Abstract
Panniculitis is a rare clinical finding in dermatomyositis, with less than 30 cases reported and there is only one case associated with the amyopathic subtype described in the literature. The present report describes a 49-year-old female patient that one year after being diagnosed with amyopathic dermatomyositis, presented indurated, painful, erythematous to violaceous nodules located on the upper limbs, thighs and gluteal region. Skin biopsy revealed lobular panniculitis with a lymphocytic infiltrate. The patient was treated with prednisone and methotrexate, but remained unresponsive to treatment.
Keywords: Dermatomyositis, Inflammation, Panniculitis
INTRODUCTION
Dermatomyositis is an autoimmune, chronic, idiopathic, inflammatory disease that affects the striated skeletal muscles, the skin and other organs.1 Clinical features of the disease vary greatly and have been classified into five groups: amyopathic dermatomyositis, juvenile dermatomyositis, primary dermatomyositis, dermatomyositis associated with neoplasms and dermatomyositis associated with other connective tissue disorders.1 Amyopathic dermatomyositis constitutes 2-18% of patients with dermatomyositis and is characterized by pathognomonic cutaneous lesions of dermatomyositis, histopathology compatible with the disease and no evidence of muscle disease.2,3 Panniculitis is a rare skin manifestation of dermatomyositis and less than 30 cases of such association have been published since 1924, of which only one reported such association with the amyopathic subtype.4 We present a case of a 49-year-old patient that one year after being diagnosed with amyopathic dermatomyositis showed a clinical condition compatible with lobular panniculitis.
CASE REPORT
We attended a 49-year-old female patient with erythematous papules on metacarpophalangeal joints and violaceous erythema on the face, cervical region, upper back and upper limbs (Figures 1-3). The patient also showed progressive dyspnea, but did not show muscle weakness. Laboratory tests showed normal values of creatine phosphokinase, aldolase, SGOT, SGPT, anti-Ro, anti-La, anti-Jo1, anti-RNP, rheumatoid factor, and a positiveantinuclear factor (ANA) 1:640 with a speckled pattern. Computed tomography of the chest revealed ground glass attenuation involving one third of the middle portion of both lungs. Skin biopsy of the back of the hand and elbow identified a chronic interface dermatitis with amorphous material on dermal papilla suggesting mucin, favoring the diagnosis of dermatomyositis. Screening for neoplasm was negative.
Figure 1.

Heliotrope rash
Figure 3.

Shawl sign
The patient was treated with methylprednisolone pulse-therapy and discharged with prednisone at 0.5mg/kg/day given her respiratory condition had improved. However, after one month, the patient showed respiratory and cutaneous impairment and treatment with pulse cyclophosphamide combined with the maintenance of corticosteroid was started. The patient's pulmonary condition improved during treatment, but she showed repeated urinary infections. Therefore, cyclophosphamide was discontinued and hydroxychloroquine was introduced. Two months later, the patient was also given azathioprine due to a deterioration of her pulmonary condition and cutaneous lesions.
One year after the patient's first symptoms, indurated, painful, violaceous, erythematous, subcutaneous nodules appeared on the upper limbs, thighs, back, breasts, gluteal region and abdomen (Figure 4). Skin biopsy of the left inner thigh revealed lymphocytic panniculitis with plasma cells of a lobular pattern and vasculopathy (vascular endothelial hyperplasia and edema) (Figure 5). After the onset of panniculitis, we increased the dosage of prednisone and introduced chlorambucil, which was suspended two months later given the deterioration of the inflammatory condition. Thus, we decided for a new pulse of methylprednisolone and maintained the doses of prednisone. One month later, an increase of the panniculitis lesions was noticed and the patient began treatment with methotrexate for five months. From then on, despite the presence of active lesions, the patient suspended the drug on her own. . The patient was once again treated with chlorambucil combined with prednisone 1mg/kg/day. One year after the onset of panniculitis, her skin manifestations remained unresponsive to treatment, but she continued showing no sign of muscle disease.
Figure 4.

