Abstract
Background:
Liposuction–curettage (LC) is a popular and effective surgical method for the treatment of axillary bromhidrosis (AB). However, residual malodour and skin necrosis often appear after this type of surgery. We investigated the efficacy and complications of 4 methods of LC.
Methods:
A total of 280 patients with AB comprised the study cohort, of which 228 were followed up. We carried out 4 methods of modified tumescent LC through mini-incisions and provided a questionnaire for evaluation of surgical outcome. Evaluations were malodour elimination, scarring, reduced growth of hair, and complications. Mean follow-up was 15 months.
Results:
The study involved 449 axillae. In patients with LC in the final phase of improvement (programmed and well-organized LC, skin pinching to wrap up the cannula, LC to the skin around 2 surgical incisions, and cotton balls packed in gauze and an elastic set for post-operative management), excellent elimination of malodor was observed in 141 (89.81%) of 157 axillae. Only 4 (2.55%) cases encountered a small area of skin necrosis, and 28 (17.83%) had local damage to the epidermis.
Conclusion:
These data suggest that LC with a final phase of improvement through mini-incisions is effective for AB treatment.
Keywords: axillary osmidrosis, improvement, liposuction–curettage, mini-incisions
Abstract
Historique :
La liposuccion-curetage (LC) est un mode opératoire efficace et populaire pour traiter la bromidrose axillaire (BA). Cependant, de mauvaises odeurs résiduelles et une nécrose cutanée se produisent souvent après ce type d’opération. Les auteurs ont examiné l’efficacité et les complications de quatre types de LC.
Méthodologie :
Au total, 280 patients ayant une BA ont formé la cohorte de l’étude, dont 228 ont fait l’objet d’un suivi. Les auteurs ont effectué quatre types de LC tumescente modifiée par mini-incisions et ont remis un questionnaire d’évaluation des résultats de l’opération. Les points évalués étaient l’élimination des mauvaises odeurs, la cicatrice, la réduction de la pilosité et les complications. Le suivi moyen était de 15 mois.
Résultats :
L’étude portait sur 449 aisselles. Chez les patients ayant subi une LC qui en étaient à la dernière phase d’amélioration (LC programmée et bien organisée, pincement de la peau pour installer la canule, LC jusqu’à la peau par deux incisions chirurgicales, tampons d’ouate emballés dans de la gaze et bandage élastique pour la prise en charge postopératoire), les auteurs ont observé une excellente élimination des mauvaises odeurs dans 141 aisselles sur 157 (89,81%). Seulement quatre cas (2,55%) ont présenté une petite région de nécrose cutanée et 28 (17,83%), une atteinte locale de l’épiderme.
Conclusion :
Selon ces données, la LC accompagnée d’une phase finale d’amélioration par mini-incisions est efficace pour traiter la BA.
Introduction
Axillary bromhidrosis (AB) is a troublesome and distressing problem that interferes with the quality of life of affected individuals. The main characteristic of AB is an excessive foul odour in the axillary region due to the interaction of secretions from the apocrine glands with micro-organisms.1 Axillary bromhidrosis occurs exclusively in post-pubertal individuals. Axillary bromhidrosis is especially common in Asian populations. Because of the unpleasant odour, AB can cause severe personal distress in social situations.
Several treatments have been suggested for eliminating the malodour associated with AB. The effect of non-surgical methods such as topical deodorants, perfumes, antibiotics, and iontophoresis is temporary and limited. Surgical procedures include excision of subcutaneous fatty tissue2 with or without partial to total removal of axillary hair-bearing skin, subcutaneous shaving,3 superficial4 or ultrasonic5,6 liposuction, and laser treatment.7
Several reports have shown the efficacy of liposuction–curettage (LC) in AB treatment.8–10 Liposuction–curettage is a classic treatment for AB, but residual malodour and skin necrosis often appear after this type of surgery. Research on modification of tumescent LC for better efficacy and fewer complications has not been well described.
We modified the LC method into 3 phases. Four improvements were made and evaluated: programmed and well-organized LC, pinching the skin to wrap up the cannula, LC to the skin around 2 surgical incisions, cotton balls packed in gauze and elastic for post-operative management. In the present study, we evaluated the efficacy of our modified LC method with regard to outcome and complications.
Materials and Methods
We followed the principles outlined in the Declaration of Helsinki. Written informed consent was obtained from all patients.
