Abstract
Background
Behavioral interventions for weight loss have been less effective in lower income and black women. These poorer outcomes may in part be related to these women having more frequent exposures to social and physical situations that are obesogenic, i.e., eating and sedentary cues or situations.
Objectives
Working with obese, lower income black and white women, Addressing People and Place Microenvironments (APP-Me) was designed to create awareness of self-behavior at times and places of frequent eating and sedentary behavior.
Design
APP-Me is being evaluated in a randomized controlled trial with 240 participants recruited from federally qualified health centers located in a single Midwestern city. All participants complete four weeks of ecological momentary assessments (EMA) of situations and behavior. At the end of the four weeks, participants are randomized to enhanced usual care (UC) or UC plus APP-Me.
Methods
APP-Me is an automated short messaging system (SMS). Messages are text, image, audio, or a combination, and are delivered to participants’ mobile devices with the intent of creating awareness at the times and places of frequent eating or sedentary behavior.
Summary
This project aims to create and test timely awareness messages in a subpopulation that has not responded well to traditional behavioral interventions for weight loss. Novel aspects of the study include the involvement of a low income population, the use of data on time and place of obesogenic behavior, and message delivery time tailored to an individual’s behavioral patterns.
Keywords: Randomized controlled trial, weight loss, mobile health, health disparities, user-centered design
Introduction
Obesity rates are high among middle-aged adults generally and among poorer and minority adults particularly. Adults living in poverty, for example, have rates that are 50% higher than adults not living in poverty. (1) Racial disparities also exist, where 59% of black women have a body-mass index (BMI) of 30 or greater (indicating obesity) while only 36% of white middle-aged women have an obese BMI. (2)
Notably, the National Academy of Medicine (formerly the IOM) identified obesity in the urban poor as high priority research. (3) For middle-aged black women, four of five leading causes of death are obesity-related.(4) The concluding article in an October 2014 Obesity Reviews Special Issue on Achieving Healthy Weight in Black American Communities reports that studies of obesity prevention and treatment in black adults are few and insufficient. The authors recommend exploration of electronic health approaches.(5)
Weight loss trials have generally had low representation of adults living in poverty.(6) And while black adults have been represented in large weight loss trials such as the Diabetes Prevention Program (DPP) and Look Ahead,(7) black women in these trials have consistently lost less weight compared to white women.(8–13) Reasons for this are unclear but qualitative studies point to frequent exposure to obesogenic situations for black women.(5, 14) Regardless, weight loss disparities translate into significant disparities in health and longevity—a relatively modest weight loss of 2kg has been shown to meaningfully reduce one’s risk of hypertension and diabetes.(15)(16)
Several recent studies have tested short message service (SMS) “text” messaging as an approach to monitoring and supporting behaviors conducive to weight loss. (17–21) The theoretical frameworks guiding these studies are social cognitive and self-regulation theories, and transtheoretical model. These studies sent messages from the study staff or machine. The frequency of text messaging ranged from two per week to six times a day. Only one study attempted to send text messages that were coordinated with a participant’s reported daily schedule. (20)
Weight loss success was variable across the studies. However, consistently across all of the studies, participants who interacted most with messaging had greater weight loss. Furthermore, only one study enrolled low-income or black women. (20) Attrition was well over 50% at 6 months in this trial, but among those who did not attrit, weight loss was 3.7 kilograms for those receiving supportive texts versus those in standard care.
Our project first measures and compares obesogenic behavior and situations to which black and white middle-aged women are exposed and, second, tests whether timely messaging via a smartphone application can offset some of the influence of these situations. The black and white women in the proposed study live in the same neighborhoods of a single urban county and seek care in the same safety-net health system. This health system operates a lifestyle weight loss program called Healthy Me, (10, 22) which is part of enhanced usual care. The purpose of this paper is to describe the study design, assessments, and intervention.
