Abstract
Cardiovascular disease is a leading cause of disability and death worldwide. Yoga, a mind-body exercise, utilizes breathing techniques with low-impact physical activity that may be an alternative treatment for cardiovascular disease. The purpose of this systematic review was to examine yoga interventions for patients at-risk for and/or suffering from cardiovascular disease. The inclusion criteria for interventions were (a) published in the English language between 2005 and 2015; (b) indexed in MEDLINE/PubMed, CINAHL, or Alt HealthWatch; (c) employed a quantitative design; and (d) applied a yoga intervention. Twelve interventions met the inclusion criteria, of which, all documented significant improvements in one or more factors associated with cardiovascular disease. Limitations to the studies in this review included a lack of studies adhering to the inclusion criteria, small sample sizes, and high attrition rates. Despite the limitations, this review demonstrates the clear potential yoga has as an alternative and complementary means to improve cardiovascular disease risk.
Keywords: cardiovascular disease, yoga, mind-body interventions
It is estimated that by the year 2030 the number of deaths attributable to cardiovascular disease will reach 23.6 million.1 A number of risk factors have been identified for cardiovascular disease, including hypertension, hyperlipidemia, hyperglycemia, and abdominal and visceral obesity.2 Additionally, psychological factors such as depression, anxiety, and stress are also associated with cardiovascular disease morbidity and mortality.1 Because a myriad factors are attributed to cardiovascular disease, those affected by the disease tend to have a lower quality of life.3
Advances in pharmacological therapy have been utilized to reduce or reverse cardiovascular disease (cholesterol, blood pressure, etc).4 In some instances, medication is cost prohibitive and/or inappropriate, due to deleterious side effects, for certain patients. Another therapy for those suffering from cardiovascular disease, specifically heart arrhythmias, is the implantable cardioverter defibrillator. Although this device is known to save lives, it can also increase anxiety and depressive symptoms—increasing the heart rate of these patients that could lead to heart attack and death. It is estimated that, in some instances, as many as 46% of patients with implantable cardioverter defibrillators experience anxiety and nearly the same percentage experience depression.5 Despite these technological developments, the morbidity and mortality of cardiovascular disease incidence remains high.4
A number of studies have recommended decreasing fat intake to reduce the risk factors associated with coronary artery disease. Unfortunately, while short-term reductions in fat intake can lower low-density lipoprotein cholesterol and total cholesterol, high-density lipoprotein and triglyceride levels do not typically change. In contrast, exercise has shown favorable changes in cardiovascular disease factors, including high-density lipoprotein, low-density lipoprotein, and blood pressure.6
While exercise is oftentimes recommended to prevent and manage cardiovascular disease, many types of high-intensity exercises, are inappropriate, due to the physical limitations of patients suffering from the disease.3 Alternatively, yoga, a mind-body exercise, consists of low-intensity slow movements, which are appropriate for individuals of all physical activity levels.7 In addition, yoga’s stimulation of the parasympathetic nervous system has been to known to increase the relaxation response imperative for patients with or at-risk for cardiovascular disease.8
Yoga originated in India as part of the spiritual practice for hundreds of years.2 It has been described as a path to reduce stress, anxiety, and depression in both healthy and mentally ill adults.1 Yoga combines physical exercise with breathing techniques, and is characterized as a lifestyle intervention that can result in improved cardiorespiratory fitness.9,10 As a result, yoga has been studied for its efforts to address the psychological and physical risk factors associated with cardiovascular disease.
In this systematic review, the research questions addressed included the following
Is yoga an efficacious form of therapy to reduce risk factors associated with cardiovascular disease?
Are the articles reviewed comprised of valid research studies?
Are there sufficient data to draw conclusions about the efficacy of yoga for cardiovascular disease?
Methods
The inclusion criteria for this review included studies that were (a) published in the English language between 2005 and 2015; (b) indexed in MEDLINE/PubMed, CINAHL, or Alt HealthWatch; (c) employed a quantitative design; and (d) applied a yoga intervention. Because cardiovascular disease risk includes a number of factors (ie, metabolic syndrome, coronary artery disease, pulmonary dysfunction, high cholesterol, obesity, blood pressure, etc) the studies reviewed measured diverse functions as risk factors for cardiovascular disease.