Patients
From January 2009 to May 2012, 280 consecutive patients were enroled in the present study, of which 228 patients could be followed up for post-operative evaluation. There were 98 male and 130 female patients, with a mean age of 22 (range: 16-41) years. All surgical procedures were carried out on an outpatient basis, with local anaesthetic. Patients were divided into 4 groups according to the time order of the 3 phases of modified LC. Forty-three patients had conventional LC (85 axillae and 1 for unilateral surgery), 36 had LC of the first phase of improvement (72 axillae and 0 for unilateral surgery), 69 had LC of the second phase of improvement (135 axillae and 3 for unilateral surgery), and 80 had LC of the final phase of improvement (157 axillae and 3 for unilateral surgery). This strategy resulted in 449 axillae (Table 1).
Table 1.
The Demography of Patients Before Surgery.
| Variables | Value |
|---|---|
| Study period | January 2009-May 2012 |
| Number of patients | 228 |
| Male/female | 98/130 |
| Mean age, range | 22 years (16-41years) |
| Family history | 210 patients (92.11%) |
| Axillary hyperhidrosis | 216 patients (94.74%) |
| Recurrence cases after laser treatment | 6 patients (1 for unilateral surgery) |
| Recurrence cases after subcutaneous shaving | 6 patients (2 for unilateral surgery) |
| Recurrence cases after liposuction–curettage | 5 patients (3 for unilateral surgery) |
| Recurrence cases after mini-incisions for excision of tissue | 2 patients (1 for unilateral surgery) |
| Mean follow-up period (standard deviation) | 15 months (7.9) |
Patients were asked to complete a questionnaire for the assessment of outcome with respect to malodour elimination, scarring, reduced growth of hair, and complications. The mean follow-up period was 15 months (standard deviation = 7.9).
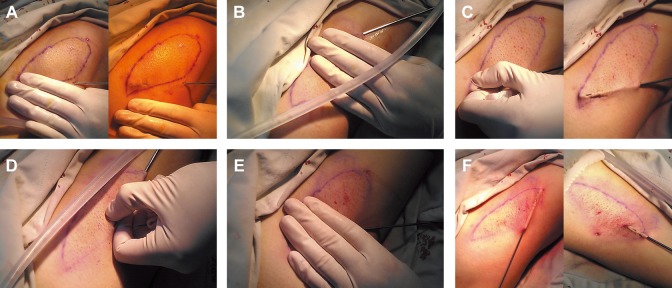
Surgical Equipment
The equipment used for LC was comprised mainly of 2 types of cannulas and a suction device. The first cannula was 17 cm in length and 2 or 2.5 mm in diameter with 1 pointed end and 2 suction holes (one on the same direction of the pointed end and the other on the opposite direction). The second cannula was 17 cm in length and 3 mm in diameter with 1 blunted end and 3 suction holes (1 on the upper side and 2 on the lateral side [Figure 1]). The suction device offered a negative pressure of 0.09 to 0.1 atm.
Figure 1.
General view of the cannulas used for liposuction–curettage (LC). One was 2.5 mm in diameter and 17 cm in length with 2 suction holes (one in the same direction of the pointed end and the other in the opposite direction) and 1 pointed end. The other was 3 mm in diameter and 17 cm in length with 3 suction holes (1 on the upper side and 2 on the lateral side) and 1 blunted end.
Preoperative Management
The patient was placed in the supine position with the upper arms abducted by ≈150°. It is believed that the distribution of the apocrine glands is similar to that of axillary hair, so the regions of axillary hair were marked. Armpit hair was shaved before surgery. A few residual armpit hairs could be used for post-operative examination. Two tiny “stab” incisions were made at the inferior and lateral sides of each axilla, ≈0.5 to 1.0 cm beyond the outline.
Anaesthesia
Local anaesthesia was induced with tumescent solution, which consisted of 500 (0.9%) mL of normal saline, 0.5 mL of epinephrine (1:1000 dilution), 20 mL (2%) of lidocaine, and 15 mL (5%) of sodium bicarbonate. Between 300 and 750 mL of tumescent solution was injected according to the weight of the patient. Infiltration was done with a 23-G needle through the incisions marked previously. Subcutaneous fat was infiltrated with tumescent solution first. The subdermal layer (adjacent to the dermis) was infiltrated thereafter. The infiltration area was ≥2 cm beyond the axillary hairline. By the end of the induction of local anaesthesia, the axillary skin became puffy, the surgical area was sufficiently tough, and the vault of the axilla was flat.
