Abstract
This qualitative study explored and compared the subjective experiences of 102 veterans with posttraumatic stress disorder (PTSD) who were randomly assigned to 1 of 4 arms: (a) body scan, (b) mindful breathing, (c) slow breathing, or (d) sitting quietly. Qualitative data were obtained via semistructured interviews following the intervention and analyzed using conventional content analysis. The percentage of participants within each intervention who endorsed a specific theme was calculated. Two-proportion z tests were then calculated to determine if the differences among themes endorsed in specific groups were statistically significant. Six core themes emerged from analysis of participant responses across the 4 groups: (a) enhanced present moment awareness, (b) increased nonreactivity, (c) increased nonjudgmental acceptance, (d) decreased physiological arousal and stress reactivity, (e) increased active coping skills, and (f) greater relaxation. More participants in the mindfulness intervention groups reported improvement in PTSD symptoms when compared to participants in non-mindfulness groups. Different types of intervention targeted different symptoms and aspects of well-being. Furthermore, type of intervention may have also differentially targeted potential mechanisms of action. This article highlights the importance of employing both quantitative and qualitative research methods when investigating the dynamic process of mindfulness and may inform how practices can be tailored to the needs of the veteran with PTSD.
Keywords: veterans, trauma, mindfulness
A recent systematic review of complementary and alternative medicine for posttraumatic stress disorder (PTSD) found positive evidence for mindfulness-based interventions (MBIs).1 To date, the literature mostly comprises cross-sectional analyses and prospective outcome studies that compare MBIs to treatment as usual (TAU) or wait-list control groups.2–9 Randomized control trials (RCTs) are generally considered the most scientifically rigorous method of assessing the efficacy of MBIs. While several RCTs have found promising results with MBIs among veterans,10,11 some mindfulness researchers have argued that a purely quantitative approach provides a limited understanding of the processes and outcomes of mindfulness training.12
One concern is that MBIs are multidimensional and include multiple components within a single intervention (eg, body scan, walking meditation, mindful breathing, psychoeducation). The concern is exacerbated when MBIs are provided to individuals with complex and chronic conditions. For example, symptoms experienced by veterans with PTSD are often grouped into related, but distinct clusters: recurrent and intrusive recollections of traumatic events(s), avoidance behaviors, emotional numbing, and alterations in arousal and reactivity.13,14 Furthermore, individuals with PTSD are also likely to experience depression, distractibility, irritability, outbursts of anger, disruption of sleep patterns, discord in interpersonal relationships, reduction in work abilities, moral injury, and elevated risk of medical disorders, chronic pain, substance abuse, and suicide.13,15–19 Outcome studies that compare MBIs to TAU are limited in their ability to discern whether pre- to posttreatment change is due to a specific component of the MBI, or the synergy of multiple components. Furthermore, outcome studies that compare MBIs to TAU are unable to assess if specific components of the intervention differentially affect distinct symptom clusters. While these studies can assess for meaningful change in preidentified variables, due to the complexity of the interventions and the symptoms, a number of related and critically important variables and their mechanisms of action that enhance well-being and reduce suffering may go undetected.20
Finally, RCTs are limited in their ability to provide insight into participants’ contextual and subjective understanding of how and why the intervention works. By supplementing quantitative approaches with qualitative data analyses, researchers can further develop a theoretical construct by placing emphasis on the meaning, experience, and subjective viewpoint of the participant.21 Investigating the phenomenon in its natural context through the collection of rich, dynamic, and personal narratives may enhance our understanding of the psychological mechanisms and processes associated with mindfulness, resulting in more targeted interventions for veterans.22,23
There are few first-person accounts in the literature on veterans’ subjective experiences of how they use mindfulness practices to alleviate PTSD symptoms. Price et al24 found mindfulness body-oriented therapy to be effective in reducing PTSD symptoms among female veterans. Data from interviews and focus groups led to the important inclusion of self-efficacy measures and provided insight into how to improve recruitment, intervention delivery, and physical environment/comfort. To identify barriers to enrollment and participation, Martinez et al25 conducted a content analysis of 48 semistructured interviews with veterans who had enrolled in a mindfulness-based stress reduction (MBSR) intervention. The authors concluded that Women Only and tele-health MBSR groups could improve accessibility to MBSR for veterans by addressing barriers such as commute anxiety, time restrictions, and an aversion to mixed gender groups among women. Further recommendations by the authors included educating MBSR teachers about veteran culture and health challenges faced by veterans, adding psychoeducation materials that related mindfulness practice to conditions common among veterans, and improving visual aids for mindful movement exercise in the workbooks. Individual interviews and focus groups among 65 outpatient veterans with PTSD enrolled in a mindfulness-based Mantram Repetition Program provided insight into how the veterans used the practices to manage a wide range of emotional reactions to internal and external stimuli.26 Researchers found 12 discreet categories, including relaxing and calming down, letting go of negative feelings, thinking clearly and rationally, diverting attention away from triggering events, focusing attention, refining mantram skills, dealing with sleep disturbances, coming back from flashbacks, slowing down, communicating thoughts and feelings more effectively, feeling in touch spiritually, and letting go of physical pain. Finally, in a feasibility study of an 8-week mindfulness meditation training for military combat veterans at a community mental health agency, findings revealed that despite continued challenges with mental focus and intrusive memories, participants who completed the intervention reported reduced rage, anxiety, and emotional reactivity, and increased feelings of relaxation, peace, self-awareness, and self-efficacy.27
By interviewing participants about the different components of a multifaceted MBI, such as the specific practices, instructions, and techniques, insight could be garnered from the participants’ differential experiences, bringing us closer to understanding which elements may be most effective for whom. Additionally, qualitative research may assist us in understanding the contextual relationship among individuals’ psychological processes, behaviors, and situationally defined environments, that is, how the interventions fit within the context of the participants’ own lives.20 Finally, qualitative research invites a broader perspective and informs researchers about what was most important to the participants, which, ultimately, may be helpful in the further development of appropriate questions and outcome measures for future MBI interventions, as well as increasing our ability to optimize mechanisms in future interventions. Therefore, the primary aim of this study was to explore and compare the subjective experience of veterans with PTSD who participated in either (a) body scan meditation, (b) mindful breathing, (c) slow breathing without mindfulness training, or (d) a sitting quietly control group.
Methods
This study examined de-identified, archival data collected as part of a larger study conducted at the Oregon Health and Science University (OHSU) Neurology Department during May 2009 to April 2013. This parent study was approved by the OHSU’s institutional review board board, and all participants signed informed consent. The purpose of the parent study was to characterize the mechanism of action of slow breathing versus mindfulness in people with PTSD, and to examine 3 potential physiological pathways of individual components of meditation.28 For the parent study, the researchers employed an RCT design in which 102 veterans with chronic PTSD were assigned to 1 of 4 arms: (a) body scan, (b) mindful breathing, (c) slow breathing, or (d) sitting quietly. Specific details regarding the methods and procedures of the parent study can be found in Wahbeh et al.28 Following the intervention, participants were asked open-ended interview questions regarding the effects of the training.
