Abstract
Complementary and alternative medicine covers a wide variety of therapies and practices, which vary from country to country and region to region. The study was conducted to assess the knowledge, attitude, and practice of complementary and alternative medicine among the residents of Wayu town, Western Ethiopia. A descriptive cross-sectional study was carried out on 302 residents. A systematic sampling was used to select households. Data were entered in SPSS (version 20; IBM Corp) and descriptive statistics was carried out. Of 302 participants, 51.65% have a good knowledge, 78.6% were aware of complementary and alternative medicine, and 74.22% used it in the past 2 years. A total of 23.83% believe that complementary and alternative medicine is more effective than modern medicine and 28.8% preferred complementary and alternative medicine to modern medicine. This study revealed that in Wayu town, there is relatively high public interest in complementary and alternative medicine practices and a significant number has a good knowledge but generally the attitude toward complementary and alternative medicine is relatively low.
Keywords: knowledge, attitude, practice, complementary and alternative medicine, Wayu Town, Western Ethiopia
Complementary and alternative medicine definition is inconclusive and varies in different contexts. However, Ernst et al1 described complementary and alternative medicine as “diagnosis, treatment, and/or prevention which complements mainstream medicine by contributing to a common whole, satisfying a demand not met by orthodoxy, or diversifying the conceptual frameworks of medicine.”
The Cochrane Complementary Medicine Field describes complementary and alternative medicine as “practices and ideas that are defined by their users as preventing or treating illness, or promoting health and wellbeing…and which are outside the domain of conventional medicine in several countries.”2 The National Institutes of Health has defined complementary and alternative medicine as “a group of diverse medical and health care systems, practices, and products that are not presently considered to be part of conventional medicine.”3 As for the difference between “complementary” and “alternative” medicine, the former is used together with conventional medicine, whereas the latter is used in place of it.4
Nearly half of the population in many developed countries regularly use some form of complementary and alternative medicine (the United States 42%, Australia 48%, France 49%, Canada 70%).5,6 A considerable use exists in many developing countries (Colombia 40%, Chile 71%, and up to 80% in Africa counties).7
Data on the current patterns of use and effectiveness of various complementary and alternative medicine treatments being used alone and in combination are inadequate. Complementary and alternative medicine is used by the people for the management of chronic conditions that are costly to society, such as chronic pain and arthritis, and more life-threatening diseases such as heart disease and cancer.7
Complementary and alternative medicine services are often used alongside (and in addition to) conventional medical treatments. Thus, a vast informal and silent health care sector exists in all countries, and no comprehensive picture of this sector exists as yet in any country. Most estimates of complementary and alternative medicine use have not been population based, particularly in Africa and Asian countries, where estimates of use range from very low to very high.8
The World Health Organization estimates the prevalence of use of nutritional supplements and alternative medicines among African countries to range between 20% and 80%.9
Many herbal substances that are used in Ethiopian traditional medicine are also used as ingredients and spices in Ethiopian food. Consumption of these herbs and spices as part of a normal diet is not likely to cause adverse herb-drug interactions because they are consumed in relatively small quantities. However, when these herbs and spices are used for medicinal purposes there may be an increased likelihood of adverse interactions with conventional medicines. There are several classes of medications that are at a higher risk for adverse herb-drug interactions, including antiarrhythmic, antiseizure, antidiabetic, and anticoagulant medication. Health care providers are particularly attuned to these interactions because these drugs are typically monitored with serum levels and serum markers (eg, warfarin, digoxin).10
Although complementary and alternative medicine plays an important role in Ethiopian society, knowledge about the extent and characteristics of complementary and alternative medicine practices is limited and has frequently been ignored in the national health system.11,12
As it is evident that the majority of society in developing countries rely on complementary and alternative medicine for various reasons like accessibility, affordability, and perceived belief of being safe and efficacious than modern medicine.13 However, it is not yet sufficiently investigated that such practices are based on sufficient knowledge on the safety and efficacy of these practices or not. Moreover, there is also limited evidence on scientific bases for safety and efficacy the majority of complementary and alternative medicine practices.14
Despite Western medicine becoming more widespread in Ethiopia, Ethiopians tend to rely more on complementary and alternative medicine. Modern health services remain concentrated in urban areas and have failed to keep pace with the growing population, keeping health care access out of reach for most Ethiopians living in rural Ethiopia.11 In Ethiopia, little has been done in recent decades to enhance and develop the beneficial aspects of complementary and alternative medicine, including relevant research to explore possibilities for its gradual integration into modern medicine.15
Furthermore, there has been little investigation on knowledge, attitude, and practice of different complementary and alternative medicine practices particularly in rural societies of the country and as far as the knowledge of the investigators is concerned, there was no such study conducted in the study area. Thus, based on the above insight, this study was focused mainly on identifying the knowledge, attitude, and practice of complementary and alternative medicine through community based cross-sectional study in Wayu town, Western Ethiopia.
