Abstract
Foot osteoarthritis (OA) is a common problem in older adults yet is under-researched compared to knee or hand OA. Most existing studies focus on the first metatarsophalangeal joint, with evidence relating to midfoot OA being particularly sparse. Symptomatic radiographic foot OA affects 17% of adults aged 50 years and over. The first metatarsophalangeal joint is most commonly affected, followed by the second cuneometatarsal and talonavicular joints. Epidemiological studies suggest the existence of distinct first metatarsophalangeal joint and polyarticular phenotypes, which have differing clinical and risk factor profiles. There are few randomized controlled trials in foot OA. Existing trials provide some evidence of the effectiveness for pain relief of physical therapy, rocker-sole shoes, foot orthoses and surgical interventions in first metatarsophalangeal joint OA and prefabricated orthoses in midfoot OA. Prospective epidemiological studies and randomized trials are needed to establish the incidence, progression and prognosis of foot OA and determine the effectiveness of both commonly used and more novel interventions.
Keywords: epidemiology, foot osteoarthritis, randomized controlled trials, treatment
Introduction
Symptomatic osteoarthritis (OA) affects 10% of people aged over 60 years and is the leading global cause of years lost to disability in older people.1,2 Musculoskeletal problems are the commonest reason for consultation in primary care, and OA accounts for 15% of these in people aged 45 years and over.3 OA leads to significant impairments of quality of life,4 locomotor function,5 social participation6 and economic productivity.7 The foot was included in early descriptions of generalized OA,8 yet most subsequent OA research has focused on the knee, hip and hand. A systematic review of population-based epidemiological studies of radiographic foot OA published in 2010 identified only 27 publications arising from 22 studies.9 This contrasts greatly with the findings of similar reviews published 2 years earlier which identified 176 population-based epidemiological studies of radiographic hand OA10 and 190 studies that had applied the Kellgren and Lawrence (K&L) grading system to knee OA.11 A Cochrane review published in 2010 included only one randomized trial of interventions for first metatarsophalangeal (MTP) joint OA.12
OA seems likely to be a significant cause of foot pain in older people, in whom painful foot disorders are major contributors to restricted activity, locomotor disability, poor balance and risk of falling, and account for a substantial number of healthcare consultations.13–16 The prevalence and incidence of foot pain and related disability increase with age. Foot pain affects one in four people aged over 75 years, two-thirds of whom have related locomotor disability.15,17,18 One in 10 people aged over 70 years will develop new disabling foot pain over a 3-year period.19
A significant barrier to the study of foot OA has been the lack of a foot-specific grading system to define radiographic foot OA. The majority (90%) of studies included in the recent systematic review used the K&L grading system which is widely used to grade radiographic OA at a range of different joint sites.20,21 While a generic system such as K&L has the advantage of allowing prevalence and features of OA at different sites to be compared, it has been criticized for relying heavily on the presence of osteophyte and for grading features of OA in such a way that assumes osteophyte formation chronologically precedes joint space narrowing and subchondral sclerosis in the pathogenesis of OA.22–24 A further shortcoming has been said to be inconsistent interpretation and application of the grades between studies.11 A major recent advance therefore has been the advent of a foot-specific radiographic atlas and grading system to score radiographic features (osteophytes and joint space narrowing) of foot OA.25 This atlas grades features of OA at five different foot joints: the first MTP, first and second cuneometatarsal (CMT), navicular first cuneiform (NC), and talonavicular (TN) joints (Figure 1). These joints were chosen as they are easily visualized on dorsoplantar and lateral views and were considered by the authors to be the foot joints most commonly affected by OA. Hence, this atlas does not provide a means to grade OA occurring in the lateral column or hindfoot. It has the advantages, however, of scoring osteophytes and joint space narrowing separately (Figures 2 and 3) and requiring weight-bearing dorsoplantar and lateral views, addressing the observation that existing studies frequently failed to specify whether radiographs were weight-bearing or obtained only a single radiographic view.9 Obtaining more than one view allows greater accommodation of the specific features of individual joints. For example, osteophytes at the TN joint are most commonly visualized on the lateral view, whereas joint space narrowing at the second CMT joint is more easily assessed on the dorsoplantar than the lateral view (Figure 3). Osteophytes (absent = 0, small =1, moderate = 2, severe = 3) and joint space narrowing (absent = 0, definite = 1, severe = 2, joint fusion = 3) are scored separately on a 0–3 scale on both the dorsoplantar and lateral views. Radiographic OA is present at a specific joint if there is a score of at least 2 for either osteophyte or joint space narrowing on either the dorsoplantar or lateral view. Intra-rater reliability was moderate to excellent (weighted κ 0.45–0.95) whereas inter-rater reliability was lower (weighted κ 0.13–0.87), consistent with reliability studies at the hip and knee.26
Figure 1.
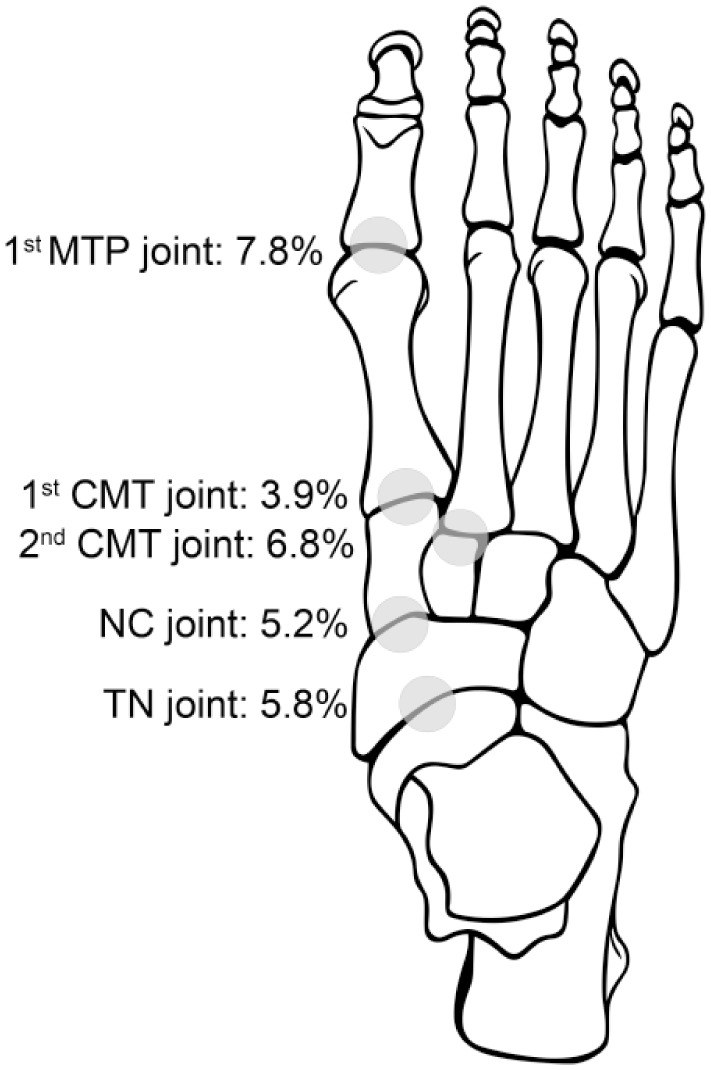
Population prevalence of symptomatic radiographic OA in joints of the foot.