Participants
Inclusion criteria were as follows: (a) combat veteran, (b) chronic PTSD diagnosis confirmed through clinician interview, (c) age (25-65 years), (d) any gender, (e) good general medical health; (f) stable dose of medications and therapy for duration of the study, and (g) a willingness and ability to provide informed consent. Exclusion criteria were as follows: (a) significant chronic medical illness in which symptoms and/or treatment precluded participation; (b) psychiatric or behavioral illness such as schizophrenia, schizoaffective disorder, bipolar disorder, psychotic disorder (not including transient dissociative states or flashbacks associated with PTSD re-experiencing symptoms), any Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) cognitive disorder, current delirium, psychiatric instability or situational life crises (including evidence of being actively suicidal or homicidal), or any behavior that posed an immediate danger to the participant or others; (c) substance use disorder within 3 months of the study or current substance use other than marijuana and alcohol (no more than 2 drinks/day by self-report); (d) sexual assault as primary PTSD event(s) (to reduce heterogeneity from traumatic event); (e) planning to move from the area in the next year; or (f) prior or current meditation practice defined as more than 5 minutes per day for 30 days over the last 6 months. PTSD diagnosis was confirmed through the Clinician-Administered PTSD Scale for DSM-IV29 and other mental disorders were assessed through the Structured Clinical Interview for DSM-IV.30
Procedures
Veterans with PTSD were recruited through multiple methods including flyers, local newspapers, and outreach talks that were conducted at veteran PTSD support groups, mental health clinics, and veteran centers. All participants had a telephone screening, screening visit, baseline visit, 6 training visits, and an endpoint visit. If an individual was deemed eligible, she/he completed the baseline assessments and was randomized into 1 of the 4 groups: (a) body scan meditation (BS; n = 27), (b) mindful breathing (MB; n = 25), (c) slowed breathing without mindfulness training (SB; n = 25), or (d) a sitting quietly (SQ; n = 25) control group. Participation allocation was determined with a covariate adaptive randomization approach to reduce selection bias and to ensure arms were well matched on important baseline characteristics (age, gender, and depressive symptoms).31 Qualitative data were obtained via semistructured interviews following the intervention. Participants were asked, “Did you benefit from the intervention?” and “Did your PTSD symptoms improve?” Audio recordings of the interviews were transcribed verbatim.
Intervention
Participants were trained one-on-one by a research assistant once a week for 6 weeks. The BS intervention employed the body scan meditation, which is the first formal mindfulness technique introduced and practiced intensively in MBSR. The body scan meditation is a somatically oriented, attention-focusing practice designed to increase nonreactive, interoceptive awareness.32 Interoceptive awareness enhances the felt sense of being localized within one’s physical body; references the lived, immediate experience of one’s own body; and cultivates a subtle distinction between thinking about the body and perceiving the body.33 During the body scan practice, attention is directed sequentially throughout the body with the intention of cultivating a nonjudgmental awareness of physical sensations, cognitions, and emotions.34 Sensations in each area are carefully observed with a particular consideration to simply perceive rather than think about or evaluate them. As the mind becomes distracted, attention is gently returned to the bodily sensations arising and dissolving within that moment. A 20-minute guided meditation was done in silence, stillness, and sitting upright. When the mind became distracted by thoughts or emotions, the participants were instructed to bring their attention back to the part of the body that was the focus of awareness. Nowhere in the script was attention directed to the breath or breathing process. To reduce variability, recordings were used to ensure everyone in each group received exactly the same meditation each time.
The MB intervention employed another common component of MBSR: mindful breathing. Using a 20-minute guided meditation, participants sat upright and attempted to focus attention on their breath as it passed through the opening of the nostrils or on the rising and falling of the abdomen or chest. Whenever attention wandered from the breath, participants were instructed to simply notice the distracting thought, let it pass, and return attention to the breath. This process continued as a scripted meditation. As with the BS group, to reduce variability recordings were used to ensure everyone in each group received exactly the same meditation each time. Both groups received psychoeducation of mindfulness at each visit, and participants were given a tape or CD to guide them through the meditation for their daily home practice between sessions.
SB participants were trained on the breathing device RESPeRATE designed to reduce respiratory rate. RESPeRATE consists of a respiration sensor, headphones, and a control box containing a microprocessor. The system registers the participant’s breathing rate and pattern and personalizes a melody with 2 tones that correspond to inspiration and expiration. These tones then gradually slow to a rate of less than 10 breaths per minute. Participants practiced with RESPeRATE once a week for 20 minutes in the laboratory with the interventionist. Respiration was monitored and recorded continuously at all laboratory trainings to ensure participants were actually slowing their breath from their resting breath rate. The participants were given a RESPeRATE device for use at home and asked to practice daily between laboratory trainings. This group did not receive any mindfulness training.
The SQ control group sat quietly and listened to a neutral-content book on tape for 20 minutes to serve as a time and attention control at each laboratory session. Participants were also asked to sit quietly at home daily and read, listen to a book on tape, or watch TV. No formal instruction was given about what to do, other than to sit quietly. At the end of their participation in the study, SQ participants were given tapes of the mindfulness body scan and mindfulness breathing meditations.
Analytic Strategy
Audio recordings of the interviews were transcribed verbatim. Analysis of the interviews was conducted by employing a conventional content analysis in which coding categories were derived directly from the text data.35 To analyze the current data, the first and fourth authors independently reviewed the transcripts in their entirety to get an overall sense of the data. Next, each transcript was individually reread to identify recurring words, phrases, or concept and develop preliminary codes (ie, open coding). The 2 researchers then discussed their independently developed codes, resolved differences, and devised a final coding scheme. The final coding scheme was then applied to all the transcripts by 3 coders (first, third, and fourth authors). Once all transcripts had been coded, the first author examined all data within a particular code. Codes were then sorted into categories based on how different codes are related and linked. These emergent categories were used to organize and group codes into meaningful clusters. Some codes were combined during this process, whereas others were split into subcategories. Definitions for categories were developed.35,36 Next, to make the emerging patterns more explicit, qualitative themes were transformed into quantitative data.37,38 This allowed for the application of statistical analytical techniques.39 The percentage of participants who endorsed a specific theme within each intervention was calculated. Two-proportion z tests (2-tailed) were then calculated to determine if the differences among treatment groups were statistically significant.
