Abstract
Background.
The aims of this study were to determine whether a modified Qigong breathing exercise can reduce the sense of hunger and identify possible mechanisms.
Methods.
The results from the test group, which performed the exercise, are compared with the control group, which performed deep breathing. Intestinal pressure measurements, stomach pH monitoring, and participant surveys were used for assessment.
Results.
Stomach pH was increased by 3 (0.2) and intestinal pressure was reduced by 12 (0.5) mm Hg in the experimental group and did not change significantly in the control group. The study provides strong evidence that the exercise can significantly reduce, or even suppress the sense of hunger on an empty stomach.
Conclusion.
This breathing exercise provides comfort in different circumstances, such as lack of regular meals, limited volume or caloric diet, and even during temporary complete absence of food in therapeutic fasting.
Keywords: sense of hunger, acid suppressive therapy, intestinal pressure, pH monitoring, Qigong, yoga, eating behavior, fasting, overeating, obesity
Obesity is a major health problem in the United States. The National Institutes of Health (NIH) weight categories define overweight people with the body mass index (BMI) of 25 to 29.9 kg/m2, obese with BMI of 30 to 35 kg/m2, and severely obese with BMI >35 kg/m2.1 According to the most recent data, adult obesity rate is close to 38% nationwide,2 exceeding 35% in 4 states, 30% in 25 states, and is more than 20% in all states. Louisiana has the highest adult obesity rate of 36.2% and Colorado has the lowest at 20.2%.3
NIH reports obesity as one of the leading health risk factors for mortality and morbidity. Allison et al4 reported that an estimated 300 000 deaths are due to the obesity epidemic each year in the United States, which is the second leading cause of preventable death following tobacco use.4 Besides morbidity attributed to obesity, most prevalent medical diagnosis, including diabetes, hypertension, cardiovascular disease, are all related to overweight and obesity. Thus, prevention and treatment of overweight and obesity should be one of the top health care priorities in order to improve health care outcomes and save health care dollars.
Major reasons causing excessive weight gain are availability and abundance of high-calories food,5 along with sedentary modern lifestyle.5,6 Suggested treatments of obesity include dietary therapy, physical activity, combined therapy, behavior therapy, pharmacotherapy, surgery, and other interventions.1 Today, dietary restrictions and vigorous exercises are the primary means of treating obesity offered by the health care providers. If diet and exercise are not effective, doctors resort to bariatric surgery. Balloon in the stomach or bariatric surgery, which reduces its volume, leads to satiety when less food is consumed.7,8
The sense of hunger is believed to be the main motive of food intake. Many people report that it is the main reason for overeating and resulting excess weight. Physiologically, the senses of hunger and satiety are processed in the central nervous system of animals and humans. Hypothalamus in the midbrain performs an integral function in the formation of these senses, and is recognized as regulator.9–11 These 2 senses are referred to as basic behavior motivators. Imbalance between satiety and hunger may lead to food rejection and consequent exhaustion, or overeating and consequent excess weight and obesity.12 Some researchers consider hunger as a result of changes in body’s biochemistry. Receptors that respond to glucose levels in the blood, certain hormones or metabolism products, affect the hypothalamus, changing feeding behavior.13 Pharmaceutical and nutritional dietary recommendations are based on this knowledge.
Other researchers believe that the senses of hunger and satiety are directly related to pressure on the stomach or intestinal walls.14 For example, the sense of hunger disappears when stomach is stretched and is present with no pressure.15,16 Inflated balloon stretching the stomach walls inhibits feeding behavior in animals. Modern bariatric surgery is based on this principle.17,18 Controlling the sense of hunger is the critical first step in successful dietary therapy, as well as the aim of bariatric surgery to control body weight and treat obesity. However, methods of controlling the sense of hunger without chemicals and surgical procedures would be more beneficial, considering the side effects of pharmaceutical approach and the risks of surgical procedures.
Acupuncture and Qigong as ancient Chinese traditional medicine have been documented to be effective in treating obesity.19 Literature showing that the desire to eat and the feeling of hunger, along with prospective food consumption in patients with obesity can be significantly reduced by acupuncture combined with electroacupuncture and ear point tapping.20–22 However, there was no significant difference between acupuncture and nonacupuncture groups in gastric fullness feeling.23
Zhou24 summarized Chinese literature, and described an exercise called “yuchan fanlang gong” (玉蟾翻浪功) or “frog making waves,”25 which is a hunger suppression exercise from Chinese Qigong (气功), and is often used by monks during their religious fasting. This exercise is documented to be done in supine position (lying down on your back). Knees are bent to 90°. Left hand is placed on the chest, while right hand is placed on the abdominal region. Expand the chest and depress the abdomen while inhaling, and withdraw the chest and bulge the abdomen while exhaling. Then repeat the same respiratory cycle, and a set of 40 to 60 repetitions is recommended for each exercise session with a normal breathing rate.24 In carrying out this exercise, the chest and abdomen rise and fall mimicking a frog’s breathing, thus it gets the Chinese name, which means “frog making waves.” It is advisable to do it only when feeling hungry, or before breakfast, lunch, and dinner. After this exercise, it is usually easy to skip a meal, or significantly reduce the amount of eaten food.25
The authors of this study modified this Qigong exercise from the physioanatomical perspective. The purpose of this study is to research the effectiveness and potential mechanism of the modified Qigong breathing exercises in controlling patients’ sense of hunger and reducing food intake for body weight management and obesity treatment. The hypothesized mechanism of this modified Qigong breathing exercises in controlling patients’ sense of hunger is by changing gastrointestinal system pressure and altering gastrointestinal physiological environment and activities.