MTP, metatarsophalangeal; CMT, cuneometatarsal; NC, navicular-cuneiform; TN, talonavicular. From Roddy and colleagues.27
Figure 2.

Radiographic appearance of first metatarsophalangeal joint osteoarthritis. Open arrow indicates joint space narrowing and filled-in arrow indicates osteophyte.
Figure 3.

Radiographic appearance of midfoot osteoarthritis. Arrows indicate first cuneometatarsal and second cuneometatarsal joint space narrowing.
In this perspective review, we discuss recent advances in the published literature concerning the epidemiology, diagnosis and treatment of foot OA.
Epidemiology of foot OA: prevalence and incidence
The systematic review of population-based epidemiological studies of radiographic foot OA9 identified seven studies that used similar methods to estimate the prevalence of radiographic OA affecting the first MTP joint.28–34 Defining OA as a K&L grade 2 or above, the prevalence of radiographic first MTP joint OA ranged from 6.3% in rural African women aged 40 years and over28 to 39% in women aged 35–64 years resident in Wensleydale, UK.29 Radiographic first MTP joint OA was more common in women than men (Table 1). Although few studies were identified that used the same definition to provide population prevalence estimates for radiographic OA at other sites within the foot, OA at these sites appeared to occur less frequently than at the first MTP joint. One study reported estimates for the prevalence of radiographic OA affecting the second to fifth MTP joints of 2% of men and 5% of women in Wensleydale, UK and 3% in both men and women in Jamaica.29 Two studies have reported population prevalences from Zoetermeer in the Netherlands.30,31 In the first study of adults aged 45–64 years, the prevalence of radiographic OA was 4.3% in men and 5.4% in women at the second to fifth MTP joints, 4.3% in men and 5.0% in females at the tarsometatarsal joints, and 6.7% in men and 7.2% at the proximal interphalangeal joints.30 In the second study of adults aged 19 years or over, similar prevalences of 3.4% in men and 4.7% in women at the second to fifth MTP joints, 3.1% in men and 3.3% in women at the tarsometatarsal joints, and 4.3% in men and 4.5% in women at the proximal interphalangeal joints were reported.31 Much higher prevalences were reported for midfoot OA in a population of retirement village residents in Australia: first CMT joint 23%, second CMT joint 60%, NC joint 39%, TN joint 33%.35
Table 1.
Prevalence of radiographic foot osteoarthritis.
| First author | Country | Age (years) | Radiographic definition | Joint | Prevalence (%) | Prevalence in men (%) | Prevalence in women (%) |
|---|---|---|---|---|---|---|---|
| Bremner29 | Jamaica | 35–64 | K&L ⩾ 2 | First MTP joint | 23 | 17 | 29 |
| Second to fifth MTP joints | 3 | 3 | 3 | ||||
| Bremner29 | UK | 35–64 | K&L ⩾ 2 | First MTP joint | 35 | 30 | 39 |
| Second to fifth MTP joints | 3.5 | 2 | 5 | ||||
| Brighton28 | South Africa | >18 | K&L ⩾ 2 | First MTP joint | 5.0 | 11.1 | 2.5 |
| Solomon33 | South Africa | >35 | K&L ⩾ 2 | First MTP joint | 21.5 | 15.1 | 24.0 |
| Menz35 | Australia | 62–94 | Menz atlas ⩾ 2 | First MTP joint | 42.4 | – | – |
| First CMT joint | 22.6 | – | – | ||||
| Second CMT joint | 60.2 | – | – | ||||
| NC joint | 39.1 | – | – | ||||
| TN joint | 32.7 | – | – | ||||
| Van Sasse31 | The Netherlands | 45–64 | K&L ⩾ 2 | First MTP joint | 33.1 | 28.5 | 37.6 |
| Second to fifth MTP joints | 4.9 | 4.3 | 5.4 | ||||
| Tarsometatarsal joints | 4.7 | 4.3 | 5.0 | ||||
| Toe PIP joints | 7.0 | 6.7 | 7.2 | ||||
| Van Sasse30 | The Netherlands | ⩾19 | K&L ⩾ 2 | First MTP joint | 22.7 | 20.0 | 25.0 |
| Second to fifth MTP joints | 4.1 | 3.4 | 4.7 | ||||
| Tarsometatarsal joints | 3.2 | 3.1 | 3.3 | ||||
| Toe PIP joints | 4.4 | 4.3 | 4.5 | ||||
| Wilder32 | USA | 40–94 | K&L ⩾ 2 | First MTP joint | 20.0 | 25.1 | 17.7 |
| Wilder34 | USA | ⩾40 | K&L ⩾ 2 | First MTP joint | 20.0 | – | – |
CMT, cuneometatarsal; K&L, Kellgren and Lawrence; MTP, metatarsophalangeal; NC, navicular first cuneiform; PIP, proximal interphalangeal joints; TN, talonavicular.
The studies identified by this review focused on the presence of radiographic OA without considering its contribution to symptoms. However, a recent population-based study has reported the prevalence of symptomatic radiographic foot OA, requiring the presence of pain and radiographic OA at the same location in the foot. The Clinical Assessment Study of the Foot recruited 5109 adults aged 50 years and over registered with four general practices in North Staffordshire, UK.27 Defining radiographic foot OA using the foot atlas described above, the population prevalence of symptomatic radiographic foot OA was 16.7% [95% confidence interval (CI) 15.3%, 18.0%]. The most commonly affected joint was the first MTP joint (7.8%; 95% CI 6.7%, 8.9%). Symptomatic radiographic OA at any one of the four midfoot joints included in the atlas affected 12.0% of participants (95% CI 10.9, 13.2).36 The most commonly affected individual joint in the midfoot was the second CMT joint (prevalence 6.8%; 95% CI 5.7%, 7.8%), followed by the TN (5.8%; 95% CI 4.8%, 6.9%), NC (5.2%; 95% CI 4.0%, 6.4%) and first CMT (3.9%; 95% CI 2.9%, 4.9%) joints (see Figure 1).27
There have been far fewer population-based estimates of the incidence of radiographic foot OA. In the Clearwater Osteoarthritis Study, a community-based longitudinal cohort study of risk factors for the development and progression of OA in 1592 adults aged 40–91 years who were free of radiographic first MTP joint OA (defined as K&L grade ⩾2) at baseline, 25% developed first MTP joint OA in the left foot and 27% in the right foot over an average follow up of 7 years.37
Phenotypes of foot OA and associated risk factors
As summarized above, most studies to date have focused on the first MTP joint and have neglected other foot joints such as those in the midfoot. Hence, little is known about symmetry and clustering of OA at different joints in the feet. Better understanding of patterns of involvement across different joints in the feet and associated risk factor profiles has the potential to provide new insights into aetiology and the relative contributions of systemic and local biomechanical factors, and hence guide the development of new interventions for foot OA. In the Clinical Assessment Study of the Foot, radiographic OA clustered significantly within individuals more than was expected by chance when both feet were considered together but not for the left or right foot separately.38 Radiographic first MTP joint OA most commonly occurred in isolation from the other joints in the affected foot, whereas OA in the midfoot joints tended to co-occur with OA in other joints in the same foot. Involvement was highly symmetrical, with the NC joint being the most likely to be affected symmetrically. Latent class analysis identified three distinct classes of foot OA in the cohort of 560 people with foot pain: no/minimal foot OA (64%), isolated first MTP joint OA (22%), and polyarticular foot OA (15%). The isolated first MTP joint class had high probabilities of radiographic OA in the first MTP joint in both the left and right feet, but low probabilities of midfoot involvement. The polyarticular class had medium-to-high probabilities of OA in both second CMT and NC joints with medium probabilities of OA in the TN joints and first MTP joints. The isolated first MTP joint and polyarticular foot OA classes were significantly older than the no/minimal foot OA subgroup. The polyarticular class had a higher probability of being female and having nodal hand OA, and more persistent and severe pain, greater functional impairment and higher BMI than the other classes. The association of the polyarticular class with female gender and nodal OA raises the possibility that polyarticular foot OA could be a form of generalized OA.39 Since first MTP joint involvement was common both as an isolated phenomenon and in association with midfoot OA, it is also possible that isolated first MTP joint OA is a precursor to more widespread polyarticular foot OA. However, longitudinal studies are required to examine this.
