Abstract
The objective of this study was to assess complementary and alternative medicine use and its related factors among Iranian dermatology outpatients. In this cross-sectional study, a self-structured questionnaire was administered to 600 dermatology outpatients. Mann-Whitney U test, chi-square test, and binary logistic regression test were used. A total of 188 (31.3%) patients had used one of complementary and alternative medicine methods. The most frequent method used was herbal medicine (89.9%). The mean years of duration of the skin condition were significantly higher in complementary and alternative medicine users compared with nonusers (P = .037). Patients with acne and alopecia significantly used more complementary and alternative medicine (odds ratio: 2.48 and 3.19, respectively). There was a significant relationship between education and using complementary and alternative medicine (P < .001). Complementary and alternative medicine use is prevalent among our patients and we should think of ways of educating general population about complementary and alternative medicine methods and their potential risks and benefits and encourage our health care workers to communicate these materials with their patients.
Keywords: complementary therapies, dermatology, outpatient, Iran, traditional
Complementary and alternative medicine has received more attention through the previous decades and it has been used by the patients around the world more frequently.1,2 However, the frequency of alternative medicine use is different between countries and it varies from 5% to 74.8% in the general population.1
Patients have their reasons for demanding complementary and alternative medicine, including other treatments not being helpful, concerns or experiences of adverse effects of conventional medicine treatments, and prolonged conditions.3,4
Also, it has been seen that patients who seek unconventional methods of complementary and alternative medicine, are mostly the ones with chronic diseases, with the most frequent use in musculoskeletal disorders such as back pain,1–3,5 depression and anxiety,1–3,5,6 diabetes mellitus, 7–9 and cancers.10 Dermatologic diseases are not an exception, as complementary and alternative medicine was frequently reported to be used by dermatologic patients ranged from 35% to 69%.11
Dermatologic patients affected by psoriasis, atopic dermatitis, and melanoma seeking complementary and alternative medicine have been well established in previous studies.11–14 In addition, studies on patients referred to dermatology clinics showed that acne,15–17 contact dermatitis, and fungal infections were among the most frequent complementary and alternative medicine use indications in patients.15,17 The most popular methods of complementary and alternative medicine among these patients were herbal therapy, cologne, and prayer.15–17
Considering the long history of using traditional medicine in our country, previous studies have found that there is a positive attitude toward complementary and alternative medicine usage and an increasing demand among our people but their knowledge is limited.3,7
To the best of our knowledge, complementary and alternative medicine usage among dermatologic patients has not been surveyed in our region. Therefore, we aimed to conduct a survey to assess the complementary and alternative medicine use among Iranian dermatologic outpatients in Shiraz, Iran.
Materials and Methods
This is a cross-sectional study conducted in Shiraz, Iran from August 2014 to July 2015.
Our participants were dermatologic patients referred to Shaheed Faghihi Hospital’s outpatient clinic. Sample size was calculated to be 600. The only exclusion criterion was the lack of consent of the patients to cooperate.
We used a self-structured questionnaire with 14 items to assess the participants’ demographic, complementary and alternative medicine use, the most frequent complementary and alternative medicine method used, reason for complementary and alternative medicine use, and other related factors. Cronbach’s alpha was .7 and the experts in the field checked the validity of the questionnaire. The questionnaire was self-administered after explanation of the aim of the study and instruction for completing the questionnaire; an interviewer helped the illiterate respondents to take the survey.
For completing the questionnaires, we chose a week in each month by systematic randomization and then randomly 2 days in each week (from the 5 working days of the clinic per week) and the participants were selected conveniently in each selected day.
SPSS software version 18 was used for statistical analysis including the descriptive reported by mean ± standard deviation (mean ± SD) and frequency, Mann-Whitney U test, chi-square test, and binary logistic regression test. Alpha level of significance was considered .05.
Shiraz University of Medical sciences ethics committee approved this study.
Results
Of the 600 respondents to the survey, 214 (35.7%) were male and 386 (64.3%) were female. The mean age ± SD of the participants was 33.77 ± 16.48 years.
One hundred and eighty-eight (31.3%) of the participants had used one of complementary and alternative medicine methods for resolving their dermatologic problems and 412 (68.7%) of them had not used any complementary and alternative medicine.
Of the patients who had used complementary and alternative medicine methods, 58 (30.9%) were male and 130 (69.1%) were female. Their mean age ± SD was 36.68 ± 16.65 years. Their mean disease duration ± SD was 5.3 ± 0.53 months. The mean age and the mean years of duration of the skin condition were significantly higher in the patients using complementary and alternative medicine than those, who had not used these methods, with P values of .001 and .037, respectively. Forty-one percent of them had academic education, 36 (19.1%) had high school diploma, 40 (21.3%) elementary and middle school education, and 35 (18.6%) were illiterate. Demographic of the participants with regard to usage and nonusage of complementary and alternative medicine are shown in Table 1.