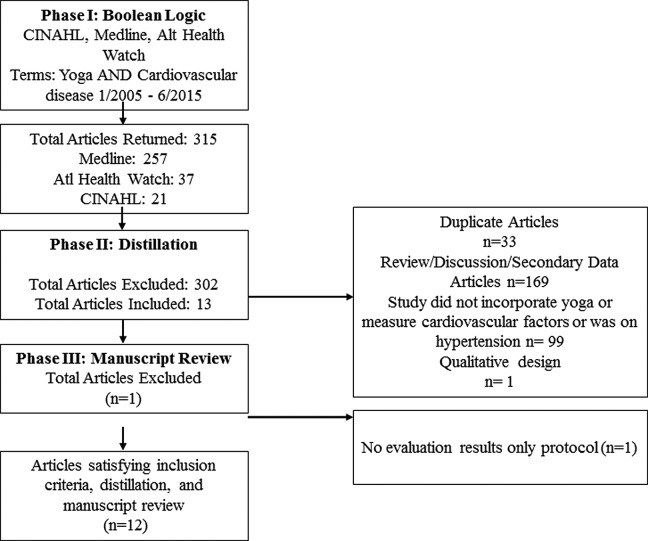
The 3 phases utilized to find studies to meet the aforementioned criteria included a Boolean search, distillation, and reference review (Figure 1). CINAHL, MEDLINE, and Alt HealthWatch databases were indexed to find studies meeting the criteria for this review as part of phase 1. The Boolean search term used was “Yoga AND Cardiovascular disease OR CVD” and “Yoga AND Coronary Artery Disease OR CAD.”
Figure 1.
Flow Chart depicting the three-phase data extraction process.
Using the above search terms, 315 articles were returned from MEDLINE (n = 257), CINAHL (n = 21), and Alt HealthWatch (n = 37). Phase II, distillation, consisted of eliminating: duplicates (n = 32), review/discussion/secondary data articles (n = 169), studies not incorporating yoga as an intervention (n = 99), and those not using a quantitative design (n = 1). Of the remaining articles (n = 13), 1 was excluded that was only an intervention protocol. The remaining (n = 12) articles satisfied the eligibility criteria (Figure 1).
Results
The results of the data extraction process included 12 articles meeting the eligibility criteria set forth in this review. The year of publication, authors, country of origin, study design, sample size, age of participants, intervention modality and dosage, outcome measures, and salient finding are listed in Table 1. The studies are listed in ascending order by year of publication.
Table 1.
Summary of Yoga Interventions for Cardiovascular Disease Performed Between 2005 and 2015 (n = 12).
| Year | Authors/Country | Design, Sample, and Setting | Age | Intervention Modality | Intervention Dosage | Outcome Measures | Salient Findings |
|---|---|---|---|---|---|---|---|
| 2005 | Bijlani, Vempati, Yadav, Ray, Gupta, Sharma, Mehta, and Mahapatra11/India | Pretest-posttest design (n = 98) of subjects with hypertension, coronary artery disease, diabetes mellitus, and/or a variety of other illnesses | 20-74 years | Asanas (postures), pranayama (breathing exercises), relaxation techniques | Integrated program of 3-4 hours daily of practice and theory for 8 days | Fasting glucose, cholesterol; low-density lipoproteins (LDL) and high-density lipoproteins (HDL), and triglycerides were measured | Fasting plasma glucose, total cholesterol, LDL, VLDL, triglycerides, and total cholesterol/HDL ratio were all significantly lower (pre vs post). HDL cholesterol was significantly higher posttest (P < .001) |
| 2006 | Marshall, Vernalis, Remaley, Walizer, Scally, and Taylor6/United States | Pretest-posttest design (n = 96) of adults known to have coronary risk factors or coronary artery disease | Adults >18 years | Unspecified yoga and supervised exercise | From weeks 2-12 (of the 3-month intervention) subjects had twice weekly yoga and exercise sessions (4 hours) | Blood pressure, heart rate, weight, body mass index, body composition, LDL, and HDL measurements | Fitness level improved (pre to post) by 22% (P < .0005). Significant decreases in LDL (13%). Significant increases in triglyceride HDL (28%). Largest HDL decrease was in the subgroup that exercised the least, but decreased their fat intake the most |
| 2009 | Howie-Esquivel, Lee, Collier, Mehling, and Fleischmann3/United States | Pretest-posttest design (n = 12) of patients with heart failure | 30-74 years | A modified yoga program (with a focus on pranayama—breathing) for patients with past injuries | Eight weeks of 3 times weekly 1-hour yoga classes and a CD for at-home practice | Physical function measures, endurance tests, quality of life assessment, Beck Depression Inventory, and the Kentucky Inventory of Mindfulness Skills | Quality of life symptom stability subscale significantly improved (P = .02) |
