Abstract
Background:
Physicians are increasingly using smartphones to take clinical photographs. This study evaluates a smartphone application for clinical photography that prioritizes and facilitates patient security.
Methods:
Ethics approval was obtained to trial a smartphone clinical photography application, PicSafe Medi. Calgary plastic surgeons and residents used the application to obtain informed consent and photograph patients. Surveys gauging the application’s usability, consent process, and photograph storage/sharing were then sent to surgeons and patients.
Results:
Over a 6-month trial period, 15 plastic surgeons and residents used the application to photograph 86 patients. Over half of the patients (57%) completed the survey. The majority of patients (96%) were satisfied with the application’s consent process, and all felt their photographs were secure. The majority (93%) of surgeons/residents completed the survey. The application was felt to overcome issues with current photography practices: inadequate consent and storage of photographs (100%), risk to patient confidentiality (92%), and unsecure photograph sharing (93%). Barriers to regular use of the application included need for cellphone service/Internet (54%), sanitary concerns due to the need for patients to sign directly on the phone (46%), inability to obtain proactive/retroactive consent (85%), and difficulty viewing photographs (80%). The majority of surgeons (85%) believe a smartphone application would be suitable for clinical patient photography, but due to its limitations, only 23% would use the trialed application.
Conclusions:
A smartphone clinical photography application addresses the patient confidentiality risks of current photography methods; however, limitations of the trialed application prevent its broad implementation.
Keywords: cellphones, confidentiality, photography, privacy, smartphone
Abstract
Historique :
Les médecins utilisent de plus en plus leur téléphone intelligent pour prendre des photographies cliniques. La présente étude vise à évaluer une application photographie clinique pour téléphone intelligent qui priorise et favorise la sécurité des patients.
Méthodologie :
Les auteurs ont obtenu l’approbation éthique nécessaire pour mettre à l’essai PicSafe Medi©, une application photographie clinique pour téléphone intelligent. Des plasticiens et des résidents de Calgary l’ont utilisée pour obtenir le consentement éclairé des patients et les photographier. Les plasticiens et les patients ont ensuite reçu un sondage pour évaluer la facilité d’utilisation de l’application, le processus de consentement et le processus d’entreposage et de partage des photos.
Résultats :
Sur une période d’essai de six mois, 15 plasticiens et résidents ont utilisé l’application pour photographier 86 patients. Plus de la moitié des patients (57 %) ont rempli le sondage. La majorité d’entre eux (96 %) étaient satisfaits du processus de consentement de l’application et avaient l’impression que leurs photographies étaient sécurisées. La plupart des plasticiens et des résidents (93 %) ont rempli le sondage. Ils trouvaient que l’application réglait des problèmes liés aux pratiques actuelles de photographie : consentement et entreposage inadéquats (100 %), risque de ne pas respecter la confidentialité des patients (92 %) et partage non sécurisé des photographies (93 %). Les obstacles à l’utilisation régulière de l’application incluaient la nécessité d’avoir accès à un service de téléphonie cellulaire ou à Internet (54 %), les problèmes d’hygiène puisque les patients devaient signer directement sur le téléphone (46 %), l’impossibilité d’obtenir un consentement proactif ou rétroactif (85 %) et la difficulté à visualiser les photographies (80 %). La majorité des chirurgiens (85 %) trouvaient qu’une application pour téléphone intelligent conviendrait à la prise de photos cliniques des patients, mais à cause de ses limites, seulement 23 % utiliseraient celle mise à l’essai.
Conclusions :
Une application photographie clinique pour téléphone intelligent résout les risques potentiels des modes de photographie actuels liés à la confidentialité des patients, mais les limites de celle à l’essai en empêchent l’utilisation généralisée.