Painful and indurated, erythematoviolaceous subcutaneous nodules on the abdomen
Figure 5.
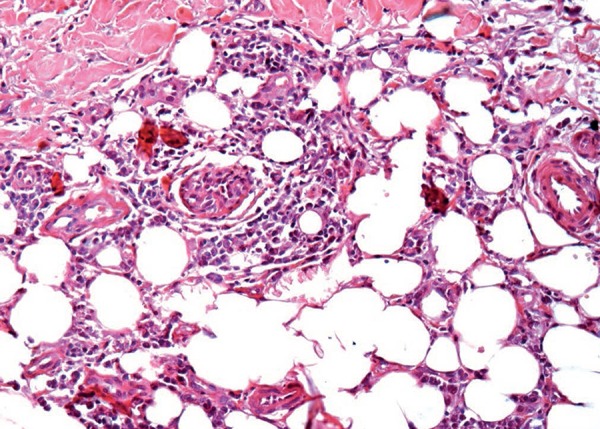
Inflammatory lymphocytic infiltrate in the hypodermis, permeating adipose cells without septal thickening (Hematoxylin & eosin, X400)
DISCUSSION
Panniculitis is an inflammation of the subcutaneous adipose tissue characterized by indurated, painful, erythematous, subcutaneous nodules commonly located on the upper and lower limbs.5 It may be associated with infections, ischemia, trauma, cold, systemic lupus erythematosus, rheumatoid arthritis, and Sjogren's syndrome among others.6 However, its association with dermatomyositis is rare and only about 25 cases have reported such association since it was first described by Weber and Gray in 1924.7 Nonetheless, only one case reported panniculitis related to the amyopathic subtype, which constitutes 2-18% of patients with dermatomyositis.3,8
The clinical manifestations of panniculitis may precede other symptoms of dermatomyositis, appear simultaneously with the disease or during the first five years of the disease.8 In cases where skin lesions occur coupled with muscle disease, panniculitis and dermatomyositis follow a parallel clinical course, with both conditions improving simultaneously during treatment. Thus, muscle disease should be investigated if the subcutaneous inflammation deteriorates.9 However, in this case report, muscle enzyme levels and electroneuromyography showed normal results during the course of two years of the disease.
Histology findings usually reveal lobular panniculitis with lymphoplasmocytic infiltrate that leads to necrosis of fatty tissue and fibrosis. Moreover, calcified areas, vasculitis and endothelial edema may also be observed. Studies have shown that a wide range of subcutaneous inflammation can occur in dermatomyositis, and microscopic alterations of the adipose tissue are more common than clinical manifestations.5,10
The presence of panniculitis in a patient with dermatomyositis may be indicative of a good prognosis as it responds better to treatment and is rarely associated with underlying neoplasms. Of the 25 cases published, only in five solid neoplasms were detected in patients with dermatomyositis manifesting panniculitis.8 In the present case, screening for malignancy was negative.
The treatment of choice consists of corticosteroids, which in most cases results in a fast and complete recovery. Methotrexate and intravenous immunoglobulin may be used in patients who fail to respond to corticosteroids4,8 Chao et al. reported a case of a patient with dermatomyositis and panniculitis in which the lesions improved after treatment with methotrexate, however, the patient still felt ill and intravenous immunoglobulin was necessary.10 Even though treating panniculitis with corticosteroids will usually result in a good clinical response, our patient's condition did not improve and multiple, painful subcutaneous nodules were still observed after treatment with prednisone (1mg/kg/day) and methotrexate.
Although the association of dermatomyositis and panniculitis is rare, one must consider dermatomyositis in patients with lobular panniculitis, even if there is no evidence of muscle disease. In fact, such association may be indicative of a good prognosis.
Figure 2.

Gottron's papules observed on the hands
Footnotes
Work preformed at the Faculdade de Medicina de Jundiaí (FMJ) - Jundiaí (SP), Brasil.
Financial support: none.
Conflict of interest: none.
REFERENCES
- 1.Cegatto LMO, Manoel V. Dermatomiosite. An Bras Dermatol. 2008;83:247–259. [Google Scholar]
- 2.Euwer RL, Sontheimer RD. Amyopathic dermatomyositis (dermatomyositis siné myositis). Presentation of six new cases and review of the literature. J Am Acad Dermatol. 1991;24:959–966. [PubMed] [Google Scholar]
- 3.Arnson Y, Dovrish Z, Hadari R, Amital H. Amyopathic dermatomyositis - An uncommon presentation of dermatomyositis. Isr Med Assoc J. 2007;9:492–493. [PubMed] [Google Scholar]
- 4.Rodríguez-Vázqueza M, Romero-Aguileraa G, García-Arpaa M, Martín-Dávilab F, Calle PC de la. Paniculitis asociada a dermatomiositis amiopática. Actas Dermosifiliogr. 2004;95:189–192. [Google Scholar]
- 5.Arias M, Hernández MI, Cunha LG, Kien MC, Abeldaño A. Panniculitis in a patient with dermatomyositis. An Bras Dermatol. 2011;86:146–148. doi: 10.1590/s0365-05962011000100023. [DOI] [PubMed] [Google Scholar]
- 6.Lin J, Chu C-Y, Lin R-Y. Panniculitis in Adult Onset Dermatomyositis. Report of Two Cases and Review of the Literature. Dermatol Sin. 2006;24:194–200. [Google Scholar]
- 7.Weber F, Gray A. Chronic relapsing polydermatomyositis with predominant involvement of subcutaneous fat. Br J Dermatol. 1924;36:544–560. [Google Scholar]
- 8.Chairatchaneeboon M, Kulthanan K, Manapajon A. Calcific panniculitis and nasopharyngeal cancer-associated adult-onset dermatomyositis: a case report and literature review. Springerplus. 2015;4:201–201. doi: 10.1186/s40064-015-0994-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Douvoyiannis M, Litman N, Dulau A, Ilowite NT. Panniculitis, infection, and dermatomyositis: Case and literature review. Clin Rheumatol. 2009;28:S57–S63. doi: 10.1007/s10067-009-1160-9. [DOI] [PubMed] [Google Scholar]
- 10.Chao YY, Yang LJ. Dermatomyositis presenting as panniculitis. Int J Dermatol. 2000;39:141–144. doi: 10.1046/j.1365-4362.2000.00870.x. [DOI] [PubMed] [Google Scholar]


