Abstract
Objective: The objective of this study is to determine whether the health effects of smoking and moderate alcohol use persist with aging. Method: Smoking status, alcohol use, and measures of function and health were obtained from 9,704 women aged ≥65 years at baseline and over 10- and 20-year follow-up periods. Adjusted multiple linear and logistic regression and Cox proportional hazard models estimated associations. Results: Current versus never smokers had worse walking speed, self-reported health, difficulty with instrumental activities of daily living (IADLs), and depression at 10 years and higher death rates at 10 and 20 years. Moderate versus never drinkers had better grip strength, walking speed, self-reported health, and less difficulty with IADLs and were less likely to live in nursing homes at 10 years and die at 10 and 20 years. Discussion: Among aging women over 20 years, smoking is associated with worse physical function, including death, while moderate alcohol use is associated with better outcomes.
Keywords: alcohol, smoking, epidemiology, institutionalization, mortality, falls, depression, active life/physical activity
Introduction
Smoking is consistently associated with worse health outcomes and increased mortality in epidemiologic studies (Inoue-Choi et al., 2017; Tran, Falster, Douglas, Blyth, & Jorm, 2015), whereas moderate alcohol use, generally defined as fewer than two drinks per day, is associated with better health and longevity (Chan, von Mühlenb, Kritz-Silverstein, & Barrett-Connor, 2009; Davis et al., 2014; Knott, Coombs, Stamatakis, & Biddulph, 2015; Leon-Munoz, Guallar-Castillón, García-Esquinas, Galan, & Rodríguez-Artalejo, 2017). While these relationships are well established in studies of general populations, their persistence across time in aging cohorts is less clear because of a lack of well-designed prospective studies that evaluate effects on the oldest old. As populations age in societies for which smoking and alcohol use are common, such as the United States, their effects on health are increasingly important to providing effective health care for the elderly.
In a previous study, we demonstrated cross-sectional relationships between smoking, moderate alcohol use, and health at a baseline examination among 9,704 women aged 65 years and older enrolled in the Study of Osteoporotic Fractures (SOF; Nelson et al., 1994). Now, with continued follow-up of the SOF cohort, the objective of the current longitudinal analysis is to determine whether associations between smoking and alcohol use are associated with functional and mortality outcomes obtained at follow-up intervals at 10 and 20 years.
Method
The SOF is a prospective cohort study primarily designed to determine risk factors for osteoporosis, fractures, and other age-related conditions in community-dwelling older women. At the baseline examination, participants completed questionnaires about smoking and alcohol use and functional status and underwent performance-based examinations of neuromuscular function. Selected components of the questionnaires and examinations were repeated during follow-up visits across 20 years or more at the study sites. Procedures were standardized across sites and participant visits and administered by the same SOF investigators, although some individuals collecting data changed over 20 years. Follow-up data for fractures and mortality were collected every 4 to 6 months (>95% follow-up contacts completed), and mortality was verified from death certificates. This analysis is an over 20-year longitudinal study that builds on previous cross-sectional data from the SOF cohort to determine associations of participants’ smoking status and alcohol use and their long-term function and health outcomes. This study was approved by the Kaiser Permanente Institutional Review Board for Northwest and Hawaii (NW-01EHarr-03).
Participants
This analysis includes 9,704 women at least 65 years of age who were enrolled in SOF beginning in 1986 to 1988 and followed longitudinally until death, loss to follow-up, or to April 2016. Enrolled women were recruited from the community irrespective of their baseline osteoporosis status and living independently in one of four areas in the United States including Portland, Oregon; Minneapolis, Minnesota; Baltimore, Maryland; and outside Pittsburgh, Pennsylvania (Cummings et al., 1990). Black women were originally excluded from SOF because of the low incidence of hip fractures in this group; women unable to walk without assistance or those with bilateral hip replacements were also excluded (Cummings et al., 1995).
Smoking and Alcohol Use Categories
Participants’ responses to questionnaires defined categories of smoking status and alcohol use. For smoking, categories included current, former, and never smokers as determined at the time of the final outcome measurement during the initial 10-year follow-up interval. Smoking status was based on this single measure because of the strong association of current smoking and health, and the lack of data to accurately determine cumulative effects of smoking over time. Women who smoked fewer than 100 cigarettes in their lifetime were considered never smokers.
