Abstract
Introduction:
There is very little information in the literature evaluating the natural history of adult trigger fingers and their rate of spontaneous resolution over time.
Methods:
A consecutive case series of patients with trigger finger was generated. For each patient, we recorded whether the patient’s disease resolved from either no treatment versus active treatment options and over what time period.
Results:
Three hundred forty-three patients with trigger finger were included in the study. Fifty-two percent of patients resolved without any treatment whatsoever after waiting a mean (and median) of 8 months from initial consultation. The thumb was the most frequent digit to resolve without treatment (72%).
Conclusions:
We found that just over half of patients with trigger fingers who are referred to our office resolve spontaneously without any intervention.
Keywords: trigger, finger, digit, untreated
Abstract
Historique :
Très peu de publications portent sur l’évolution naturelle des doigts à ressort chez les adultes et sur leur taux de résolution spontanée au fil du temps.
Méthodologie :
Les chercheurs ont produit une série de cas consécutifs de patients ayant un doigt à ressort. Pour chaque patient, ils ont vérifié si le problème s’était résolu sans traitement ou après un traitement actif ainsi que le laps de temps nécessaire pour parvenir à ce résultat.
Résultats :
Au total, 343 patients ayant un doigt à ressort ont participé à l’étude. Le problème s’est résolu sans traitement chez 52 % des patients au bout d’une période moyenne (et médiane) de huit mois après la première consultation. C’est le pouce qui guérissait le plus souvent sans traitement (72 %).
Conclusion :
Les chercheurs ont découvert qu’un peu plus de la moitié des patients ayant un doigt à ressort qui sont dirigés vers leur bureau guérissent spontanément sans intervention.
Introduction
Shortly after the phenomenon of trigger finger was first described in the literature by Notta,8 a surgical procedure to release the fibrous tendon sheath was pronounced as a definitive solution for the problem.1 Several treatment options have been described for the management of trigger fingers including splinting, steroid injection, and surgery. Each treatment option has its own side effects and costs. It is important that patients, family physicians, and hand specialists know that many trigger fingers are expected to spontaneously resolve completely without any treatment at all. In our literature search, we could not find any case series specifically evaluating the natural history of untreated trigger fingers. The aim of this study was to evaluate “no treatment” as a truly conservative management option for adult patients suffering from trigger fingers.
Methods
A retrospective case series analysis was performed using consecutive patients evaluated by our office between January 2004 and August 2016. Patients were included in the study if they were diagnosed with at least 1 trigger finger by the senior author (D.L.) at the time of initial consultation. Exclusion criteria were pediatric trigger finger (age <16) or a previous trigger finger release in the same digit. All patients were followed until complete symptom resolution. Loss to follow-up was <1%. For each patient, we recorded whether the patient’s disease resolved from either no treatment versus active treatment options and over what time period. Treatment options offered by our team included steroid injection and surgical trigger finger release; however, patients were instructed to wait for 6 months for their symptoms to resolve naturally prior to engaging in any of the above active treatment options. Patients were also offered the opportunity to be expedited directly to treatment if symptoms became severe before 6 months. Our mechanism to establish symptom resolution was clinic follow-up or to take their word for it when we followed them up on the telephone. The study data were collected and analyzed separately by 2 independent evaluators other than the solo surgeon. We also performed a subgroup analysis of specific digits affected.
Results
Our chart review produced 343 patients with a diagnosis of trigger finger who met the inclusion criteria. The majority of patients were female: 57% (197 females). The average wait time to be seen in our office after family physician referral for a trigger finger was 6 to 8 weeks. At the time of initial hand surgery consultation, 6% of patients presented with a resolved trigger finger diagnosis, having had no treatment at all. Steroid injection and/or splinting were not utilized by our patients during the study period. Complete spontaneous resolution of symptoms was found in 52% of patients. In this group of 178 patients who resolved without treatment, 50% were found to have done so within 8 months of initial consultation (median) and 90% were found to have resolved completely within 1 year (Figure 1). The mean wait time for spontaneous resolution was also 8 months. None of these patients complained of any functional loss.