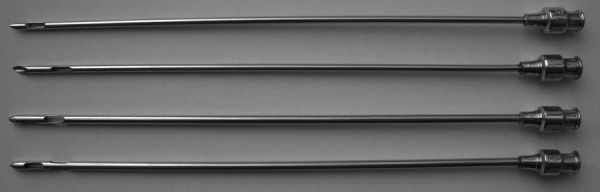
Surgical Procedure
We used 6 programmed and well-organized steps when employing the final modified version of LC. The first step was primarily through the inferior incision. The cannula with a pointed end (2.5 mm in diameter) was placed in the subdermal tunnel with the suction hole in the upward direction facing the subdermis. Stroke movements were made with the aid of the other hand to compress the skin for effective subdermal scraping (Figure 2A). The suction hole could not be seen at first. As LC progressed, subcutaneous fat and sweat glands were eliminated gradually, the flap became thin, and the suction hole could be seen increasingly clearly. The second step was through the lateral incision, application of the cannula was the same as for the first step (Figure 2B). The third step was pinching the skin to wrap up the cannula while carrying out radiating stroke movements through the inferior incision (Figure 2C). In this step, the cannula was changed to the blunted type (3.0 mm in diameter), and effective curettage was achieved through the 3 suction holes. The suction holes could be seen clearly. The fourth step was pinching the skin to wrap up the cannula while carrying out radiating stroke movements (as in the third step) through the lateral incision (Figure 2D). The fifth step was to repeat the first step and undertake additional LC if some areas of the skin were thicker than required (Figure 2E). The final step was LC to the skin around the 2 surgical incisions. Effective LC of 1 incision was achieved through curettage with pinching the skin from the incision and curettage without pinching the skin from the other incision (Figure 2F). In each step, the other incision could be used if a marked surgical area was missing from LC through 1 incision. This was the case in the second and fourth steps, in which ≈50% of the area could not be reached through the lateral incision. The 2 surgical approaches of the cannula met at 90°, thereby enabling curettage and suction over the entire area. By the end of the surgical procedure, the skin became sufficiently thin to be pinched readily, the residual armpit hair was easy to pull out, and skin color turned from white to purple.
Figure 2.
A, In the first step, the cannula was placed in the subdermal tunnel with the suction hole at the tip facing the subdermis through the inferior incision. Stroking movements were made with the aid of the other hand to compress the skin for radiation and effective subdermal scraping. The outline of the suction hole could not be seen at first. As liposuction–curettage (LC) progressed, subcutaneous fat and sweat glands were eliminated gradually, the flap became thin, and the suction hole could be seen increasingly clearly. B, In the second step, the cannula was placed in the subdermal tunnel with the suction hole at the tip facing the subdermis through the lateral incision. Radiating stroking movements were made with the aid of the other hand to compress the skin for effective subdermal scraping. The outline of the suction hole could not be seen at first. As LC progressed, subcutaneous fat and sweat glands were eliminated gradually, the flap became thin, and the suction hole could be seen increasingly clearly. C, In the third step, LC was done through the inferior incision. Skin pinching to wrap up the cannula was necessary while undertaking radiating stroking movements. The blunted cannula with 3 suction holes ensured complete curettage of the skin around the cannula. The outline of the suction hole could be seen clearly. D, In the fourth step, LC was done through the lateral incision. Skin pinching to wrap up the cannula was necessary while undertaking radiating stroking movements. The blunted cannula with 3 suction holes ensured complete curettage of the skin around the cannula. The outline of the suction hole could be seen clearly. E, In the fifth step, additional LC was done to eliminate residual sweat glands. The pointed cannula was used, and the suction holes could be seen clearly. F, In the sixth step, LC was applied to the skin around the 2 incisions, and the suction holes could be seen clearly. Effective LC of 1 incision was achieved through curettage with skin pinching from the incision and curettage without skin pinching from the other incision.
Post-operative Management
After squeezing the residual liquid in the axillary, stab incisions were covered by dressings. In the final phase of LC improvement, a bulky compressive dressing with cotton balls packed in the sterile gauze and an elastic axillary set were applied to bilateral axillae (Figure 3).
Figure 3.

Dressings with cotton balls packed in sterile gauze were applied to press the operative area. Meanwhile, an elastic set was used for pressure application to the surgical area and post-operative immobilization so that complications could be avoided (male).