| 2010 | Pullen, Thompson, Benardot, Brandon, Mehta, Rifai, Vadnais, Parrott, and Khan9/United States | Randomized control design (n = 40) of patients with ischemic or nonischemic etiology of heart failure randomized to a yoga or control group | 31-76 years | Low-intensity yoga | One hour yoga sessions twice weekly for a total of 16 sessions | Living with Heart Failure Questionnaire, electrocardiography tests, plasma sampling, and a quality of life assessment | Significant increases in treadmill time (P = .002) and maximum oxygen uptake (P = .003) for yoga group compared with pretest. Plasma serum levels of interleukin-6 (IL-6), and C-reactive Protein (CRP) decreased significantly in the yoga group (pre- vs posttest) |
| 2011 | Pal, Srivastava, Tiwari, Verma, Narain, Agrawal, Natu, and Kumar12/India | Randomized control design (n = 154) of patients with coronary artery disease randomized to yoga or control groups | 40-75 years | Medication + Unspecified yoga | 35-40 minutes/day 5 days of week for 6 months of yoga practice | Body fat, body mass index, fat mass, and cholesterol levels were measured | Significant decreases in fat percentage, body mass index, fat-free mass, systolic and diastolic blood pressure, heart rate, total cholesterol, HDL and, LDL among yoga group (pre to post) |
| 2013 | Pal, Srivastava, Narain, Agrawal, and Rani13/India | Randomized control design (n = 258) of patients with coronary artery disease randomized to yoga and nonyoga groups | 35-82 years | Medication + unspecified yoga | 18 months of 5 days a week 35- to 40-minute yoga sessions | Autonomic functions, heart rate, blood pressure, and isometric strength were measured | Body mass index, waist:hip ratio, heart rate, systolic and diastolic blood pressure decreased significantly in yoga versus control group (P < .01) |
| 2013 | Sarvottam, Magan, Yadav, Mehta, and Mahapatra14/India | Pretest-posttest design (n = 30) overweight or obese male subjects (body mass index ≥23 to <35 kg/m2) | 18-55 years | Unspecified yoga | Two hours daily for 10 days of yoga practice and theory and a nutrition awareness program | Body weight, body mass index, height, blood pressure, and lipid profiles | Significant weight loss for participants (P < .001) resulting in significant reduction in body mass index (P < .001). Reduction in pulse rate (P = .02) and systolic blood pressure (P = .042). Clinically meaningful improvement in serum lipid profile (nonsignificant) |
| 2013 | Toise, Sears, Schoenfeld, Blitzer, Marieb, Drury, Slade, and Donohue5/United States | Randomized control design (n = 46) of implantable cardioverter defibrillator (ICD) recipients randomized to standard medical (control) or yoga groups | Adults >18 years | Unspecified yoga program | Eight weekly sessions of 80-minute yoga and a 30-minute at-home yoga CD to be performed 3 times a week | Florida Shock Anxiety Scale, Center for Epidemiologic Studies Depression, Positive Health Expectation Scale, State-Trait Personality Inventory, etc | Yoga group had significantly fewer device-treated ventricular (DTV) events than the control group. Yoga group had a 32% lower risk relative to control of experience DTV events. Anxiety also decreased significantly in the yoga group (pre- to postintervention) while it increased significantly for the control group |
| 2014 | Krishna, Pal, Pal, Balachander, Jayasettiaseelon, Sreekanth, Sridhar, and Gaur4/India | Randomized control design (n = 130) patients with heart failure randomized to a yoga or standard medical therapy groups | Yoga: 49.34 ± 5.70 years Control: 50.14 ± 4.54 years | Modified yoga focusing on pranayama breathing techniques | 12 weeks of 3 times weekly 60-minute yoga sessions | Heart rate, blood pressure, heart rate variability, and RPP (measurable index of myocardial oxygen consumption and load on the heart) | Significant decrease in heart rate, RPP, systolic blood pressure, and diastolic BP, and heart rate variability (low frequency) for yoga group (pre vs post). |