To strengthen the validity of the qualitative analyses, triangulation was employed. Triangulation involves making use of multiple and diverse sources, methods, investigators, and theories to provide corroborating evidence to illuminate a theme or perspective.40 Evidence of triangulation in this study included interviews with multiple participants in the study (n = 102), and frequent consultation with a research mentor who has extensive expertise in qualitative methods with MBIs. Furthermore, each interview was examined by 3 coders using the conventional content analysis.35,41
Results
Sample Characteristics
The sample consisted of 102 veterans (96 males and 6 females) diagnosed with chronic PTSD. The mean age for participants was 52 years (range = 25-65; SD = 12). Fifty-five percent of the veterans reported duty in the Vietnam War, 34% in Operation Enduring Freedom or Operation Iraqi Freedom, and 11% in other conflicts. Seventy-seven percent identified as Caucasian, 2.6% as African American, 3.5% as Native American, 1.8% as Asian, 3.5% as Hispanic, and 0.9% identified as other. Sixty-six percent reported being married. Two percent of the participants reported fewer than 12 years of education, 47% reported 12 to 14 years, 26% reported 15 to 16 years, and 25% reported more than 16 years of education. There were no significant differences on important demographics variables.
PTSD and Related Symptoms
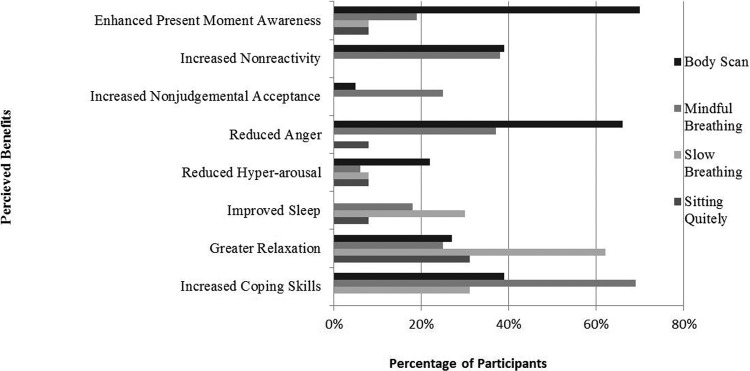
More participants in the mindfulness intervention groups (BS and MB) reported improvement in PTSD symptoms when compared to participants in the SB or SQ groups (BS 70%, MB 69%, SB 42%, SQ 42%; see Table 1). Six core themes emerged from analysis of participant responses across the 4 groups: (a) enhanced present moment awareness, (b) increased nonreactivity, (c) increased nonjudgmental acceptance, (d) decreased physiological arousal and stress reactivity, (e) increased active coping skills, and (f) greater relaxation. Each of the themes and subthemes are displayed in Table 2 and are explored below with illustrative quotes from the participants. Type of intervention appeared to influence the perceived benefits (Figure 1), which will be described in more detail below.
Table 1.
Percentage of Veterans Who Endorsed Benefiting From the Study.
| Did You Benefit? |
Percentage of Veterans Who Endorsed Benefiting Compared With Other Groups, Z Scores (P Values) |
|||||
|---|---|---|---|---|---|---|
| Group | Yes | No | BS | MB | SB | SQ |
| Body Scan | 70% | 30% | — | 0.1 (.94) | 2.0 (.04*) | 2.0 (.04*) |
| Mindful Breathing | 69% | 31% | 0.1 (.94) | — | 1.9 (.05*) | 1.9 (.05*) |
| Slow Breathing | 42% | 58% | 2.0 (.04*) | 1.9 (.05*) | — | 0 (1) |
| Sitting Quietly | 42% | 58% | 2.0 (.04*) | 1.9 (.05*) | 0 (1) | — |
Abbreviations: BS, Body Scan group; MB, Mindful Breathing group; SB, Slow Breathing group; SQ, Sitting Quietly control group.
*P < .05.
Table 2.
Final Coding Scheme.
| Theme | Subtheme | Illustrative Quotation(s) |
|---|---|---|
| 1. Enhanced present moment awareness | Deliberate focus of attention or awareness on the present moment physical, mental, emotional, or behavioral states | “I am more aware of personal breathing, sitting, posture, moment to moment.” |
| “I am more aware of negative behaviors. I notice them earlier.” | ||
| Increased ability to remember to return to the present moment | “I can leave past and future and live in the present.” | |
| 2. Increased Nonreactivity | General improvement in responding to symptoms | “Symptoms have not changed but my response to them as changed. Most notable change is the process of dealing with them.” |
| Newly developed spaciousness to pause, or an ability to “step back” from internal or external stimuli | “I am able to step back, calm down, not enrage as would have been the case before.” | |
| 3. Enhanced Nonjudgmental Awareness | “I am able to acknowledge my thoughts and put them at ease.” | |
| 4. Decreased physiological arousal and stress reactivity | Decrease in hypervigilance/hyperarousal | “[I have] less amplified triggers, feeling less nervous, more calm, and more comfortable in general.” |
| Reduced anger and irritability | “Anger management and road rage [has improved]. [I] don’t get anger as often and it is easier to cool down.” | |
| Enhanced sleep | “I have not had as many bad dreams. I am sleeping better.” | |
| 5. Increased employment of active coping skills | “I do the breathing exercises if I feel crowded and I can think more clearly than I did before to handle the situation.” | |
| 6. Greater relaxation | “I am more calm and relaxed.” |
Figure 1.
Themes revealed from qualitative content analysis by intervention group.
Theme 1: Present Moment Awareness
A salient component of the practice of mindfulness is an intentional allocation of attention to the present moment. This perceived benefit was more likely to be endorsed in the mindfulness interventions groups and most frequently endorsed in the BS group (BS 55%, MB 19%, SB 8%, SQ 8%; see Table 3). Furthermore, if an individual endorsed enhanced present moment awareness, the type of intervention appeared to influence how enhanced present moment awareness was described. For example, participants in the BS group frequently described present moment awareness as a deliberate focus of attention or awareness to their physical, mental, emotional, and behavioral states.
Table 3.