The dressing and the elastic axillary set could be removed after 7 days. The patient was advised to avoid elevation of the upper arms and rotation of the shoulder joints for ≈1 week.
A comparison of the conventional surgical procedure and 3 modified procedures is shown in Table 2. In the step of opening the surgical plane rapidly, a cannula (2 mm in diameter) was inserted through the 2 stab incisions for opening the subcutaneous tunnel without negative pressure. First, the step of opening the surgical plane rapidly was included in the conventional method, LC was carried out 5 to 7 times in a non-specific order, and gauze, cotton pads, and the elastic set were used for post-operative management. Second, compared with the conventional method, LC was carried out in 5 programmed steps, skin pinching was used in the first phase of modified LC, and post-operative management was not changed. Third, compared with the first phase of modified LC, post-operative management was changed because cotton balls packed in sterile gauze and an elastic axillary set were employed. Finally, compared with the second phase of modified LC, the step of rapid opening of the surgical plane was not included in the final modified method, the sixth step of LC to the skin around the 2 incisions was added, and the dressings were not changed.
Table 2.
Comparison of Four Treatment Methods for Axillary Osmidrosis
| Steps | Conventional Method | First Phase of Improvement | Second Phase of Improvement | Final Phase of Improvement |
|---|---|---|---|---|
| Method of anaesthesia | Infiltration of tumescent solution in the subcutaneous fat layer and subdermal layer | |||
| Surgical procedure | ||||
| Quickly opening the surgical plane | Yes | Yes | Yes | No |
| LC for the first step | Five to 7 times of unordered LC from 2 mini-incisions until the skin became sufficiently thin | Yes | Yes | Yes |
| LC for the second step | Yes | Yes | Yes | |
| LC for the third step | Yes (skin pinching) | Yes (skin pinching) | Yes (skin pinching) | |
| LC for the fourth step | Yes (skin pinching) | Yes (skin pinching) | Yes (skin pinching) | |
| LC for the fifth step | Yes | Yes | Yes | |
| LC for the sixth step | No | No | Yes | |
| Post-operative management | Gauze, cotton pad, and elastic set | Gauze, cotton pad, and elastic set | Cotton balls packed in gauze and elastic set | Cotton balls packed in gauze and an elastic set |
Abbreviation: LC, liposuction–curettage.
Statistical Analysis
All data were analyzed with SPSS 17.0, differences between the 4 groups were tested using the Kruskal-Wallis test, and multiple pairwise comparisons were performed with the Mann-Whitney U test. A P value of <.05 was considered statistically significant.
Results
The 4 methods were carried out in 67 male and 93 female patients. Outcome was assessed by subjective (patient reporting) and objective (surgical) evaluation. A summary of post-operative results (malodour elimination, change in hair growth, post-operative scar, patient satisfaction, and complications) is shown in Table 3.
Table 3.
Post-Operative Evaluation of 228 Patients (449 Axillae) After Tumescent Liposuction–Curettage for Axillary Osmidrosis.
| Evaluation Criteria | No. of Axillae (%) | |||
|---|---|---|---|---|
| Conventional Method | First Phase of Improvement | Second Phase of Improvement | Final Phase of Improvement | |
| Malodour elimination | ||||
| Excellent | 56 (65.88) | 63 (87.5) | 117 (86.67) | 141 (89.81) |
| Good | 20 (23.53) | 5 (6.94) | 9 (6.67) | 14 (8.92) |
| Fair | 7 (8.24) | 3 (4.17) | 5 (3.70) | 2 (1.27) |
| Poor | 2 (2.35) | 1 (1.39) | 4 (2.96) | 0 (0.00) |
| Reduced hair growth | ||||
| No hair | 0 (0.00) | 2 (2.78) | 6 (4.45) | 10 (6.37) |
| Greatly decreased | 48 (56.47) | 56 (77.78) | 99 (73.33) | 123 (78.34) |
| Slightly decreased | 37 (43.53) | 14 (19.44) | 30 (22.22) | 24 (15.29) |
| Unchanged | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| Scar | ||||
| Inconspicuous | 70 (82.35) | 38 (52.78) | 112 (82.96) | 133 (84.71) |
| Slightly visible | 15 (17.65) | 26 (36.11) | 21 (15.56) | 21 (13.38) |
| Conspicuous | 0 (0.00) | 8 (11.11) | 2 (1.48) | 3 (1.91) |
| Very marked | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| Complications | ||||
| Hematoma of seroma | 0 (0.00) | 3 (4.17) | 1 (0.74) | 1 (0.64) |
| Small area of necrosis | 1 (1.18) | 13 (15.29) | 2 (1.48) | 4 (2.55) |
| Large area of necrosis | 0 (0.00) | 1 (1.39) | 0 (0.00) | 0 (0.00) |