Methods
Addressing People and Place Microenvironments (APP-Me) is funded by the National Institute of Heart, Lung, and Blood Institute. The study is approved by the Indiana University Institutional Review Board and registered in clinicaltrials.gov (NCT03083964).
Setting and population
This study will recruit a sample of 150 non-Hispanic black women and 150 non-Hispanic white women ages 35–64 who receive care in one of eight federally qualified health centers (FQHC). Participants will reside in Indianapolis, Indiana, a city with slightly less than one million persons as of 2016—66% non-Hispanic white and 28% black—and a median household income of $42,168 (23).
The FQHCs from which participants will be recruited serve a patient population with high rates of poverty—one recently completed study indicated that 50% of obese middle-aged adults in these FQHCs report household incomes of less than $20,000 per year.(24) Further, two thirds of the participants from this study self-identified as black.
Living in the same city, black and white women in the study will have been exposed to largely the same macro physical environments (e.g., number of fast food restaurants and signs) but perhaps not the same micro level physical or social environments (e.g., food in the household, social network eating behavior). Given the influence of automaticity on weight-related behaviors,(25) addressing the influence of micro level exposures is likely critical to furthering research on disparities in weight loss.
User-Centered Design
In the creation of the awareness tool, we adopted a user-centered design process for the development of consumer-facing health information technology.(26–30) This iterative design process was comprised of three phases that (1) sought to understand the users, their tasks and goals, and the different aspects of their surrounding environments (study phase), (2) design abstract representations followed by more traditional artifacts such as wireframes or user interface prototypes, and (3) evaluate the designs against users’ needs and goals.
Phase 1
This study phase included conducting 30–60 minute semi-structured individual interviews with FQHC health coaches and black and white women aged 35–64 years. A basic framework of questions served to probe and understand the characteristics of participants, their perceptions toward nutrition and physical activities, and their corresponding motivations, goals, and barriers. Data collected in this phase were transcribed and used to build an affinity diagram. We identified three key user requirements that influenced our subsequent design process: (1) lack of information, (2) need for social engagement around weight management, and (3) support while making decisions related to eating or physical activity.
Phase 2
Adapting the work discussed by Iacucci and colleagues (31–34), the design phase included a role-playing game that required players to enact and envision potential products or services that will help support their needs specific to information, social engagement, and support in healthy weight loss behaviors. This game included a board designed to mimic a city and took into account the mobility of users, their various contexts, activities, and group interactions. Each of three games required 4–5 players, with each player enacting a scenario, identifying user needs for the scenario, proposing a solution, and participating in a group-based discussion of the identified needs and solution by all the players. Participants converged on the necessity for increased awareness of obesogenic behavior, which included healthy eating and increased physical activity. From this, our team designed a short messaging system (SMS) aimed at creating awareness at the right place and time to offset the influence of obesogenic behaviors.
Findings from the game sessions indicated the need to send SMS messages in a timely manner (e.g., during times when participates were likely to consume calories or remain sedentary). To achieve timely awareness messaging, our team designed an onboarding process where users set approximate times appropriate to receive messages.
Phase 3
Working again with potential participants, our team developed a mobile ecological momentary assessment (EMA) system. EMA assessments occur in the moment and reduce recall bias(35) and is considered the gold standard of experiential sampling.(36) EMA question formats were co-designed and evaluated by users, and include eating, drinking, social interaction, physical activity, and location questions. The onboarding process included users setting approximate times when they woke up, ate, slept, and wished to not be disturbed. This information was envisioned to guide the timing of EMA questions for each participant. Further, APP-Me was envisioned to use EMA information to learn personalized user behavior and send awareness messages to users at the right time.
Study aim
The study Primary Aim was to randomize participants who have EMA response rates of at least 50 percent to enhanced usual care or enhanced usual care plus APP-Me messaging. APP-Me messages were scheduled for up to four delivery times per day that were partially determined by each participant’s EMA patterns (e.g., times of frequent eating). It was hypothesized that, compared to UC participants, APP-Me participants would lose more weight, including a greater proportion achieving weight loss of 2kg or more.