Table 1.
Demographic of the Participants With Regard to Usage and Nonusage of Complementary and Alternative Medicine (CAM).
| CAM Use | Parameter | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Gender | Marital Status | Education Levela | |||||||
| Male, n (%) | Female, n (%) | Single, n (%) | Married, n (%) | Widowed, n (%) | Group 1, n (%) | Group 2, n (%) | Group 3, n (%) | Group 4, n (%) | |
| Yes | 58 (9.7) | 130 (21.7) | 73 (12.2) | 112 (18.7) | 3 (0.5) | 35 (5.8) | 40 (6.7) | 37 (6.2) | 76 (12.7) |
| No | 156 (26) | 256 (42.7) | 199 (33.2) | 212 (35.3) | 1 (0.2) | 30 (5.0) | 109 (18.2) | 128 (21.3) | 145 (24.2) |
| Total | 214 (35.7) | 386 (64.3) | 272 (45.3) | 324 (54) | 4 (0.7) | 65 (10.8) | 149 (24.8) | 165 (27.5) | 221 (36.8) |
aGroup 1 = illiterate; group 2 = elementary and middle school; group 3 = high school diploma; group 4 = academic degree.
The most prevalent disease was eczema with 161 (26.8%) of all patients’ diagnosis, the second and third most frequent diagnosis were infectious skin problems 112 (18.7%), including warts, varicella, and fungal infections; and acne 79 (13.2%), respectively. Eczema was the most frequent disease for using complementary and alternative medicine (17%), followed by acne (16.5%) and alopecia (13.3%). There was a significant relationship between patients’ diagnosis and complementary and alternative medicine use (P = .001). Whereas, after entering the disease groups into logistic regression model, patients with acne and alopecia significantly used complementary and alternative medicine more than other diseases group (odds ratio = 2.48, 95% confidence interval 1.28-4.78) and (odds ratio 3.19, 95% confidence interval 1.62-6.27) respectively. Other disease group in this analysis includes vitiligo, skin cancers, seborrhea, hirsutism, scleroderma, vasculitis, Paget’s disease, hyperhidrosis, nail problems, Stevens-Johnson syndrome, burn, lupus erythematosus, ichthyosis, and tuberous sclerosis. Diagnosis of all patients and use and non-use of complementary and alternative medicine in each group are shown in Figure 1.
Figure 1.
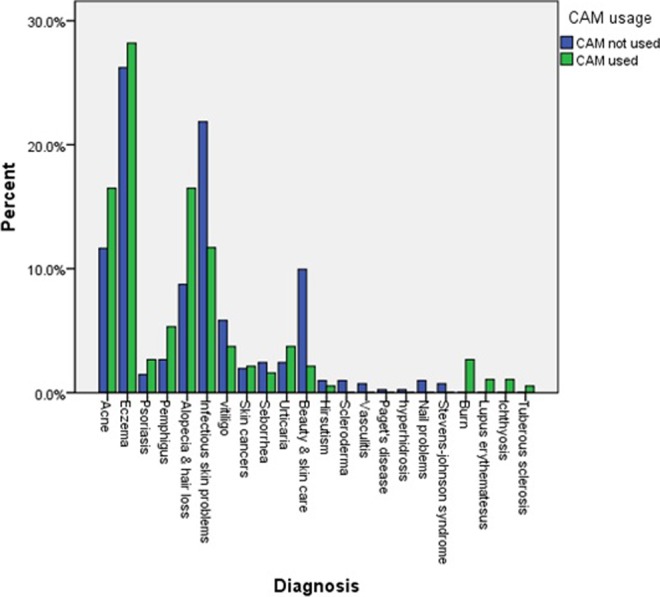
The percentage of use and nonuse of complementary and alternative medicine among different diagnosis of the participants.
The most frequent method used by our respondents was herbal medicine with 169 (89.9%) of them experiencing the use, and the second frequently used method was mineral and/or animal products (5.3%). Other methods, including acupuncture (0.5%), leeching (0.5%), hijama (cupping) (2.7%), aromatherapy (0.5%), and energy therapy (0.5%) were used very rarely.