A drink was defined as one 12-oz (360 mL) can of beer, one 5-oz (150 mL) glass of wine, or a mixed drink containing approximately 1¼ oz (38 mL) or a shot of liquor. Women consuming 14 drinks per week or more were considered heavy drinkers and excluded from the analysis (n = 411 at baseline and n = 69 at the 10-year follow-up visit) that focuses on moderate alcohol use. Women who had at least one drink during the month before their baseline or follow-up visits were considered current drinkers, and those who maintained current drinking status at the time of the outcome measurement during the initial 10-year follow-up interval were considered continuous users. Intermittent users were women who reported use of alcohol during at least one follow-up visit prior to the 10-year visit, while never users were those who reported no use at any time. In an additional analysis focusing on alcohol users at baseline, categories were further defined by whether women continued use or quit during the follow-up interval.
Physical and Clinical Function Measures
Outcomes included results of questionnaires, physical function tests, and clinical measures of function obtained at follow-up intervals at 10 and 20 years, or the closest point of follow-up because not all outcomes were measured at the same visits. Measures included grip strength using a handheld Jamar dynamometer (kg); walking speed (time in seconds to walk 6 m at usual pace in m/sec); prevalence of threshold scores for self-reported health (fair/poor/very poor vs. excellent/good health), difficulty with three or more instrumental activities of daily living (IADLs; Ensrud et al., 1994; Ensrud et al., 2007; Ensrud et al., 2008), and depression (score 6 or more on the 15-item Geriatric Depression Scale [Sheikh & Yesavage, 1986]); and prevalence of falls 1 year after a follow-up visit (as reported from postcards sent every 4 months), living in a nursing home, and death after 10- or 20-year follow-up.
Additional covariates were included in regression models. Physical activity at baseline was determined by a modified version of the Harvard Alumni Questionnaire (kilocalories per week; Gregg et al., 2003; Paffenbarger, Wing, & Hyde, 1978). History of a physician diagnosis of stroke was determined at baseline and throughout follow-up visits by questionnaires. At the baseline examination, height was measured using a standard held-expiration technique with a wall-mounted Harpenden stadiometer (Holtain, UK), and weight was recorded with a balance beam scale. Height and weight were used to calculate body mass index (BMI, kg/m2).
Statistical Analysis
Relationships between smoking and alcohol use as defined during the initial 10-year follow-up interval, and function and health measures obtained during both the 10- and 20-year follow-up intervals were examined using multiple linear regression models for continuous dependent measures and multiple logistic regression models for dichotomous outcomes. A Cox proportional hazard model was used to estimate the risk of mortality. Models included age, history of stroke, BMI, clinic site, physical activity at baseline, initial function measure results for serial measures, and follow-up time as covariates. Models estimating the effects of alcohol exposure included smoking status at the time of the final outcome measure, while models estimating the effects of smoking included alcohol-use status over 10 years of follow-up. Using never use of alcohol and never smoking as reference groups, p values, hazard ratios (HRs), or odds ratios (ORs) with 95% confidence intervals (CIs) were determined. Data analysis was performed with SAS v9.4.
Results
Participants
A total of 9,224 SOF participants with a mean baseline age of 71.7 years (range 65-99) provided data for baseline measures (Table 1). Of these, 99.7% were White and 0.3% self-identified as Asian, Hispanic, or other racial or ethnic groups. Participants included 9.1% current smokers who consumed an average of 15.4 cigarettes per day, 28.6% who smoked formerly, and 62.3% who never smoked. Compared with nonsmokers (including former and never smokers), current smokers were younger, had a lower BMI, and expended fewer total kilojoules of activity per week, but had similar rates of stroke. At baseline, 51.8% of participants had an alcoholic drink during the preceding month and were classified as current drinkers (with average of 2.3 drinks per week), 17.2% consumed alcohol in the past but not within the preceding month, and 31.0% said they never consumed alcohol. Compared with nondrinkers (including former and never drinkers), current drinkers were younger, had a lower BMI, expended more total kilojoules of activity per week, and had lower rates of stroke. Current drinking and current smoking were associated with each other (p < .05).
Table 1.