| 2014 | Yadav, Magan, Yadav, Sarvottan, and Netam15/India | Pretest-posttest design (n = 238) of Indian adults | 38.81 ± 11.40 years | Integral Health Clinic yoga program with asanas and pranayamas | Two weeks of 10 total 2-hour yoga sessions followed by an interactive lecture on stress management and nutrition | Lipid profile, body mass index, blood pressure, and blood glucose | Significant increase in HDL, significant reduction in blood pressure and body mass index (pre vs post) |
| 2015 | Siu, Benzie, and Woo7/China | Randomized control design (n = 182) of adults diagnosed with metabolic syndrome randomized to either a yoga or health status assessment questionnaire (control) group | 56 ± 9.1 years | Hatha yoga | Year-long thrice weekly 60-minute hatha yoga sessions | Systolic and diastolic blood pressure, fast glucose, waist circumference triglycerides, HDL cholesterol, and depression | Significant decreases in waist circumference and blood pressure (yoga vs control group posttest) (P < .005) |
| 2015 | Yadav, Singh, Singh, and Pai16/India | Randomized control design (n = 80) of patients with coronary artery disease randomized to a yoga or conventional medicine (control) group | 45-65 years | Yoga regimen of yogasanas and pranayamas | Three-month 6 days a week of 60-minute yoga practice followed by lectures/group discussions regarding lifestyle change, weight management, stress, anxiety, and diet followed by 10 weeks of at-home practice | Pulmonary function measurements—slow vital capacity, forced expiratory volume, and maximum voluntary ventilation | Significant improvement in almost all pulmonary function measurements (yoga group pre vs post). No significant improvements for control (pre vs post) |
Discussion
A total of 12 articles met the inclusion criteria for this systematic review. Of these 12 studies, 7 took place in India,4,11–16 4 studies were based in the United States,3,5,6,9 and 1 took place in China.7 All found significant improvements in some risk factor for cardiovascular disease, including both physical and mental factors, including body mass index, blood pressure, cholesterol, anxiety, depression, quality of life, weight, and pulmonary function. In each of the studies standard protocols were used to measure baseline levels of factors related to cardiovascular disease. Less than half of the studies (4 studies3,5,9,16) measured mental health and/or quality of life components of participants, which is a limitation for this review as anxiety and depression are known to play a role in cardiovascular health.5 Specifically, 1 study testing the efficacy of yoga on cardiac outcomes for patients with implantable cardioverter defibrillators, utilized the Florida Shock Anxiety Scale, Florida Patient Acceptance Survey, Center for Epidemiologic Depression Scale, Positive Health Expectation Scale, State-Trait Personality Inventory, among many others.5 In 2 other studies examined, which tested yoga for patients diagnosed with heart failure, the Kansas City Cardiomyopathy Questionnaire and the Minnesota Living with Heart Failure Questionnaire were used to measure patient’s quality of life, respectively.3,9
In this review, 5 studies3,6,11,12,14 utilized pretest-posttest design while the remaining 7 studies4,5,7,9,12,13,16 implemented randomized control trials. Pretest-posttest designs, although the simplest as no control group is enlisted, compare changes from baseline to posttest among one cohort of participants, all of which receive the intervention. Randomized control designs, however, are defined as the most rigorous as they enlist pre- and posttests, and randomize participants into a control or experimental group. By doing so, this minimizes threats to internal and external validity.