The easier application of complementary and alternative medicine methods and their being less harmful in comparison to conventional methods and medications were among the most frequent reasons for using complementary and alternative medicine; 86 (45.7%) and 47 (25%) of the complementary and alternative medicine users’ reasons respectively. Thirty-eight patients (20.2%) thought these methods are less expensive and 9% believed they would be more effective than other treatments.
The majority of the patients using complementary and alternative medicine reported low satisfaction and believed in them having no or very low effect; 23% of the patients were moderately satisfied and only 9 (4.8%) of them had high satisfaction with complementary and alternative medicine effectiveness. However, 133 (71.1%) of the patients, who had used complementary and alternative medicine, would recommend its use to other patients and 54 (28.9%) would not recommend it.
Nonexpert people recommended complementary and alternative medicine for the skin conditions to the majority of the participants (56.9%). Sixteen percent were introduced to these methods by media, 14.4% by pharmacies, and only 24 (12.8%) of the participants were referred to complementary and alternative medicine by physicians and health care workers. Only 10 (5.3%) of them had been referred to specialized centers for complementary and alternative medicine use.
The mean duration of the complementary and alternative medicine use among the patients was 2.2 ± 1.4 months. Only 15 (8%) of the patients using complementary and alternative medicine had experienced some complications with 93.3% of that being skin complications versus one nonskin problem.
Proportion of dermatologic patients using complementary and alternative medicine was not significantly different between men and women (P = .096). There was a significant relationship between education and using complementary and alternative medicine (P < .001); the illiterate group used more complementary and alternative medicine compared with patients with academic degree (odds ratio 2.93, 95% confidence interval 1.59-5.41).
Discussion
The usage of alternative methods for different disease treatments is growing in our country and Iranian traditional medicine as a part of complementary and alternative medicine is well-known in the region and has been used from long time ago.3,18 Nevertheless, the information about the complementary and alternative medicine usage in dermatologic patients is scarce and our study is the first one in our country, which specifically assess complementary and alternative medicine use in dermatologic patients.
Approximately one-third of our patients (31.3%) had used at least one method of complementary and alternative medicine for their current skin condition. However, the lifetime prevalence of complementary and alternative medicine usage among dermatologic patients was reported to be 35% to 69% in a systematic review.11 But our result is close to the that of Gönül et al17 in Turkey, which was 33.5%, while it is less than the finding of Biligili et al15 (43.7%) in the eastern part of Turkey. This may be caused by regional or cultural differences or similarities between our country and other countries.
One of the characteristics of the patients using complementary and alternative medicine, which differed from nonusers, was their mean age. The significantly higher mean age of complementary and alternative medicine users in our study was not consistent with the findings of Tukenmez Demirci and Altunay,19 which show lower mean age of complementary and alternative medicine users. Chen et al20 found higher percentage of users in <30- and >50-year-old patients, which is partially similar to our results. Such differences may be due to difference in methodology and therefore the difference between the prevalence of dermatologic diseases and different age distribution of these diseases in studies’ samples.
The mean duration of the disease was significantly higher in complementary and alternative medicine users. This is consistent with the results of Tukenmez Demirci and Altunay.19 This shows that patients with prolonged conditions may seek alternative methods in order to improve their disease course. Higher prevalence of complementary and alternative medicine use in patients with chronic disease was also reported by other studies.4,13,21
Eczema, acne, and alopecia were the 3 most frequent diseases with complementary and alternative medicine use among the affected patients. These were among the most frequent diagnosis of complementary and alternative medicine users in other studies.16,17 We also found that patients with acne and alopecia approximately used 2.5- to 3-fold more complementary and alternative medicine than those with other skin diseases. This shows that diseases, which influence the appearance of the patients, may raise their concerns more and lead them to seek different methods of treatment.
Herbal therapy consisted about 90% of the complementary and alternative medicine methods used by our patients. We found that other complementary and alternative medicine methods, including acupuncture, leeching, cupping, aromatherapy, and energy therapy were used very rarely among our patients. The widespread use of herbal medicine in our participants may be due to the availability and accessibility of these products in our region, people’s attitude toward herbal products being more natural than other methods, and/or it may stem from its common use in Iranian traditional medicine. Herbal medicine was also one of the most frequently used methods in other studies.11,16,19
Complementary and alternative medicine methods being easier to use, less harmful and less expensive were the most, second and third frequent reasons of the patients for using them. Only a low percentage of the respondents believed that complementary and alternative medicine would be more effective. On the other hand, the majority of them had low satisfaction with the effectiveness of the complementary and alternative medicine treatments they had used. These 2 finding of our study corroborate one another. Other studies also reported these reasons of using complementary and alternative medicine.18,22 Even though the majority of the patients using complementary and alternative medicine methods believed in having no or low effect on their disease, yet the majority of them recommended others to use it. This may be due to the perception of these methods not being harmful and their perceived no or low risks versus some potential benefits, so they recommend it to others. Eşer et al16 found a significant decrease in the complaints of patients who had used complementary and alternative medicine but a low percentage of them had recommended it to other patients.