Characteristics of Participants.
| Characteristic | Baseline | 10-year follow-upa | 20-year follow-upa |
|---|---|---|---|
| Participants, n | 9,224 | 6,665 | 2,051 |
| Age, M, year | 71.7 | 81.0 | 88.7 |
| Smoking, n (%) | |||
| Current | 838 (9.1) | 232 (3.8) | 48 (2.4) |
| Former | 2,632 (28.6) | 1,984 (32.7) | 592 (29.5) |
| Never | 5,724 (62.3) | 3,856 (63.5) | 1,368 (68.1) |
| Alcohol useb, n (%) | |||
| Current or continuous | 4,781 (51.8) | 1,565 (25.2) | 573 (28.5) |
| Former or intermittent | 1,584 (17.2) | 3,285 (52.8) | 961 (47.7) |
| Never | 2,859 (31.0) | 1,373 (22.1) | 480 (23.8) |
| Functional outcomes | |||
| Grip strength, M (SD), kg | 22.2 (4.4) | 18.6 (4.5) | 16.1 (4.2) |
| Walking speed, M (SD), m/sec | 1.01 (0.22) | 0.87 (0.23) | 0.72 (0.24) |
| Fair/poor self-reported health, % | 17.1 | 22.8 | 28.5 |
| Difficulty with ≥3 IADLs, % | 11.5 | 22.9 | 42.8 |
| Depression score ≥6, % | 6.4 | 13.5 | 12.4 |
| Falls in the last 12 months, % | 30.0 | 32.3 | 42.4 |
| Lives in nursing home, % | NA | 1.6 | 6.9 |
| Death, % | NA | 68.3 | 69.5 |
Note. IADLs = instrumental activities of daily living; NA = not applicable.
Defined by smoking status at 10 years and alcohol use from baseline to Visit 6 (10-year follow-up).
At baseline, categories include current, former, or never; at follow-up, categories include continuous, intermittent, or never.
The numbers of active participants declined over time to 6,665 at the 10-year follow-up interval and 2,051 at the 20-year follow-up interval for the analysis, primarily due to expected mortality (see Appendix Figure A1).
Smoking and Physical Function
Women who were smokers at the 10-year follow-up interval had consistently poorer outcomes than never smokers for measures of walking speed, fair/poor self-rated health, difficulty with three or more IADLs, depression score of 6 or more, and death, but not grip strength, falls 1 year after the visit, and living in a nursing home, after adjustment for age, history of stroke, BMI, clinic site, physical activity, initial function measure results for serial measures, follow-up time, and current and past alcohol use (Table 2). Comparisons of never smokers with former smokers showed similar results, indicating better outcomes for never smokers. In general, results of measures for former smokers were intermediate between the findings for current and never smokers, although former smokers had significantly weaker grip strength and more falls than nonsmokers.
Table 2.
Smoking: Associations With Clinical Measures of Function at 10- and 20-Year Follow-Up Intervals.
| Measure | Outcome at end of 10-year follow-upa |
Outcome at end of 20-year follow-upa |
||||||
|---|---|---|---|---|---|---|---|---|
| Smoking status |
Smoking status |
|||||||
| Current |
Former |
Never |
Difference |
Current |
Former |
Never |
Difference |
|
| Adjusted M (SE) | p valueb | Adjusted M (SE) | p valueb | |||||
| Grip strength, M, kg | 17.96 (0.28) | 18.07 (0.11) | 18.32 (0.09) | .20, .030 | 16.73 (0.72) | 15.96 (0.22) | 15.92 (0.15) | .26, .87 |
| Walking speed, M, m/sec | 0.80 (0.014) | 0.83 (0.006) | 0.85 (0.005) | .0006, .002 | 0.74 (0.042) | 0.69 (0.013) | 0.69 (0.009) | .29, .63 |
| Prevalence (%) | OR (95% CI) | Prevalence (%) | OR (95% CI) | |||||
| Fair/poor self-reported healthc | 31.9 | 24.0 | 21.6 | 1.98 [1.44, 2.73] 1.32 [1.14, 1.53] |
31.9 | 31.1 | 26.9 | 1.27 [0.65, 2.46] 1.26 [1.00, 1.58] |
| Difficulty with ≥3 IADLs | 25.1 | 23.6 | 22.4 | 1.61 [1.14, 2.28] 1.39 [1.20, 1.62] |
31.0 | 42.2 | 43.3 | 0.73 [0.31, 1.73] 1.03 [0.78, 1.36] |
| Depression score ≥6 | 22.1 | 13.8 | 12.8 | 1.95 [1.30, 2.93] 1.27 [1.04, 1.55] |
13.8 | 15.1 | 11.2 | 1.39 [0.43, 4.52] 1.40 [0.92, 2.13] |
| Any postvisit falls | 31.1 | 34.6 | 33.1 | 1.03 [0.76, 1.40] 1.15 [1.02, 1.31] |
46.7 | 44.8 | 42.5 | 1.21 [0.66, 2.23] 1.09 [0.88, 1.34] |
