a high degree of adherence we were anticipating.
A prior phase II clinical trial of cognitive behavioral stress management training on measures of MS disease activity showed that the stress management programs not only lessened reported symptoms but also reduced disease activity compared to a control group, an effect which disappeared after the completion of therapy suggesting a need for ongoing therapy to maintain these benefits.37 It will be of interest in future studies of GI modalities to determine their durability as well as effects on measures of MS disease–specific activity.
In sum, the findings from this exploratory study suggest that HLGI has potential to benefit the well-being of patients with RRMS. There is at present strong demand by MS patients for mind-body modalities and many patients in this study expressed their gratitude that there was research being conducted examining integrative approaches to improve their quality of life. Needed are future studies that include more standard active control groups and that incorporate relevant biomarkers and disease activity outcomes to further advance this work.
Acknowledgments
We are grateful to the patients who contributed their time to this study.
Appendix A
Procedure for Healing Light Guided Imagery (HLGI)
The 10-week HLGI program included 10 weekly individual sessions with a coach consisting of an overview of the process followed by sessions consisting of relaxation, an induction, and specific HLGI milestones that were repeated with each session. The initial intake session includes a brief visualization exercise, and the final session includes a wrap-up and debriefing with no active treatment. During intake, the patient identifies a guided imagery “go-to place” that is returned to and developed with ongoing sessions. Patients are introduced to the process of induction, educating them about systems of affirmations and guided imagery used to improve creative imagination and evoke positive thoughts as often as possible.
HLGI uses a standardized framework that helps the patient relax into a mild trance. Here they are guided through standardized visual cues to access their beliefs and concerns related to their affliction. The framework is designed to empower the patient to face negative influences and see them transformed in their mind. The patient uses creative imagination to visualize light entering the top of their head, they then see certain color(s) from the spectrum of the white light reach the physical and mental areas of concern, permeating and bringing relief. This simulation of life-affirming images and positive outcomes when repeated by the patient as a part of their daily routine is believed to create new pathways for thought processing and in effect improve their overall ability to combat the comorbid symptoms such as depression and fatigue and enhance their quality of life.
The following are components of a typical HLGI session. Note that session steps and formats were individualized depending on the patient needs and experience.
The first step is an induction process to relax the patient.
Once relaxed, the patient is given a suggestion that a set of 20 stairs is in front of them, and, in their creative imagination, to walk over to the top of the stairs. Once they have arrived, they are asked what they are aware of.
Pending their visualization of the stairs, the patient and therapist either walk together down the stairs (to deepen the experience), or if there is a block, to identify and resolve the block.
The next step is a suggestion of a favorite chair they will see and become comfortable sitting in.
The next step is a suggestion that in the distance they see a rainbow and a certain color will stand out to them. Through their creative imagination, the patient either sees or does not see the rainbow. If there are visualization difficulties, for example, the patient sees only a single color light (usually white), this is worked with until they allow the light to embrace them as the imagery process allows, and needed steps are made in their creative imagination to do so.
A suggestion is given that they can bend this light in their creative imagination for their particular needs at that moment- for example, that the light is in their neural pathways, providing support to their nervous system. This is often reported as a tingling sensation by the patient. Once the patient’s capacity to work with the light is in place, the same support process is done for the heart, the circulatory system, organs, and cells, and that the patient sees these systems lighting up, pending their visualization process that day. During this part of the process, there are subtle changes in the patient’s posture and expression. Additional suggestions might be provided to keep them engaged in this process.
Following this main element of a session, the patient and therapist return up the stairs together and the patient is brought out of the guided imagery state.
The session concludes with a debriefing and discussion of the patient’s experience, and what to focus on for their daily at-home sessions for the upcoming week.
Appendix B
Positive Journaling Prompts
Week 1: Three Good Things in Life
Reminder for all weeks: what you write is confidential. We will ask to see that you filled up the page, but will not read or collect your writing. Please use the front and/or back of this page and add your own pages as needed.
Take time to think of three good things that happened today. These things can be relatively small in importance (eg, I managed to clean the fridge, or received an email from a friend) or relatively large (eg, I received a promotion at work). Next to each positive item on the list, write explanations for the following:
“Why did this good thing happen?”