The majority of recommendations to our patients for using complementary and alternative medicine was by nonprofessional lay people and then by media and only a low percentage of physicians and health care workers had recommended it. It is important to notice the influence of community members on one another’s health-related behavior and regarding the potential risk of side effects of these methods, especially in combination with conventional medications; health policy makers should think of educating people about various methods of complementary and alternative medicine. Such findings were also reported by Eşer et al.16
Only 8% of complementary and alternative medicine users in our study had experienced side effects with majority of them being dermatologic complications. The prevalence of unwanted effects of complementary and alternative medicine among our patients was less than that reported by Tukenmez Demirci and Altunay,19 which was 18.2%, but the nature of the side effects was similar, which were mostly dermatologic allergic reactions due to herbal medicine use. Since using herbal remedies was common among our patients and it is known that these products may interact with conventional treatments, it is necessary to train our health care workers to communicate the risks with the patients in order to prevent drug adverse events.
We found that complementary and alternative medicine use was not significantly different between men and women. This was also reported in other studies.16,17 However, a population-based study in our country found that women use complementary and alternative medicine more frequently than men.3
Illiterate patients significantly used complementary and alternative medicine approximately 3-fold more than patients with academic education do in our study. This can be because people with no or low educations are more influenced by their community members’ recommendations and since nonexpert lay people mostly recommended usage of alternative treatments in our study; it may have caused more complementary and alternative medicine usage among this group. In addition, the lack of knowledge of side effects of complementary and alternative medicine methods among people with no education may have led to more use among them. Other studies did not find any significant relationship between education and complementary and alternative medicine use.16,17 However, some studies reported more complementary and alternative medicine use in people with higher education.3,23
The limitation of our study was that it was conducted in just one dermatology outpatient clinic in Shiraz. Although it is a referral center and many patients from the southern region of our country are referred to this clinic, but this study must be repeated in other parts of the country with different environmental situations and cultures to assess the generalizability and compare different regions with one another.
Conclusion
Complementary and alternative medicine use, especially herbal medicine usage, is prevalent among our dermatologic patients. People with no or low education and patients with acne and alopecia, which are related directly to their appearance, significantly used more complementary and alternative medicine than others did, while it was recommended to them mostly by nonexpert persons and not by health care workers. However, the majority of them had experienced no or low effect of complementary and alternative medicine methods on their symptoms yet they would recommend it to others. Thus, we conclude that community members’ behavior in complementary and alternative medicine use without adequate knowledge may have a nonnegligible influence on one another and since it is a prevalent matter, we should think of ways of educating general population about complementary and alternative medicine methods and their potential risks and benefits and encourage our health care workers to communicate these to their patients.
Acknowledgments
This article was adapted from the thesis of Zeinab Adelpour, using the approved proposal number 5014 by the Shiraz University of Medical Sciences.
Footnotes
Author Contributions: LD suggested the idea of the research, designed the questionnaire, and contributed toward proofreading and editing of the final manuscript. SF conducted the statistical analysis and inference and wrote and edited the final manuscript. ZA contributed toward writing the proposal and data collection. AS suggested the idea of the research, designed the questionnaire, and contributed toward proofreading and editing of the final manuscript.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This article was funded by the Vice-Chancellor for Research of the Shiraz University of Medical Sciences.
Ethic Approval: Shiraz University of Medical Sciences Ethics Committee approved this study.