| ≥2 postvisit falls | 15.6 | 17.7 | 17.3 | 1.07 [0.72, 1.60] 1.15 [0.98, 1.34] |
33.3 | 26.4 | 23.9 | 1.64 [0.85, 3.17] 1.15 [0.90, 1.47] |
| Lives in nursing home | 0.6 | 1.2 | 1.8 | 0.79 [0.18, 3.50] 1.21 [0.72, 2.02] |
8.7 | 6.7 | 6.7 | 1.86 [0.63, 5.52] 1.07 [0.70, 1.63] |
| Prevalence (%) | HR (95% CI) | Prevalence (%) | HR (95% CI) | |||||
| Death | 72.4 | 67.8 | 67.9 | 1.96 [1.67, 2.30] 1.27 [1.19, 1.37] |
70.8 | 70.8 | 68.6 | 1.35 [0.95, 1.92] 1.19 [1.06, 1.34] |
Note. OR = odds ratio; CI = confidence interval; IADLs = instrumental activities of daily living; HR = hazard ratio; BMI = body mass index.
Adjusted for age, history of stroke, BMI, clinic site, physical activity at baseline, outcome measurement at baseline (except nursing home and death), follow-up time, and current and past alcohol use.
For each outcome, the first value listed compares current smokers versus nonsmokers; the second compares former smokers versus nonsmokers.
Fair/poor/very poor versus excellent/good health.
At 20-year follow-up, former smokers had a higher mortality rate compared with never smokers (70.8% vs. 68.6%; HR = 1.19, 95% CI = [1.06, 1.34]). Otherwise, differences between groups were not statistically significant.
Alcohol Use and Physical Function
Women who were continuous drinkers at baseline and across 10 years of follow-up had statistically significantly better function compared with women who had never used alcohol on all measures after adjustment for age, history of stroke, BMI, clinic site, physical activity, initial function measure results for serial measures, follow-up time, and current and past smoking status (Table 3). Women who drank only intermittently during the 10-year follow-up interval had outcomes that were similar to never drinkers except for better self-reported health measures.
Table 3.
Alcohol Use: Associations With Clinical Measures of Function at 10- and 20-Year Follow-Up Intervals.
| Measure | Outcome at end of 10-year follow-upa |
Outcome at end of 20-year follow-upa |
||||||
|---|---|---|---|---|---|---|---|---|
| Alcohol use |
Alcohol use |
|||||||
| Continuous |
Intermittent | Never |
Differenceb |
Continuous | Intermittent | Never | Differenceb |
|
| Adjusted M (SE) | p value | Adjusted M (SE) | p value | |||||
| Grip strength, M, kg | 18.31 (0.14) | 18.07 (0.13) | 17.97 (0.16) | .032, .48 | 16.15 (0.31) | 16.14 (0.28) | 16.32 (0.34) | .57, .51 |
| Walking speed, M, m/sec | 0.85 (0.007) | 0.81 (0.007) | 0.81 (0.008) | <.0001, .40 | 0.73 (0.019) | 0.70 (0.017) | 0.68 (0.020) | .004, .17 |
| Prevalence (%) | OR (95% CI) | Prevalence (%) | OR (95% CI) | |||||
| Fair/poor self-reported healthc | 14.1 | 24.9 | 27.2 | 0.50 [0.40, 0.62] 0.84 [0.71, 0.99] |
23.5 | 30.0 | 31.3 | 0.79 [0.58, 1.08] 0.92 [0.71, 1.20] |
| Difficulty with ≥3 IADLs | 12.2 | 25.8 | 28.4 | 0.53 [0.42, 0.66] 0.95 [0.80, 1.12] |
36.5 | 44.9 | 46.7 | 0.80 [0.56, 1.16] 0.93 [0.68, 1.28] |
| Depression score ≥6 | 7.2 | 15.3 | 16.3 | 0.44 [0.32, 0.59] 0.87 [0.70, 1.09] |
12.1 | 12.3 | 13.5 | 1.05 [0.60, 1.85] 0.83 [0.51, 1.35] |
| Any postvisit falls | 31.3 | 34.2 | 35.0 | 0.79 [0.67, 0.95] 0.88 [0.76, 1.02] |
43.2 | 44.2 | 42.3 | 1.07 [0.81, 1.42] 1.09 [0.85, 1.39] |
| ≥2 postvisit falls | 13.3 | 19.2 | 18.7 | 0.64 [0.51, 0.80] 0.93 [0.77, 1.11] |
24.5 | 25.3 | 24.5 | 0.99 [0.72, 1.37] 1.04 [0.78, 1.37] |
| Lives in nursing home | 0.2 | 2.3 | 1.5 | 0.11 [0.03, 0.36] 1.22 [0.73, 2.05] |
6.8 | 7.4 | 5.6 | 1.11 [0.62, 2.01] 1.33 [0.80, 2.22] |
| Prevalence (%) | HR (95% CI) | Prevalence (%) | HR (95% CI) | |||||
| Death | 59.1 | 70.4 | 74.3 | 0.72 [0.66, 0.79] 0.96 [0.89, 1.04] |
66.0 | 69.7 | 73.3 | 0.79 [0.68, 0.93] 0.92 [0.80, 1.05] |
Note. OR = odds ratio; CI = confidence interval; IADLs = instrumental activities of daily living; HR = hazard ratio; BMI = body mass index.