Differences of Themes Endorsed Among Groups.
| Group With Highest |
Percentages of Themes Endorsed and Z Scores (P Values) Comparing Group With Highest Percent Endorsed to Other Groups |
|||||
|---|---|---|---|---|---|---|
| Theme | Percentage Endorsed | Body Scan | Mindful Breathing | Slow Breathing | Sitting Quietly | |
| Present moment awareness | ||||||
| BS | 55% | — | 19% | 8% | 8% | |
| — | 2.5 (.008*) | 3.6 (.0003*) | 3.6 (.0003*) | |||
| Nonreactivity | ||||||
| BS | 39% | — | 38% | 8% | 0% | |
| — | 0.10 (.95) | 2.6 (.009*) | 3.5 (.005*) | |||
| Nonjudgmental acceptance | ||||||
| MB | 25% | 5% | — | 0% | 0% | |
| 2.0 (.04*) | — | 2.7 (.008*) | 2.7 (.008*) | |||
| Decreased arousal and stress reactivity | ||||||
| BS | 72% | — | 57% | 30% | 8% | |
| — | 1.1 (.26) | 3.0 (.003*) | 4.7 (<.0001*) | |||
| Hypervigilance | ||||||
| BS | 22% | — | 6% | 8% | 8% | |
| — | 1.6 (.10) | 1.4 (.16) | 1.4 (.16) | |||
| Anger | ||||||
| BS | 66% | — | 37% | 0% | 0% | |
| — | 2.1 (.03*) | 3.4 (.007*) | 3.4 (.007*) | |||
| Sleep | ||||||
| SB | 30% | 0% | 18% | — | 8% | |
| 3.0 (.003*) | 1.0 (.32) | — | 2.0 (.04*) | |||
| Coping skills | ||||||
| MB | 69% | 31% | — | 39% | 0% | |
| 2.7 (.007*) | — | 2.1 (.03*) | 5.2 (<.0001*) | |||
| Relaxation | ||||||
| SB | 62% | 27% | 25% | — | 31% | |
| 2.5 (.01*) | 2.6 (.008*) | — | 2.2 (.03*) | |||
Abbreviations: BS, Body Scan group; MB, Mindful Breathing group; SB, Slow Breathing group; SQ, Sitting Quietly control group.
*P < .05.
BS177: I am more aware of personal breathing, sitting, and posture moment-to-moment.
BS 214: (I) am more aware of negative behaviors. (I) recognize them sooner.
BS 227: I learned how to pay attention better, noticed things I never did before, pay attention to myself.
BS 213: When triggered, I notice mind wandering.
BS 222: Even when I am not stressed, I take a few minutes to be mindful of things I would not [normally] pay attention to.
However, participants in the MB group were more likely to describe enhanced present moment awareness as an enhanced ability to remember to return to the present moment when drifting into thinking about the past or future:
MB 186: I am focused on the here and now, rather than the past troubling events.
MB 185: I am learning how to live in the present, leave the future and past alone, and live in the now.
MB 223: I can leave past and future and live in the present.
Theme 2: Nonreactivity
A second theme that emerged from participant responses was enhanced nonreactivity to internal experiences. Nonreactivity entails observing thoughts and emotions without overidentifying with them or reacting to them in an automatic, habitual way. Enhanced nonreactivity introduces a space between one’s perceptions and one’s behavioral, mental, or emotional responses. In this way, mindfulness practices help individuals respond reflectively to situations, instead of reacting to them based on conditioned habits. Nonreactivity was more frequently endorsed in the BS (39%) and MB (38%) groups than in the SB group (8%) or SQ group (0%). One participant in the MB group, MB 222, described enhanced nonreactivity as follows: “I can let negative feelings go, be in the moment, and not let them consume me so much.” Participants in both mindfulness intervention groups (BS and MB) acknowledged that, although the PTSD symptoms were still present, their ability to respond to the symptoms had markedly changed.
BS 227: Symptoms haven’t changed but [my] response to them has changed. Most notable change is in process of dealing with them.
MB 162: Yes [my symptoms did improve]. If not the symptoms themselves, my reactions to them.
MB 194: Symptoms didn’t go away, but can better deal. It’s one more tool in my kit.
Participants who received the body scan intervention were more likely to describe a newly developed spaciousness, an ability to pause before responding, or an enhanced ability to “step back.” This language was used consistently within the BS group, but not among participants in other groups.
BS 165: I am also more able to sit back and think of something before I do it.
BS 171: I sit back and breathe instead of getting mad and getting in someone’s face.
BS 208: It encouraged me and reminded me to slow down. Not reacting so fast. Actively attempting to pause before I speak, I put more thought into what I say rather than blurt out what I FEEL.
BS 193: [I am] able to step back, calm down, not enraged as would have been the case before.
Theme 3: Nonjudgmental Acceptance
A third theme that emerged was enhanced nonjudgmental acceptance. Nonjudgmental acceptance is an alternative to experiential avoidance and involves an awareness and openness to cognitions, emotions, and sensations as they occur without unnecessary attempts to change their frequency or form. Acceptance abandons the attempt to control internal experiences that are not readily controllable and that may paradoxically increase in frequency and intensity when efforts are made to avoid these experiences. Acceptance is a willingness to fully experience the present moment without defense and to make space for all aspects of the internal experience, whether pleasant, unpleasant, or neutral. This theme was only endorsed in the 2 mindfulness intervention groups, and most frequently in the MB group (BS 5%, MB, 25%, SB 0%, SQ 0%).
BS 184: I am less judgmental.
MB 162: It made it easier for me to accept when I have a flashback. I am able to better accept it and move on.
MB 223: I am able to acknowledge my thoughts and put them at ease.
Theme 4: Decreased Physiological Arousal and Stress Reactivity
A fourth endorsed benefit was decreased physiological arousal and stress reactivity, which included diminished hypervigilance/hyperarousal, reduced irritability and frequency or intensity of angry outbursts, and enhanced sleep. Participants in the BS group most frequently endorsed decreased physiological arousal and stress reactivity (72%) when compared to the other group participants (MB 57%, SB 30%, SQ 8%); however, type of intervention appeared to influence which symptoms of physiological arousal and stress reactivity were improved. For example, though not statistically significant, participants in the BS group reported a decrease in hypervigilance/hyperarousal more frequently than did participants in the other groups, (BS 22%, MB 6%, SB 8%, SQ 8%).
BS 223: I feel less jumpy.
BS 161: [I have] less amplified triggers, feeling less nervous, more calm, and more comfortable generally.
BS 208: I don’t feel as vulnerable as I did. I have learned to identify my triggers, and the triggers are not as amplified.
Reduced anger was only reported in the mindfulness interventions, and most frequently in the BS group (BS 66%, MB 37%, SB 0%, SQ 0%).
BS 231: I learned to control my anger better.
BS 191: Recovery time [from anger] has improved.
MB 231: Anger management and road rage [has improved]. [I] don’t get angry as often and [it’s] easier to cool down.
MB 212: [I am] less frustrated at “stupid Portlanders.” [I] get less angry.
Improved quality of sleep was endorsed in the breathing interventions (MB 18%, SB 30%) and SQ (8%) groups, but not the BS group (0%). Furthermore, only participants in the SB group reported reduced nightmares.
MB 170: I can sleep a little longer.
MB 217: I still have nightmares and intrusive thoughts, [but now] I can get back to sleep quicker.
SB 187: I have not had as many bad dreams. I am sleeping better.
SB 195: After a while, some nights [I] did not have dreams or problems.