For randomized control design, it is imperative that the researchers compare baseline data between both groups to ensure that no significant differences could confound the outcomes. For a study of patients with heart failure, no significant differences (age, left ventricular ejection fraction, resting heart rate, blood pressure, weight, body mass index, flexibility, treadmill time, of biomarkers associated with cardiovascular disease) were observed at baseline between the control and intervention groups.9 In a study from 2013 that also utilized a randomized controlled design, the mean age of the control group (56.4 years) versus the intervention group (59.1 years) differed; however, whether or not this difference was significant was not addressed.13 In a study of patients with implantable cardioverter defibrillators, significant differences at baseline were associated with comorbidities. Specifically, the yoga group was significantly more likely to report comorbidities—based on the sum of the number of medication categories (antianxiety, antidepressants, beta-blockers, etc) they listed in their initial examination.5 Of the remaining studies, 3 reported no significant differences at baseline between the groups,4,7,12 while 1 study did not address this.16
Among the studies reviewed in this article, the dosage and duration of intervention varied immensely. The duration of studies ranged from 8 days11 to 1 year.7 Similarly, the dosage of the intervention ranged dramatically. One randomized controlled trial of patients with coronary artery disease practiced 60-minute yoga sessions 6 times weekly for 3 months with an additional 10 weeks of at-home practice.16 For the study with the shortest duration, a pretest-posttest design, the longest daily practice was required—3 to 4 hours daily for 8 days.11 The intervention over the longest period, 1 year,7 requested that subjects practice yoga 3 times weekly for a year. Outcomes for these studies were as follows: For the study with the shortest duration, but an intense dosage, fasting plasma glucose, total cholesterol, low-density lipoprotein, very low–density lipoprotein, triglycerides, and total cholesterol/high-density lipoprotein ratio were all significantly lower (pre vs post), while high-density lipoprotein cholesterol was significantly higher posttest (P < .001)11; for the study with the longest duration, a randomized controlled trial, only waist circumference was significantly decreased (P < .005), while researchers noted that blood pressure was decreasing following the intervention (nonsignificant) (posttest control vs yoga).7 This may suggest that a higher dosage may play a role in improving cardiovascular risk factors. To further highlight this, evidenced by a randomized controlled trial of patients with heart failure that practiced yoga 3 times weekly for 60 minutes over 12 weeks, significant decreases in heart rate, blood pressure, and rate pressure product for yoga group (vs control group posttest) (P < .001) were observed.4 Because there were few studies meeting the inclusion criteria for this review, these observations are not conclusive, but, rather, suggest additional avenues to explore regarding the efficacy of yoga to treat and improve cardiovascular disease. Additionally, comparing the improvements at 6 months and 1 year postintervention could help researchers determine optimal dosage and duration for participants, being cognizant of the feasibility for working adults, parents, and those who must travel to participate in such an intervention.
Feasibility, as defined for this review, is the likelihood that subjects could meet the expectations of the intervention, including required at-home practice and a minimum number of classes with an instructor. For the purposes of this study, attrition rates can help determine the probability that certain interventions could prove effective, not just efficacious. Few studies addressed attrition rates,4,5,9,12,14 either the reasoning behind the loss of subjects or the actual attrition they observed. In 1 study, of the 258 subjects initially enrolled in the study, 50 were lost either lost to follow-up, were deceased, or completed less than 16% of the yoga classes.12 In another study, almost 50% of the participants initially enrolled (from n = 51 to n = 30) completed the study. This study also noted poor yoga compliance, offering an explanation of work commitments and job schedules taking precedence.14 One study mentioned that, although attrition rates were not as high for their sample size, there was potential bias in favor of participants that lived close to where the yoga classes were held as well as those able to drive or commute.5
Weaknesses associated with the studies reviewed include quality of instruction and generalizability. Specifically, no study offered any type of quality assessment tool of the instructors. Terms like “yoga experts,”12–14 and “supervised sessions”4 were used in some studies, 1 study mentioned the use of a certified yoga instructor,7 but only 2 mentioned specified credentials that included years of experience instructing members of the target population (the chronically ill or those with heart problems).3,9 Three studies did not mention the use of expert instructors, making it difficult to determine the quality and/or presence of such instruction.5,6,11,14,16 Instructional classes can also be costly and inconvenient for participants, as they must travel to receive the intervention, adding to the problem of attrition. Considering the types of yoga varied among the studies (hatha yoga, yoga with supervised exercise, unspecified yoga, yoga consisting of asanas and pranayamas) along with varying instructors and populations (those with implantable cardioverter defibrillators, those diagnosed with heart failure, etc) it is difficult to compare the studies. It can be said, though, that mind-body therapies, which reinforce meditative states and focus on breathing, were similar throughout the studies reviewed.