Materials and Methods
The study involved 60 people (28 men and 32 women). The following anthropometric indicators were measured: height, weight, and BMI. The criterion for participants’ inclusion in the study was BMI >25 kg/m2. Exclusion criteria were the following: severe comorbidity, hemodynamic decompensation and carbohydrate metabolism disorders. All necessary permissions for conducting this research were obtained in Ukraine. The studies were conducted in Kiev, Ukraine in compliance with “The Convention for the Protection of Human Rights and Dignity of the Human Being with regard to the Application of Biology and Medicine” and World Medical Association Declaration of Helsinki “Ethical Principles for Medical Research Involving Human Subjects.” The subjects were not compensated for participating in the study. Participants were randomly divided into 2 groups of 30 people, as experimental group and control group. Each group consisted of 14 men and 16 women.
The Modified Qigong Breathing Exercise
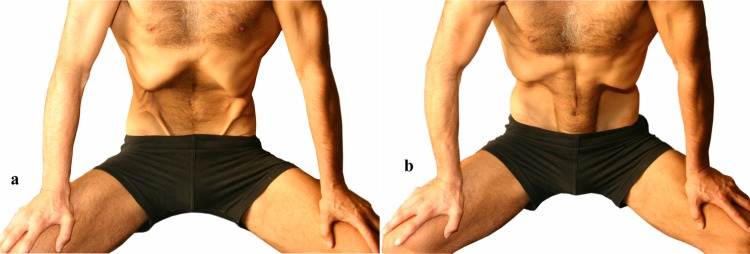
The exercise is recommended to be performed standing, or modified standing with trunk leaning forward and bilateral upper extremities support on countertop as illustrated in Figure 1. Initial position: Stand up with feet shoulder-width apart, hands down along your body, or put your palms on the abdomen (Figure 1a). Take a deep breath, squaring your shoulders, and pull in your belly at the same time. Hold your breath for 3 to 4 seconds, while keeping abdomen retracted with maximally contracting abdominal muscles (Figure 1b). Exhale, so the shoulders go back to the starting position, while chest and abdominal muscles relax. Repeat this exercise 10 times. Note. If the stomach is difficult to draw in a standing position, for example in case of obesity, it is possible to perform the exercise with both hands resting on support (Figure 1c and d).
Figure 1.
Breathing exercise. Option 1: (a) initial position; (b) holding breath for 3 to 4 seconds, while keeping abdomen retracted. Option 2 with support for obese people: (a) initial position; (b) holding breath for 3 to 4 seconds, while keeping abdomen retracted.
Intervention
The experimental group was taught how to perform this breathing exercise before the experiment. Control group consisted of people not familiar with this technique. During the experiments, each group received corresponding instructions: abstain from food for 24 hours and when hungry perform this breathing exercise as described above (experimental group) or breath deeply (control group). Instructions for control group were as follows: Take a deep breath, squaring your shoulders. Hold your breath for 3 to 4 seconds. Exhale, so the shoulders go back to the starting position, while chest and abdominal muscles relax. The rate of deep breathing is approximately 6 to 10 breaths per minute. Repeat this exercise 10 times.
To reduce bias, the patients were told that they are participating in the distraction and refocusing experiment to study their effects on the sense of hunger. Note: In the original instructions,25 holding the breath was not mentioned, but our experience has shown that this is very important. All subjects were warned that the exercise is only effective in the absence of food in the stomach. Drinking water throughout the day was allowed.
The effects of the intervention on the sense of hunger were evaluated using the following parameters.
Intensity of the Sense of Hunger
Data were collected throughout the day in points based on the survey results. Study participants evaluated their health over the past day the next morning. They answered how abstinence from food has affected them, their attention, comfort, performance, mood, and sociability. This impact was expressed on a scale from 0 (not affected) to 5 (fully affected). The full text of the questionnaire is provided in the appendix.
Stomach Acidity
Stomach acid-forming functions were evaluated by intragastric pH measurements before and after the modified breathing exercise (experimental group), and deep breathing (control group). Express pH monitoring was utilized to measure the basal gastric acidity.26 Nasogastric tube was inserted into the esophagus, reaching the lower esophageal sphincter. Initial probe length was roughly determined by the distance from the patient’s earlobe to the xiphoid process, or from the upper lip to the navel. Then pH measurements were performed every centimeter with further insertion of the probe. Overall, 20 pH measurements were made in 3 minutes. Then the probe was fixed and retained in the stomach for 10 minutes. After 10 minutes, the probe was partially extracted, and pH was measured every centimeter.27
The experimental group participants were asked to perform the modified breathing exercise 10 times between the 2 sets of pH measurements. Subjects in the control group were asked to deeply breathe for 1 minute between the 2 sets of pH measurements. After 2 to 3 minutes, the study was conducted again using the same procedure.28,29 Highest measured stomach acidity values were used for comparing the modified breathing exercise and deep breathing results.