Methods
Study Area and Period
The study was conducted in Wayu town, which is the capital of Jimma Rare District, in Horu Guduru Wellega Zone of Oromia regional state, which is situated in Western Ethiopia. The town is about 230 km west of Addis Ababa, the capital of Ethiopia and 90 km away from Shambu town, which is the capital of Horu Guduru Wollega Zone. Its climatic condition is “Woina Dega.” Currently, it has a total population of 5415 people of which 2479 (45.77%) are males and 2936 (54.23%) females. There are about 4 private clinics and 1 public health center in the town. The study was conducted from February 15 to April, 30, 2016.
Study Design
A community based descriptive cross-sectional study design was used to assess knowledge, attitude, and practice of the community toward complementary and alternative medicine.
Source Population
All the households in Wayu town were the source population of the study.
Study Population
The study population included individuals aged older than 18 years and living for at least 6 months in the town.
Sample Size Determination and Sampling Technique
The sample size for this study was determined using single population proportion formula: assuming, 95% confidence interval and 5% margin of error and a prevalence of 50% to get possible minimum large sample size. So, total of 384 was calculated and since the number of population was less than 10 000, the correction formula was used and by adding 5% for nonresponse rate, the final sample size became 302 study participants.
To identify the study participants, a systematic sampling technique was used. The town was divided into 4 villages and a sample from each village was taken proportionally based on total number of households in each village.
Sampling interval was determined by dividing the total number of households in each village by sample size corresponding to that village which gives the interval k = 5 and selecting the first study unit from each village by using “lottery” method. For households with 2 or more adults, only 1 individual was selected by lottery method.
Data Collection Tools and Procedures
A structured questionnaire was used as data collection tool. The questionnaire was developed after reviewing relevant literatures and then the questionnaire is translated to Afaan Oromo language. The questionnaire contains 4 sections mainly for collecting data on socio demographic, knowledge, attitude, and practice of study subjects. Data were collected by interviewing the individuals, using the questionnaires by trained health workers. Daily close supervision at the end of every data collection was made; the questionnaire was reviewed and checked for completeness, accuracy and consistency by supervisors and investigators and timely corrective measures have been taken.
Data Processing and Analysis
After checking for completeness and consistency, data were entered in SPSS (version 20; IBM Corp) and descriptive statistics was carried out. Data were presented using narratives, tables, and figure.
Results
Sociodemographic Characteristics of Respondents
A total of 302 respondents were interviewed with 100% response rate. Among them 172 (56.95%) were female and 130 (43.05%) were male. The age range of respondents was 18 to 75 years, with mean age of 46 years and nearly half of the respondents, 143 (47.4%), were in the age range of 29 to 40 years. Large number of respondents, 116 (38.41%), have attended primary school while 87 (28.81%) respondents attended secondary school and more than a quarter (n = 88) of the respondents were illiterate. A total of 161 (53.31%) of the respondents were married. More than half 160(52.98%) of people earn more than 500 ETB per month. The majority of the population of the town were Protestant 140 (46.36%) and Oromo constituted the highest ethnic group, 298 (98.68%), followed by Amhara, 4 (1.32%) (Table 1).
Table 1.