References
- 1. Frass M, Strassl RP, Friehs H, Müllner M, Kundi M, Kaye AD. Use and acceptance of complementary and alternative medicine among the general population and medical personnel: a systematic review. Ochsner J. 2012;12:45–56. [PMC free article] [PubMed] [Google Scholar]
- 2. Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990-1997: results of a follow-up national survey. JAMA. 1998;280:1569–1575. [DOI] [PubMed] [Google Scholar]
- 3. Abolhassani H, Naseri M, Mahmoudzadeh S. A survey of complementary and alternative medicine in Iran. Chin J Integr Med. 2012;18:409–416. [DOI] [PubMed] [Google Scholar]
- 4. Sharples FM, van Haselen R, Fisher P. NHS patients’ perspective on complementary medicine: a survey. Complement Ther Med. 2003;11:243–248. [DOI] [PubMed] [Google Scholar]
- 5. Adams RJ, Appleton SL, Cole A, Gill TK, Taylor AW, Hill CL. Oral complementary medicine and alternative practitioner use varies across chronic conditions and attitudes to risk. Clin Epidemiol. 2010;2:251–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yekta Z, Zamani A, Mehdizade M, Farajzadegan Z. Pattern of complementary and alternative medicine use in urban population. J Res Health Sci. 2007;7:24–31. [PubMed] [Google Scholar]
- 7. Adib-Hajbaghery M, Hoseinian M. Knowledge, attitude and practice toward complementary and traditional medicine among Kashan health care staff, 2012. Complement Ther Med. 2014;22:126–132. [DOI] [PubMed] [Google Scholar]
- 8. Hashempur MH, Heydari M, Mosavat SH, Heydari ST, Shams M. Complementary and alternative medicine use in Iranian patients with diabetes mellitus. J Integr Med. 2015;13:319–325. [DOI] [PubMed] [Google Scholar]
- 9. Hasan SS, Ahmed SI, Bukhari NI, Loon WC. Use of complementary and alternative medicine among patients with chronic diseases at outpatient clinics. Complement Ther Clin Pract. 2009;15:152–157. [DOI] [PubMed] [Google Scholar]
- 10. Ernst E, Cassileth BR. The prevalence of complementary/alternative medicine in cancer: a systematic review. Cancer. 1998;83:777–782. [DOI] [PubMed] [Google Scholar]
- 11. Ernst E. The usage of complementary therapies by dermatological patients: a systematic review. Br J Dermatol. 2000;142:857–861. [DOI] [PubMed] [Google Scholar]
- 12. Fleischer AB, Jr, Feldman SR, Rapp SR, Reboussin DM, Exum ML, Clark AR. Alternative therapies commonly used within a population of patients with psoriasis. Cutis. 1996;58:216–220. [PubMed] [Google Scholar]
- 13. Hughes R, Ward D, Tobin AM, Keegan K, Kirby B. The use of alternative medicine in pediatric patients with atopic dermatitis. Pediatr Dermatol. 2007;24:118–120. [DOI] [PubMed] [Google Scholar]
- 14. Söllner W, Zingg-Schir M, Rumpold G, Fritsch P. Attitude toward alternative therapy, compliance with standard treatment, and need for emotional support in patients with melanoma. Arch Dermatol. 1997;133:316–321. [DOI] [PubMed] [Google Scholar]
- 15. Bilgili SG, Ozkol HU, Karadag AS, Calka O, et al. The use of complementary and alternative medicine among dermatology outpatients in Eastern Turkey. Hum Exp Toxicol. 2014;33:214–221. [DOI] [PubMed] [Google Scholar]
- 16. Eşer I, Khorshid L, Demir Y, Denat Y. The use of complementary and alternative medicine in dermatology patients in western Turkey. Int J Hum Sci. 2010;7:384–400. [Google Scholar]
- 17. Gönül M, Gül U, Cakmak SK, Kiliç S. Unconventional medicine in dermatology outpatients in Turkey. Int J Dermatol. 2009;48:639–644. [DOI] [PubMed] [Google Scholar]
- 18. Astin JA. Why patients use alternative medicine: results of a national study. JAMA. 1998;279:1548–1553. [DOI] [PubMed] [Google Scholar]
- 19. Tukenmez Demirci G, Altunay IK. Use of complementary and alternative medicine and assessment of dermatology quality of life index among dermatology outpatients: a cross-sectional comparative study. Br J Med Med Res. 2014;4:1812–1820. [Google Scholar]
- 20. Chen YF, Chang JS. Complementary and alternative medicine use among patients attending a hospital dermatology clinic in Taiwan. Int J Dermatol. 2003;42:616–621. [DOI] [PubMed] [Google Scholar]
- 21. Ben-Arye E, Massalha E, Bar-Sela G, et al. Stepping from traditional to integrative medicine: perspectives of Israeli-Arab patients on complementary medicine’s role in cancer care. Ann Oncol. 2014;25:476–480. [DOI] [PubMed] [Google Scholar]
- 22. Pirotta MV, Cohen MM, Kotsirilos V, Farish SJ. Complementary therapies: have they become accepted in general practice? Med J Aust. 2000;172:105–109. [DOI] [PubMed] [Google Scholar]
- 23. Schäfer T, Riehle A, Wichmann HE, Ring J. Alternative medicine in allergies—prevalence, patterns of use, and costs. Allergy. 2002;57:694–700. [DOI] [PubMed] [Google Scholar]