Pressure in the Colon
Measurements were conducted when members of the test group performed the breathing exercise. The same measurements were performed with the control group when breathing deeply. This part of the study involved 15 people from the experimental group and 15 from the control group. No patients had contraindications for this study.
To estimate intra-abdominal pressure and its dynamics, techniques proposed by Kron et al30 and Iberti et al31 were used by measuring the pressure in the bladder. However, this method requires aseptic urological conditions and trained personnel. Moreover, traditionally intra-abdominal pressure is measured when the patient is in the horizontal position. The authors used the method of measuring intra-abdominal pressure in the colon, since it is a less demanding procedure and does not require trained urologists. Also, all participants cleaned their intestines, which greatly simplified the pressure measurements.32 Comparability of the data obtained by different intra-abdominal pressure measurement methods was confirmed in references.33,34
Pressure Measurement Technique
The patients were prepared for the experiment in the following way. Prior to measurements, all research subjects cleaned their bowels by drinking Epsom salt laxative (MgSO4x7H2O) at a dose of 0.5 g of Epsom salt per 1 kg of body weight. Pressure was measured using Benetech GM510 digital manometer. Foley catheter was attached to a silicone tube connected to the manometer. Catheter was filled with water before insertion into the colon to prevent its clogging by the intestinal contents. Manometer was connected to a computer with the USB cable to record the pressure data during experiments at 1 Hz frequency. Manometer was properly calibrated before experiments.
After the insertion of the catheter into the patient’s rectum to a 15-20 cm depth,32 pressure was recorded during regular breathing in a standing position. During the next 60 seconds, the subjects of the experimental group performed the breathing exercise, and the subjects in the control group were breathing deeply. Pressure measurements were conducted in the differential mode, which allowed recording pressure change with respect to the zeroed-out value.
In fact, the front end of the catheter was located at a depth of about 15 cm, that is, in the area of the sigmoid colon, since the rectum length is 12 cm on average.35 It is necessary to remember that during the intestinal pressure measurements, hydrostatic pressure component provides no useful information. Hydrostatic pressure only reflects the person’s height and relative body position. To quantify pressure changes one needs to select the reference point, taken as the “zero value.” If the subject is standing up, the manometer should be placed at sufficient height so that it measures atmospheric pressure when respiratory and abdominal muscles are relaxed after expiration. Typically, this level corresponds to the upper boundary of the stomach, at the xiphoid process of the sternum. The pressure in the intestine, measured after expiration, in a state of relaxation of the respiratory and abdomen muscles is considered “zero pressure.”
Statistical Analysis
The experimental data were analyzed using the STATISTICA software package from StatSoft Inc (USA). The data are reported as the mean value(standard deviation) or lower range–upper range (standard deviation).
Results
The study involved 60 participants. Their BMI was interpreted according to the NIH weight categories and 1997 World Health Organization classification. In the study, 10 men and 12 women had BMI in the range of 25 to 29 kg/m2 (overweight), 13 men and 15 women had BMI 30 to 34.9 kg/m2 (first-degree obese), 4 men and 3 women had BMI 35 to 39.9 kg/m2 (second-degree obese), and 1 man and 1 woman had BMI >40 kg/m2 (third-degree obese).
All participants volunteered to abstain from food for 24 hours as a part of the weight loss program. All participants previously tried water fasting or calorie-restricted diet. Each participant filled out a questionnaire, which assessed their health over the past 24 hours at the end of water fasting. All participants were randomly divided into 2 groups of 30 persons each. Experimental group participants were instructed how to conduct the breathing exercise, trying to avoid suggestive or leading statements. They received instructions to perform the breathing exercise for 1 minute every time they felt hungry and note any changes in how they felt.
Control group participants were not familiar with the breathing exercise. They were instructed to breathe deeply and slowly when feeling hungry and note any changes in how they felt.
Breathing Exercise Effects on the Sense of Hunger
The survey was used to collect patients’ subjective data on their sense of hunger before and after each intervention for both groups. The following parameters were included in the survey: attention, comfort, operability, mood, and sociability. The experimental group consisted of patients taught how to perform the breathing exercise. The control group consisted of patients not familiar with this technique.
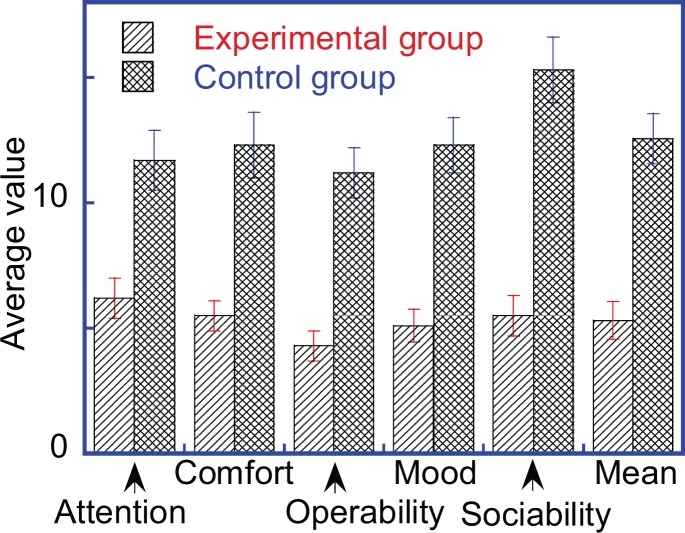
As seen from Figure 2, the control group was more negatively affected by the sense of hunger compared with the experimental group. Members of the experimental group reported significant reduction of the subjective perception of the sense of hunger after performing the breathing exercise. No significant changes were reported in the control group after deep breathing.