Introduction
Within the field of medicine, provision of patient care is by means of multidisciplinary teams. Clinical photography is an important tool that enhances patient care by providing visual documentation of their condition throughout the treatment process and allowing accurate communication with the many members of their treatment team.1-7
An increasing number of physicians and medical students are now using smartphones to take clinical photographs of patients, largely as a means of enhancing communication.8-10 A survey to all members of the Canadian Society of Plastic Surgeons in 2013 found that 89% of responding surgeons and 100% of responding residents have taken photographs of patients using smartphones and believe they are both practical and necessary to provide the best patient care.10 Australian11 and United Kingdom9 surveys had similar findings. Despite the ubiquitous use of smartphones for clinical photography, surgeons remain uncomfortable with their use, as they are unsure of hospital policies, fear it appears unprofessional, and worry about security breaches.10
These concerns are warranted, as current clinical photography practice poses both risk to patients, with breach of their confidentiality, and legal risk to physicians.12-14 With the increasing role of technology in providing patient care, a technological solution in the form of a smartphone application could address the lack of secure, effective, and efficient options for clinical photography.8,12,15 The purpose of this study was to find and trial a smartphone application that would allow secure clinical photography by including a consent process, photograph storage, and a secure sharing function.
Methods
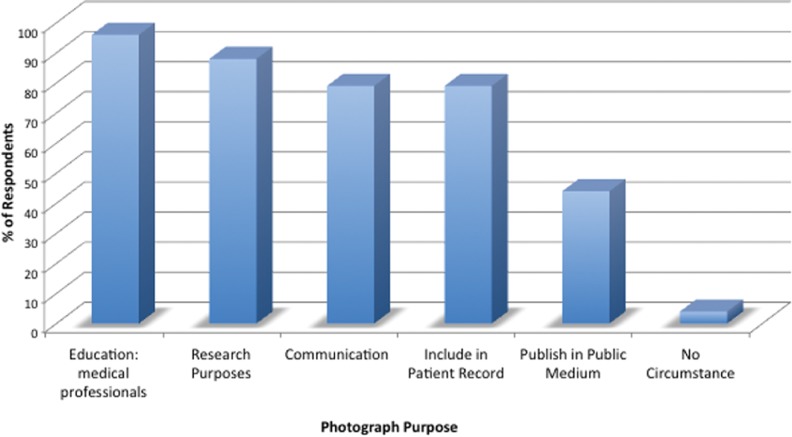
A search of the literature and commercially available applications on the smartphone “app store” was conducted to find available clinical photography applications that incorporated consent, offered secure photograph storage, and facilitated patient care. Two applications were found, Photoconsent and PicSafe Medi. PicSafe Medi, an Australian application developed for medical photography, was chosen for its user-friendly interface and transparency around its privacy laws. The photographs were stored on a secure cloud and could be shared through the application with the use of a secure link. Written consent was incorporated within the application by having the patient sign using their finger on the application screen. Patients could consent to one or more of the following categories: “assessment, treatment, or referral,” “research and education,” and “medically related publication” (Figure 1). As this was only the trial phase of the application, should the physicians require the photograph for publication, the standard Alberta Health Services written consent form was recommended in addition to the “medically related publication” category being selected.
Figure 1.
PicSafe Medi Consent.
Ethics was obtained via the Conjoint Health Research Ethics Board to conduct a 6-month trial of PicSafe Medi within the Section of Plastic Surgery in the Calgary Zone of Alberta Health Services. Calgary plastic surgeons and residents were recruited to use the application and to recruit patients. Eligible patients were those under the care of the physicians enrolled in the study who would have had their photograph taken regardless of the study occurring (for enhancement of their care or for educational purposes). Both physician participants and patient participants were required to complete a written consent to participate in the study.
Surveys were sent out to recruited patients after they had had their photograph taken and to the participating physicians after the 6-month trial period. The patient survey assessed the patient’s general experience having their photograph taken using the application, whether they felt their information was secure, the purposes for clinical photography that they felt most comfortable providing consent (ie, educational, publication, etc), and through which medium they felt most secure being photographed (ie, digital camera, smartphone camera).
The physician surveys assessed their methods of clinical photography, photograph storage and sharing, and consent process prior to the use of this application, as well as gauged the usability, consent process, and photograph storage and sharing process of the application. The various purposes for clinical photography were also assessed.
Results
Over the 6-month trial period, 3 Calgary plastic surgeons and 12 residents used the application to photograph 86 patients.