A number of studies have investigated the association between foot posture and radiographic first MTP joint OA. A systematic review of case-control studies of structural factors associated with hallux rigidus/limitus found two studies that reported no difference in arch height between people with and without hallux rigidus/limitus.40 In contrast, in the Clinical Assessment Study of the Foot, three measures of static foot posture each showed a trend of a flatter or more pronated foot with more severe radiographic first MTP joint OA.41 There was also a dose–response relationship between radiographic severity and hallux valgus, first interphalangeal joint hyperextension, dorsal keratotic skin lesions, and reduced range of first MTP joint dorsiflexion, ankle/subtalar joint eversion and ankle joint dorsiflexion, suggesting that first MTP joint OA has structural and biomechanical consequences for the whole foot–ankle complex. Prospective data from the Clearwater Osteoarthritis Study found that having a hindfoot valgus deformity of greater than 5º was a risk factor for subsequent development of radiographic first MTP joint OA.37 It has been postulated that excessive foot pronation increases plantar fascial tension, which in turn impairs hallux dorsiflexion and predisposes to first MTP joint OA.42 The Clearwater Osteoarthritis Study also found that radiographic OA affecting the knee, finger interphalangeal joints and first carpometacarpal joints occurs more commonly in people with first MTP joint OA, again suggesting that foot OA may be a component of generalized OA.32
Although isolated midfoot OA appears to be an uncommon phenomenon, symptomatic midfoot OA was found to be more common in females, in lower socioeconomic classes and with older age in the Clinical Assessment Study of the Foot, but was also associated with obesity, previous injury and pain at all other weight-loaded joint sites, but not nodal interphalangeal joint OA.36 Furthermore, patients with midfoot OA have flatter feet and higher midfoot plantar pressures during barefoot walking than controls without midfoot OA, and these plantar pressures have been shown to correlate with midfoot pain severity.36,43–45 These findings fit with a hypothesis that mechanical loading may play an important role in the aetiology of symptomatic and structural midfoot OA. Different studies have reported that the second CMT joint is more commonly affected by symptomatic and radiographic OA by other joints in the midfoot.25,27,35,36 The anatomical location of the second CMT joint at the apex of the transverse arch and its recessed position relative to the first and third metatarsals potentially render it more vulnerable to adverse mechanical stresses.46
Diagnosis of foot OA
Plain radiographs are widely used to diagnose foot OA in clinical practice. Attempts to develop robust clinical diagnostic prediction rules have been more successful at the first MTP joint than the midfoot. In a study of 181 people with first MTP joint pain, a diagnostic rule incorporating pain duration greater than 25 months, the presence of a dorsal exostosis, hard end-feel, crepitus and less than 64º of first MTP joint dorsiflexion was found to accurately predict the presence or absence of first MTP joint OA.47 The presence of three or more of these five features had a sensitivity of 88%, specificity of 71%, accuracy of 84%, positive likelihood ratio of 3.07 and negative likelihood ratio of 0.17. In contrast, a study of 274 adults aged 50 years and over with midfoot pain found that brief clinical assessment added little to demographic and anthropometric characteristics in the differentiation of people with and without radiographic midfoot OA.48 Although the presence of radiographic midfoot OA was associated with a number of measures of static foot posture and range of movement, the final model retained only the arch index (a measure of static foot posture derived from a carbon paper foot imprint49) in addition to age, gender and body mass index. However, the sensitivity and specificity of this final model were 30% and 88%, respectively. At present, therefore, the diagnosis of symptomatic midfoot OA continues to require imaging to augment clinical history and examination.
Management of foot OA
Management of foot OA generally commences with conservative interventions, including analgesic or anti-inflammatory medications, intra-articular injections, physical therapy, footwear modifications and foot orthoses.50–53 If these treatments are ineffective, surgical options may be considered. However, in contrast to OA affecting other body regions, the body of evidence examining the effectiveness of treatments for foot OA is meagre. A Cochrane systematic review published in 2010 found only one randomized trial of physical therapy for the treatment of first MTP joint OA.12 Since the publication of this review, two conservative trials54,55 and one surgical trial56 for first MTP joint OA have been completed, but only one pilot trial has so far been conducted for midfoot OA.57 Clinical guidelines for the treatment of first MTP joint OA have been published by the American College of Foot and Ankle Surgeons,58 but no such guidelines are available for midfoot OA.
Nevertheless, clinical audit data suggest that many patients appear to benefit from conservative treatment. In a 14-year follow-up study of 22 people with first MTP joint OA who had elected not to have surgery, only one reported that their pain had worsened over time, and 16 (73%) would still choose not to have surgery if they had to make the decision again. A large proportion of these patients had changed their footwear to that with more room in the toe-box, suggesting that selection of appropriate footwear may be a sufficient stand-alone treatment in some individuals.59 Similar findings were reported by Grady and colleagues,60 who reviewed 772 cases of first MTP joint OA over a 7-year period and reported that just over half were successfully managed with conservative care alone, defined as a marked reduction in discomfort and return to previous activity levels. Of these, 84% were managed with foot orthoses, 10% with intra-articular corticosteroid injections and 6% with a change in footwear.
Pharmacological management
Oral non-steroidal anti-inflammatory drugs (NSAIDs) are the most widely used first-line pharmacological treatment for OA. Only one study has specifically evaluated the effectiveness of NSAIDs for foot OA, concluding that piroxicam and naproxen were similarly effective at reducing pain over an 8-week period.61 Nevertheless, it is reasonable to assume that the findings from studies of OA in other joints are broadly generalizable to the foot. The most recent network meta-analysis of 74 randomized trials of eight medications (seven different NSAIDs and paracetamol) in people with knee or hip OA concluded that all NSAIDs were more effective at reducing pain compared to placebo. Diclofenac at the maximum daily dose of 150 mg/day was found to be more effective than the maximum doses of frequently used NSAIDs such as ibuprofen, naproxen and celecoxib, while paracetamol was not effective at any dose.62 However, choice of NSAID for individual patients should be informed by considerations of their comparative side-effect profiles in the context of the patient’s comorbidities as well as the likelihood of effectiveness.