Figure 2.
Survey parameter results from the experimental and control groups assessing attention, comfort, operability, mood, and sociability.
Prolonged Fasting
Although therapeutic fasting is not the subject of this article, it should be noted that most of the participants (52 people) have used it after this study. Their abstinence from food, but not water lasted from 3 to 14 days. All participants noted high efficiency of the breathing exercise during all stages of fasting. It should be noted that the side effects of the breathing exercise included complete absence of gastric damage symptoms usually accompanying fasting. Namely, dense fur on the tongue, putrid breath, pain in the stomach, belching air and heartburn, poor tolerance of food in the first few days after fasting. Many patients with gastric and duodenal ulcer diseases felt better during and after fasting.
Breathing Exercise Effects on Stomach Acidity
The study involved 25 participants (out of a total group of 60 subjects). Of these, 10 people were in the control group and 15 people in the experimental group. pH measurements in both groups were carried out twice after the same time interval. Between pH measurements, control group participants were deeply breathing for 1 minute. Experimental group participants performed the modified breathing exercise for 1 minute.
The null hypothesis was that the stomach pH in the control and experimental groups was the same before the experiments. The P value was .9969, thus the hypothesis is accepted, and the stomach pH in the control and experimental groups is the same. After the intervention, the null hypothesis was that the pH did not change as a result of the modified breathing exercise in the experimental group. As seen in Table 1, gastric pH practically did not change significantly in the control group. However, after the modified breathing exercise, experimental group showed an increase in gastric pH of 2.8 to 3.1 (0.2, P < .001), and the acidity level decreased by an average of 2.15 (0.6) in the experimental group (Table 1). This change in stomach acidity is typical after a meal. The P value corresponding to the measured pH before and after the modified breathing exercise was 6.36 × 10−6, and the null hypothesis was rejected. Thus, the modified breathing exercise lowers the acidity of the stomach in the experimental group.
Table 1.
Stomach pH in the Experimental and Control Groups.
| Control Group | Experimental Group | ||
|---|---|---|---|
| First Measurement | Second Measurement | Before Breathing Exercise | After Breathing Exercise |
| 1.8-2.4 (0.5) | 1.7-2.3 (0.5) | 1.6-2.6 (0.6) | 4-4.5 (1.2) |
Pressure in the Large Intestine
Increased activity (or lack thereof) of baroreceptors in individual segments of the digestive system affects stomach and intestinal functions, and thus the feelings of hunger and satiety.36 The authors studied how the intestinal pressure is changing during normal breathing and performing various exercises, including regular breathing, deep breathing, breathing exercise (in which the belly is sucked in during inhalation), retraction of the abdomen after exhaling, and when performing nauli exercise from yoga.
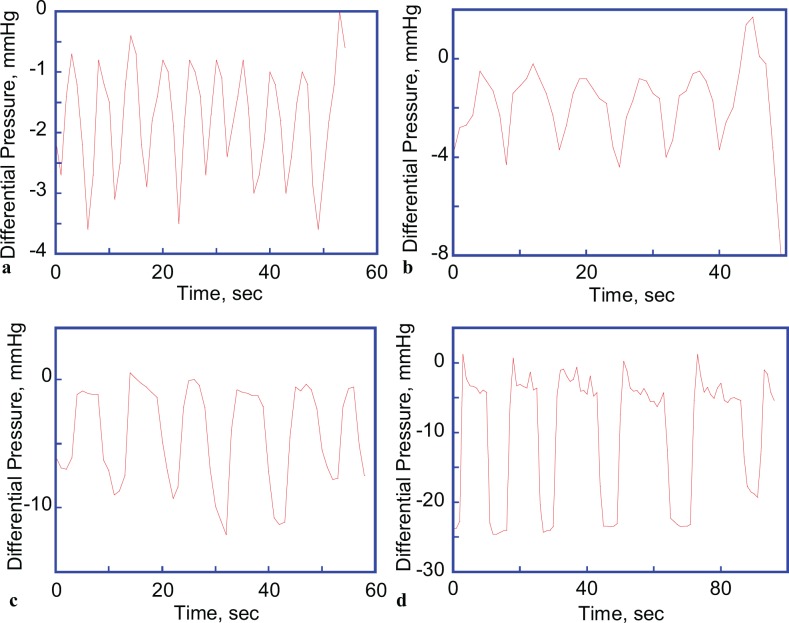
All measurements were performed in a standing position. When breathing normally, intestinal pressure changed in the 2 to 2.5 (0.5) mm Hg range during the respiratory cycle (Figure 3a), which corresponds to the pressure measured in hollow organs (Table 2).32,36–42
Figure 3.
Intestinal pressure: (a) during normal breathing in the 2 to 2.5 (0.5) mm Hg range; (b) during deep breathing with abdomen retraction on exhalation in the 2.5 to 3 (0.5) mm Hg range; (c) during performing breathing exercise with abdomen retraction on exhalation in the 9 to 12 (3) mm Hg range; and (d) during abdomen retraction after exhaling, which changed in the 20.5 to 24.3 (5) mm Hg range. Abdomen retraction was performed after exhalation, after which the subject conducted 3 normal respiration cycles. These are representative graphs of a single subject from each group.