Sociodemographic Characteristics of Respondents in Wayu Town.
| Variable | Frequency | Percentage |
|---|---|---|
| Sex | ||
| Male | 130 | 43.05 |
| Female | 172 | 56.95 |
| Age (years) | ||
| 18-28 | 84 | 27.81 |
| 29-40 | 143 | 47.35 |
| 41-59 | 51 | 16.89 |
| ≥60 | 24 | 7.95 |
| Occupation | ||
| Merchant | 70 | 23.18 |
| Government employee | 59 | 19.54 |
| Student | 45 | 14.90 |
| Self-employed | 27 | 8.94 |
| Unemployed | 21 | 6.95 |
| Housewife | 57 | 18.87 |
| Others | 23 | 7.62 |
| Ethnicity | ||
| Oromo | 298 | 98.68 |
| Amhara | 4 | 1.32 |
| Monthly income (ETB) | ||
| <500 | 16 | 5.30 |
| 500-1500 | 160 | 52.98 |
| 1500-2500 | 94 | 31.13 |
| >2500 | 32 | 10.59 |
| Marital status | ||
| Married | 161 | 53.31 |
| Single | 114 | 37.75 |
| Divorced | 8 | 2.65 |
| Widowed | 19 | 6.29 |
| Education | ||
| Illiterate | 88 | 29.14 |
| Primary school | 116 | 38.41 |
| Secondary school | 87 | 28.81 |
| Higher education | 11 | 3.64 |
| Religion | ||
| Protestant | 140 | 46.36 |
| Orthodox | 116 | 38.41 |
| Muslim | 35 | 11.59 |
| Others | 11 | 3.64 |
Knowledge of Respondents Toward Complementary and Alternative Medicine
Majority, 237 (78.6%), of the respondents know alternative treatment options apart from modern medicine. The type of complementary and alternative medicine known to the respondents were medicinal herbs (168, 55.7%), spiritual or faith healing (57, 18.8%), traditional bone setting (41, 13.7%), massage (21, 7%), and other products (15, 4.8%).
Almost all of them had promotional information on complementary and alternative medicine practice only from informal sources like family member and friends (298, 98.6%).
More than half of the respondents, 184 (60.79%), were aware of the major side effects of complementary and alternative medicine, such as diarrhea (111, 36.64%), vomiting (62, 20.5%), abdominal pain (45, 14.91%), and the remaining (84, 27.95%) were not aware of the side effects of complementary and alternative medicine (Table 2).
Table 2.
Knowledge of Respondents in Wayu Town.
| Variables | Attributes | Number | Percentage |
|---|---|---|---|
| Know treatments apart from modern medicine | Yes | 237 | 78.6 |
| No | 65 | 21.4 | |
| Forms of therapy respondents know | Medical herbalism | 168 | 55.7 |
| Spiritual/faith healing | 57 | 18.8 | |
| Traditional bone setting | 41 | 13.7 | |
| Massage | 21 | 7 | |
| Others | 15 | 4.8 | |
| Had promotional information on complementary and alternative medicine | Yes | 237 | 78.6 |
| No | 65 | 21.4 | |
| Source of information | Formal | 4 | 1.4 |
| Informal | 298 | 98.6 | |
| Know harmful effects of complementary and alternative medicine | Yes | 183 | 60.7 |
| No | 119 | 39.3 | |
| Reported harmful effects | Diarrhea | 111 | 36.64 |
| Vomiting | 62 | 20.5 | |
| Abdominal pain | 45 | 14.91 | |
| Not known | 84 | 27.95 |
According to this study, respondents reported different kinds of diseases that can be treated by complementary and alternative medicine. Nearly half of the respondents, 148 (49.15%), replied that hemorrhoids are treated by complementary and alternative medicine. Rabies (72, 23.75%), jaundice (51, 16.95%), and bone fracture (31, 10.15%) were other diseases reported to be treated by complementary and alternative medicine.
On the other hand, participants responded that complementary and alternative medicine fails to treat diseases like cancer (179, 59.3%), malaria (65, 21.5%), tuberculosis (30, 9.9%), and others (28, 9.3%) (Table 3).
Table 3.
Diseases Reported to Be Treated by Complementary and Alternative Medicine Rather Than Modern Medicine in Wayu Town.