Patient Survey Responses
Over half of the patients (57%) completed the survey. All of the patients felt their photograph was secure when taken using the PicSafe Medi application, and all would have also felt secure if their photograph was taken with a digital camera. The majority (89%) still felt that that their information would have been secure had their photograph been taken using the built-in smartphone camera. Patients did not feel pressure to provide consent (95%) and were satisfied with the application’s consent process (96%). Only 4% would have preferred to provide consent using a pen and paper.
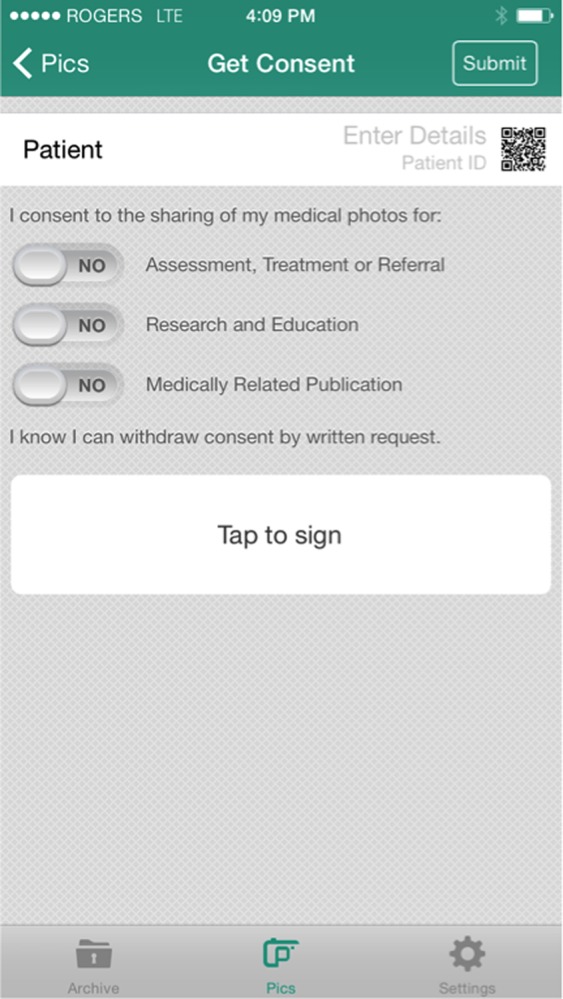
Patients felt they would most likely provide consent for clinical photography when the photograph was “to be used for educational purposes by medical professionals” (96%), for research purposes (88%), to enhance communication with the care team (79%), and to be included in their patient record (79%). Patients felt least comfortable having their photograph taken for publication in a public medium (44%). A small minority (4%) did not feel comfortable having their photograph taken in any circumstance (Figure 2).
Figure 2.
Photograph’s intended use.
Patients would prefer to have their photograph taken with a smartphone (54%), whether this is a smartphone camera (29%) or a secure application (25%), and about a quarter of the patients (23%) were indifferent to the method of photography used (Figure 3). Only 4% would prefer the use of a digital camera and the remaining 19% did not respond. The predominant reason for the preference of the smartphone stated in the comments was a sense of efficiency and the ability to add to their care by facilitating communication with other health-care professionals.
Figure 3.
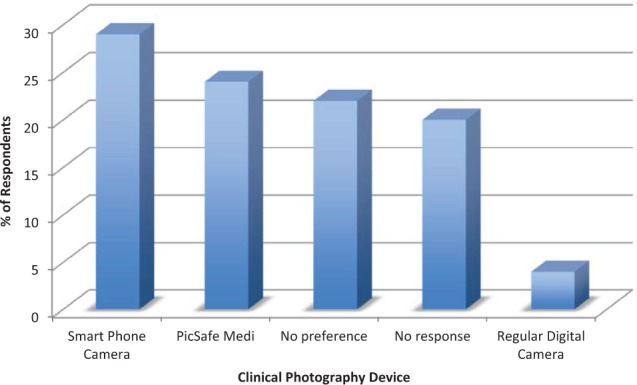
Patient preference of device used.