Table 2.
Pressure measured in different areas of the digestive system.42
| Part of the Digestive System | Pressure Measured in Horizontal Position, mm Hg | Pressure Measured in Vertical Position, mm Hg |
|---|---|---|
| Mouth | 0 | 0 |
| Esophagus | 3-4 | 7.5-10 |
| Stomach | ||
| Bottom of the stomach | 4-5 | 11-12.5 |
| Pylorus | 7-9 | 20-30 |
| Small intestine | 4-5 | 18-26 |
| Large intestine | 1.5-2 | 35-45 |
It is noteworthy that during normal (Figure 3a) and deep breathing (Figure 3b), intestinal pressure decreases briefly only during inhalation. During the modified breathing exercise, pressure decreases more significantly and the duration of the negative pressure phase is slightly longer than during normal or deep breathing (Figure 3c). When retracting the abdomen after exhaling, the pressure drop is twice compared with the breathing exercise, and pressure remains low as long as the abdomen is retracted (Figure 3d). Pressure in the colon was reduced by 9 to 12 (0.5) mm Hg in the experimental group during the modified breathing exercise, and only by 0 to 1 (0.5) mm Hg in the control group during deep breathing.
This study showed high efficiency of the modified exercise in eliminating the sense of hunger during fasting. Modified breathing exercise is associated with the reduction of colonic pressure and increase in the stomach pH.
Discussion
Here are the facts observed in this study:
The modified breathing exercise reliably eliminated the sense of hunger.
Gastric acidity decreased after performing the modified breathing exercise.
Pressure reduction in the colon was registered during the modified breathing exercise.
Reduced sense of hunger lasted from 1 to several hours after performing the breathing exercise. When fasting for several days, patients did not experience hunger and starting from the second or third day of fasting they often forgot to perform the breathing exercise. What affected the sense of hunger? Based on the current study results, these changes are due to decreased stomach acidity and lowering the intestinal pressure. However, the authors believe that the primary effect is due to decreased intestinal pressure, since stomach pH control with antacid drugs does not affect the sense of hunger.43
The intestinal tube is divided by sphincters (valves) into 4 sections: the esophagus, stomach, small intestine, and large intestine. There is a certain pressure differential between these sections. Valves along with gastrointestinal motility provide movement of food in one direction, its gradual absorption and digestion.38,39 When the pressure difference on both sides of the valve reaches a certain critical value, the valve opens and the contents moves to the lower section.40 A valve or a sphincter is formed of special muscle tissue (smooth or striated), which allows adjusting the magnitude and/or duration of connection between the segments of hollow organs, preventing pressure equalization.38 During regular breathing, the pressure in the abdominal cavity changes slightly and symmetrically. During inhaling, it is reduced by 1 to 3 mm Hg, while during exhaling it is increased by the same amount.44
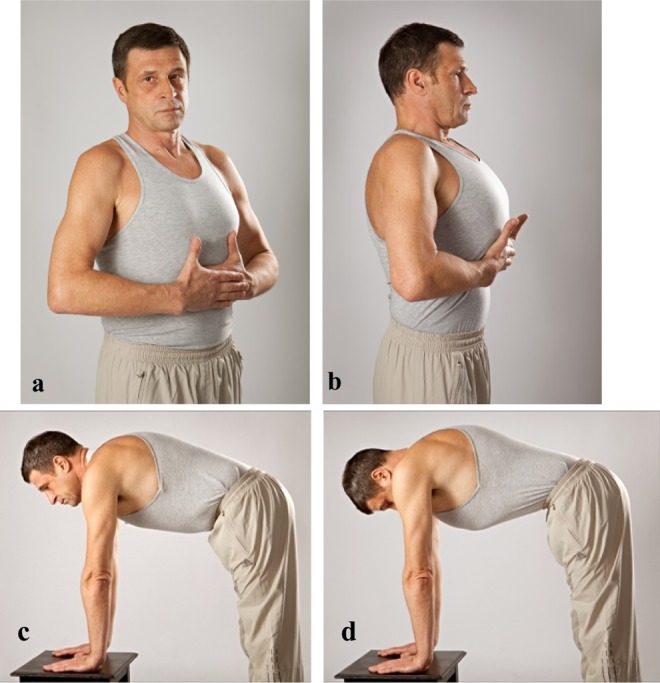
Literature suggests that measured pressure in hollow intestine strongly depends on the position of the body, that is, lying or standing.37,38,45 Typically, pressure data in body cavities have been obtained from patients in a horizontal position. If these patients were in the upright position, the gauge would have shown higher pressure. This additional hydrostatic pressure is equal to 0 in the upper part of the esophagus, and 35 to 45 mm Hg in the rectum, depending on the patient height (Table 2).42 The traditional Chinese Qigong exercise is performed in the supine position, thus the authors modified the Qigong exercise performing position from supine to standing, to achieve a larger pressure change in the body cavities, more specifically between the valves in each gastrointestinal segment. Anatomically, because of the position of the rib cage, the effect of pressure change in colon is significantly reduced with the breathing exercise performed in the supine position. This is another way to explain why the modified breathing exercise performed in standing position is more effective at achieving pressure change in the colon. Abdominal muscle retraction is another distinctive feature of this modified breathing exercise compared with the traditional Chinese Qigong exercise, which is achieved by an isolated transverse abdominal muscles activation (musculus transversus abdominis), which are typically not affected by breathing.46,47 By contracting abdominal muscles, the abdominal space is actively depressed and the intestinal tubes are also depressed with higher pressure. This isometric technique is also available in yoga, called Uddiyana Bandha (Figure 4a) and Nauli Kriya (Figure 4b).48
Figure 4.