Adjusted for age, history of stroke, BMI, clinic site, physical activity at baseline, outcome measurement at baseline (except nursing home and death), follow-up time, and current and past smoking status.
For each outcome, the first value listed compares continuous users versus never users; the second compares intermittent users versus never users.
Fair/poor/very poor versus excellent/good health.
At 20-year follow-up, continuous drinkers had a faster walking speed and a lower mortality rate (66.0% vs. 73.3%; HR = 0.79, 95% CI = [0.68, 0.93]) compared with never drinkers. Other differences between groups were not statistically significant.
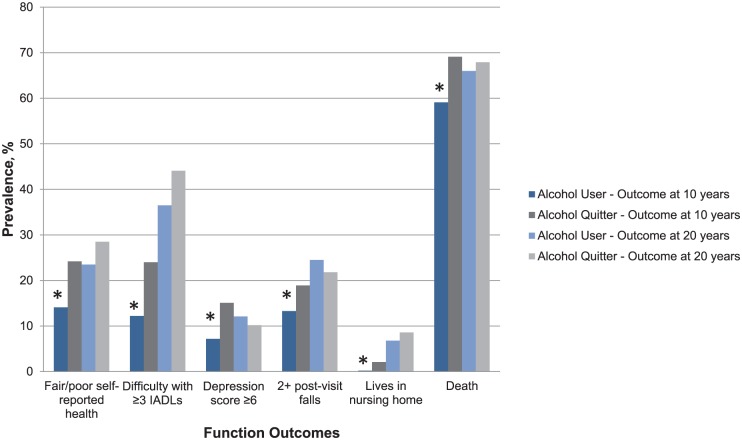
To further evaluate the relationship between continuing use of alcohol over time and better physical and function outcomes, comparisons between ongoing users and women who were drinkers at baseline but quit during the 10-year follow-up interval were also evaluated. Differences between users and quitters were statistically significantly different for all measures (Figure 1), including grip strength (18.51 kg vs. 18.23 kg, p = .046), walking speed (0.87 m/sec vs. 0.83 m/sec, p < .0001), fair/poor self-reported health (14.1% vs. 24.2%; OR = 0.58, 95% CI = [0.47, 0.71]), difficulty with three or more IADLs (12.2% vs. 24.0%; OR = 0.58, 95% CI = [0.47, 0.72]), depression score of 6 or more (7.2% vs. 15.1%; OR = 0.46, 95% CI = [0.35, 0.61]), two or more falls 1 year after the visit (13.3% vs. 18.9%; OR = 0.71, 95% CI = [0.58, 0.87]), living in a nursing home (0.2% vs. 2.1%; OR = 0.11, 95% CI = [0.03, 0.38]), and death (59.1% vs. 69.1%; HR = 0.74, 95% CI = [0.67, 0.80]). Differences between groups were not statistically significant at 20-year follow-up except for mortality (66.0% vs. 67.9%; HR = 0.86, 95% CI = [0.74, 1.00]).
Figure 1.
Function outcomes of alcohol users versus quitters at 10-year and 20-year follow-up.