“What does it mean to you?”
“How can you increase the likelihood of more good things happening in your life?”
Please write freely and bend the rules to fit your needs. If you find the exercise too difficult, you may wish to consider positive events from yesterday or from the past week.
Week 2: You at Your Past Best
In this exercise, list times when you were at your best, and reflect on the personal strengths that you needed to use in order to achieve this personal best. Write about how you felt and how you got there.
Week 3: Three Good Things in Life (Repeated From Week 1)
Take time to think of 3 good things that happened today. These things can be relatively small in importance (eg, I managed to clean the fridge, or received an email from a friend) or relatively large (eg, I received a promotion at work). Next to each positive item on the list, write explanations for the following:
“Why did this good thing happen?”
“What does it mean to you?”
“How can you increase the likelihood of more good things happening in your life?”
Week 4: Gratitude Letter
Spend some time reflecting on the past week and write down approximately five things for which you are currently grateful or thankful for.
Examples could be “waking up this morning,” “for the care received from another person,” or “for my resilience and effort.” Reflect on why you are grateful and how your life has been enriched by this experience and what it means to you.
Option 2: Write a letter of gratitude to someone who has been especially kind to you but you have never properly thanked.
Option 3: Write down several reasons you are grateful for each of the important people who are in your life—family members, friends, colleagues, etc.
Week 5: Three Good Things in Life
Take time to think of 3 good things that happened today. These things can be relatively small in importance (eg, I managed to clean the fridge, or received an email from a friend) or relatively large (eg, I received a promotion at work). Next to each positive item on the list, write explanations for the following:
“Why did this good thing happen?”
“What does it mean to you?”
“How can you increase the likelihood of more good things happening in your life?”
Week 6: Identifying Signature Strengths
Psychologists have identified 24 character strengths recognized by most all cultures38, which have been categorized into 6 main areas. First, identify at least 5 of your own personal strengths from this list:
Wisdom and knowledge: Creativity, Judgement, Curiosity, Love of Learning, Perspective
Courage: Bravery, Perseverance, Integrity, Enthusiasm
Love: Intimacy, Kindness, Sociability
Justice: Sense of responsibility, Fairness, Leadership
Temperance: Forgiveness, Modesty and Humility, Caution, Self-control
Transcendence: Appreciation, Gratitude, Optimism, Humor, Spirituality
Having identified 5 signature strengths, consider the following questions:
Do these fit with your expectations?
Have others previously remarked that you have these characteristics?
When you were “at your best”, were these character strengths present or did they assist in helping you achieve your goal?
When you act on these strengths how does it impact your state?
Week 7: Three Good Things in Life
Take time to think of 3 good things that happened today. These things can be relatively small in importance (eg, I managed to clean the fridge, or received an email from a friend) or relatively large (eg, I received a promotion at work). Next to each positive item on the list, write explanations for the following:
“Why did this good thing happen?”
“What does it mean to you?”
“How can you increase the likelihood of more good things happening in your life?”
Week 8: Using Signature Strengths in a New Way
Using the personal strengths identified from Week 6 (or think of new ones), how might you put these into practice?
How might you draw on your strengths further?
What are some of the ways you could use these strengths in a new way?
Are there further ways you can use your top two strengths in combination, perhaps to deal with a challenging situation, or an opportunity?
Week 9: Three Good Things in Life
Take time to think of 3 good things that happened today. These things can be relatively small in importance (eg, I managed to clean the fridge, or received an email from a friend) or relatively large (eg, I received a promotion at work). Next to each positive item on the list, write explanations for the following:
“Why did this good thing happen?”
“What does it mean to you?”
“How can you increase the likelihood of more good things happening in your life?”
Week 10: You at Your Future Best
In this exercise, think about your future self at your best, and reflect on the personal strengths that you can use to use in order to achieve this personal best. Transport yourself to the future and write about how you feel at this future personal best, and how you got there.
Footnotes
Author Contributions: LKC and PJ designed the study. PJ designed and administered the HLGI intervention. PJM managed and oversaw the conduct of the study. LKC analyzed the data. LKC and PJM wrote the manuscript and RK helped with further writing and editing. All authors read and approved the final manuscript.