(a) Uddiyana Bandha and (b) Nauli Kriya exercises.48
Colon pressure drops by 25 to 35 (5) mm Hg when performing Uddiyana Bandha and by 40 to 50 (5) mm Hg when performing Nauli Kriya. This explains why water is sucked into the intestines when performing these exercises in water. However, the phenomenon of pressure reduction is still not explained. Abdominal volume decrease should be accompanied by the intra-abdominal pressure increase in all hollow organs, including the intestines. There is a simple relationship between pressure (P) and volume (V), which follows the Boyle’s law:
| 1 |
At constant temperature, the pressure in the system can be reduced only by increasing the volume. In our opinion, when performing the breathing exercise (along with Uddiyana Bandha and Nauli Kriya), descending colon (colon descendens) is subjected to tension, and its length increases, while the diameter remains constant. Thus, the overall volume of the large intestine increases, while the pressure in the large intestine decreases.49 Change of hydrostatic pressure on the borders of ileocecal and gastroduodenal valves, determined by the position of bowel loops, is perhaps one of the reasons for reduced sense of hunger.
Conclusions
The effect of the sense of hunger on the eating behavior is undeniable. This study demonstrated that the sense of hunger can be consciously controlled. It can be significantly reduced or even suppressed. Practical application of the modified breathing experience lies in the fact that any person, who mastered it, can more effectively control their eating behavior, preventing overeating and obesity. Including the modified breathing exercise in therapeutic weight loss programs makes them more effective and attractive. Conducted experiments have demonstrated that the modified breathing exercise reduces stomach acidity, similar to the action of antacid drugs, which suppresses mucosa rejection after prolonged abstinence from food.
The following conclusions can be drawn:
Subjective sense of hunger was significantly lower in the experimental group, which performed the modified breathing exercise than in the control group, which performed deep breathing exercises.
Gastric juice acidity in the experimental group was reduced by 3 (0.2), and remained unchanged in the control group.
When performing the modified breathing exercise, the pressure in the colon in the experimental group was reduced by 12 (0.5) mm Hg. In the control group, the pressure change was not observed.
The study showed high efficiency of the modified breathing exercise as a way to reduce the feeling of hunger during abstinence from food. The observed effect may be coupled with a decrease in the intra-abdominal pressure and more rapid movement of the acidic stomach contents into intestines.
It should be noted that the modified breathing exercise is effective only when feeling hungry. If the patient had food before performing it, the effect was minimal or absent. Proposed breathing exercise is somewhat different from its description in the literature.25 Experience has shown that the changes made increase its efficiency by reducing the number of required repetitions from 40 to 60 times per day to 3 to 6 times per day. The authors have observed an association between the suppressed sense of hunger and the conditions of gastric mucosa and oral cavity. The subjects who performed the modified breathing exercise had no fur on the tongue and no bad breath after a few days. Patients with hyperacid gastritis, peptic ulcers, and gastroesophageal reflux disease felt a significant improvement when performing the modified breathing exercise, even without medications. The ability to remove acidic contents of the stomach by means of the modified breathing exercise during breaks between the meals can be utilized for nondrug treatment of the diseases associated with Helicobacter pylori.41
Perhaps some variations in the obtained results are due to the fact that we did not pay special attention to the individual characteristics of the participants, such as eating habits, taste preferences, previous eating regimen, psychological features, and so on and have only focused on identifying commonalities. Future work requires using more subtle and intelligent methods, integrating digestion physiology, neurophysiology of the subcortical center, and eating behavior psychology. The authors would also like to increase the number of participants in such a study.
The fact that excessive consumption of food is not required from the biochemical sense, allows creating medical and educational programs, where moderate and adequate nutrition is the result of rational governance of hunger. This approach is preferable to dietary restrictions, intense exercise, or bariatric surgery. This is especially true for children, adolescents, and the elderly.
Acknowledgments
The authors acknowledge participants’ contributions to this study. Valuable discussions with Dr. Vladimir Marchenko, MD and Dr. Yuriy Marchenko, MD are also greatly appreciated.
Appendix
A Brief Health Assessment Form
In the survey, a standard Short Form–36 (SF-36) health questionnaire was used, by replacing the word “health” with “hunger.”50
Survey
Answer each question by marking the selected answer as indicated. If you are not sure how to answer a question, please choose the answer that best reflects your opinion.