| Variables | Frequency | Percentage |
|---|---|---|
| Disease treated by complementary and alternative medicine | ||
| Hemorrhoids | 148 | 49.0 |
| Rabies | 72 | 23.8 |
| Jaundice | 51 | 16.9 |
| Bone fracture | 31 | 10.3 |
| Diseases complementary and alternative medicine fail to treat | ||
| Cancer | 179 | 59.3 |
| Malaria | 65 | 21.5 |
| Tuberculosis | 30 | 9.9 |
| Others | 28 | 9.3 |
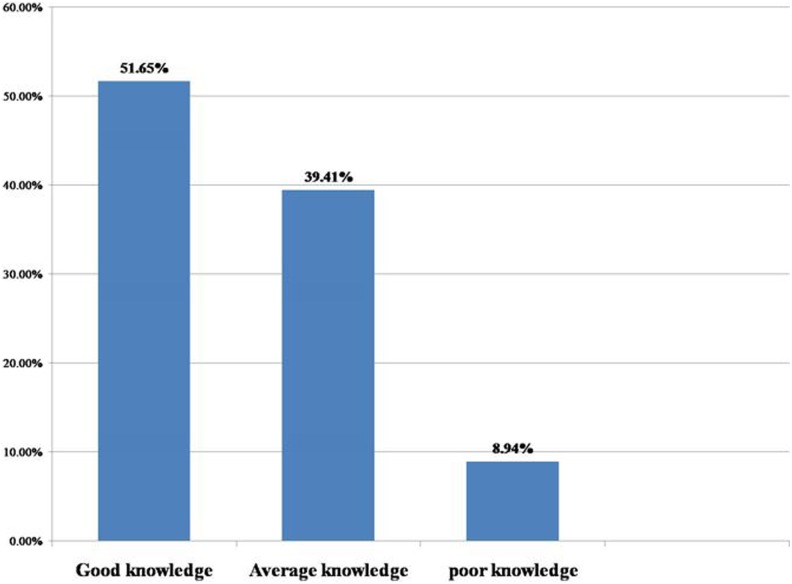
As indicated in Figure 1, a total of 156 (51.65%) of the study participants were found to have good knowledge about complementary and alternative medicine, 119 (39.41%) had average knowledge, and 27(8.94%) had poor knowledge level.
Figure 1.
Level of knowledge of respondents about complementary and alternative medicine in Wayu Town.
Attitude of Respondents to Complementary and Alternative Medicine Therapy
Regarding the effectiveness of the complementary and alternative medicine, 222 (73.5%) participants disagreed or strongly disagreed that complementary and alternative medicine is more effective than modern medicine. A majority, 236 (78.2%), of the respondents replied their disagreement that complementary and alternative medicine is safer than modern medicine. More than half, 174 (57.62%), of the respondents agreed that complementary and alternative medicine should be integrated to modern medicine. Most of the respondents disagreed (133, 44%) and strongly disagreed (82, 27.2%) about their first preference of visiting complementary and alternative medicine practitioners than modern medicine practitioners. Only 60 (19.8%) of participants recommend visiting complementary and alternative medicine practitioners first than modern medicine. A total of 191(63.4%) of the study population agreed that complementary and alternative medicine is cheaper than modern medicine (Table 4).
Table 4.
Attitude of the Respondents Toward Complementary and Alternative Medicine in Wayu Town.
| Variable | Response | |||||
|---|---|---|---|---|---|---|
| Strongly Disagree (1) | Disagree (2) | Not Known (3) | Agree (4) | Strongly Agree (5) | ||
| 1. Complementary and alternative medicine is more effective than modern medicine | Frequency | 87 | 135 | 8 | 55 | 17 |
| Percentage | 28.8 | 44.7 | 2.7 | 18.2 | 5.6 | |
| 2. Complementary and alternative medicine is more safe than modern medicine | Frequency | 172 | 64 | 3 | 23 | 40 |
| Percentage | 57 | 21.2 | 1 | 7.6 | 13.2 | |
| 3. Complementary and alternative medicine should be integrated to modern medicine | Frequency | 45 | 65 | 7 | 174 | 11 |
| Percentage | 14.9 | 21.52 | 2.32 | 57.62 | 3.64 | |
| 4. Prefer first to visit complementary and alternative medicine practitioner than modern medicine | Frequency | 82 | 133 | 0 | 63 | 24 |
| Percentage | 27.2 | 44 | 0 | 21 | 7.8 | |
| 5. Recommend a sick person first to visit complementary and alternative medicine practitioner | Frequency | 91 | 142 | 9 | 45 | 15 |
| Percentage | 30.2 | 47 | 3 | 14.9 | 4.9 | |
| 6. Complementary and alternative medicine is more affordable than modern medicine | Frequency | 21 | 57 | 33 | 97 | 94 |
| Percentage | 6.9 | 18.8 | 10.9 | 32.1 | 31.3 | |
Practice Related to Complementary and Alternative Medicine
Majority of respondents (74.22%) had practiced complementary and alternative medicine at least in the past 2 years and the remaining 25.78% did not practice complementary and alternative medicine. Only 22 (5.6%) respondents had history of concurrent use of modern medicines along with complementary and alternative medicine.