When asked for general comments regarding the application, common themes included the need for photographs to allow effective communication and care and the need for the photographs to be taken in a secure manner. Specifically, patients were “more than happy to provide pictures of a procedure they are undergoing if it helps improve care for future patients” and expressed their pleasure that “finally someone thought of having this info (in) the medical field, (where) pictures are proof of the first impressions doctors have. I’m glad for this app” and overall thought “this is a fantastic program and benefits the healing of all injuries.” Patients emphasized the importance of photograph security, especially when involving sensitive areas, stating that they “have no issue with a photograph taken by my medical team as long as it EXCLUDES my face,” and on a similar theme, “if only bust shots are taken, confidentiality should remain safe regardless of (the) device used.”
Surgeon and Resident Survey Responses
The majority (93%) of surgeons (2 of 3) and residents (11 of 12) completed the survey.
Prior to the use of this application
All resident respondents and 1 staff surgeon (93%) used their smartphone camera application as their primary method for patient photography. The remaining staff surgeon respondents used a regular camera. The consent method used was primarily verbal (93%), whereas 7% used Alberta Health Services (AHS) written consent. When transfer of photographs was required, 85% transferred photographs using their smartphone text message application, 7% used encrypted e-mail, and 7% showed the photograph directly on their phone.
Respondents mainly stored their photographs on 2 devices, their laptops and smartphones (50%), 14% stored them on their smartphones alone, 14% on 3 devices, their laptops, desktops, and smartphones, and the remainder did not store their photographs (14%). Of those who stored their photos, all had a password on their smartphone device and 1 respondent additionally used a separate password-protected application. Most (64%) did not back up their stored photographs; the remainder (36%) used dropbox, external hard drive, laptop, and iCloud to back up the photographs. The respondents felt that their biggest concerns with their current methods of storage were lack of organization (42%) and lack of security (67%).
Trial of PicSafe Medi
The majority (64%) of respondents used the application 1 to 5 times, 21% used it 6 to 10 times, and 14% used it over 10 times. The application was felt to overcome the following issues with the respondents’ current photography practices: inadequate consent and storage of patient photographs (100%), risk to patient confidentiality (92%), and unsecure photograph transmission to other health-care professional (93%; Figure 4). The majority of respondents believed that the application’s consent was suitable for communication with the patient care team (71%), educational purposes (79%), and research purposes (79%), whereas fewer thought it was adequate for the patient record (43%), publication (50%), and disclosure to the public (15%). The application’s consent was thought by 39% of participants to be better than the consent they had been obtaining before, 46% thought it was equivalent to their prior method (same discussion, just getting a signature to accompany it), and 39% thought it was worse (no reasons specified).Most participants (57%) used the application to receive a secure link to view a photograph, and half sent a photograph to a team member using the application’s secure link. When unable to speak to a team member in person and the need to securely share a patient photograph arose, 93% of respondents felt that a secure link to share the photograph using a smartphone application was adequate, 86% felt that encrypted e-mail was adequate, 21% felt transmission using text message was adequate, and none felt that using regular e-mail was adequate.
Figure 4.
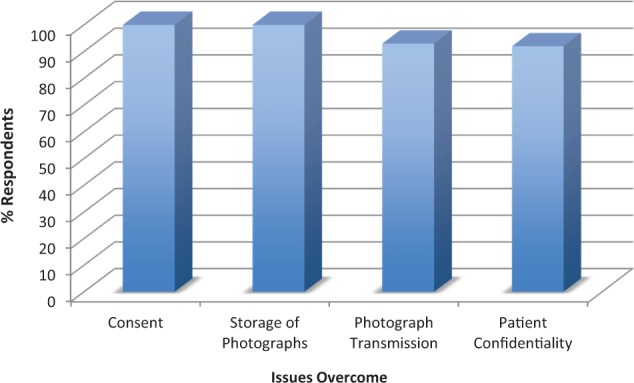
Issues overcome.
Respondents felt that the issues that remained with clinical photography practice using the application included inadequate consent (33%), unintentional showing of patient photographs to friends or family members (33%), and potential breach of patient confidentiality (100%). Specific barriers to the regular use of this particular application included the inability to obtain proactive and retroactive consent (85%), difficulty viewing photographs (80%), the need for cellphone service or Internet (54%), sanitary concerns due to the need for patients to sign directly on the phone (46%), and general usability of the application (43%). The issues with viewing the photographs included photograph distortion, photographs not immediately available for viewing, difficulty downloading the images to a personal computer, and inability to obtain or view the photograph in a format other than PDF. The need to obtain a separate written patient consent to participate in the study in addition to the application’s consent deterred 79% of surgeon participants from using the application and recruiting patients as much as they would have otherwise.