Figure 1.
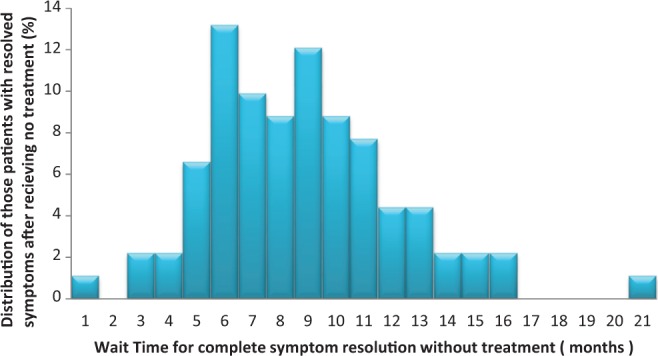
How long do patients wait before they achieve spontaneous resolution of their trigger finger without treatment?
Surgery was ultimately requested and performed in the other 48% of our patients. In this group of 165, 50% opted for surgery after waiting 5 months from the initial consultation (median) and 90% opted for surgery within 14 months (Figure 2).
Figure 2.
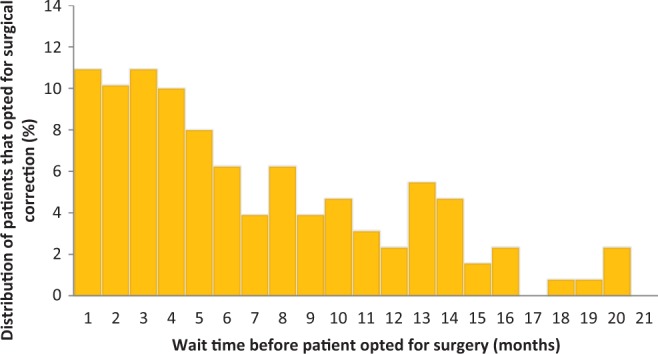
Of those patients with trigger finger who opted for surgery, how long do they first wait for spontaneous improvement before choosing to have surgery instead?
With a subgroup analysis, we found that the most commonly affected digit was the ring finger followed by the long finger, the thumb, the index finger, and the small finger. Compared to other digits, trigger thumb was found to be the most favoured digit for spontaneous resolution without treatment (72%). There was no significant difference between male and female outcomes.
Discussion
Our study provides evidence that a significant number of trigger fingers fully improve without any treatment whatsoever. We found that the majority of patients were willing to wait at least 6 months for early signs of symptom resolution and an eventual chance of complete symptom resolution while avoiding treatment. We hypothesize that there is some remodelling over time of the pulley and decreased inflammation and tendinitis with temporary rest and lifestyle modification guided by the patient’s symptoms.
To our knowledge, there are no case series that focuses on evaluating the natural history and spontaneous resolution of symptoms in adult patients with trigger finger. Lambert et al found that 16% of trigger fingers resolved spontaneously without treatment within 1 month of initial specialist consultation.2 Murphy et al found that 20% of patients treated with a placebo of normal saline injection within the sheath resolved spontaneously without any treatment at a 4-month follow-up.3 Another study presented 30 consecutive adult trigger thumbs managed without treatment and found that 80% of the trigger thumbs had complete spontaneous resolution without any treatment, after waiting an average of 7 months (range: 2-15 months).4 The other 20% of patients in the study were unwilling to wait at all and insisted on immediate surgery or injection, but it is possible that they also would have resolved spontaneously had they waited. The thumb is likely to improve more frequently without treatment since there is only 1 flexor tendon gliding, and also the thumb can be quite functional with minimal movement of the interphalangeal joint during periods of rest and healing. In the pediatric literature, spontaneous resolution of trigger thumb has been shown to occur in over 50% of patients if the families are willing to wait several years.5–7
Surgery is the definitive management option for adult trigger finger, and we reserve this treatment option for those patients who do not undergo spontaneous resolution and whose symptoms have plateaued or for patients who are too impatient or symptomatic to wait. In our practice, we do not have a significant role for steroid injection or splinting, as the literature provides comparable success rates to our patients who receive no treatment at all. Steroids and splinting also subjects the patient to small risks such as infection and stiffness, respectively, and may also cause worsening of symptoms.8 In patients who present with secondary causes of trigger finger such as diabetes and rheumatoid arthritis, the literature suggests that they are less likely to resolve without surgery, in comparison to primary trigger finger.9 This subgroup was not evaluated in this study.