Note. Drinking status was determined at the 10-year follow-up interval, and prevalence rates were measured at 10-year and 20-year follow-up intervals. IADLs = instrumental activities of daily living.
*Indicates statistically significant difference between prevalence rates of alcohol user and quitter groups measured at 10-year follow-up. Differences measured at 20 years are not statistically significant.
Discussion
In this study of older women followed over 20 years, compared with never smokers, current smokers had worse walking speed, self-reported health, difficulty with IADLs, and depression at 10 years and higher death rates at 10 and 20 years. Compared with never drinkers, moderate drinkers had better grip strength, walking speed, and self-reported health, and less difficulty with IADLs and were less likely to live in nursing homes at 10 years and die at 10 and 20 years. Outcomes were worse for all measures for women who quit using alcohol over 10-year follow-up compared with those who continued. Death was the only outcome consistently associated with smoking or alcohol use at 20 years. It is unclear whether the lack of associations at 20 years was due to the attenuation of the effects of alcohol and smoking over time, attrition of participants and lack of statistical power to detect differences, or survivor bias.
Results of this longitudinal analysis are consistent with our previous cross-sectional estimates of baseline data (Nelson et al., 1994). In this study, current smokers had significantly poorer function on 11 of 12 measures of neuromuscular and physical performance compared with nonsmokers, and most measures worsened with increasing numbers of pack-years. Current moderate drinkers had better function on 11 of 12 measures compared with nondrinkers. The effects of higher levels of alcohol use could not be determined in this study because only few women used higher amounts. Our cross-sectional analysis was unable to describe whether these associations persist over time. These relationships are particularly important as women age because the performance tests evaluated in the study are essential to independence in many basic and IADLs, and healthy aging is dependent upon maintaining function.
This longitudinal analysis is unique in measuring specific serial function and health outcomes in a cohort of healthy older women over a 20-year period as they advance to become the “oldest old” of their generation. Prior studies have rarely evaluated the oldest old and have been generally limited by their cross-sectional designs, shorter follow-up times, and less rigorous and standardized data collection and assessment of functional outcomes and mortality.
While the effects of smoking on health are well established, few studies focus specifically on smoking in older individuals. A large study of middle age and older Australian men and women demonstrated strong dose-response relationships between smoking duration, intensity, and cumulative smoking doses on risk for hospitalization (Tran et al., 2015). In a study of American men and women aged 59 to 82 years, long-term, low-intensity smoking as low as one cigarette per day was associated with higher all-cause mortality and several smoking-related causes of death, particularly lung cancer (Inoue-Choi et al., 2017). In both studies, smoking cessation, even at older ages, reduced risks for adverse outcomes.
Previous studies of older individuals comparing alcohol users with nonusers also report benefits. These include higher global cognitive function scores (Davis et al., 2014); reduced functional limitations including mobility, agility, and IADLs (Leon-Munoz et al., 2017); better quality of life measures (Chan et al., 2009); and reduced likelihood of placement in long-term care facilities (Kaplan et al., 2014). How alcohol exerts these beneficial effects is not clear, and it may be best explained by the intrinsic differences between drinking groups rather than through biological mechanisms. Associations between moderate alcohol use and health outcomes were markedly attenuated after controlling for socioeconomic status indicators in a large study of men and women aged 50 years and older (Knott et al., 2015). In this study, higher socioeconomic status facilitated regular alcohol use as well as better health. The concept that moderate alcohol use serves as a marker of health is further supported by studies comparing users and quitters who consistently have worse health measures (Davis et al., 2014; Knott et al., 2015). This relationship was confirmed in the current study by the poorer function and health of the quitters in SOF cohort. Quitting alcohol or smoking could be secondary to deteriorating health, moving to a care facility, or limited mobility.
Strengths of this study include the large number of participants who were initially selected to represent healthy, community-dwelling women from four different geographic areas of the United States. Data were prospectively collected over a 20-year period with high levels of participation, follow-up, and data capture. The study used repeated standardized measures of smoking, alcohol use, and function and health that allowed direct comparisons across time. Many additional social, demographic, lifestyle, and health measures were collected in SOF, and some of these served as confounder variables in the regression models. The distributions of never, former, and current smokers and never, former, and current moderate alcohol users in SOF were similar to other epidemiologic studies (Chan et al., 2009; Towers, Philipp, Dulin, & Allen, 2016; Tran et al., 2015), increasing the likelihood that participants reflected general populations. However, because this study enrolled predominantly White women, the applicability of results to women of other racial and ethnic groups may be limited.