Self-reporting is frequently an issue with any intervention that requests participants to comply with an at-home regimen as part of the intervention. Three studies incorporated an at home component as part of the intervention.3,5,16 Of these, 2 identified methods to determine, not ensure, compliance. For example, one intervention noted low subject compliance with at-home diaries (only 3 of the 27 subjects returned the diaries to the researchers) and an inability to monitor their at-home yoga practice.3 In another study, which required subjects to practice yoga for 10 weeks at home after visiting a yoga studio for 3 months, researchers called once every 3 days to check compliance as well as requested subjects come weekly to the laboratory for follow-up. It should be noted that although this follow-up can be timely and expensive, there was no attrition rate reported in this particular study (n = 80).16 Although these studies attempted to determine at-home compliance, it was impossible to assess, definitively, the amount and quality of at home practice subjects performed. It should be noted, however, that all 12 studies, not exclusively the ones that required at-home practice, reported significant improvements in risk factors associated with cardiovascular disease.
None of the interventions utilized any explicit behavior change theory. Behavior change theory helps in discerning measurable program outcomes, specifies methods for behavior change, identifies the timing of interventions, helps in choosing the right mix of strategies, enhances communication between professionals, improves replication, and improves program efficiency and effectivenss.17 There is need to incorporate behavioral theories that explain and predict behavior or behavior change such as social cognitive theory, theory of planned behavior, transtheortical model, or multi-theory model of health behavior change.17
Finally, only 1 study suggested a synergistic effect of dietary changes with yoga practice,11 3 offered nutrition lectures,14–16 but none explicitly required dietary changes as part of their intervention. Nutrition along with a yoga intervention needs to be more thoroughly explored to determine an optimal lifestyle intervention for those suffering from cardiovascular disease.
Conclusions
Only 12 studies met the inclusion criteria for this review, with only 7 utilizing randomized control design, and only three addressing the psychosocial components of cardiovascular disease. Therefore, it is clear that additional studies utilizing randomized controlled trials, performing sample size calculations, and implementing feasible duration and dosage modalities to reduce attrition rates must be performed. Additionally, it is important to take into account the social support component associated with yoga practice as all studies examined here provided group yoga classes, but there was no such social support component identified in control groups. Studies examining group yoga versus at-home yoga versus a control could be of value to measure the benefits of social support for patients at-risk for or diagnosed with cardiovascular disease. Although generalizing the efficacy of yoga may be difficult do to the variety of interventions, outcomes measured, and populations examined in the studies reviewed here, it should be noted that all 12 reported at least one significant improvement in factors associated with cardiovascular risk.
Footnotes
Author Contributions: TH conceptualized the study, collected the data, analyzed the data, developed the table, and wrote the first draft of the manuscript. MS conceptualized the study, developed the inclusion criteria, collected the data, developed the figure, analyzed the data, and reviewed the manuscript. PB collected the data, helped develop the figure, analyzed the data, and reviewed the manuscript.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: This study did not warrant institutional review board review as no human subjects were involved.