Complementary and alternative medicine was most commonly given to the elderly (32.62%), adults (24.11%), children (17.02%), pregnant women (2.13%), and the remaining 24.11% did not know for whom complementary and alternative medicine was most commonly given (Table 5).
Table 5.
Practice of Complementary and Alternative medicine of Respondents in Wayu Town.
| Variable | Attributes | Frequency | Percentage |
|---|---|---|---|
| Used complementary and alternative medicine in the past 2 years | Yes | 224 | 74.22 |
| No | 78 | 25.78 | |
| Mostly complementary and alternative medicine is given for | Elderly | 99 | 32.62 |
| Adult | 73 | 24.11 | |
| Children | 51 | 17.02 | |
| Pregnant women | 64 | 2.13 | |
| Combine complementary and alternative medicine and modern medicine in their lifetime | Yes | 17 | 5.6 |
| No | 285 | 94.4 |
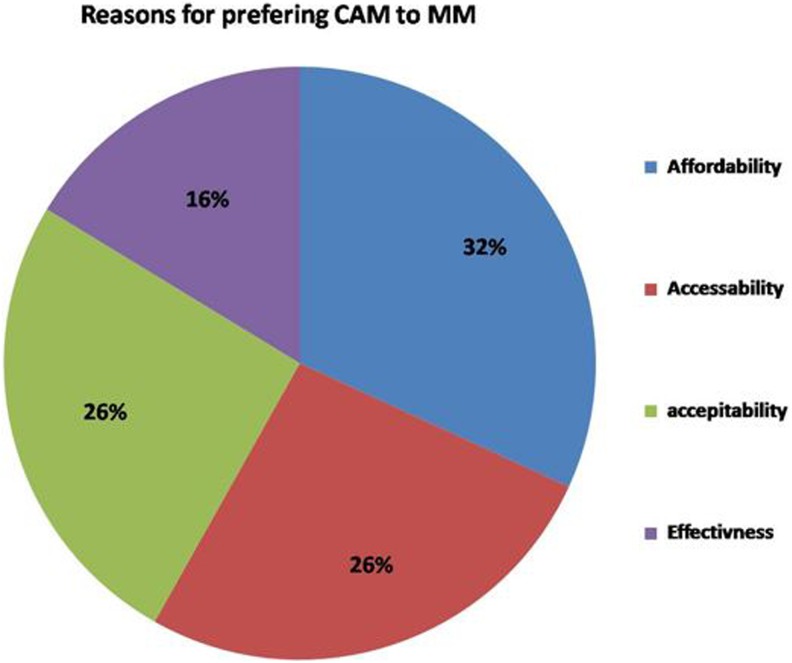
Figure 2 shows the reasons of the respondents who prefer complementary and alternative medicine to modern medicine.
Figure 2.
Reasons to Prefer complementary and alternative medicine to modern medicine among respondents of Wayu Town.
In this study, identified types of complementary and alternative medicine include the following medicinal herbs (70.57%), bone setting (16%), animal or mineral product (11.43%), and spiritual faith healing (2%). Most of the species (50%) were harvested for their leaves to prepare remedies.
Remedies were reported to be administered through oral (53.85%), dermal or topical (36.54%), buccal (3.85%), and anal (5.77%), which are shown in Table 6.
Table 6.
Percentage Distribution of Part of Herbal Medicines and Route of Administration According to the Respondents of Wayu Town.
| Variable | Attributes | Number | Percentage |
|---|---|---|---|
| Part of herbal medicine commonly used | Leaves | 151 | 50 |
| Roots | 64 | 21.15 | |
| Seed | 41 | 13.46 | |
| Others (fruit, bark, flower) | 46 | 15.39 | |
| Common route of administration | Oral | 162 | 53.64 |
| Dermal/topical | 110 | 36.42 | |
| Buccal | 13 | 4.31 | |
| Anal | 17 | 5.63 |
Discussion
This community-based cross-sectional study has investigated the knowledge, attitude, and practice of complementary and alternative medicine among the residents of Wayu town, Horu Goduru Wollega Zone, West Ethiopia.