The true percentage of trigger fingers that would have fully improved without treatment is likely underestimated in this study for 2 reasons: Firstly, the majority of patients who opted for surgical correction were not willing to wait for spontaneous resolution. We presume that a significant number of the trigger fingers that underwent surgery would have spontaneously resolved had they waited longer. Secondly, many trigger fingers likely improve prior to seeing their family doctor or prior to being referred to a hand specialist. Primary care physicians may delay the referral of patients with mild trigger fingers to specialists, as they know from experience that some patients will get better on their own.10 The natural history of trigger finger as a disease would be better assessed by the family physician, as they become involved earlier in the disease process. The timing and percentage of trigger fingers that resolve without treatment from initial consultation will likely vary depending on patient population, primary physician education and practice style, and specialist wait time.
Conclusion
In our practice, we found that the majority of patients referred to our office got better without treatment. We suggest offering no treatment as a viable option for the management of adult trigger finger. This option reduces treatment complications and costs but requires patient education and patience.
Footnotes
Level of Evidence: Therapeutic Level 4
Authors’ Note: Informed consent was given by all patients in this study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Weilby A. Trigger finger. Acta Orthop Scandinav. 1970;41:419–427. [DOI] [PubMed] [Google Scholar]
- 2. Lambert M, Morton R, Sloan J. Controlled study of the use of local steroid injection in the treatment of trigger finger and thumb. J Hand Surg Br. 1992;17(1):69–70. [DOI] [PubMed] [Google Scholar]
- 3. Murphy D, Failla J, Koniuch M. Steroid versus placebo injection for trigger finger. J Hand Surg Am. 1995;20(4):628–631. [DOI] [PubMed] [Google Scholar]
- 4. Schofield C, Citron N. The natural history of adult trigger thumb. J Hand Surg Br. 1993;18(2):247–248. [DOI] [PubMed] [Google Scholar]
- 5. Watanabe H, Hamada Y, Toshima T, Nagasawa K. Conservative treatment for trigger thumb in children. Arch Orthop Trauma Surg. 2001;121(7):388–399. [DOI] [PubMed] [Google Scholar]
- 6. Koh S, Horii E, Hattori T, Hiroishi M, Otsuka J. Pediatric trigger thumb with locked interphalangeal joint: can observation or splinting be a treatment option. J Pediatr Orthop. 2012;32(7):724–726. [DOI] [PubMed] [Google Scholar]
- 7. Baek G, Lee H. The natural history of pediatric trigger thumb: a study with a minimum of five years follow-up. Clin Orthop Surg. 2011;3(2):157–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wolfe S. Tendinopathy. In: Wolfe S, Hotchkiss R, Pederson W, Kozin S. . Green’s Operative Hand Surgery. 6th ed: Elsevier Churchill Livingstone; 2011:2067–2088. [Google Scholar]
- 9. Ryzewicz M, Wolf J. Trigger digits: Principles, management, and complications. J Hand Surg Am. 2006;31(1):135–146. [DOI] [PubMed] [Google Scholar]
- 10. Sempowski I. The management of the occasional trigger finger. Can J Rural Med. 2008;13(3):136–138. [PubMed] [Google Scholar]