Declaration of Conflicting Interests: The authors declared that there are no conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was supported by the University of California San Diego Department of Family Medicine and Public Health Center of Excellence for Research and Training in Integrative Health.
Ethical Approval.: This project was approved by the University of California San Diego Human Research Protection Program (IRB #121412).
References
- 1. Ma VY, Chan L, Carruthers KJ. Incidence, prevalence, costs, and impact on disability of common conditions requiring rehabilitation in the United States: stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, rheumatoid arthritis, limb loss, and back pain. Arch Phys Med Rehabil. 2014;95:986–995.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Niedziela N, Adamczyk-Sowa M, Pierzchała K. Epidemiology and clinical record of multiple sclerosis in selected countries: a systematic review. Int J Neurosci. 2014;124:322–330. [DOI] [PubMed] [Google Scholar]
- 3. Hourihan SJ. Managing fatigue in adults with multiple sclerosis. Nurs Stand. 2015;29:51–58. [DOI] [PubMed] [Google Scholar]
- 4. Kes VB, Cengić L, Cesarik M, et al. Quality of life in patients with multiple sclerosis. Acta Clin Croat. 2013;52:107–111. [PubMed] [Google Scholar]
- 5. Nayak S, Matheis RJ, Schoenberger NE, Shiflett SC. Use of unconventional therapies by individuals with multiple sclerosis. Clin Rehabil. 2003;17:181–191. [DOI] [PubMed] [Google Scholar]
- 6. Bowling AC. Complementary and alternative medicine and multiple sclerosis. Neurol Clin. 2011;29:465–480. [DOI] [PubMed] [Google Scholar]
- 7. Wright S, Yadav V, Bever C, Jr, et al. Summary of evidence-based guideline: complementary and alternative medicine in multiple sclerosis: report of the guideline development subcommittee of the American Academy of Neurology. Neurology. 2014;83:1484–1486. [DOI] [PubMed] [Google Scholar]
- 8. Frank R, Larimore J. Yoga as a method of symptom management in multiple sclerosis. Front Neurosci. 2015;9:133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Levin AB, Hadgkiss EJ, Weiland TJ, Jelinek GA. Meditation as an adjunct to the management of multiple sclerosis. Neurol Res Int. 2014;2014:704691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Najafidoulatabad S, Mohebbi Z, Nooryan K. Yoga effects on physical activity and sexual satisfaction among Iranian women with multiple sclerosis: a randomized controlled trial. Afr J Tradit Complement Altern Med. 2014;11:78–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Namjooyan F, Ghanavati R, Majdinasab N, Jokari S, Janbozorgi M. Uses of complementary and alternative medicine in multiple sclerosis. J Tradit Complement Med. 2014;4:145–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tavee J, Rensel M, Planchon SM, Butler RS, Stone L. Effects of meditation on pain and quality of life in multiple sclerosis and peripheral neuropathy: a pilot study. Int J MS Care. 2011;13:163–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Grossman P, Kappos L, Gensicke H, et al. MS quality of life, depression, and fatigue improve after mindfulness training: a randomized trial. Neurology. 2010;75:1141–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Levin AB, Hadgkiss EJ, Weiland TJ, et al. Can meditation influence quality of life, depression, and disease outcome in multiple sclerosis? Findings from a large international web-based study. Behav Neurol. 2014;2014:916519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Senders A, Wahbeh H, Spain R, Shinto L. Mind-body medicine for multiple sclerosis: a systematic review. Autoimmune Dis. 2012;2012:567324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ackerman KD, Heyman R, Rabin BS, et al. Stressful life events precede exacerbations of multiple sclerosis. Psychosom Med. 2002;64:916–920. [DOI] [PubMed] [Google Scholar]
- 17. Confavreux C, Vukusic S. The clinical course of multiple sclerosis. Handb Clin Neurol. 2014;122:343–369. [DOI] [PubMed] [Google Scholar]
- 18. Brand S, Holsboer-Trachsler E, Naranjo JR, Schmidt S. Influence of mindfulness practice on cortisol and sleep in long-term and short-term meditators. Neuropsychobiology. 2012;65:109–118. [DOI] [PubMed] [Google Scholar]
- 19. Elder C, Nidich S, Moriarty F, Nidich R. Effect of transcendental meditation on employee stress, depression, and burnout: a randomized controlled study. Perm J. 2014;18:19–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. National Center for Complementary Integrative Health. Relaxation techniques for health. https://nccih.nih.gov/health/stress/relaxation.htm. Accessed December 13, 2017.