Accordingly, 78.6% of the respondents were aware of an alternative way of getting treatment for their ailments apart from modern medicine. This finding is lower than the finding of the study conducted in Nigeria where 90.4% of the respondents aware of alternative way of getting treatment.16 The major source of information regarding complementary and alternative medicine were through: Informal sources (friends, family) 98.6%, which was higher than the finding of the study done in Arsi Zone, Ethiopia where informal source was 56.2% of cases.13 This might be due to lack of documentation or written standards and information concerning complementary and alternative medicine as it was transmitted orally from generation to generation.
This study indicated that 51.65% of the respondents has a good knowledge about complementary and alternative medicine. This finding is lower than the finding of the study carried out in Merawi District, Northwest Ethiopia where 61.5% of the population has a good knowledge. But it is higher than the finding of the study conducted in Lagos, Nigeria where only 44.7% of the population has a good knowledge.17,18 This might be because of the time gap between our study and the study conducted in Lagos, Nigeria, as awareness of the community may have improved through time.
In this study, the percentage of respondents who practiced complementary and alternative medicine in the past 2 years was 74.22%, which is slightly lower than the finding reported by the World Health Organization, where 80% Ethiopian people practice or use complementary and alternative medicine.16 This might be because the World Health Organization study shows the average finding for Ethiopians whereas our study was only limited to one town.
This study revealed that about 60.7% of the respondents were aware of the side effects of complementary and alternative medicine, which is slightly higher than the finding of the study conducted in Nigeria where 54.9% of the respondents were aware of side effects and in this study the side effects include diarrhea (36.67%), vomiting (20.5%), and abdominal pain (14.91%) whereas in Nigerian study larger proportion of study participants know the side effects; diarrhea 69.7%, vomiting 40.2%, and abdominal pain 42% [14].
In this study, only 23.83% of all the respondents who were aware of alternative medical therapies believed that complementary and alternative medicine is more effective than modern medicine. This is lower than the finding of the study conducted in Nigeria, where about 42% of all respondents believed in complementary and alternative medicine.16 The respondents’ fear of complementary and alternative medicine might be due to its side effects.
This study indicated that about 28.8% of the respondents preferred complementary and alternative medicine to modern medicine. This is slightly lower than the finding of the study carried out in Fiche, Ethiopia where 35.7% prefer complementary and alternative medicine.11 The reason for nonpreference in this study might be the absence of formal communication regarding complementary and alternative medicine.
In this study, hemorrhoids (49%) and rabies (23.8%) were among common illness better treated by complementary and alternative medicine than modern medicine, whereas cancer (59.4%) and malaria (21.6%) are among the ailments complementary and alternative medicine fail to treat. This is inconsistent with the finding of the study carried out in Addis Ababa where the most common ailment reported to be treated by traditional medicine was “Wef beshita” (jaundice).15 This might be attributable to the fact that sociodemographic deference of populations in the 2 study settings.
In the current study, parts of herbal medicine commonly used are leaves in (50%) of cases and the roots takes the second proportion 21.15%. This is consistent with the finding of ethnobotanical research carried out in another part of the country, which reported leaves (64.52%) followed by roots (19.35%), to be mostly used in the treatment of various health problems.14
This study revealed that oral (53.64%) and topical (dermal) (36.42%) were the major routes of administration of herbal remedies. This finding is similar with finding of the study conducted in Gindeberet district, West Ethiopia where oral route and topical application were the 2 commonest routes of administration.14
Conclusion
This study revealed that there is relatively high prevalence and high public interest in complementary and alternative medicine practices in Wayu town. A fair number of respondents in the town has a good knowledge but generally the attitude of respondents toward complementary and alternative medicine is relatively low.
Acknowledgments
The authors’ sincere thanks go to Ambo University for provision of the opportunity to conduct the research. They also like to express their deepest gratitude for Jimma Rare Woreda health office staffs for their cooperation in providing basic information. Finally, their thanks go to data collectors and all research participants who took part in the study.
Footnotes
Author Contributions: NB, TT, and AAG conceived and designed the study. AAG and TT analyzed the data. NB and TT wrote the first draft of the manuscript. AAG contributed to the writing of the manuscript. NB, TT, and AAG agree with manuscript results and conclusions. NB, TT, and AAG jointly developed the structure and arguments for the article. AAG made critical revisions and approved the final version. All authors reviewed and approved the final manuscript.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Ethical clearance was obtained from the ethical review committee of College of Medicine and Health Sciences, Ambo University. A formal letter was given to Wayu town administrative bureau. In addition, informed consent was obtained from study participants to confirm willingness for participation after explaining the objective of the study. And the respondents were notified that they have the right to refuse or terminate at any point of the interview.