Topical medications are also commonly used in the management of foot OA, particularly when there are concerns regarding the gastrointestinal and cardiovascular side effects of oral NSAIDs. However, to our knowledge, there are no studies of topical therapies for foot OA. Evidence from systematic reviews suggests that topical diclofenac and ketoprofen are effective at reducing pain in knee OA,63 and capsaicin, the neurotoxin derived from chilli, reduces pain in both knee and hand OA.64 However, salicylate-containing rubefacient creams do not appear to be effective in the management of symptoms associated with OA.65
Intra-articular injections
A wide range of intra-articular preparations have been trialled for the treatment of OA, the most widely used being corticosteroid injection. In people with knee OA, meta-analyses indicate that intra-articular injection of corticosteroid produces moderate improvements in pain but only small improvements in physical function up to 6 weeks following treatment.66 No placebo-controlled trials of intra-articular corticosteroid have been conducted for foot OA. However, a clinical audit of 73 people with midfoot OA and 22 with first MTP joint OA reported that corticosteroid injection was effective at reducing pain in the short term, although between 30% and 50% of patients required surgery within 2 years.67 Similarly, a case series of 59 patients with midfoot OA who underwent ultrasound-guided corticosteroid injection reported that while 78% of patients experienced pain relief at 2 weeks, this had reduced to 15% at 3 months post-injection.68
Viscosupplementation, the intra-articular injection of a lubricating fluid (hyaluronan) with the aim of restoring the viscoelasticity of the synovial fluid, has attracted considerable interest in recent years. However, the effectiveness of this treatment is uncertain.69 Two case-series studies of viscosupplementation for first MTP joint OA reported significant reductions in joint pain,70,71 and one small randomized trial of 37 patients with hallux rigidus or hallux valgus reported that hyaluronan injection was more effective at reducing gait-related pain than corticosteroid injection.72 However, the only randomized controlled trial so far undertaken found intra-articular injection of hyaluronan to be no more effective at reducing pain (using the pain subscale of the Foot Health Status Questionnaire) than a saline placebo in the treatment of 151 people with first MTP joint OA.54 No randomized trials of viscosupplementation have yet been undertaken for midfoot OA.
Physical therapy
Mobilization of the sesamoid apparatus and strengthening of hallux plantarflexors may provide some benefit in the conservative management of first MTP joint OA. Shamus and colleagues73 conducted a small trial in which one group of patients were provided with whirlpool, therapeutic ultrasound, first metatarsophalangeal joint mobilization, calf stretching, toe-strengthening exercises, cold packs and electrical stimulation, and the second group were provided with each of these interventions in addition to distal gliding mobilizations of the sesamoids, hallux plantarflexor-strengthening exercises and gait training. After 12 therapy sessions, the group who received the sesamoid mobilizations exhibited greater improvements in first MTP joint range of motion, toe flexor strength and pain levels (using a 0–10 verbal analogue scale).
Manipulation may also be performed in conjunction with corticosteroid and local anaesthetic injection for first MTP joint OA, although the therapeutic benefits of this technique appear to be limited to milder forms of the condition. Solan and colleagues74 reported that patients with mild OA obtained symptomatic relief for a median of six months, and only one-third required surgery. However, in more advanced cases, little symptomatic relief was obtained and all patients eventually required surgery.
Footwear
Footwear modification plays a key role in the conservative management of foot OA, by modifying the load distribution of the foot when walking. In individuals with first MTP joint OA, pain generally occurs during the propulsive phase of gait when the proximal phalanx is compressed against the first metatarsal head. This can be addressed using a footwear modification known as a rocker-sole, in which the sole of the shoe is curved.75 The aim of this modification is to allow the body’s centre of mass to ‘roll over’ the base of support, reducing the need for first MTP joint dorsiflexion. Biomechanical studies indicate that wearing rocker-sole shoes reduces peak pressure under the first MTP joint by 12% in individuals with OA,76 and a recent randomized trial comparing rocker-sole shoes with prefabricated foot orthoses in 102 people with first MTP joint OA found that both groups demonstrated a significant reduction in symptoms over a 12-week period. For the rocker-sole group, the Foot Health Status Questionnaire pain score improved by 22 points, which exceeds the minimal important difference for this outcome measure (13 points).55
Foot orthoses
Foot orthoses are inserts placed inside the shoe with the goal of altering the magnitude and location of forces acting on the plantar surface of the foot. For foot OA, two main types of orthosis are commonly used: (1) shoe-stiffening inserts, which are manufactured from a flat, thin, semi-rigid material and generally extend the full length of the shoe; and (2) contoured orthoses, which contour the arch of the foot and generally extend just proximal to the metatarsal heads.