- 21. Trakhtenberg EC. The effects of guided imagery on the immune system: a critical review. Int J Neurosci. 2008;118:839–855. [DOI] [PubMed] [Google Scholar]
- 22. Caudell KA. Psychoneuroimmunology and innovative behavioral interventions in patients with leukemia. Oncol Nurs Forum. 1996;23:493–502. [PubMed] [Google Scholar]
- 23. Hudacek KD. A review of the effects of hypnosis on the immune system in breast cancer patients: a brief communication. Int J Clin Exp Hypn. 2007;55:411–425. [DOI] [PubMed] [Google Scholar]
- 24. Lewandowski W, Jacobson A. Bridging the gap between mind and body: a biobehavioral model of the effects of guided imagery on pain, pain disability, and depression. Pain Manag Nurs. 2013;14:368–378. [DOI] [PubMed] [Google Scholar]
- 25. Jones D, Owens M, Kumar M, Cook R, Weiss SM. The effect of relaxation interventions on cortisol levels in HIV-seropositive women. J Int Assoc Provid AIDS Care. 2014;13:318–323. doi:10.1177/2325957413488186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lewandowski W, Jacobson A, Palmieri PA, Alexander T, Zeller R. Biological mechanisms related to the effectiveness of guided imagery for chronic pain. Biol Res Nurs. 2011;13:364–375. [DOI] [PubMed] [Google Scholar]
- 27. Torem MS. Mind-body hypnotic imagery in the treatment of auto-immune disorders. Am J Clin Hypn. 2007;50:157–170. [DOI] [PubMed] [Google Scholar]
- 28. Shrank WH, Choudhry NK. Therapy. Affect and affirmations—a ‘basic’ approach to promote adherence. Nat Rev Cardiol. 2012;9:263–265. [DOI] [PubMed] [Google Scholar]
- 29. Zahourek RP. Trance and suggestion: timeless interventions and implication for nurses in the new millennium. Holist Nurs Pract. 2001;15:73–82. [DOI] [PubMed] [Google Scholar]
- 30. Menzies V, Lyon DE, Elswick RK, Jr, McCain NL, Gray DP. Effects of guided imagery on biobehavioral factors in women with fibromyalgia. J Behav Med. 2014;37:70–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Richardson MA, Post-White J, Grimm EA, Moye LA, Singletary SE, Justice B. Coping, life attitudes, and immune responses to imagery and group support after breast cancer treatment. Altern Ther Health Med. 1997;3:62–71. [PubMed] [Google Scholar]
- 32. Jensen MP, Barber J, Romano JM, et al. A comparison of self-hypnosis versus progressive muscle relaxation in patients with multiple sclerosis and chronic pain. Int J Clin Exp Hypn. 2009;57:198–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-Second Edition (BDI-II). San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 34. Nunnari D, De Cola MC, D’Aleo G, et al. Impact of depression, fatigue, and global measure of cortical volume on cognitive impairment in multiple sclerosis. Biomed Res Int. 2015;2015:519785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46:1121–1123. [DOI] [PubMed] [Google Scholar]
- 36. Vickrey B, Hays RD, Harooni R, Myers LW, Ellison GW. A health-related quality of life measure for multiple sclerosis. Qual Life Res. 1995;4:187–206. [DOI] [PubMed] [Google Scholar]
- 37. Mohr DC, Lovera J, Brown T, et al. A randomized trial of stress management for the prevention of new brain lesions in MS. Neurology. 2012;79:412–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Park N, Peterson C, Seligman MEP. Strengths of character and well-being. J Soc Clin Psychol. 2004;23:603–619. [Google Scholar]