Theoretical framework
The theory of automaticity proposes that behavior is largely based on learned habits, with conscious awareness playing a relatively small role.(37) Habits, and therefore behaviors, are triggered by familiar situations and environments. (38)
Both social and physical environments have been shown to have powerful effects on automatic weight-related behaviors.(39, 40) Experiments have shown that caloric consumption increases from 28% of usual intake while eating with one other person to over 70% while eating with six or more.(25) Moreover, research has shown that, compared to normal weight individuals, obese individuals have an attentional bias when exposed to calorically dense, palatable food cues.(41, 42) Prior research has identified that changing cue exposures may change the behavior. A cue can be virtually anything that triggers a desire, thought, or action in an individual. A laboratory-based study exposed obese individuals to diet words (i.e., a cues) and found less attentional bias toward palatable food words.(41) A recent European randomized trial with overweight dieters offered an “all-you-can-eat”, free bite-sized meat snacks from a tray placed in the corner of a meat store. Participants from this trial entered the meat shop with the smell of grilled chicken coming from a large visible grill in the store. This trial included an experimental arm presenting a prominent poster and a control arm with no poster. The poster exposed participants to an advertisement for a low-calorie recipe available in the store. Control arm participants consumed 40% more snacks than those in the experimental arm.(41) The Theory of Automaticity suggests that exposure to the diet word ‘low calorie’ affects short-term awareness—our brains give more attention to certain stimuli in a situation. Thus we suppose that timely messages may affect attention, positively (more attention to the stimuli) or negatively (less attention to the stimuli).(9)
Participant selection, recruitment and randomization protocol
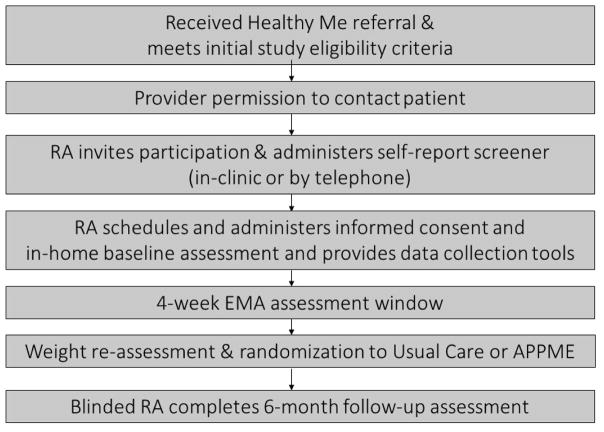
Recruitment involves several steps. First, health system data managers with access to electronic medical records (EMR) identify patients who met study BMI and demographic criteria and received a Healthy Me referral. Second, study research assistants (RAs) seek permission to contact potential participants from FQHC providers. Third, potentially eligible participants are approached at a FQHC visit or receive a telephone call from an RA who invite the patient’s participation in the study. Those indicating interest complete a brief telephone screen. Fourth, those who are eligible are invited to schedule a home visit for informed consent, baseline assessment, and onboarding for EMA. At the end of four weeks of EMA, weight is re-assessed, and randomization was completed using field envelopes created by our biostatistician. To select participants with a higher probability of study completion, only those who responding to at least 50 percent of the EMA question “eating these past 15 minutes?” are eligible for randomization. Finally, at 6 months, blinded RAs completed the 6-month follow-up assessment and collect any study equipment.
Inclusion and Exclusion Criteria
As noted, eligibility requirements include women within the age range of 35–64yrs, with a BMI of 30 or greater, and who received a Healthy Me referral. In addition, participants are required to be English speaking and self-identify as being non-Hispanic black or non-Hispanic white. Those with conditions that may affect weight management are excluded (e.g., psychosis, current cancer treatment, pregnancy or nursing within 6 months, prior bariatric surgery), Current cigarette smokers and alcohol or substance abusers as indicated by their electronic medical record, are also excluded.