In individuals with first MTP joint OA, the objective of shoe-stiffening inserts is to reduce dorsiflexion at the first MTP joint during the propulsive phase of gait, thereby reducing dorsal compression at the joint.77,78 A recent case-series study of 31 participants with first MTP joint OA found clinically worthwhile improvements in foot pain and foot-related disability over a 3-month follow-up period,79 and a 12-month randomized controlled trial is currently underway to evaluate the effectiveness of this treatment compared to a flexible ‘sham’ insert.80 Contoured orthoses aim to support the medial longitudinal arch and often feature a cut-out section beneath the first metatarsal head, which allows the first metatarsal to plantarflex and minimize joint compression during propulsion. Evidence to support the effectiveness of contoured orthoses for first MTP joint is limited to a case series of 32 participants81 and one recent randomized trial that demonstrated equivalent pain reduction to rocker-sole footwear, but with fewer adverse events and greater adherence.55
Both shoe-stiffening inserts and contoured foot orthoses have also been evaluated in individuals with midfoot OA. The objective of orthotic treatment is to control excessive rearfoot eversion and support the medial longitudinal arch, as it has been shown that individuals with midfoot OA have more pronated feet and generate higher loads under the midfoot when walking.43,44 A case-series study of 20 participants treated with full-length carbon fibre inserts reported significant improvements in self-reported pain and function (using the Foot Function Index outcome measure) over a 4-week period,45 although no change in plantar loading was observed. More recently, a pilot randomized trial demonstrated significant improvements in pain and function in individuals with midfoot OA treated with semi-rigid contoured orthoses compared to a sham insert over a 12-week period, with kinematic analyses indicating that the contoured orthosis inverted the rearfoot and increased support under the midfoot.57
Surgery
Surgical intervention for foot OA may be indicated in individuals with advanced disease or in those whose symptoms have failed to resolve with conservative therapy. For first MTP joint OA, there are three main categories of surgical procedure: (1) joint preservation procedures such as cheilectomy which involve the removal of the dorsal exostosis from the metatarsal head and proximal phalanx and debridement of the degenerative articular cartilage; (ii) implant arthroplasty, which involves resecting a proximal portion of the proximal phalanx, remodelling the metatarsal head and inserting a metallic or silicone joint prosthesis; and (iii) arthrodesis, which involves the resection of cartilage from the metatarsal head and proximal phalanx and fusion of the joint using internal fixation.82 Currently, no surgical treatment algorithm for first MTP joint OA has reached broad consensus. As a general rule, however, joint-preserving procedures are considered more appropriate for early OA, while arthrodesis is preferable for end-stage OA or as a revision procedure.83
Cheilectomy has been shown to increase dorsiflexion range of motion at the first MTP joint and is associated with high levels of patient satisfaction (72–90%).84–89 However, this approach does not appear to alter the degenerative process, so recurrence of the dorsal osteophyte is common.85–88 Implant arthroplasty was first introduced in the 1950s, and several designs and materials have been trialled with mixed results.82 Early implants were associated with high rates of mechanical failure, formation of exogenous bone around the implant, loosening of the phalangeal component and reduction in first MTP joint plantarflexion.90 Recent implants using more durable materials and more biomechanically optimal designs have achieved better structural outcomes, although formation of exogenous bone remains a common complication.91 Finally, arthrodesis remains the gold standard surgical treatment for end-stage first MTP joint OA, with successful patient-reported outcomes ranging from 77% to 100%.92–94 Following this procedure, however, the first MTP joint is fixed in dorsiflexion, so the selection of the optimum angle of dorsiflexion is a critical consideration. Inadequate dorsiflexion may impair normal propulsion when walking, while excessive dorsiflexion may lead to dorsal impingement of the hallux from footwear. Generally, the first MTP joint is fixed in 10–15º of dorsiflexion; however, this may be increased in female patients to enable the wearing of moderate heeled footwear.95 Complications associated with arthrodesis include transfer lesions, metatarsalgia, non-union and development of interphalangeal joint OA.82
Only two randomized trials have been conducted to assess the efficacy of surgical procedures in people with first MTP joint OA associated with hallux rigidus. The first compared arthrodesis to implant arthroplasty, and reported better outcomes in the arthrodesis group, due primarily to the high rate of loosening of the phalangeal component of the implant.96 More recently, a multi-centre non-inferiority clinical trial compared a new synthetic cartilage implant to arthrodesis in 202 people with hallux rigidus, and reported the two techniques to have equivalent outcomes in relation to pain relief and physical function.56 Finally, a trial has recently been registered to compare the effectiveness of arthrodesis compared to proximal phalanx hemiarthroplasty.97
Surgical management of midfoot OA generally requires arthrodesis of the affected joints, although most studies have evaluated traumatic midfoot OA as a result of Lisfranc injury.51 Three case-series studies including patients with atraumatic midfoot OA have reported high levels of patient satisfaction following tarsometatarsal or midtarsal arthrodesis, with the most common complications being sesamoid pain, metatarsal head pain, metatarsal stress fracture and non-union, particularly in older people.98–100 The majority of surgical cases require fusion of the medial column midfoot joints (i.e. the first CMT, second CMT and the NC joints), which reflects the observation that lateral column involvement is less common. In small case-series studies of patients with lateral column involvement, good results have been reported following arthrodesis101 and interpositional arththroplasty102,103 of the fourth and fifth tarsometatarsal joints. No randomized trials have been conducted to evaluate the effectiveness of surgical intervention for midfoot OA.
Summary
Foot OA has been neglected for many years and the evidence base lags significantly behind other commonly affected sites such as the knee and hand. However, interest in foot OA has recently awakened, leading to advances in our knowledge of its burden, aetiology and treatment. Foot OA appears to be a common problem affecting one in six adults aged 50 years and over. Emerging evidence suggest that first MTP joint and midfoot OA are separate clinical entities with differing risk factor profiles. However, prospective epidemiological studies are needed to explore this further. There is a paucity of randomized controlled trial evidence to support the effectiveness of treatments for foot OA, although trials have demonstrated the effectiveness of physical therapy, rocker-sole shoes, foot orthoses and surgical interventions for first MTP joint OA. Randomized trial evidence in midfoot OA is limited to a single small pilot trial suggesting effectiveness of a prefabricated orthosis. Further randomized studies are needed to improve treatment options for people who have these common, painful, disabling conditions.