| Question | Points |
|---|---|
| Attention: How hunger influenced your usual work during the day (your work outside your home and your household work)? | |
| Didn’t bother me | 0 |
| Insignificantly | 1 |
| Moderately | 2 |
| Noticeably | 3 |
| Strongly | 4 |
| Unbearably | 5 |
| Comfort: How much time during the day did you feel calm and complacent? | |
| All the time | 0 |
| Most of the time | 1 |
| Significant part of the time | 2 |
| Some time | 3 |
| Insignificant part of the time | 4 |
| Never | 5 |
| Operability: How much time during the day you were full of energy? | |
| All the time | 0 |
| Most of the time | 1 |
| Significant part of the time | 2 |
| Some time | 3 |
| Insignificant part of the time | 4 |
| Never | 5 |
| Mood: How much time during the day you were depressed and sad? | |
| Never | 0 |
| Insignificant part of the time | 1 |
| Some time | 2 |
| Significant part of the time | 3 |
| Most of the time | 4 |
| All the time | 5 |
| Sociability: What part of the time during the day hunger interfered with your usual communication or social life? | |
| Never | 0 |
| Insignificant part of the time | 1 |
| Some time | 2 |
| Significant part of the time | 3 |
| Most of the time | 4 |
| All the time | 5 |
Footnotes
Author Contributions: APV designed and conducted the study reported in the article, and he also wrote majority of the article in Russian. AAV designed the pressure measurement technique, interpreted the data, and translated the article from Russian into English. ZW conducted the literature search and edited the article. EVM analyzed the data and conducted statistical analysis of the data.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Alex A. Volinsky, PhD http://orcid.org/0000-0002-8520-6248
Ethical Approval: The studies were conducted in Kiev, Ukraine in compliance with “The Convention for the Protection of Human Rights and Dignity of the Human Being with regard to the Application of Biology and Medicine” and World Medical Association Declaration of Helsinki “Ethical Principles for Medical Research Involving Human Subjects.”
References
- 1. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report. National Institutes of Health. Obes Res. 1998;6(suppl 2):51S–209S. [PubMed] [Google Scholar]
- 2. Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315:2284–2291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Trust for America’s Health and Robert Wood Johnson Foundation. The State of Obesity project. http://stateofobesity.org/adult-obesity/. Accessed January 16, 2017.
- 4. Allison DB, Fontaine KR, Manson JE, Stevens J, Van Itallie TB. Annual deaths attributable to obesity in the United States. JAMA. 1999;282:1530–1538. [DOI] [PubMed] [Google Scholar]
- 5. Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79:6–16. [DOI] [PubMed] [Google Scholar]
- 6. Nestle M, Jacobson MF. Halting the obesity epidemic: a public health policy approach. Public Health Rep. 2000;115:12–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. James WP. The fundamental drivers of the obesity epidemic. Obes Rev. 2008;9(suppl 1):6–13. [DOI] [PubMed] [Google Scholar]
- 8. Imaz I, Martinez-Cervell C, Garcia-Alvarez EE, Sendra-Gutiérrez JM, González-Enríquez J. Safety and effectiveness of the intragastric balloon for obesity. A meta-analysis. Obes Surg. 2008;18:841–846. [DOI] [PubMed] [Google Scholar]
- 9. Pinel JPJ. Biopsychology. 6th ed Boston, MA: Allyn & Bacon; 2005. [Google Scholar]
- 10. Pinel JPJ, Assanand S, Lehman DR. Hunger, eating, and ill health. Am Psychol. 2000;55:1105–1116. [DOI] [PubMed] [Google Scholar]
- 11. Weinstock M. The facts about obesity. H&HN Daily, June 21, 2013. American Hospital Association. [Google Scholar]
- 12. Malik S, McGlone F, Bedrossian D, Dagher A. Ghrelin modulates brain activity in areas that control appetitive behavior. Cell Metab. 2008;7:400–409. [DOI] [PubMed] [Google Scholar]
- 13. Carlson AJ. Hunger. Sci Mon. 1931;33:77–79. [Google Scholar]
- 14. Booth DA. The physiology of appetite. Br Med Bull. 1981;37:135–140. [DOI] [PubMed] [Google Scholar]
- 15. Ikeda J, Hayes D, Satter E, et al. A commentary on the new obesity guidelines from NIH. J Am Diet Assoc. 1999;99:918–919. [DOI] [PubMed] [Google Scholar]
- 16. Moore KL, Agur AMR. Essential Clinical Anatomy. Hagerstown, MD: Lippincott Williams & Wilkins. [Google Scholar]
- 17. Gastrointestinal surgery for severe obesity: National Institutes of Health Consensus Development Conference Statement. Am J Clin Nutr. 1992;55(2 suppl):615S–619S. [DOI] [PubMed] [Google Scholar]
- 18. Colquitt J, Clegg A, Sidhu M, Royle P, Sidhu MK. Surgery for morbid obesity. Cochrane Database Syst Rev. 2003;2:CD003641 doi:10.1002/14651858.CD003641. [DOI] [PubMed] [Google Scholar]
- 19. Lacey JM, Tershakovec AM, Foster GD. Acupuncture for the treatment of obesity: a review of the evidence. Int J Obes Relat Metab Disord. 2003;27:419–427. [DOI] [PubMed] [Google Scholar]