This study has several additional limitations. As an observational study, it cannot establish causality, but only describe associations between smoking, moderate alcohol use, and health outcomes. However, because the chronic effects of smoking and alcohol use can never be evaluated in randomized controlled trials, these relationships are best determined by large, long-term prospective studies, such as SOF. Although observational studies are inherently limited by confounding and selection bias, studies that enroll large population-based participants, consider multiple confounders, and prospectively collect data aim to minimize these limitations.
In addition, the number of current smokers in the study is low, particularly at the 20-year follow-up interval, reducing statistical power for comparisons between groups. Smoking and alcohol use were based on self-report, which could be inaccurate, particularly if participants considered these habits socially unacceptable. Also, the role of socioeconomic status could not be evaluated because it was not routinely collected over time. While the high overall attrition rate due to deaths is expected in a longitudinal study of older women, survivor bias may underestimate effects.
Future studies should address current research gaps and include additional populations, such as men and non-White individuals. The role of important social determinants of health, such as socioeconomic status, community, and family support, should also be considered in examining the relationships between smoking, alcohol use, and functional outcomes. Identifying predictors of desirable outcomes could ultimately lead to studies of interventions or health practices that could help maintain function.
In conclusion, in a cohort of older women followed over 20 years, smoking is associated with worse physical function and health, including death, while moderate alcohol use is associated with better outcomes. Alcohol use may serve as a marker of function and health in societies where it is common and related to social activity, and quitting alcohol may signal a decline in health among older women. These findings may inform patients’ health decisions to optimize their health as they age, particularly regarding smoking cessation and moderate alcohol use.
Appendix
Figure A1.
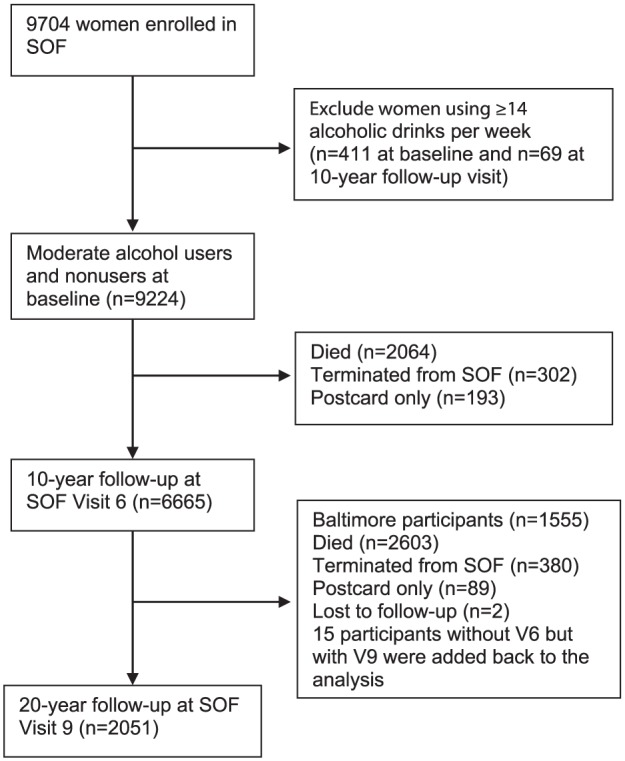
Participant flow chart.
Note. SOF = Study of Osteoporotic Fractures.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The Study of Osteoporotic Fractures (SOF) is supported by National Institutes of Health funding. The National Institute on Aging (NIA) provides support under the following grant numbers: R01 AG005407, R01 AR35582, R01 AR35583, R01 AR35584, R01 AG005394, R01 AG027574, R01 AG027576, and R01 AG026720.