Interventions
Enhanced Usual Care
All participants have access to enhanced usual care, which includes access to the Healthy Me program.(10, 22) The Healthy Me program is structured around the 5A’s of behavior change (43) operates in Eskenazi FQHCs with a health coach (44) counseling adult obese patients. The Healthy Me patients are typically referred by their primary care providers after they receive a message about the patient’s high BMI in the EMR system. A primary care provider may refer a patient with a BMI of 30 or greater to meet with a Healthy Me coach. Healthy Me coaches are certified in behavior change counseling and fitness instruction, and are present two or more days per week in each of 12 FQHC.
The Healthy Me program emphasizes increased physical activity, healthy food choices, and portion control. Referred patients can meet with coaches to have their current weight-related behavior assessed, receive assistance in problem-solving, and set an action plan for weight loss. The action plan is entered into a Healthy Me database and becomes part of the patient’s EMR. Health coaches give patients guidance and information on community-based opportunities for physical activity and also provide weekly FQHC based exercise and nutrition classes. In addition, dietary and physical activity self-monitoring instructions and logs are provided. A “passport to wellness” incentive program gives patients points for participation that earn them small incentive rewards (e.g., t-shirt, produce coupons, gym trial). If desired, patients can also meet with the FQHC dietitian for nutrition guidance. A consistent message of the program is “eat less, move more.”
APP-Me
The APP-Me intervention consists of personalized, automated messages. The messages are intended to bring participants’ attention and awareness back to healthy eating and physical activity. The messages that achieve this are likely very personal. Hence, the system we created allows participants to create and rate messages. Messages are coded by broad themes (e.g., activity, food, neutral) and subthemes (e.g., gardening, inspiration, grocery shopping, eating out, walking, family, religion, celebrities). An example of a food themed message with a religion subtheme is shown in Figure 2. This message was created by the study team. An example of a neutral themed inspirational message created by a participant during design work is shown in Figure 3.
Figure 2.

Example of a study team created food themed message with religious subtheme.
Figure 3.
Example of a participant created neutral themed inspirational message.
Both study staff and participants create the messages. Our team uses a web-based system to produce a master library of messages. As for participant-created messages, text is created and saved, images are taken or selected from camera gallery, and audio-recordings are made—all within the app. When a participant creates a message, it is saved to her message library.
To avoid predictability, messages are randomly generated from both the master and participant libraries. As these were received, participants are able to respond by selecting a thumbs up or thumbs down icon. These responses provide data for the prioritizing or deletion of messages from a participant’s library.
Participants receive a minimum of four messages per day. Every two weeks, participants have the opportunity to increase this frequency by one message. Delivery is scheduled for morning, mid-day, early and late evening but the actual times of these four periods are based upon each participant’s onboarding selections (e.g., wake and physical activity times) and EMA-determined times or places of frequent eating. Onboarding data automatically populate the message scheduler but EMA patterns are reviewed by team members prior to being considered for automatic scheduling. By initially observing patterns and accumulating data, we will be able to create an algorithm of EMA patterns that will then allow automated message scheduling based on EMA data.
Measures
Baseline RA-administered assessments are completed in participants’ homes to allow a physical environment assessment of the home. The in-home baseline assessment requires less than 30 minutes. Interviewer-administered assessments and surveys are carried out using Research Electronic Data Capture (REDCap). Table 1 shows the assessments and schedule.
Table 1.