| Scar contracture | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| Local infection | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| Wound disruption | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| Local epidermis damage | 15 (17.65) | 43 (59.72) | 22 (16.30) | 28 (17.83) |
| Subjective assessment | ||||
| Very satisfied | 55 (64.71) | 47 (65.28) | 121 (89.63) | 149 (94.90) |
| Satisfied | 15 (17.65) | 13 (18.06) | 9 (6.67) | 6 (3.83) |
| Not satisfied | 13 (15.29) | 9 (12.50) | 4 (2.96) | 2 (1.27) |
| Very unsatisfied | 2 (2.35) | 3 (4.16) | 1 (0.74) | 0 (0.00) |
| Total | 85 (100.00) | 72 (100.00) | 135 (100.00) | 157 (100.00) |
The degree of malodour elimination was graded as “excellent” (neither the patient nor close friends were aware of malodour), “good” (very marked improvement; minimal malodour was noted sometimes during heavy perspiration), “fair” (marked improvement but the patient was aware of slight malodour during daily activities), and “poor” (the patient had limited improvement and both the patient and people nearby were easily aware of malodour).8
Of 157 (80 cases) axillae with the final phase of improvement, 141 (89.81%) showed excellent results. Hair growth vanished or was greatly decreased in 133 (84.71%) axillae. Post-operative scarring was mostly inconspicuous in 154 (98.09%) axillae. Subjective assessment showed that 149 (94.90%) of patients were very satisfied. Only 4 (2.55%) patients encountered a small area of skin necrosis, and 28 (17.83%) had local damage to the epidermis.
There was better elimination of malodour in patients with the 3 modified methods of LC than pre-modified LC (P < .01). No significant difference was observed among the 3 modified methods (P > .05). Slight improvement was found in the final modified method compared with the first and second modified methods. Post-operative scarring was more obvious in patients with the first phase of improvement than the other 3 methods (P < .01), but no significant difference was observed among the conventional method and other 2 modified methods (P > .05). Reduced hair growth was achieved more efficiently in patients using the 3 modified methods than the conventional method (P < .01), but no significant difference was observed between the 3 modified methods (P > .05). Prevalence of local damage to the epidermis was higher in patients with the first phase of improvement than the other 3 methods (P < .01), but no significant difference was observed between the conventional method and the other 2 modified methods (P > .05). Subjective assessment revealed a better result in patients with the second and final phase of improvement than the conventional method and the first phase of improvement (P < .01), but no significant difference was observed between the conventional method and the first modified method (P > .05), and the result was identical upon comparison of the second modified method and the final method (P > .05).
We concluded that the first modified method was more effective but was associated with more complications than the conventional method. Fewer complications were observed in the second modified method compared with the first modified method. Surgical effectiveness was improved in the final modified method compared with the second modified method.
No serious complications were noted except for skin necrosis covering a small area and local damage to the epidermis in some patients. In patients who had skin necrosis covering a small area, it healed in 1 to 3 weeks after appropriate dressings were applied. In patients with local damage to the epidermis, the skin healed in ≈7 days after appropriate dressings were applied. Hair growth was missing in a small number of patients and was decreased considerably in most patients. Furthermore, neither the patient or nearby persons were aware of malodour (Figures 4 –7). Recurrence was not observed in any patient during a minimum follow-up of 3 months.
Figure 4.

Recovery of axillae 3 weeks after the surgery. The 2 incisions healed well, and a slightly visible scar could be seen (male).
Figure 5.

Recovery of axillae 4 months after the surgery. Scarring was inconspicuous. Hair growth was not seen in this patient. Hair did not grow out because hair growth recovers in <3 months (male).
Figure 6.

Recovery of left axillae 6 months after the surgery. Few armpit hairs were seen, and malodour elimination graded as “excellent” (left). Recovery of right axillae 6 months after the surgery. There were more armpit hairs than those in the left axillae, and malodour elimination was graded as “good” (right). The 2 images were from the same patient and indicated different levels of effectiveness of surgery (male).