Theme 5: Increased Active Coping Skills
Coping can be viewed as a collection of purposeful effort to regulate aspects of the self and the environment when under stress. Passive coping refers to avoidance of the stress, whereas active coping refers to self-regulatory mechanisms that help a person adapt to the stress through cognitive reappraisal, positive thinking, acceptance, or distraction.42,43 Individuals in all 3 intervention groups described having an increase in active coping strategies to employ when faced with stress, triggers, or adversity; participants in the MB group most frequently endorsed increased employment of coping skills (69%) when compared to the other groups (BS 31%, SB 39%, SQ 0%).
BS 227: [The body scan practice] has given me another tool.
MB 180: Yes, I use mindful breathing now when I encounter stressful situations.
MB 207: I do the breathing exercises if I feel crowded, and I can think more clearly than I did before to handle the situation.
SB 211: I use slow breathing mode to slow down. It has become a response to a stressor.
Theme 6: Greater Relaxation
Bodily tension is released through relaxation, leading to a psychophysiological state of decreased arousal that opposes that of the stress response and is experienced as a calming state.44 Greater relaxation was most frequently endorsed in the non-mindfulness intervention sitting quietly control groups (BS, 27%, MB 25%, SB 62%, SQ 31%).
SB 203: I am more calm and relaxed.
SB 207: Being more calm and relaxed helps me cope with other people.
SQ 173: It helps me relax.
Sitting Quietly Control Group Findings
Despite not receiving any formal intervention, 42% of veterans reported improvements in PTSD symptoms. Control group participants did not report benefits of increased nonreactivity, nonjudgmental acceptance, or employment of active coping skills in the face of stress and adversity. Very few participants reported enhanced present moment awareness, decreased physiological arousal and stress reactivity, reduced anger, or improved sleep. Interestingly, however, they did report benefits that did not fit within the main themes found among experimental group participants. For example, a few participants reported that setting aside some time each day to reflect on the day’s occurrences was beneficial. One participant reported enjoying being put in a “time-out” and have a “20-minute break alone with my thoughts.” Another participant reported that sitting quietly helped him “collect (his) thoughts and digest the day.”
Discussion
The aim of this study was to explore and compare the subjective experiences of veterans with PTSD who participated in either (a) body scan meditation; (b) mindful breathing meditation; (c) slow breathing without mindfulness training; or (d) a sitting quietly control group. Posttreatment interviews following the 6-week interventions suggested that more participants in the mindfulness intervention groups (BS and MB) experienced improvements in PTSD symptoms when compared to participants in the SB or the SQ group. Six core themes emerged from an analysis of participant responses across the 4 groups: (a) enhanced present moment awareness, (b) increased nonreactivity, (c) increased nonjudgmental acceptance, (d) decreased physiological arousal and stress reactivity, (e) increased active coping skills, and (f) greater relaxation.
The results are largely consistent with theoretical models and empirical data that have suggested a range of potential mechanisms in mindfulness practice and MBIs. In a systematic review, Hölzel et al45 integrated neuroscientific findings with self-report and experimental data to propose 4 mechanisms through which mindfulness works: (a) attention regulation, (b) body awareness, (c) emotion regulation, and (d) change in perspective on a “static” self. In a recent systematic review and meta-analysis, Gu et al46 found strong consistent evidence for cognitive and emotional reactivity and moderate and consistent evidence for mindfulness, rumination, and worry as mechanisms underlying MBIs. In the current study, veterans’ subjective experiences suggest that type of treatment may also differentially affect potential mechanisms of action, including attention regulation, body awareness, emotional regulation, rumination, and cognitive and emotional nonreactivity. These results may inform how mindfulness and breathing practices can be tailored to the needs of the veteran with PTSD.
A majority of veterans in the mindfulness groups reported enhanced present moment awareness. In the BS group, participants described enhanced present moment awareness by a marked improvement in deliberately focusing attention or awareness on their physical, mental, emotional, and behavioral states. Veterans in this group were also more likely to describe a newly developed spaciousness, an ability to pause before responding, or an enhanced ability to “step back,” closely associated with reperceiving as described by Shapiro et al.47 Enhanced present moment awareness has previously been shown to affect emotional regulation skills.48 A prerequisite of successful emotion regulation is the awareness of emotional states, which, in turn, is associated with the awareness of bodily signals, or interoceptive awareness. Furthermore, recent research has found that enhanced interoceptive awareness facilitated downregulation of affect and created cognitive processing advantages in tasks referring to these bodily markers.49 Relatedly, 72% of participants in the BS group reported a decrease in physiological arousal and stress reactivity and 66% reported reduced anger. For therapists and clinicians working with veterans with PTSD, the body scan practice may be a beneficial preliminary intervention to enhance present moment awareness and emotional regulation skills, including reduced hyperarousal and anger.
During the MB intervention, veterans were instructed to focus their attention on the sensations of breath. When a thought or emotion arose, they were instructed to notice the passing thought or emotion without reacting to it, and return the attention to the breath. Veterans in the MB group reported enhanced present moment awareness as described by an increased ability to remember to return to the present moment when drifting into thoughts about the future or the past. This finding is associated with reduced rumination, or the tendency to repetitively think about the causes, situational factors, and consequences of one’s negative emotional experiences.50 Mindfulness has been shown to reduce rumination.51 and rumination has been found to mediate the relationship between beliefs about the trauma memory and PTSD symptoms. Together, these findings suggest that rumination is an important mechanism through which mindfulness influences PTSD symptoms.52 Enhanced awareness of the mind’s habitual tendency to ruminate, and the ability to return to the present moment, may interrupt automatic engagement in unproductive styles of cognitive processing, and ultimately, break the cycle of automatic rumination and depression associated with PTSD.53 For veterans who experience significant rumination, mindful breathing practices may be a beneficial preliminary intervention.