Measures
| Construct or Object | Measure or Source | Frequency |
|---|---|---|
| Age | EMR | Baseline (B) |
| Household income | Interview Qs | B |
| Employment hours | Interview Qs | B |
| Years of education | Interview Qs | B |
| Health literacy and numeracy | New Vital Sign(46) | B |
| Current/Desired weight and body shape | Interview Qs and body figure rating scale | B, 6 months |
| Disease diagnoses | EMR | B, 6 |
| Prescription medications | EMR | B, 6 |
| Smoking status | Interview Qs | B, 6 |
| Perceived health | SF-36 scale | B, 6 |
| Depression and Anxiety | PHQ-2 and GAD-2 scales | B, 6 |
| Food security | USDA 6-item Form USDA Food Security Survey(47) | B, 6 |
| Binge eating | SCOFF screener(48) | B, 6 |
| Physical activity | Accelerometry | 4 weeks |
| Eating frequency | EMA | 4 weeks |
| Social network | Interview Qs | B |
| Physical home environment | Interview Qs and home assessment | B |
| Social contacts | EMA | 4 weeks |
| Height | Portable stadiometer | B |
| Weight (primary outcome) | Portable scale | B, 6 months |
We obtain some covariates to allow us to adjust for potentially important correlates of weight loss or gain and any group differences. Age, gender, race, and smoking are obtained initially from EMR data but confirmed at the time of screening. Literacy and numeracy affects weight management and varies by ethnicity(45) and we use the New Vital Sign as a representation of both. (46) Food security and binge eating are measured as covariates but also as screeners for need of assistance. Our IRB protocol contains a procedure for referral in cases of a positive screen. Eating disorders (i.e., anorexia nervosa), however, are rare in our target population and a formal screen is not practical.
The baseline assessment includes a semi-structured individual interview with questions on how many televisions are in the home, whether there is a scale or fitness equipment, how often fast food, chips, sodas, fruit juices, desserts, and fried foods are in the home, and whether these foods are visible or hidden. The RA also records whether there is a television in or visible from the kitchen, whether a television was turned on when entering the home, and whether there is visible food, frying pans, or fitness equipment.
The RAs also measure the participants’ weight using the Tanita BWB-800 scale, which has a capacity of 440lbs +/− 0.1lbs. Participants stand flat footed, shoes removed, while wearing light clothing. Two separate measurements are taken and averaged; if weight differs by more than 0.2lbs, a third measurement is taken; and the least congruent measurement is dropped.
Immediately following RA-administered assessments, participants completed onboarding questions within the study app, which includes setting a usual schedule of sleep, wake, and do not disturb times to inform the timing of EMA assessments. We have chosen a maximum of three samples in each quadrant of a participant’s waking day; or a maximum of 12 samples per day. As our investigation of eating behavior patterns does not require detailed data on food type or energy intake, to minimize burden and maximize response the EMA assessment asks a single eating and single drinking question, “Eating now or in the past 15 minutes?” [Yes, No] and “Drinking now or in the past 15 minutes?” [No, nothing to drink, Water, Coffee/Tea—no milk or sugar, Other].
The APP-Me app captures location (as longitude and latitude) every 10 seconds from the mobile device. Using the Google Places API, we obtained a probability that the captured latitude and longitude represents a particular place. To improve this, when it appears from GPS that a participant’s location changed we ask participants via EMA to report their current location (e.g., home, work, restaurant, retail store, etc). Over time, our system constructs a library of frequented places for a participant and any future latitude and longitude readings with coordinates within 50 meters of a participant’s frequent place are assumed to be that place.
We ask participants to give the first names of up to four persons (ties) they feel close to, any additional household members, and how many people live in their household. This facilitates responses to the EMA question “With anyone?”—the first names of close contacts are displayed as response options. To avoid reminding participants of possible loneliness, this question is not asked when at home for participant’s who report living alone.
EMA responses, GPS location, and accelerometry data are captured from the mobile devices are stored in a secure Indiana University server, and later merged with interviewer-administered data stored in REDCap. Participants either use their own smartphone, or a study supplied smartphone (Google Pixel, 32 GB).