- 20. Zhao HY. Clinical observation on acupuncture for treatment of central obesity. Zhongguo Zhen Jiu. 2006;26:629–631. [PubMed] [Google Scholar]
- 21. Mi YQ. Clinical study on acupuncture for treatment of 80 cases of simple obesity. Zhongguo Zhen Jiu. 2005;25:95–97. [PubMed] [Google Scholar]
- 22. Tang X. 75 cases of simple obesity treated with auricular and body acupuncture. J Tradit Chin Med. 1997;17:55–56. [PubMed] [Google Scholar]
- 23. Yao H, Chen JX, Zhang ZQ, Pan Y, Zheng J, Tong J. Effect of acupuncture therapy on appetite of obesity patients. Zhen Ci Yan Jiu. 2012;37(6):49. [PubMed] [Google Scholar]
- 24. Zhou S. Qigong for Body-Build and Weight Control. Beijing, China: Tsinghua University Press; 1989. [Google Scholar]
- 25. Chen NN. Breathing Spaces. Qigong, Psychiatry, and Healing in China. New York, NY: Columbia University Press; 2003. [Google Scholar]
- 26. McCarthy TA. Validity of rectal pressure measurements as indication of intra-abdominal pressure. Urology. 1982;20:657–660. [DOI] [PubMed] [Google Scholar]
- 27. Stendal C. Practical Guide to Gastrointestinal Function. Oxford, England: Blackwell Science; 1997. [Google Scholar]
- 28. Tutuian R, Castell DO. Gastroesophageal reflux monitoring: pH and impedance. GI Motility Online. 2006. doi:10.1038/gimo31. [Google Scholar]
- 29. Clark GWB, Jamieson JR, Hinder RA, et al. The relationship of gastric pH and the empting of solid, semisolid and liquid meals. J Gastroinest Motil. 1993;5:273–279. [Google Scholar]
- 30. Kron IL, Harman PK, Nolan SP. The measurement of intra-abdominal pressure as a criterion for abdominal re-exploration. Ann Surg. 1984;199:28–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Iberti TJ, Lieber CE, Benjamin E. Determination of intra-abdominal pressure using a transurethral bladder catheter: clinical validation of the technique. Anesthesiology. 1989;70:47–50. [DOI] [PubMed] [Google Scholar]
- 32. Vegesna AK, Prabhu SP, Sampath AM, et al. Measurement of ileal cecal valve pressures. Gastroenterology. 2011;140:867–868. [Google Scholar]
- 33. Wall LL, Hewitt JK, Helms MJ. Are vaginal and rectal pressures equivalent approximations of one another for the purpose of performing subtracted cystometry? Obstet Gynecol. 1995;85:488–493. [DOI] [PubMed] [Google Scholar]
- 34. Cheatham ML, Safcsak K. Intraabdominal pressure: a revised method for measurement. J Am Coll Surg. 1998;186:594–595. [DOI] [PubMed] [Google Scholar]
- 35. Colon and Rectum, AJCC Cancer Staging Atlas. Chicago, IL: American Joint Committee on Cancer; 2006. [Google Scholar]
- 36. Mayer EA, Naliboff BD, Craig AD. Neuroimaging of the brain-gut axis: from basic understanding to treatment of functional GI disorders. Gastroenterology. 2006;131:1925–1942. [DOI] [PubMed] [Google Scholar]
- 37. Falkovich G. Fluid Mechanics. A Short Course for Physicists. New York, NY: Cambridge University Press; 2011. [Google Scholar]
- 38. Kapoor VK. Large intestine anatomy. Medscape. http://emedicine.medscape.com/article/1948929-overview. Accessed April 11, 2017.
- 39. Vitebsky YD. Basic Valvular Gastroenterology [in Russian]. Chelyabinsk: Yuzh-Ural; 1986. [Google Scholar]
- 40. Kolesnikov LL. Human sphincter system: a new look at the problem [in Russian]. Success Mod Scie. 2006;1:86–87. [Google Scholar]
- 41. Giusti C. Association of Helicobacter pylori with central serous chorioretinopathy: hypotheses regarding pathogenesis. Med Hypotheses. 2004;63:524–527. [DOI] [PubMed] [Google Scholar]
- 42. Vitebsky YD. Valve Anastomoses in Digestive Tract Surgery [in Russian]. Moscow, Russia: Medicine; 1988. [Google Scholar]
- 43. Zajac P, Holbrook A, Super ME, Vogt M. An overview: current clinical guidelines for the evaluation, diagnosis, treatment, and management of dyspepsia. Osteopath Fam Physician. 2013;5:79–85. [Google Scholar]
- 44. Burchard KW, Ciombor DM, McLeod MK, Slothman GJ, Gann DS. Positive end-expiratory pressure with increased intra-abdominal pressure. Surg Gynecol Obstet. 1985;161:313–318. [PubMed] [Google Scholar]
- 45. Lower Gastrointestinal Tract. US National Library of Medicine Medical Subject Headings (MeSH) 2011.
- 46. Raven P, Johnson G, Mason K, Losos J, Singer S. The Capture of Oxygen: Respiration. 8th ed New York, NY: McGraw-Hill. [Google Scholar]
- 47. Patton KT, Thibodeau GA. Anatomy & Physiology. 7th ed St Louis, MO: Mosby; 2009. [Google Scholar]
- 48. Yoga Synergy Blog. http://blog.yogasynergy.com/2010/09/secrets-of-advanced-breath-control-pranayama-with-internal-locks-bandha-energy-control-gestures-mudra-and-internal-cleansing-kriya/. Accessed March 1, 2017.
- 49. Gastrointestinal Tract. US National Library of Medicine Medical Subject Headings (MeSH).
- 50. Ware JE. SF-36® Health Survey update. http://www.sf-36.org/tools/SF36.shtml. Accessed March 1, 2017. [DOI] [PubMed]