Due to these limitations, only 23% of respondents would use the application as is. The majority of surgeons (85%) felt that if a smartphone application was modified to overcome the above limitations, it would be suitable to broadly implement for clinical patient photography, whereas 15% would still prefer to use their smartphone camera and none would prefer a digital camera.
Discussion
Clinical photography has been recognized as an essential part of medicine, specifically in fields such as Plastic Surgery where visualization of a clinical problem and transmission of this image to other team members are key to ensuring high-quality patient management.1-4 These photographs are also of critical importance to further the education of trainees,1 to facilitate the triage of patients from peripheral sites,3,4,16-18 and to improve communication between health-care professionals.17-19 Gathering photographic information for certain clinical scenarios (eg, amputated digits, burns, wounds, postoperative free-flap monitoring, etc) helps to allocate resources, determine the urgency to see a specialist, and limit unnecessary interventions.3,4,18-21 For example, in the case of amputated digits, a photograph can help determine the possibility for emergent replantation versus less urgent revision amputation. For these reasons, clinical photography has been said to have “the potential to revolutionize the practice of plastic surgery.”2,3
This need for clinical photography and communication among various health-care professionals has led to common practices that have some serious flaws and pose a legal risk to health-care providers with risk of complaints of professional misconduct that may lead to disciplinary action,1,14,22-24 along with a privacy risk to patients. Recently, the Australian privacy act was updated, and with these changes, health-care professionals and their institutions face large fines for simply having unsecured patient photographs on their devices.12 Our study trials a smartphone application for clinical photography, with the hope of finding a solution that would facilitate all the potential benefits of clinical photography mentioned above, while limiting the confidentiality risks to patients.
The physician population in this trial feels that a smartphone application for clinical photography is needed, with 85% believing this is a simple, promising solution to the current issues with clinical photography. The Canadian Medical Protective Association (CMPA) recommends that express consent for patient photography should be obtained—if verbal, the discussion should be documented, but as a precaution, especially if the photograph is to be used for promotional purposes, then written consent should be obtained. Prior studies demonstrated that the most common method of consent for clinical photography is verbal (86%-92%), but only 75% believe it is sufficient to ensure patient privacy,9-11 and 83% would obtain written consent if it could be done more efficiently.10,11 These findings were supported in our trial, where 85% of physician participants feel that the application’s consent process is better or equivalent to their prior method of consent, by allowing documentation of the consent discussion. Importantly, 96% of the patient participants were also satisfied with the applications consent process.
Despite the wide acceptability of consent using this smartphone application, it remains important to tailor the consent process and documentation to the individual scenario. Most patients feel comfortable providing consent for photographs to be used for medical education (96%), research purposes (88%), and communication with their care team (79%). For these situations, the smartphone applications consent process is likely sufficient, and the other features of secure photograph storage and transmission to other medical professionals facilitate the provision of patient care. Fewer patients feel comfortable having their photograph published in a public medium (44%), and for this type of scenario, perhaps a different, more extensive consent discussion and documentation should exist to ensure thorough patient understanding of the added risks.
The value of ease of clinical photography and communication with the care team to physicians is well recognized in this study, as well as others.9-11 Perhaps surprisingly, this same value is expressed by patients. In our study, over half of the patients prefer to have their photograph taken with a smartphone, whereas only 4% prefer a digital camera, with the reason being a sense of efficiency and ability to add to their care by facilitating communication with other health-care professionals. These comments point to patient understanding of the importance of photographs in providing their care, as well as an understanding of the many team members involved in their care who depend on efficient communication, particularly in a hospital setting. This is supported in other studies that demonstrate patient recognition of the benefits of smartphone photography and photograph transmission to enhance not only their care but also the care of others via physician education.5,25 As an example of one of the possible patient perceived benefits of clinical photography, Wang et al26 demonstrate that patients feel that clinical photography enhances their autonomy in the management of their chronic wounds. From a patient acceptance standpoint, a smartphone application with its added security features is an excellent option for clinical photography.