In the current study, we were also able to assess which specific elements of mindfulness were mostly likely to influence the subjective experience of sleep. Disrupted sleep is a common symptom associated with PTSD and has been found to increase the occurrence of a psychiatric condition onset or exacerbation of a current psychiatric condition.54,55 In a systematic review of the effects of MBIs on sleep quality, Neuendorf et al56 found that MBIs have positive effects on sleep; however, lacking in the literature are studies that consider potential mechanisms that improved sleep outcomes. In our current study, we found improved quality of sleep was only endorsed in the breathing groups (MB and SB) but not the BS group. Furthermore, only veterans in the SB group reported reduced nightmares. These findings suggest that slow and mindful breathing practices may assist with enhanced sleep quality and that participants who received training in slow breathing via biofeedback may have experienced reduced nightmares due to improved breathing patterns.57
Additionally, veterans in the BS, MB, and SB groups reported an increased ability to employ active coping strategies when facing stressors, triggers, or adverse conditions. This is a critically important finding considering approximately half of the military personnel and veterans with PTSD do not seek treatment,58,59 in part because they have insufficient coping skills that are needed for successful engagement and compliance with treatment.60,61 Passive coping, considered the avoidance of stress, is considered maladaptive and may contribute to the maintenance of PTSD symptoms. Alternatively, active coping strategies include changing the perception of an experience in a way that neutralizes the problem62 and are considered protective factors for PTSD.63 The body scan, mindful breathing, and slow breathing all appear to cultivate active coping skills. The findings are congruent with the Department of Defense and Veterans Affairs practice guidelines that suggest complementary and alternative medicines, such as mindfulness, may facilitate more engagement in care, and should be considered as a supplementary treatment for veterans with PTSD.64 Moreover, these findings provide support for non–trauma-focused approaches, such as mindfulness, for veterans with PTSD.11
Another interesting finding was that the veterans’ subjective experiences and reported benefits as revealed from qualitative analysis were incongruent with the quantitative findings reported in the parent study.28 While the parent study may have been underpowered to detect differences, quantitative results did not demonstrate meaningful change among groups in physiological or self-reported measures of PTSD symptoms. Because of the brevity of the interventions, it may be reasonable to speculate that if the interventions had been more intensive or longer in duration, changes in quantitative outcome measures might have emerged. Yet, even with the brief interventions, the qualitative data clearly displayed differences in the mindfulness arms compared to the non-mindfulness arms. The qualitative results revealed a rich understanding of how the interventions affected veterans that were not captured by quantitative analysis, including how the veterans understood the processes of mindfulness, how they integrated the processes of mindfulness into their lives, and differential effects of the individual elements.
Disparate findings between the quantitative and qualitative results may provide preliminary insight into the temporal sequence of how MBIs assuage PTSD symptoms. Although veterans in both mindfulness groups acknowledged that PTSD symptoms were still present, approximately 40% reported marked improvement in their ability to respond to the symptoms. This is congruent with literature on MBSR studies for veterans with PTSD that show a rate of clinically significant improvements of around 50%.5,11 The current findings are significant because all the veterans had been diagnosed with chronic PTSD, suggesting a prolonged course of symptoms marked by remissions and relapses.65 Yet, after 6 weeks of a brief individual mindfulness practice, veterans reported a marked ability to more skillfully respond to symptoms and reduce the escalation of symptoms once triggered. These findings are similar to results reported by Stankovic,27 in which veterans who completed an 8-week mindfulness meditation training endorsed reduced emotional reactivity while continuing to experience intrusive memories.
Perhaps enhanced nonreactivity to PTSD symptoms is an important precursor to PTSD symptom reduction in MBIs. Two recent studies have found increased nonreactivity predicted improvements in veterans with PTSD. Colgan et al66 found that for veterans with PTSD who engaged in a mindful breathing practice, change in nonreactivity predicted posttreatment depression. Stephenson et al67 found that increased nonreactivity following MBSR was independently associated with improved PTSD symptoms among veterans. These findings are also consistent with the hypothesis that nonreactivity may facilitate exposure, which is a key mechanism proposed to explain how mindfulness interventions positively impact PTSD.68,69 Further quantitative and qualitative mechanistic studies are necessary to determine the temporal progression of how mindfulness may reduce PTSD symptoms.
Finally, despite not receiving any formal intervention, some of the sitting quietly control group participants reported benefiting from the study. While this was surprising, the reported benefits were markedly different from those of the intervention groups. They did not endorse increased nonreactivity, nonjudgmental acceptance, or employment of active coping skills. Very few reported enhanced present moment awareness, decreased physiological arousal and stress reactivity, reduced anger, or improved sleep. Perhaps setting aside quiet time each day allows for reflection and observation of thoughts and associated emotional reactions. It may be clinically useful to understand this inadvertent finding in future research.
In summary, there are few first-person accounts in the literature that report on veterans’ subjective experiences and how they use mindfulness practices to alleviate symptoms of PTSD.24,25,27 In this study, we found that benefits endorsed by veterans who engaged in brief mindfulness and breathing practices appeared to address many of the clinical hallmarks of PTSD (avoidance of external or internal cues that can trigger re-experiencing the trauma, hypervigilance/hyperarousal, distractibility, irritability or angry outbursts, and disrupted sleep patterns14) and were associated with proposed theoretical models of mindfulness.45,46 Furthermore, different types of mindfulness treatments targeted different symptoms and aspects of well-being and, therefore, may inform how practices can be tailored to the needs of the veteran trauma survivors. Finally, the qualitative data, in contrast to the quantitative data, provided a richer understanding of the differential effects of the specific interventions and highlighted the importance of employing both quantitative and qualitative research methods when investigating the dynamic process of mindfulness.
Limitations
The results of this study must be interpreted with caution due to several limitations. First, although our data analysis followed a systematic, rule-governed procedure to ensure a certain degree of intersubjectivity of the findings, qualitative methodology remains a subjective approach that reflects the participants’ experiences and is, therefore, prone to researcher bias. Additionally, veterans’ reports may have been inflated by a tendency to answer in a socially desirable manner. Second, the sample was composed of mostly White men who identified as combat veterans with PTSD and who resided in a small city in the Northwest. Due to the exclusion criteria, very few females were included in the study, which further limited the generalizability of the findings, even within the larger veteran population. Third, because the interviews were conducted directly after the interventions, interviews provided a short-term perspective. Thus, the results lack information about long-lasting effects of mindfulness training among veterans with PTSD. Finally, what we thought was an inactive control group, SQ, was actually an active control for this population. It may be clinically useful to understand this inadvertent finding. Perhaps simply sitting quietly for 20 minutes each day may be helpful for improving PTSD symptoms.
Future researchers should continue to employ qualitative methods to elicit the rich and informative subjective experiences of veterans with PTSD. Furthermore, future quantitative researchers should investigate the temporal progression of how mindfulness strategies assuage symptoms of PTSD. Finally, 3-, 6-, and 12-month follow-ups are needed to assess the long-lasting effects of mindfulness training among veterans.
Footnotes
Authors’ Note: The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the funding agency.
Author Contributions: All authors contributed equally to this study.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research reported in this article was supported by the National Center for Complementary and Integrative Health of the National Institutes of Health (Grant Numbers T32AT002688, K01AT004951, and K24AT005121).
Ethical Approval: All relevant APA ethical standards and the code of ethics of the World Medical Association (Declaration of Helsinki) were followed in the conduct of the study. Additionally, institutional review board approval was granted by the institutions at which authors are located (OHSU IRB Number IRB00009864).