Footnotes
Funding: HBM is currently a National Health and Medical Research Council of Australia Senior Research Fellow (ID: 1020925).
Conflict of interest statement: The authors declare that there is no conflict of interest.
Contributor Information
Edward Roddy, Reader in Rheumatology, Research Institute for Primary Care and Health Sciences, Keele University, Keele, Staffordshire, ST5 5BG, UK; and Haywood Academic Rheumatology Centre, Staffordshire and Stoke-on-Trent Partnership Trust, UK.
Hylton B. Menz, Research Institute for Primary Care and Health Sciences, Keele University, Keele, UK; and School of Allied Health, College of Science, Health and Engineering, La Trobe University, Melbourne, Victoria, Australia
References
- 1. WHO Scientific Group on the Burden of Musculoskeletal Conditions at the Start of the New Millennium. The burden of musculoskeletal conditions at the start of the new millennium. World Health Organ Tech Rep Ser 2003; 919: i–x, 1–218. [PubMed] [Google Scholar]
- 2. Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380: 2163–2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jordan K, Clarke AM, Symmons DP, et al. Measuring disease prevalence: a comparison of musculoskeletal disease using four general practice consultation databases. Brit J Gen Pract 2007; 57: 7–14. [PMC free article] [PubMed] [Google Scholar]
- 4. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006; 3: e442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Guccione AA, Felson DT, Anderson JJ, et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health 1994; 84: 351–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wilkie R, Peat G, Thomas E, et al. Factors associated with restricted mobility outside the home in community-dwelling adults ages fifty years and older with knee pain: an example of use of the International Classification of Functioning to investigate participation restriction. Arthritis Rheum 2007; 57: 1381–1389. [DOI] [PubMed] [Google Scholar]
- 7. Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ 2003; 81: 646–656. [PMC free article] [PubMed] [Google Scholar]
- 8. Kellgren JH, Moore R. Generalized osteoarthritis and Heberden’s nodes. Br Med J 1952; 1: 181–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Trivedi B, Marshall M, Belcher J, et al. A systematic review of radiographic definitions of foot osteoarthritis in population-based studies. Osteoarthritis Cartilage 2010; 18: 1027–1035. [DOI] [PubMed] [Google Scholar]
- 10. Marshall M, Dziedzic KS, van der Windt DA, et al. A systematic search and narrative review of radiographic definitions of hand osteoarthritis in population-based studies. Osteoarthritis Cartilage 2008; 16: 219–226. [DOI] [PubMed] [Google Scholar]
- 11. Schiphof D, Boers M, Bierma-Zeinstra SM. Differences in descriptions of Kellgren and Lawrence grades of knee osteoarthritis. Ann Rheum Dis 2008; 67: 1034–1036. [DOI] [PubMed] [Google Scholar]
- 12. Zammit GV, Menz HB, Munteanu SE, et al. Interventions for treating osteoarthritis of the big toe joint. Cochrane Database Syst Rev 2010; 9: CD007809. [DOI] [PubMed] [Google Scholar]
- 13. Menz HB, Morris ME, Lord SR. Foot and ankle risk factors for falls in older people: a prospective study. J Gerontol A Biol Sci Med Sci 2006; 61: 866–870. [DOI] [PubMed] [Google Scholar]
- 14. Menz HB, Jordan KP, Roddy E, et al. Characteristics of primary care consultations for musculoskeletal foot and ankle problems in the UK. Rheumatology 2010; 49: 1391–1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Thomas M, Roddy E, Zhang W, et al. The population prevalence of foot and ankle pain in middle and old age: a systematic review. Pain 2011; 152: 2870–2880. [DOI] [PubMed] [Google Scholar]
- 16. Menz HB, Dufour AB, Casey VA, et al. Foot pain and mobility limitations in older adults: the Framingham Foot Study. J Gerontol A Biol Sci Med Sci 2013; 68: 1281–1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Keenan AM, Tennant A, Fear J, et al. Impact of multiple joint problems on daily living tasks in people in the community over age fifty-five. Arthritis Rheum 2006; 55: 757–764. [DOI] [PubMed] [Google Scholar]
- 18. Hill CL, Gill T, Menz HB, et al. Prevalence and correlates of foot pain in a population-based study: the North West Adelaide Health Study. J Foot Ankle Res 2008; 1: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Roddy E, Muller S, Thomas E. Onset and persistence of disabling foot pain in community-dwelling older adults over a 3-year period: a prospective cohort study. J Gerontol A Biol Sci Med Sci 2011; 66: 474–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kellgren JH, Lawrence JS. Radiological assessment of osteoarthritis. Ann Rheum Dis 1957; 16: 494–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kellgren JH, Jeffrey MR, Ball J. The epidemiology of chronic rheumatism: atlas of standard radiographs. Oxford: Blackwell Scientific, 1963. [Google Scholar]
- 22. Wood PHN. Osteoarthritis in the community. Clin Rheum Dis 1975; 2: 495–507. [Google Scholar]
- 23. Spector TD, Cooper C. Radiographic assessment of osteoarthritis in population studies: whither Kellgren and Lawrence? Osteoarthritis Cartilage 1993; 1: 203–206. [DOI] [PubMed] [Google Scholar]
- 24. Cicuttini FM, Spector TD. The epidemiology of osteoarthritis of the hand. Rev Rhum Engl Ed 1995; 62(6 Suppl. 1): 3S–8S. [PubMed] [Google Scholar]
- 25. Menz HB, Munteanu SE, Landorf KB, et al. Radiographic classification of osteoarthritis in commonly affected joints of the foot. Osteoarthritis Cartilage 2007; 15: 1333–1338. [DOI] [PubMed] [Google Scholar]
- 26. Sun Y, Gunther KP, Brenner H. Reliability of radiographic grading of osteoarthritis of the hip and knee. Scand J Rheumatol 1997; 26: 155–165. [DOI] [PubMed] [Google Scholar]
- 27. Roddy E, Thomas MJ, Marshall M, et al. The population prevalence of symptomatic radiographic foot osteoarthritis in community-dwelling older adults: cross-sectional findings from the Clinical Assessment Study of the Foot. Ann Rheum Dis 2015; 74: 156–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Brighton SW, de la Harpe AL, Van Staden DA. The prevalence of osteoarthrosis in a rural African community. Br J Rheumatol 1985; 24: 321–325. [DOI] [PubMed] [Google Scholar]
- 29. Bremner JM, Lawrence JS, Miall WE. Degenerative joint disease in a Jamaican rural population. Ann Rheum Dis 1968; 27: 326–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. van Saase JL, van Romunde LK, Cats A, et al. Epidemiology of osteoarthritis: Zoetermeer survey. Comparison of radiological osteoarthritis in a Dutch population with that in 10 other populations. Ann Rheum Dis 1989; 48: 271–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. van Saase JL, Vandenbroucke JP, van Romunde LK, et al. Osteoarthritis and obesity in the general population: a relationship calling for an explanation. J Rheumatol 1988; 15: 1152–1158. [PubMed] [Google Scholar]