ORCID iD: Addisu Alemayehu Gube http://orcid.org/0000-0002-8389-9554
References
- 1. Ernst E, Resch KL, Mills S, et al. Complementary medicine—a definition. Br J Gen Pract. 1995;45:506–512.7546880 [Google Scholar]
- 2. The Cochrane Library Website. Product Descriptions: http://www3.interscience.wiley.com/cgibin/mrwhome/106568753/ProductDescriptions.html . Accessed April 21, 2016.
- 3. National Care for Complementary and Integrative Health. The use of complementary and alternative medicine in the United States. http://nccam.nih.gov/news/camstats/2007/camsurvey_fs1.htm. Accessed on April 15, 2016.
- 4. Federation of State Medical Boards. Model guidelines for the use of complementary and alternative medicine in medical practice. https://www.fsmb.org/Media/Default/PDF/FSMB/Advocacy/2002_grpol_Complementary_Alternative_Therapies.pdf. Accessed November 20, 2017.
- 5. Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990-1997: results of a follow-up national survey. JAMA. 1998;280:1569–1575. [DOI] [PubMed] [Google Scholar]
- 6. MacLennan AH, Wilson DH, Taylor AW. Prevalence and cost of alternative medicine in Australia. Lancet. 1996;347:569–573. [DOI] [PubMed] [Google Scholar]
- 7. Bannerman RH, Burton J, Wen-Chieh C. Traditional Medicine and Health Care Coverage. Geneva, Switzerland: World Health Organization; 1993. [Google Scholar]
- 8. World Health Organization. Benchmarks for Training in Ayurveda: Benchmarks for Training in Traditional /Complementary and Alternative Medicine. Geneva, Switzerland: World Health Organization; 2010. [Google Scholar]
- 9. World Health Organization. Legal status of traditional medicine and complementary/alternative medicine: a worldwide review. http://apps.who.int/medicinedocs/pdf/h2943e/h2943e.pdf. Published 2001. Accessed February 12, 2016.
- 10. Sadik EA, Gobena T, Mengistu B. Aspects of common traditional medical practices applied for under-five children in Ethiopia, Oromia Region, Eastern-Harargie District, Dadar Woreda, 2011 G. C. J Community Med Health Educ. 2013;3:237. [Google Scholar]
- 11. D’Avigdor E, Wohlmuth H, Asfaw Z, Awas T. The current status of knowledge of herbal medicine and medicinal plants in Fiche, Ethiopia. J Ethnobiol Ethnomed. 2014;10:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Deribe K, Kassaye D, Amberbir A, Getachew B. A historical overview of traditional medicine practices and policy in Ethiopia. Ethiop J Health Dev. 2006;20:127–134. [Google Scholar]
- 13. Elolemy AT, AlBedah AMN. Public knowledge, attitude and practice of complementary and alternative medicine in Riyadh Region, Saudi Arabia. Oman Med J. 2012;27:20–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yirga G, Zeraburk S. Ethno botanical study of traditional medicinal plants in Gindeberet district, west Ethiopia. IJREISS. 2012;1:15–26. [Google Scholar]
- 15. Pankhurst R. Historical Examination of traditional Ethiopian Medicine and Surgery in an Introduction to Health and Health Education in Ethiopia. Addis Ababa, Ethiopia: Berhanena Selam Printing Press; 2007:30. [Google Scholar]
- 16. Gall A, Shenkute Z. Ethiopian traditional and herbal medications and their interaction with conventional drugs. https://ethnomed.org/clinical/pharmacy/ethiopian-herb-drug-interactions. Published November 3, 2009. Accessed April 23, 2016.
- 17. Samuel MW, Leul LA, Belaynew WT, Laychiluh BM. Knowledge, attitude, and utilization of traditional medicine among the communities of Merawi Town, Northwest Ethiopia: a cross-sectional study. Evid Based Complement Alternat Med. 2015;2015:138073 doi:10.1155/2015/138073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Agbaje EO, Babatunde EO. A KAP study of the attitude and practice of traditional medicine in a contemporary Nigerian community. Cent Afr J Med. 2005;51:58–62. [PubMed] [Google Scholar]