References
- 1. Wahbeh H, Senders A, Neuendorf R, Cayton J. Complementary and alternative medicine for posttraumatic stress disorder symptoms: a systematic review. J Evid Based Complement Altern Med. 2014;19:161–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Boden MT, Bernstein A, Walser RD, Bui L, Alvarez J, Bonn-Miller MO. Changes in facets of mindfulness and posttraumatic stress disorder treatment outcome. Psychiatry Res. 2012;200:609–613. [DOI] [PubMed] [Google Scholar]
- 3. Bormann JE, Thorp S, Wetherell JL, Golshan S. A spiritually based group intervention for combat veterans with posttraumatic stress disorder: feasibility study. J Holist Nurs. 2008;26:109–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bormann JE, Thorp SR, Wetherell JL, Golshan S, Lang AJ. Meditation-based mantram intervention for veterans with posttraumatic stress disorder: a randomized trial. Psychol Trauma Theory Res Pract Policy. 2013;5:259. [Google Scholar]
- 5. Kearney DJ, McDermott K, Malte C, Martinez M, Simpson TL. Effects of participation in a mindfulness program for veterans with posttraumatic stress disorder: a randomized controlled pilot study. J Clin Psychol. 2012;69:14–27. [DOI] [PubMed] [Google Scholar]
- 6. King AP, Erickson TM, Giardino ND, et al. A pilot study of group mindfulness-based cognitive therapy (MBCT) for combat veterans with posttraumatic stress disorder (PTSD). Depress Anxiety. 2013;30:638–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Thompson BL, Waltz J. Everyday mindfulness and mindfulness meditation: overlapping constructs or not? Pers Indiv Diff. 2007;43:1875–1885. [Google Scholar]
- 8. Vujanovic AA, Youngwirth NE, Johnson KA, Zvolensky MJ. Mindfulness-based acceptance and posttraumatic stress symptoms among trauma-exposed adults without axis I psychopathology. J Anxiety Disord. 2009;23:297–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wahbeh H, Lu M, Oken B. Mindful awareness and non-judging in relation to posttraumatic stress disorder symptoms. Mindfulness. 2011;2:219–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Niles BL, Klunk-Gillis J, Ryngala DJ, Silberbogen AK, Paysnick A, Wolf EJ. Comparing mindfulness and psychoeducation treatments for combat-related PTSD using a telehealth approach. Psychol Trauma Theory Res Pract Policy. 2012;4:538. [Google Scholar]
- 11. Polusny MA, Erbes CR, Thuras P, et al. Mindfulness-based stress reduction for posttraumatic stress disorder among veterans: a randomized clinical trial. JAMA. 2015;314:456–465. [DOI] [PubMed] [Google Scholar]
- 12. Grossman P, Van Dam NT. Mindfulness, by any other name…: trials and tribulations of sati in western psychology and science. Contemp Buddhism. 2011;12:219–239. [Google Scholar]
- 13. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR). Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 14. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 15. Kang HK, Bullman TA. Is there an epidemic of suicides among current and former US military personnel? Ann Epidemiol. 2009;19:757–760. [DOI] [PubMed] [Google Scholar]
- 16. McDevitt-Murphy ME, Williams JL, Bracken KL, Fields JA, Monahan CJ, Murphy JG. PTSD symptoms, hazardous drinking, and health functioning among US OEF and OIF veterans presenting to primary care. J Trauma Stress. 2010;23:108–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Possemato K, Wade M, Andersen J, Ouimette P. The impact of PTSD, depression, and substance use disorders on disease burden and health care utilization among OEF/OIF veterans. Psychol Trauma Theory Res Pract Policy. 2010;2:218. [Google Scholar]
- 18. Sharp TJ, Harvey AG. Chronic pain and posttraumatic stress disorder: mutual maintenance. Clin Psychol Rev. 2001;21:857–877. [DOI] [PubMed] [Google Scholar]
- 19. Stevanovic A, Franciskovic T, Klaric M, Rebic J. P-981-Secondary traumatic stress in wives of war veterans with PTSD. Eur Psychiatry. 2012;27(suppl 1). doi:10.1016/S0924-9338(12)75148-9. [Google Scholar]
- 20. Verhoef MJ, Casebeer AL, Hilsden RJ. Assessing efficacy of complementary medicine: adding qualitative research methods to the “gold standard.” J Altern Complement Med. 2002;8:275–281. [DOI] [PubMed] [Google Scholar]
- 21. Pope C, Mays N. Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ. 1995;311(6996):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Grossman P. On measuring mindfulness in psychosomatic and psychological research. J Psychosom Res. 2008;64:405–408. [DOI] [PubMed] [Google Scholar]
- 23. Moss AS, Reibel DK, Greeson JM, et al. An adapted mindfulness-based stress reduction program for elders in a continuing care retirement community: quantitative and qualitative results from a pilot randomized controlled trial. J Appl Gerontol. 2015;34:518–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Price CJ, McBride B, Hyerle L, Kivlahan DR. Mindful awareness in body-oriented therapy for female veterans with post-traumatic stress disorder taking prescription analgesics for chronic pain: a feasibility study. Altern Ther Health Med. 2007;13(6):32. [PMC free article] [PubMed] [Google Scholar]
- 25. Martinez ME, Kearney DJ, Simpson T, Felleman BI, Bernardi N, Sayre G. Challenges to enrollment and participation in mindfulness-based stress reduction among veterans: a qualitative study. J Altern Complement Med. 2015;21:409–421. [DOI] [PubMed] [Google Scholar]
- 26. Bormann J, Hurst S, Kell A. Responses to Mantram Repetition Program from Veterans with posttraumatic stress disorder: a qualitative analysis. J Rehabil Res Dev. 2013;50:769–784. [DOI] [PubMed] [Google Scholar]
- 27. Stankovic L. Transforming trauma: a qualitative feasibility study of integrative restoration (iRest) yoga Nidra on combat-related post-traumatic stress disorder. Int J Yoga Ther. 2011;21:23–37. [PubMed] [Google Scholar]
- 28. Wahbeh H, Goodrich E, Goy E, Oken BS. Mechanistic pathways of mindfulness meditation in combat veterans with posttraumatic stress disorder. J Clin Psychol. 2016;72:365–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Blake DD, Weathers FW, Nagy LM, et al. The development of a clinician-administered PTSD scale. J Trauma Stress. 1995;8:75–90. [DOI] [PubMed] [Google Scholar]
- 30. First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV-TR Axis 1 Disorders-Patient Edition (SCID-I/P; 11/2002 revision). New York, NY: Biometrics Research Department; 2002. [Google Scholar]
- 31. Pocock SJ, Simon R. Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial. Biometrics. 1975;31:103–115. [PubMed] [Google Scholar]