- 32. Wilder FV, Barrett JP, Farina EJ. The association of radiographic foot osteoarthritis and radiographic osteoarthritis at other sites. Osteoarthritis Cartilage 2005; 13: 211–215. [DOI] [PubMed] [Google Scholar]
- 33. Solomon L, Beighton P, Lawrence JS. Osteoarthrosis in a rural South African Negro population. Ann Rheum Dis 1976; 35: 274–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wilder FV, Leaverton P, Rogers MW. Height and radiographic osteoarthritis: an epidemiologic assessment. J Musculoskelet Res 2008; 11: 185–189. [Google Scholar]
- 35. Menz HB, Munteanu SE, Landorf KB, et al. Radiographic evaluation of foot osteoarthritis: sensitivity of radiographic variables and relationship to symptoms. Osteoarthritis Cartilage 2009; 17: 298–303. [DOI] [PubMed] [Google Scholar]
- 36. Thomas MJ, Peat G, Rathod T, et al. The epidemiology of symptomatic midfoot osteoarthritis in community-dwelling older adults: cross-sectional findings from the Clinical Assessment Study of the Foot. Arthritis Res Ther 2015; 17: 178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mahiquez MY, Wilder FV, Stephens HM. Positive hindfoot valgus and osteoarthritis of the first metatarsophalangeal joint. Foot Ankle Int 2006; 27: 1055–1059. [DOI] [PubMed] [Google Scholar]
- 38. Rathod T, Marshall M, Thomas MJ, et al. Investigations of potential phenotypes of foot osteoarthritis: cross-sectional analysis from the Clinical Assessment Study of the Foot. Arthritis Care Res 2016; 68: 217–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Nelson AE, Smith MW, Golightly YM, et al. ‘Generalized osteoarthritis’: a systematic review. Semin Arthritis Rheum 2014; 43: 713–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Zammit GV, Menz HB, Munteanu SE. Structural factors associated with hallux limitus/rigidus: a systematic review of case control studies. J Orthop Sports Phys Ther 2009; 39: 733–742. [DOI] [PubMed] [Google Scholar]
- 41. Menz HB, Roddy E, Marshall M, et al. Demographic and clinical factors associated with radiographic severity of first metatarsophalangeal joint osteoarthritis: cross-sectional findings from the Clinical Assessment Study of the Foot. Osteoarthritis Cartilage 2015; 23: 77–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Mann RA. Hallux rigidus. Instruct Course Lect 1990; 39: 15–21. [PubMed] [Google Scholar]
- 43. Rao S, Baumhauer JF, Nawoczenski DA. Is barefoot regional plantar loading related to self-reported foot pain in patients with midfoot osteoarthritis. Osteoarthritis Cartilage 2011; 19: 1019–1025. [DOI] [PubMed] [Google Scholar]
- 44. Menz HB, Munteanu SE, Zammit GV, et al. Foot structure and function in older people with radiographic osteoarthritis of the medial midfoot. Osteoarthritis Cartilage 2010; 18: 317–322. [DOI] [PubMed] [Google Scholar]
- 45. Rao S, Baumhauer JF, Becica L, et al. Shoe inserts alter plantar loading and function in patients with midfoot arthritis. J Orthop Sports Phys Ther 2009; 39: 522–531. [DOI] [PubMed] [Google Scholar]
- 46. Pearce CJ, Calder JD. Surgical anatomy of the midfoot. Knee Surg Sports Traumatol Arthrosc 2010; 18: 581–586. [DOI] [PubMed] [Google Scholar]
- 47. Zammit GV, Munteanu SE, Menz HB. Development of a diagnostic rule for identifying radiographic osteoarthritis in people with first metatarsophalangeal joint pain. Osteoarthritis Cartilage 2011; 19: 939–945. [DOI] [PubMed] [Google Scholar]
- 48. Thomas MJ, Roddy E, Rathod T, et al. Clinical diagnosis of symptomatic midfoot osteoarthritis: cross-sectional findings from the Clinical Assessment Study of the Foot. Osteoarthritis Cartilage 2015; 23: 2094–2101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Cavanagh PR, Rodgers MM. The arch index: a useful measure from footprints. J Biomech 1987; 20: 547–551. [DOI] [PubMed] [Google Scholar]
- 50. Shurnas PS. Hallux rigidus: etiology, biomechanics, and nonoperative treatment. Foot Ankle Clin 2009; 14: 1–8. [DOI] [PubMed] [Google Scholar]
- 51. Patel A, Rao S, Nawoczenski D, et al. Midfoot arthritis. J Am Acad Orthop Surg 2010; 18: 417–425. [DOI] [PubMed] [Google Scholar]
- 52. Kalichman L, Hernandez-Molina G. Midfoot and forefoot osteoarthritis. Foot 2014; 24: 128–134. [DOI] [PubMed] [Google Scholar]
- 53. Kunnasegaran R, Thevendran G. Hallux rigidus: nonoperative treatment and orthotics. Foot Ankle Clin 2015; 20: 401–412. [DOI] [PubMed] [Google Scholar]
- 54. Munteanu SE, Zammit GV, Menz HB, et al. Effectiveness of intra-articular hyaluronan (Synvisc, hylan G-F 20) for the treatment of first metatarsophalangeal joint osteoarthritis: a randomised placebo-controlled trial. Ann Rheum Dis 2011; 70: 1838–1841. [DOI] [PubMed] [Google Scholar]
- 55. Menz HB, Auhl M, Tan JM, et al. Effectiveness of foot orthoses versus rocker-sole footwear for first metatarsophalangeal joint osteoarthritis: randomized trial. Arthritis Care Res 2016; 68: 581–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Baumhauer JF, Singh D, Glazebrook M, et al. Prospective, randomized, multi-centered clinical trial assessing safety and efficacy of a synthetic cartilage implant versus first metatarsophalangeal arthrodesis in advanced hallux rigidus. Foot Ankle Int 2016; 37: 457–469. [DOI] [PubMed] [Google Scholar]
- 57. Halstead J, Chapman GJ, Gray JC, et al. Foot orthoses in the treatment of symptomatic midfoot osteoarthritis using clinical and biomechanical outcomes: a randomised feasibility study. Clin Rheumatol 2016; 35: 987–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Vanore JV, Christensen JC, Kravitz SR, et al. Diagnosis and treatment of first metatarsophalangeal joint disorders. Section 2: hallux rigidus. J Foot Ankle Surg 2003; 42: 124–136. [DOI] [PubMed] [Google Scholar]
- 59. Smith R, Katchis S, Ayson L. Outcomes in hallux rigidus patients treated nonoperatively: a long-term follow-up study. Foot Ankle Int 2000; 21: 906–913. [DOI] [PubMed] [Google Scholar]
- 60. Grady J, Axe T, Zager E, et al. A retrospective analysis of 772 patients with hallux limitus. J Am Podiatr Med Assoc 2002; 92: 102–108. [DOI] [PubMed] [Google Scholar]
- 61. Jennings MB. Comparison of piroxicam and naproxen in osteoarthritis of the foot. J Am Podiatr Med Assoc 1994; 84: 348–354. [DOI] [PubMed] [Google Scholar]
- 62. da Costa BR, Reichenbach S, Keller N, et al. Effectiveness of non-steroidal anti-inflammatory drugs for the treatment of pain in knee and hip osteoarthritis: a network meta-analysis. Lancet 2017; 387: 2093–2105. [DOI] [PubMed] [Google Scholar]
- 63. Derry S, Conaghan P, Da Silva JA, et al. Topical NSAIDs for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev 2016; 4: CD007400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Laslett LL, Jones G. Capsaicin for osteoarthritis pain. Progr Drug Res 2014; 68: 277–291. [DOI] [PubMed] [Google Scholar]
- 65. Derry S, Matthews PR, Wiffen PJ, et al. Salicylate-containing rubefacients for acute and chronic musculoskeletal pain in adults. Cochrane Database Syst Rev 2014; 11: CD007403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Juni P, Hari R, Rutjes AW, et al. Intra-articular corticosteroid for knee osteoarthritis. Cochrane Database Syst Rev 2015; 10: CD005328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Grice J, Marsland D, Smith G, et al. Efficacy of foot and ankle corticosteroid injections. Foot Ankle Int 2017; 38: 8–13. [DOI] [PubMed] [Google Scholar]