Unfortunately, the trialed application has too many limitations to physician use to allow for its broad implementation, and only 23% of respondents would use the application without extensive modifications. Limitations from a physician standpoint include poor quality of photographs, general difficulty using the application, inability to obtain retroactive consent, and sanitary concerns. Also, the application does not ensure that only health-care providers use it, and any member of the public who downloads it would be able to see the photograph attached to the “secure” link. Even in the absence of any other limitations, Canadian compliant privacy laws and “cloud” location are also needed for broad implementation.
A limitation of this study is the small sample size of physician respondents, particularly attending surgeons, likely due to the many difficulties encountered using the application, the need for a separate consent to recruit patients, and surgeon custom. Responder bias is also a limitation, as surveys were used for data collection. It is also necessary to consider that the participants of this study were residents and plastic surgeons working in teaching hospitals where the patient care teams are much larger and often the problems more complex, and thus the photography and communication needs may be different than those required in other patient care settings.
Future steps include determining current provincial and national photography guidelines and how they apply to our current photography climate. In the absence of an available photography application, we recommend following CMPA and provincial guidelines for clinical photography to avoid potential breaches of patient information. We plan to continue the search for a photography application that would meet criteria described below to allow its widespread usage and replace the current malpractices of clinical photography.
The ideal application would allow for inapplication consent, high-quality photography, and secure messaging between health-care workers. Additionally, all photographs and messages would be stored off of the phone, independently of its built-in “cloud.” This cloud would need to be Canadian based for Canadian health-care workers and allow for both photograph retention in accordance with provincial guidelines as well as auditing capabilities.
Conclusion
A smartphone application for clinical photography was trialed and addresses the patient confidentiality risks of current photography methods including patient consent, secure storage, and secure transmission of photographs, making patient acceptance of the application high. Plastic surgeons and residents also recognized the potential of a smartphone application as a solution to current issues. However, limitations of the trialed application prevent its broad implementation, and novel or modified applications still need to be developed.
Footnotes
Level of Evidence: Level 3, Risk
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Kirk M, Hunter-Smith S, Smith K, Hunter-Smith D. The role of smartphones in the recording and dissemination of medical images. J MTM. 2014;3(2):40–45. [Google Scholar]
- 2. Hunter T, Hardwicke J, Rayatt S. The smart phone: an indispensable tool for the plastic surgeon? J Plast Reconstr Aesthet Surg. 2010;63(4):e426–e427. [DOI] [PubMed] [Google Scholar]
- 3. Gardiner S, Hartzell TL. Telemedicine and plastic surgery: a review of its applications, limitations and legal pitfalls. J Plast Reconstr Aesthet Surg. 2012;65(3):e47–e53. [DOI] [PubMed] [Google Scholar]
- 4. Van der Rijt R, Hoffman S. Ethical considerations of clinical photography in an area of emerging technology and smartphones. J Med Ethics. 2014;40(3):211–212. [DOI] [PubMed] [Google Scholar]
- 5. Hacard F, Maruani A, Delaplace M, et al. Patients’ acceptance of medical photography in a French adult and paediatric dermatology department: a questionnaire survey. Br J Dermatol. 2013;169(2):298–305. [DOI] [PubMed] [Google Scholar]