Figure 7.

Recovery of axillae 18 months after the surgery. Hair growth was reduced significantly in comparison with the preoperative situation. No conspicuous scar could be seen, and malodour elimination was graded as “excellent.” Also, the surgical procedure did not cause additional scarring (female).
Discussion
Ideally, a procedure for AB should be done in an outpatient setting with local anaesthesia and result in limited discomfort to the patient and little scarring over a short recovery time.2,7,11 Various surgical methods for definitive treatment of AB have been described. Superficial liposuction with curettage is a popular procedure for AB because most of the apocrine glands are in subcutaneous tissue.12,13 Elimination of malodour was the primary concern of patients, so a surgical procedure that could remove all sweat glands was the best method. Moreover, it has been shown that aggressive curettage of the deep dermis has a strong impact upon surgical outcome.14,15
In the present study, 2 planes of suction were used. One was in the superficial fatty layer, and the other was in the subdermal plane. The operating plane was subdermal, but we could remove as many apocrine glands as we wished.
Liposuction–curettage for AB treatment has several advantages: small incisions, short operative time, simple surgical method, high success rate, rapid recovery, and low prevalence of complications. In our study, 4 modifications were made to the conventional method: programmed and well-organized LC, skin pinching to wrap up the cannula, LC to the skin around 2 surgical incisions, and cotton balls packed in gauze and an elastic set for post-operative management.
Several conclusions could be inferred from this study. First, skin pinching to aid curettage was important for malodour elimination because the difference between the conventional method and first modified method was significant. However, skin pinching brought about more skin damage, and the prevalence of complications increased. Second, the prevalence of skin necrosis and epidermis damage decreased if cotton balls were used instead of gauze and cotton pads. Third, LC to the skin around the 2 incisions improved the effectiveness of the procedure. Fourth, opening the surgical plane rapidly had no effect because the plane was opened in the first step of LC.
Upon application of the final phase of LC, excellent results were seen in 141 of 157 axillae, and the prevalence of severe complications was very low (1 for hematoma and 4 for a small area of skin necrosis). Only 28 (17.83%) patients encountered local damage to the epidermis. Compared with conventional LC, our method showed a low prevalence of complications and a high prevalence of good results. The only normal complication was superficial necrosis to the local epidermis, which healed spontaneously after appropriate dressing.
Indications for this type of surgery for males were at age ≥18 years and malodour for ≥3 years. For females, the indications were at age ≥16 years with a menstrual history and malodour for ≥3 years.
With respect to the final phase of improvement of LC, 6 main features should be considered. First, a large volume of tumescent solution and injection via the subdermal route were necessary for opening the operative tunnel. These features made the first step of the procedure easy and effective. Second, during subcutaneous scraping in the first 2 steps, the holes of the sharpened end and the cannula tip faced the dermis, and the outline of the holes could be seen during stroking movements. Furthermore, the other hand was used to compress the skin for effective curettage. As the procedure progressed, the outline of the suction hole became clearer. In fact, the first 2 steps needed slow (but numerous) stroking movements. These 2 steps were critical to the efficacy of the procedure because most of the apocrine glands could be removed in this way. Third, skin pinching to wrap up the suction holes was different from conventional LC in the third and fourth steps. Because of the 3 suction holes in the blunted cannula, all sides of the skin wrapping up the cannula underwent effective curettage. The distance between the 2 sequential radiating channels was 5 to 10 mm, and the outline of the suction holes could be seen clearly. Fourth, bulky compressive dressings with cotton balls packed in sterile gauze were applied to ensure that the surgical area was well-pressed. Theoretically, this feature of the procedure reduced the risk of skin necrosis. Fifth, the period of immobilization was 1 week. Sixth, suction–curettage to the skin around the 2 surgical incisions was included in our study.
In conclusion, the final phase of improvement of LC through mini-incisions for the AB treatment was simple, easy to carry out, practical, safe, effectively eliminated malodour, and was associated with few complications. However, in this preliminary report, the number of patients involved in each of the modified surgical methods was small, and the follow-up period was short. Further studies with more patients and a longer follow-up period are needed.
Acknowledgment
We thank all members of the Department of Plastic Surgery, The First Affiliated Hospital, College of Medicine, Zhejiang University for their suggestions to the modifications in the treatment of axillary osmidrosis.