- 68. Drakonaki EE, Kho JS, Sharp RJ, et al. Efficacy of ultrasound-guided steroid injections for pain management of midfoot joint degenerative disease. Skeletal Radiol 2011; 40: 1001–1006. [DOI] [PubMed] [Google Scholar]
- 69. Jevsevar D, Donnelly P, Brown GA, et al. Viscosupplementation for osteoarthritis of the knee: a systematic review of the evidence. J Bone Joint Surg Am 2015; 97: 2047–2060. [DOI] [PubMed] [Google Scholar]
- 70. Petrella RJ, Cogliano A. Intra-articular hyaluronic acid treatment for golfer’s toe: keeping older golfers on course. Phys Sportsmed 2004; 32: 41–45. [DOI] [PubMed] [Google Scholar]
- 71. Maher A. An audit of the use of sodium hyaluronate 1% (Ostenil® Mini) therapy for the treatment of hallux rigidus. Br J Podiatr 2007; 10: 47–51. [Google Scholar]
- 72. Pons M, Alvarez F, Sonalan J, et al. Sodium hyaluronate in the treatment of hallux rigidus: a single-blind, randomized study. Foot Ankle Int 2007; 28: 38–42. [DOI] [PubMed] [Google Scholar]
- 73. Shamus J, Shamus E, Gugel RN, et al. The effect of sesamoid mobilization, flexor hallucis strengthening, and gait training on reducing pain and restoring function in individuals with hallux limitus: a clinical trial. J Orthop Sports Phys Ther 2004; 34: 368–376. [DOI] [PubMed] [Google Scholar]
- 74. Solan M, Calder J, Bendall S. Manipulation and injection for hallux rigidus: is it worthwhile? J Bone Joint Surg Br 2001; 83B: 706–708. [DOI] [PubMed] [Google Scholar]
- 75. Tan JM, Auhl M, Menz HB, et al. The effect of Masai Barefoot Technology (MBT) footwear on lower limb biomechanics: a systematic review. Gait Posture 2016; 43: 76–86. [DOI] [PubMed] [Google Scholar]
- 76. Menz HB, Auhl M, Tan JM, et al. Biomechanical effects of prefabricated foot orthoses and rocker-sole footwear in individuals with first metatarsophalangeal joint osteoarthritis. Arthritis Care Res 2016; 68: 603–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Nawoczenski DA. Nonoperative and operative intervention for hallux rigidus. J Orthop Sports Phys Ther 1999; 29: 727–735. [DOI] [PubMed] [Google Scholar]
- 78. Shereff MJ, Baumhauer JF. Hallux rigidus and osteoarthrosis of the first metatarsophalangeal joint. J Bone Joint Surg Am 1998; 80: 898–908. [DOI] [PubMed] [Google Scholar]
- 79. Jerilyn TX, Menz HB, Murley GS, et al. Effectiveness of shoe stiffening inserts for first metatarsophalangeal joint osteoarthritis: a proof-of-concept study. Am J Phys Med Rehabil 2016; 95: 103–111. [DOI] [PubMed] [Google Scholar]
- 80. Munteanu SE, Landorf KB, McClelland JA, et al. Shoe-stiffening inserts for first metatarsophalangeal joint osteoarthritis (the SIMPLE trial): study protocol for a randomised controlled trial. Trials 2017; 18: 198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Welsh BJ, Redmond AC, Chockalingam N, et al. A case-series study to explore the efficacy of foot orthoses in treating first metatarsophalangeal joint pain. J Foot Ankle Res 2010; 3: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. DeCarbo WT, Lupica J, Hyer CF. Modern techniques in hallux rigidus surgery. Clin Podiatr Med Surg 2011; 28: 361–383, ix. [DOI] [PubMed] [Google Scholar]
- 83. Perler AD, Nwosu V, Christie D, et al. End-stage osteoarthritis of the great toe/hallux rigidus: a review of the alternatives to arthrodesis: implant versus osteotomies and arthroplasty techniques. Clin Podiatr Med Surg 2013; 30: 351–395. [DOI] [PubMed] [Google Scholar]
- 84. Mann RA, Coughlin MJ, DuVries HL. Hallux rigidus: a review of the literature and a method of treatment. Clin Orthop Relat Res 1979; 142: 57–63. [PubMed] [Google Scholar]
- 85. Hattrap SJ, Johnson KA. Subjective results of hallux rigidus following treatment with cheilectomy. Clin Orthop Relat Res 1988; 226: 182–191. [PubMed] [Google Scholar]
- 86. Mann RA, Clanton TO. Hallux rigidus: treatment by cheilectomy. J Bone Joint Surg Am 1988; 70: 400–406. [PubMed] [Google Scholar]
- 87. Geldwert JJ, Rock GD, McGrath MP, et al. Cheilectomy: still a useful technique for grade I and grade II hallux limitus/rigidus. J Foot Surg 1992; 31: 154–159. [PubMed] [Google Scholar]
- 88. Easley ME, Davis WH, Anderson RB. Intermediate to long-term follow-up of medial-approach dorsal cheilectomy for hallux rigidus. Foot Ankle Int 1999; 20: 147–152. [DOI] [PubMed] [Google Scholar]
- 89. Lau JT, Daniels TR. Outcomes following cheilectomy and interpositional arthroplasty in hallux rigidus. Foot Ankle Int 2001; 22: 462–470. [DOI] [PubMed] [Google Scholar]
- 90. Granberry WM, Noble PC, Bishop JO, et al. Use of a hinged silicone prosthesis for replacement arthroplasty of the first metatarsophalangeal joint. J Bone Joint Surg Am 1991; 73: 1453–1459. [PubMed] [Google Scholar]
- 91. Kim PJ, Hatch D, Didomenico LA, et al. A multicenter retrospective review of outcomes for arthrodesis, hemi-metallic joint implant, and resectional arthroplasty in the surgical treatment of end-stage hallux rigidus. J Foot Ankle Surg 2012; 51: 50–56. [DOI] [PubMed] [Google Scholar]
- 92. Coughlin MJ, Shurnas PS. Hallux rigidus: demographics, etiology, and radiographic assessment. Foot Ankle Int 2003; 24: 731–743. [DOI] [PubMed] [Google Scholar]
- 93. Brodsky JW, Passmore RN, Pollo FE, et al. Functional outcome of arthrodesis of the first metatarsophalangeal joint using parallel screw fixation. Foot Ankle Int 2005; 26: 140–146. [DOI] [PubMed] [Google Scholar]
- 94. Goucher NR, Coughlin MJ. Hallux metatarsophalangeal joint arthrodesis using dome-shaped reamers and dorsal plate fixation: a prospective study. Foot Ankle Int 2006; 27: 869–876. [DOI] [PubMed] [Google Scholar]
- 95. Kelikian AS. Technical considerations in hallux metatarsalphalangeal arthrodesis. Foot Ankle Clin 2005; 10: 167–190. [DOI] [PubMed] [Google Scholar]
- 96. Gibson JN, Thomson CE. Arthrodesis or total replacement arthroplasty for hallux rigidus: a randomized controlled trial. Foot Ankle Int 2005; 26: 680–690. [DOI] [PubMed] [Google Scholar]
- 97. Divecha HM, Zubairy AI, Barrie JL, et al. First metatarsophalangeal joint arthrodesis versus proximal phalanx hemiarthroplasty for hallux rigidus: feasibility study for a randomised controlled trial. Trials 2014; 15: 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Mann RA, Prieskorn D, Sobel M. Mid-tarsal and tarsometatarsal arthrodesis for primary degenerative osteoarthrosis or osteoarthrosis after trauma. J Bone Joint Surg Am 1996; 78: 1376–1385. [DOI] [PubMed] [Google Scholar]
- 99. Jung HG, Myerson MS, Schon LC. Spectrum of operative treatments and clinical outcomes for atraumatic osteoarthritis of the tarsometatarsal joints. Foot Ankle Int 2007; 28: 482–489. [DOI] [PubMed] [Google Scholar]
- 100. Verhoeven N, Vandeputte G. Midfoot arthritis: diagnosis and treatment. Foot Ankle Surg 2012; 18: 255–262. [DOI] [PubMed] [Google Scholar]
- 101. Raikin SM, Schon LC. Arthrodesis of the fourth and fifth tarsometatarsal joints of the midfoot. Foot Ankle Int 2003; 24: 584–590. [DOI] [PubMed] [Google Scholar]
- 102. Shawen SB, Anderson RB, Cohen BE, et al. Spherical ceramic interpositional arthroplasty for basal fourth and fifth metatarsal arthritis. Foot Ankle Int 2007; 28: 896–901. [DOI] [PubMed] [Google Scholar]
- 103. Berlet GC, Hodges Davis W, Anderson RB. Tendon arthroplasty for basal fourth and fifth metatarsal arthritis. Foot Ankle Int 2002; 23: 440–446. [DOI] [PubMed] [Google Scholar]