References
- 1. Yeung A, Kiat H, Denniss AR, et al. Randomised controlled trial of a 12 week yoga intervention on negative affective states, cardiovascular and cognitive function in post-cardiac rehabilitation patients. BMC Complement Altern Med. 2014;14:411–421. doi:10.1186/1472-6882-14-411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cramer H, Lauche R, Haller H, Steckhan N, Michalsen A, Dobos G. Effects of yoga on cardiovascular disease risk factors: a systematic review and meta-analysis. Int J Cardiol. 2014;173:170–183. doi:10.1016/j.ijcard.2014.02.017. [DOI] [PubMed] [Google Scholar]
- 3. Howie-Esquivel J, Lee J, Collier G, Mehling W, Fleischmann K. Yoga in heart failure patients: a pilot study. J Card Fail. 2010;16:742–749. doi:10.1016/j.cardfail.2010.04.011. [DOI] [PubMed] [Google Scholar]
- 4. Krishna BH, Pal P, Pal GK, et al. Effect of yoga therapy on heart rate, blood pressure and cardiac autonomic function in heart failure. J Clin Diagn Res. 2014;8:14–16. doi:10.7860/JCDR/2014/7844.3983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Toise SC, Sears SF, Schoenfeld MH, et al. Psychosocial and cardiac outcomes of yoga for ICD patients: a randomized clinical control trial. Pacing Clin Electrophysiol. 2014;37:48–62. doi:10.1111/pace.12252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Marshall DA, Vernalis MN, Remaley AT, Walizer EM, Scally JP, Taylor AJ. The role of exercise in modulating the impact of an ultralow-fat diet on serum lipids and apolipoproteins in patients with or at risk for coronary artery disease. Am Heart J. 2006;151:484–491. doi:10.10/j.ahj.2005.03.065. [DOI] [PubMed] [Google Scholar]
- 7. Siu PM, Yu AP, Benzie IF, Woo J. Effects of 1-year yoga on cardiovascular risk factors in middle-aged and older adults with metabolic syndrome: a randomized control trial. Diabetol Metab Syndr. 2015;7:40–52. doi:10.1186/s13098-015-0034-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Johnson CC, Taylor AG, Anderon JG, Jones RA, Whaley DE. Feasibility and acceptability of an Internet-based, African dance-modified yoga program for African-American women with or at risk for metabolic syndrome. J Yoga Phys Ther. 2014;4 doi:10.4172/2157-7595.1000174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pullen PR, Thompson WR, Benardot D, et al. Benefits of yoga for African American heart failure patients. Med Sci Sports Exerc. 2010;42:651–657. doi:10.1249/MSS.0b013e3181bf24c4. [DOI] [PubMed] [Google Scholar]
- 10. Sarvottam K, Yadav RK. Obesity-related inflammation and cardiovascular disease: efficacy of a yoga-based lifestyle intervention. Indian J Med Res. 2014;139:822–834. [PMC free article] [PubMed] [Google Scholar]
- 11. Bijlani RL, Vempati RP, Yadav RK, et al. A brief comprehensive lifestyle education program based on yoga reduces risk factors for cardiovascular disease and diabetes mellitus. J Altern Complement Med. 2005;11:267–264. [DOI] [PubMed] [Google Scholar]
- 12. Pal A, Srivastava N, Tiwari S, et al. Effect of yogic practices on lipid profile and body fat composition in patients of coronary artery disease. Complement Ther Med. 2011;19:122–127. doi:10.1016/j.ctim.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 13. Pal A, Srivastava N, Narain VS, Agrawal GG, Rani M. Effect of yogic intervention on the autonomic nervous system in the patients with coronary artery disease: a randomized controlled trial. East Mediterr Health J. 2013;19:452–458. [PubMed] [Google Scholar]
- 14. Sarvottam K, Magan D, Yadav RK, Mehta N, Mahapatra SC. Adiponectin, interleukin-6, and cardiovascular disease risk factors are modified by a short-term yoga-based lifestyle intervention in overweight and obese men. J Altern Complement Med. 2013;19:397–402. doi:10.1089/acm.2012.0086. [DOI] [PubMed] [Google Scholar]
- 15. Yadav RK, Magan D, Yadav R, Sarvottam K, Netam R. High-density lipoprotein cholesterol increases following a short-term yoga-based lifestyle intervention: a non-pharmacological modulation. Acta Cardial. 2014;69:543–549. doi:10.2143/AC.69.5.3044881. [DOI] [PubMed] [Google Scholar]
- 16. Yadav A, Singh S, Sign KP, Pai P. Effect of yoga regimen on lung function including diffusion capacity in coronary artery disease patients: a randomized control study. Int J Yoga. 2015;8:62–67. doi:10.4103/0973-6131.146067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sharma M. Theoretical Foundations of Health Education and Health Promotion. 3rd ed Sudbury, MA: Jones & Bartlett; 2017. [Google Scholar]