Level of Evidence: Level 3, Therapeutic
Authors’ Note: This work was performed in the department of Plastic Surgery, The First Affiliated Hospital, College of Medicine, Zhejiang University.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by funding from the National Natural Science Foundation of China (No. 81372072 and 81671918), Zhejiang Provincial Science and Technology Project (No. 2016C33134), and Zhejiang Provincial Natural Science Foundation (No. LY13H060002).
References
- 1. Leyden JJ, Mcginley KJ, Holzle E, Labows JN, Kligman AM. The microbiology of the human axilla and its relationship to axillary odor. J Invest Dermatol. 1981;77(5):413–416. [DOI] [PubMed] [Google Scholar]
- 2. Tung TC, Wei FC. Excision of subcutaneous tissue for the treatment of axillary osmidrosis. Br J Plast Surg. 1997;50(1):61–66. [DOI] [PubMed] [Google Scholar]
- 3. Homma K, Maeda K, Ezoe K, Fujita T, Mutou Y. Razor-assisted treatment of axillary osmidrosis. Plast Reconstr Surg. 2000;105(3):1031–1033. [DOI] [PubMed] [Google Scholar]
- 4. Ou LF, Yan RS, Chen IC, Tang YW. Treatment of axillary bromhidrosis with superficial liposuction. Plast Reconstr Surg. 1998;102(5):1479–1485. [DOI] [PubMed] [Google Scholar]
- 5. Chung S, Yoo WM, Park YG, Shin KS, Park BY. Ultrasonic surgical aspiration with endoscopic confirmation for osmidrosis. Br J Plast Surg. 2000;53(3):212–214. [DOI] [PubMed] [Google Scholar]
- 6. Yoo WM, Pae NS, Lee SJ, Roh TS, Chung S, Tark KC. Endoscopy-assisted ultrasonic surgical aspiration of axillary osmidrosis: a retrospective review of 896 consecutive patients from 1998 to 2004. J Plast Reconstr Aesthet Surg. 2006;59(9):978–982. [DOI] [PubMed] [Google Scholar]
- 7. Park JH, Cha SH, Park SD. Carbon dioxide laser treatment vs subcutaneous resection of axillary osmidrosis. Dermatol Surg. 1997;23(4):247–251. [DOI] [PubMed] [Google Scholar]
- 8. Lee D, Cho SH, Kim YC, Lee SS, Park SW. Tumescent liposuction with dermal curettage for treatment of axillary osmidrosis and hyperhidrosis. Dermatol Surg. 2006;32(4):505–511;discussion 11. [DOI] [PubMed] [Google Scholar]
- 9. Bechara FG, Sand M, Hoffmann K. Tumescent liposuction with dermal curettage for treatment of axillary osmidrosis and hyperhidrosis. Dermatol Surg. 2007;33(1):125. [DOI] [PubMed] [Google Scholar]
- 10. Seo SH, Jang BS, Oh CK, Kwon KS, Kim MB. Tumescent superficial liposuction with curettage for treatment of axillary bromhidrosis. J Eur Acad Dermatol Venereol. 2008;22(1):30–35. [DOI] [PubMed] [Google Scholar]
- 11. Park DH, Kim TM, Han DG, Ahn KY. A comparative study of the surgical treatment of axillary osmidrosis by instrument, manual, and combined subcutaneous shaving procedures. Ann Plast Surg. 1998;41(5):488–497. [DOI] [PubMed] [Google Scholar]
- 12. Bisbal J, del Cacho C, Casalots J. Surgical treatment of axillary hyperhidrosis. Ann Plast Surg. 1987;18(5):429–436. [DOI] [PubMed] [Google Scholar]
- 13. Kim HG. A new osmidrosis procedure, the scrape and suction technique: review of 4,322 patients. Aesthetic Plast Surg. 2014;38(2):282–287. [DOI] [PubMed] [Google Scholar]
- 14. Bechara FG, Sand M, Sand D, Altmeyer P, Hoffmann K. Suction-curettage as a surgical treatment of focal axillary hyperhidrosis: recommendation for an aggressive approach. Plast Reconstr Surg. 2007;119(4):1390–1391. [DOI] [PubMed] [Google Scholar]
- 15. Beer GM, Baumuller S, Zech N, et al. Immunohistochemical differentiation and localization analysis of sweat glands in the adult human axilla. Plast Reconstr Surg. 2006;117(6):2043–2049. [DOI] [PubMed] [Google Scholar]