References
- Chan A. M., von Mühlenb D., Kritz-Silverstein D., Barrett-Connor E. (2009). Regular alcohol consumption is associated with increasing quality of life and mood in older men and women: The Rancho Bernardo Study. Maturitas, 62, 294-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings S. R., Black D. M., Nevitt M. C., Browner W. S., Cauley J. A., Genant H. K., . . . Vogt T. M. (1990). Appendicular bone density and age predict hip fracture in women. Journal of the American Medical Association, 263, 665-668. [PubMed] [Google Scholar]
- Cummings S. R., Nevitt M. C., Browner W. S., Stone K., Fox K. M., Ensrud K. E., . . . Vogt T. M. (1995). Risk factors for hip fracture in White women. New England Journal of Medicine, 332, 767-774. [DOI] [PubMed] [Google Scholar]
- Davis B. J. K., Vidal J., Garcia M., Aspelund T., van Buchem M. A., Jonsdottir M. K., . . . Launer L. J. (2014). The alcohol paradox: Light-to-moderate alcohol consumption, cognitive function, and brain volume. The Journals of Gerontology, Series A: Biological Sciences & Medical Sciences, 69, 1528-1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ensrud K. E., Ewing S. K., Taylor B. C., Fink H. A., Cawthon P. M., Stone K. L., . . . Cummings S. R. (2008). Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Archives of Internal Medicine, 168, 382-389. [DOI] [PubMed] [Google Scholar]
- Ensrud K. E., Ewing S. K., Taylor B. C., Fink H. A., Stone K. L., Cauley J. A., . . . Cawthon P. M. (2007). Frailty and risk of falls, fracture, and mortality in older women: The study of osteoporotic fractures. The Journals of Gerontology, Series A: Biological Sciences & Medical Sciences, 62, 744-751. [DOI] [PubMed] [Google Scholar]
- Ensrud K. E., Nevitt M. C., Yunis C., Cauley J. A., Seeley D. G., Fox K. M., Cummings S. R. (1994). Correlates of impaired function in older women. Journal of the American Geriatrics Society, 42, 481-489. [DOI] [PubMed] [Google Scholar]
- Gregg E. W., Cauley J. A., Stone K., Thompson T. J., Bauer D. C., Cummings S. R. , . . . Study of Osteoporotic Fractures Research Group. (2003). Relationship of changes in physical activity and mortality among older women. Journal of the American Medical Association, 289, 2379-2386. [DOI] [PubMed] [Google Scholar]
- Inoue-Choi M., Liao L. M., Reyes-Guzman C., Hartge P., Caporaso N., Freedman N. D. (2017). Association of long-term, low-intensity smoking with all-cause and cause-specific mortality in the National Institutes of Health–AARP Diet and Health Study. Journal of the American Medical Association Internal Medicine, 177, 87-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan M. S., Huguet N., Feeny D., McFarland B. H., Caetano R., Bernier J., . . . Ross N. A. (2014). The association between alcohol use and long-term care placement among older Canadians: A 14-year population-based study. Addictive Behaviors, 39, 219-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knott C. S., Coombs N., Stamatakis E., Biddulph J. P. (2015). All cause mortality and the case for age specific alcohol consumption guidelines: Pooled analyses of up to 10 population based cohorts. British Medical Journal, 350, Article h384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon-Munoz L., Guallar-Castillón P., García-Esquinas E., Galan I., Rodríguez-Artalejo F. (2017). Alcohol drinking patterns and risk of functional limitations in two cohorts of older adults. Clinical Nutrition, 36, 831-838. [DOI] [PubMed] [Google Scholar]
- Nelson H. D., Nevitt M. C., Scott J. C., Stone K. L., Cummings S. R., Nevitt M. C., . . . Franco D. (1994). Smoking, alcohol, and neuromuscular and physical function of older women. Journal of the American Medical Association, 272, 1825-1831. [DOI] [PubMed] [Google Scholar]
- Paffenbarger R. S., Jr., Wing A. L., Hyde R. T. (1978). Physical activity as an index of heart attack risk in college alumni. American Journal of Epidemiology, 108, 161-175. [DOI] [PubMed] [Google Scholar]
- Sheikh J. I., Yesavage J. A. (1986). Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. Clinical Gerontologist: The Journal of Aging and Mental Health, 5, 165-173. [Google Scholar]
- Towers A., Philipp M., Dulin P., Allen J. (2016). The “health benefits” of moderate drinking in older adults may be better explained by socioeconomic status. The Journals of Gerontology, Series B: Psychological Sciences & Social Sciences: gbw152. Retrieved from https://doi.org/10.1093/geronb/gbw15210.1093/geronb/gbw152 [DOI] [PubMed]
- Tran B., Falster M. O., Douglas K., Blyth F., Jorm L. R. (2015). Smoking and potentially preventable hospitalisation: The benefit of smoking cessation in older ages. Drug and Alcohol Dependence, 150, 85-91. [DOI] [PubMed] [Google Scholar]