Sample Size and Power
The sample size of this study was determined to ensure adequate power for assessing the effect of the APP-Me intervention on weight loss. For this aim, we assume that weight loss in the study sample has a standard deviation of 10lbs (4.535 kg). We intend to recruit and prospectively follow 240 women, with 120 women in each treatment arm, to estimate the intervention effect. Assuming an attrition of 20%, the proposed sample size gives us 92% power to detect a 2.0 kg difference in weight changes between the two intervention arms using a two-sample t test at the 0.05 significance level. If we dichotomize the outcome as success (and failure) of achieving 2kg weight loss, using a chi-square test, we will have 86% power to detect a 20% difference in the rate of weight loss success between the two treatment arms (e.g., 28% vs 48%).
Analysis
The primary Specific Aim is to assess 6 month weight change between the two study arms. The main hypothesis is that more participants in the APP-Me arm will lose 2kg or more by the end of follow-up. We will test this hypothesis using a chi-square test. With the random assignment of individual participants to the two treatment arms, we will have an opportunity to re-examine the balance of baseline characteristics of the study subjects by race and by intervention arm, as in analysis of data from studies of factorial design. Before we test the main hypothesis, we will also examine the effects of obesogenic exposures on weight loss in the enhanced usual care arm using linear regression analysis. With the real time exposure data generated by the study, we will evaluate the influences of individual exposures on weight loss in the UC subjects. The effects of other contextual variables such as places of eating and activity, or lack thereof, can be accommodated similarly. We hypothesize that less frequent exposure to obesogenic cues is associated with greater weight loss. Separate analyses will be conducted for black and white women to estimate race-specific magnitudes of exposure influence. In case of data suggesting a need to control for unbalanced characteristics, we will use logistic regression analysis to accommodate the covariate adjustment. We will assess the racial disparity in 6 month weight change. We will explore whether racial disparities in 6 month weight change are less in the APP-Me arm by comparing the amount of weight loss differences due to intervention between blacks and whites. We will include a race by intervention effect in the linear regression model analysis. As in previous studies,(49) the difference in the race coefficients with and without exposure variables will represent the effect size.
Summary
APP-Me is an outcome of more than a decade of collaboration in health promotion with safety-net health care providers and the patients they serve. This project was inspired by the need to support patients outside of usual clinic physical space and time when patients are experiencing the situations that trigger eating or sedentary behavior (e.g., at home alone and at evening times) and to increase the frequency of support for weight management, which may be especially helpful for persons exposed to significant obesogenic environments and behavior in their daily lives. APP-Me is also inspired by recent advances in theoretical models of automatic behaviors and the influence of momentary situations on those behaviors. APP-Me is enabled by very recent advances in mobile technology, our highly diverse project team, and our embedment in this large urban safety-net health system.
Our project is innovative in several ways. First, we have worked for approximately 12 months with urban low-income women with obesity in the design of both EMA and awareness messaging. The app was constructed with their input at every step – few health applications have been designed with and for urban low-income women. Second, our use of an intense 4-week period of EMA data collection as a guide to the timing of awareness message delivery is novel. Third, we are aware of just one study that has incorporated user-created messages into a weight loss intervention such as APP-Me (50, 51). Fourth, APP-Me is being tested on top of a traditional coach-based model of weight loss support that is operated within safety-net clinical sites.
Commercial apps exist that provide something similar to the awareness messages APP-Me is testing. Fitbit, for example, sends messages that are intended to be motivating in relation to goals set by users within the app. We are not aware that the impact of these messages has been tested. We are also not aware of a weight management or fitness app that uses EMA data to guide the timing of messaging. MoodMission is an app that comes closest perhaps in that it has an onboarding process that includes questions about the times of day your mood may need support. Messages are then delivered at those times. With very many commercial apps and new products and existing product updates continuously added, it is likely that something similar to APP-Me exists or will arise. As pragmatic behavioral scientists, our objective is to design weight loss solutions for those most vulnerable to obesity and to establish an evidence-base for potential users or to offer guidance for future improvements or redirections.