- 32. Dreeben S, Mamberg M, Salmon P. The MBSR body scan in clinical practice. Mindfulness. 2013;4:394–401. [Google Scholar]
- 33. Mehling W, Gopisetty V, Daubenmier J, Price C, Hecht F, Stewart A. Body awareness: construct and self-report measures. Plus One. 2008;4(5):1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med. 1985;8:163–190. [DOI] [PubMed] [Google Scholar]
- 35. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–1288. [DOI] [PubMed] [Google Scholar]
- 36. Coffey A, Atkinson P. Making Sense of Qualitative Data: Complementary Research Strategies. Thousand Oaks, CA: Sage; 1996. [Google Scholar]
- 37. Flick U. The Sage Handbook of Qualitative Data Analysis. Thousand Oaks, CA: Sage; 2013. [Google Scholar]
- 38. Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- 39. Hesse-Biber SN, Leavy P. The Practice of Qualitative Research. Thousand Oaks, CA: Sage; 2010. [Google Scholar]
- 40. Creswell JW. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. Thousand Oaks: Sage; 2013. [Google Scholar]
- 41. Patton M. Qualitative Evaluation and Research Methods. Beverly Hills, CA: Sage; 1990. [Google Scholar]
- 42. Connor-Smith JK, Compas BE, Wadsworth ME, Thomsen AH, Saltzman H. Responses to stress in adolescence: measurement of coping and involuntary stress responses. J Consult Clin Psychol. 2000;68:976–992. [PubMed] [Google Scholar]
- 43. Walker LS, Smith CA, Garber J, Van Slyke DA. Development and validation of the Pain Response Inventory for Children. Psychol Assess. 1997;9:392–405. [Google Scholar]
- 44. Taylor S. Outcome predictors for three PTSD treatments: exposure therapy, EMDR, and relaxation training. J Cogn Psychother. 2003;17:149–162. [Google Scholar]
- 45. Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspect Psychol Sci. 2011;6:537–559. [DOI] [PubMed] [Google Scholar]
- 46. Gu J, Strauss C, Bond R, Cavanagh K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin Psychol Rev. 2015;37:1–12. [DOI] [PubMed] [Google Scholar]
- 47. Shapiro SL, Carlson LE, Astin JA, Freedman B. Mechanisms of mindfulness. J Clin Psychol. 2006;62:373–386. [DOI] [PubMed] [Google Scholar]
- 48. Critchley HD, Wiens S, Rotshtein P, Öhman A, Dolan RJ. Neural systems supporting interoceptive awareness. Nat Neurosci. 2004;7:189–195. [DOI] [PubMed] [Google Scholar]
- 49. Füstös J, Gramann K, Herbert BM, Pollatos O. On the embodiment of emotion regulation: interoceptive awareness facilitates reappraisal. Soc Cogn Affect Neurosci. 2012;8:911–917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hoeksema-Nolen S. Responses to depression and their effects on the duration of depressive episodes. J Abnorm Psychol. 1991;100:569–592. [DOI] [PubMed] [Google Scholar]
- 51. Jain S, Shapiro SL, Swanick S, et al. A randomized controlled trial of mindfulness meditation versus relaxation training: effects on distress, positive states of mind, rumination, and distraction. Ann Behav Med. 2007;33:11–21. [DOI] [PubMed] [Google Scholar]
- 52. Bennett H, Wells A. Metacognition, memory disorganization and rumination in posttraumatic stress symptoms. J Anxiety Disord. 2010;24:318–325. [DOI] [PubMed] [Google Scholar]
- 53. Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspect Psychol Sci. 2008;3:400–424. [DOI] [PubMed] [Google Scholar]
- 54. Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry. 1996;39:411–418. [DOI] [PubMed] [Google Scholar]
- 55. Chang P, Ford D, Mead L, Cooper-Patrick L, Klag M. Insomnia in young men and subsequent depression. The Johns Hopkins Precursors Study. Am J Epidemiol. 1997;146:105–114. [DOI] [PubMed] [Google Scholar]
- 56. Neuendorf R, Wahbeh H, Chamine I, Yu J, Hutchison K, Oken BS. The effects of mind-body interventions on sleep quality: a systematic review. Evid Based Complement Alternat Med. 2015;2015:902708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Harvey AG, Jones C, Schmidt DA. Sleep and posttraumatic stress disorder: a review. Clin Psychol Rev. 2003;23:377–407. [DOI] [PubMed] [Google Scholar]
- 58. Shiner B. Health services use in the Department of Veterans Affairs among returning Iraq war and Afghan war veterans with PTSD. PTSD Res Q. 2011;22(2):1–10. [Google Scholar]
- 59. Tanielian TJL, ed. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: RAND Corporation; 2008. [Google Scholar]
- 60. Seal KH, Maguen S, Cohen B, et al. VA mental health services utilization in Iraq and Afghanistan veterans in the first year of receiving new mental health diagnoses. J Trauma Stress. 2010;23:5–16. [DOI] [PubMed] [Google Scholar]
- 61. Stecker T, Shiner B, Watts BV, Jones M, Conner KR. Treatment-seeking barriers for veterans of the Iraq and Afghanistan conflicts who screen positive for PTSD. Psychiatr Serv. 2013;64:280–283. [DOI] [PubMed] [Google Scholar]
- 62. Olff M, Langeland W, Gersons B. The psychobiology of PTSD: coping with trauma. Psychoneuroendocrinology. 2005;30:974- 982. [DOI] [PubMed] [Google Scholar]
- 63. Park M, Chang E, Sungeun Y. Protective role of coping flexibility in PTSD and depressive symptoms following trauma. Pers Indiv Diff. 2015;(82):102–106. [Google Scholar]
- 64. Veteran Affairs and Department of Defense. Clinical practice guideline for the management of post-traumatic stress. http://www.healthquality.va.gov/PTSD-Full-2010c.pdf. Published 2010. Accessed December 14, 2016.
- 65. Friedman MJ, Schnurr PP, McDonagh-Coyle A. Post-traumatic stress disorder in the military veteran. Psychiatr Clin North Am. 1994;17:265–278. [PubMed] [Google Scholar]
- 66. Colgan D, Christopher M, Michael P, Wahbeh H. The body scan and mindful breathing among veterans with PTSD: type of intervention moderates the relationship between changes in mindfulness and posttreatment depression. Mindfulness. 2015;7:372–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Stephenson KR, Simpson TL, Martinez ME, Kearney DJ. Changes in mindfulness and posttraumatic stress disorder symptoms among veterans enrolled in mindfulness-based stress reduction [published online May 6, 2016]. J Clin Psychol. doi:10.1002/jclp.22323. [DOI] [PubMed] [Google Scholar]
- 68. Hayes SC, Wilson KG, Gifford EV, Follette VM, Strosahl K. Experiential avoidance and behavioral disorders: a functional dimensional approach to diagnosis and treatment. J Consult Clin Psychol. 1996;64:1152–1168. [DOI] [PubMed] [Google Scholar]
- 69. Treanor M. The potential impact of mindfulness on exposure and extinction learning in anxiety disorders. Clin Psychol Rev. 2011;31:617–625. [DOI] [PubMed] [Google Scholar]