- 6. Lau CK, Schumacher HH, Irwin MS. Patients’ perception of medical photography. J Plast Reconstr Aesthet Surg. 2010;63(6):e507–e511. [DOI] [PubMed] [Google Scholar]
- 7. Al-Hadithy N, Ghosh S. Smartphones and the plastic surgeon. J Plast Reconstr Aesthet Surg. 2013;66(6):e155–e161. [DOI] [PubMed] [Google Scholar]
- 8. Franko OI, Tirrell TF. Smartphone app use among medical providers in ACGME training programs. J Med Syst. 2012;36(5):3135–3139. [DOI] [PubMed] [Google Scholar]
- 9. Taylor D, Foster E, Dunkin C, Fitzgerald A. A study of the personal use of digital photography within plastic surgery. J Plast Reconstr Aesthet Surg. 2007;61(1):37–40. [DOI] [PubMed] [Google Scholar]
- 10. Chan N, Charette J, Dumestre DO, Fraulin FO. Should ‘smart phones’ be used for patient photography? Plast Surg (Oakv). 2016;24(1):32–34. [PMC free article] [PubMed] [Google Scholar]
- 11. Kunde L, McMeniman E, Parker M. Clinical photography in dermatology: ethical and medico-legal considerations in the age of digital and smartphone technology. Australas J Dermatol. 2013;54(3):192–197. [DOI] [PubMed] [Google Scholar]
- 12. Patel NG, Rozen WM, Marsh D, et al. Modern use of smartphone applications in the perioperative management in microsurgical breast reconstruction. Gland Surg. 2016;5(2):150–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mahar PD, Foley PA, Sheed-Finck A, Baker CS. Legal considerations of consent and privacy in the context of clinical photography in Australian medical practice. Med J Aust. 2013;198(1):48–49. [DOI] [PubMed] [Google Scholar]
- 14. Thomas VA, Rugeley PB, Lau FH. Digital photograph security: what plastic surgeons need to know. Plast Reconstr Surg. 2015;136(5):1120–1126. [DOI] [PubMed] [Google Scholar]
- 15. Reusche R, Buchanan PJ, Kozlow JH, Vercler CJ. A systematic review of smartphone applications for plastic surgery providers: target audience, uses, and cost. Ann Plast Surg. 2016;77(1):6–12. [DOI] [PubMed] [Google Scholar]
- 16. Trovato MJ, Scholer AJ, Vallejo E, Buncke GM, Granick MS. eConsultation in plastic and reconstructive surgery. Eplasty. 2011;11:e48. [PMC free article] [PubMed] [Google Scholar]
- 17. Pap SA, Lach E, Upton J. Telemedicine in plastic surgery: E-consult the attending surgeon. Plast Reconstr Surg. 2002;110(2):452–456. [DOI] [PubMed] [Google Scholar]
- 18. Jones SM, Milroy C, Pickford MA. Telemedicine in acute plastic surgical trauma and burns. Ann R Coll Surg Engl. 2004;86(4):239–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Engel H, Huang JJ, Tsao CK, et al. Remote real-time monitoring of free flaps via smartphone photography and 3G wireless internet: a prospective study evidencing diagnostic accuracy. Microsurgery. 2011;31(8):589–595. [DOI] [PubMed] [Google Scholar]
- 20. Verhoeven F, van Gemert-Pijnen L, Dijkstra K, Nijland N, Seydel E, Steehouder M. The contribution of teleconsultation and videoconferencing to diabetes care: a systematic literature review. J Med Internet Res. 2007;9(5):e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wallace DL, Jones SM, Milroy C, Pickford MA. Telemedicine for acute plastic surgical trauma and burns. J Plast Reconstr Aesthet Surg. 2008;61(1):31–36. [DOI] [PubMed] [Google Scholar]
- 22. Franchitto N, Gavarri L, Dedouit F, Telmon N, Rougé D. Photography, patient consent and scientific publications: medicolegal aspects in France. J Forensic Leg Med. 2008;15(4):210–212. [DOI] [PubMed] [Google Scholar]
- 23. Scheinfeld N. Photographic images, digital imaging, dermatology, and the law. Arch Dermatol. 2004;140(4):473–476. [DOI] [PubMed] [Google Scholar]
- 24. Lakdawala N, Fontanella D, Grant-Kels JM. Ethical considerations in dermatologic photography. Clin Dermatol. 2012;30(5):486–491. [DOI] [PubMed] [Google Scholar]
- 25. Jayaraman C, Kennedy P, Dutu G, Lawrenson R. Use of mobile phone cameras for after-hours triage in primary care. J Telemed Telecare. 2008;14(5):271–274. [DOI] [PubMed] [Google Scholar]
- 26. Wang SC, Anderson JA, Jones DV, et al. Patient perception of wound photography. Int Wound J. 2016;13(3):326–330. [DOI] [PMC free article] [PubMed] [Google Scholar]