Whether a machine-delivered message can carry the emotional support required for momentary behavior change is not known. Certainly, impactful message designs and optimal delivery timing are highly personalized and require continuous learning and tailoring. Sustaining engagement in such messages over time again points to a need for personalization and continuous learning. Many commercial apps enlist social ties to provide accountability and social engagement (e.g., Twinbody, Thirty, PumpUp). Social networks are smaller in lower-income adults (52), so future efforts to include social ties in APP-Me may require working with providers, pastors, or persons who may not be known to the user but who also use the app. APP-Me is a first step in the direction of continuous learning for personalization of scalable awareness messaging around weight-related behaviors in a highly vulnerable and understudied population. We anticipate that the APP-Me platform will provide guidance for future work by us and others.
Figure 1.
Study Recruitment, Randomization, and Assessments.
Acknowledgments
This project is supported by National Institutes of Health Grant R01 HL128494.
References
- 1.McGovern L, Miller G, Hughes-Cromwick P. The relative contribution of multiple determinants to health outcomes: Project HOPE. 2014. [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA: the journal of the American Medical Association. 2014;311(8):806–14. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Institute of Medicine. Comparative Effectivess Research. Washington, DC: 2009. [Google Scholar]
- 4.National Center for Health Statistics. Healthy People 2010 Final Review. Atlanta, GA: Centers Disease Control and Prevention; 2013. [Google Scholar]
- 5.Kumanyika SK, Whitt-Glover MC, Haire-Joshu D. What works for obesity prevention and treatment in black Americans? Research directions. Obesity reviews: an official journal of the International Association for the Study of Obesity. 2014;15(Suppl 4):204–12. doi: 10.1111/obr.12213. [DOI] [PubMed] [Google Scholar]
- 6.Samuel-Hodge CD, Gizlice Z, Cai J, Brantley PJ, Ard JD, Svetkey LP. Family functioning and weight loss in a sample of african americans and whites. Annals of behavioral medicine: a publication of the Society of Behavioral Medicine. 2010;40(3):294–301. doi: 10.1007/s12160-010-9219-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pi-Sunyer X. The look AHEAD trial: a review and discussion of its outcomes. Current nutrition reports. 2014;3(4):387–91. doi: 10.1007/s13668-014-0099-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The Diabetes Prevention Program: baseline characteristics of the randomized cohort. The Diabetes Prevention Program Research Group. Diabetes care. 2000;23(11):1619–29. doi: 10.2337/diacare.23.11.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bargh JA, Chen M, Burrows L. Automaticity of social behavior: direct effects of trait construct and stereotype-activation on action. Journal of personality and social psychology. 1996;71(2):230–44. doi: 10.1037//0022-3514.71.2.230. [DOI] [PubMed] [Google Scholar]
- 10.Clark D, Chrysler L, Perkins A, Keith NR, Willis DR, Abernathy G, et al. Screening, referral, and participation in a weight management program implemented in five CHCs. Journal of health care for the poor and underserved. 2010;21(2):617–28. doi: 10.1353/hpu.0.0319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clark DO, Keith N, Chrysler L, Perkins AJ, Willis D. Design and reach of a primary care weight management program. J Health Care Poor Underserved. 2008b;19(1):171–9. doi: 10.1353/hpu.2008.0014. [DOI] [PubMed] [Google Scholar]
- 12.Bronner Y, Boyington JE. Developing weight loss interventions for African-American women: elements of successful models. J Natl Med Assoc. 2002;94(4):224–35. [PMC free article] [PubMed] [Google Scholar]
- 13.Kumanyika SK, Wadden TA, Shults J, Fassbender JE, Brown SD, Bowman MA, et al. Trial of family and friend support for weight loss in African American adults. Archives of internal medicine. 2009;169(19):1795–804. doi: 10.1001/archinternmed.2009.337. [DOI] [PubMed] [Google Scholar]
- 14.Keith NR, Xu H, de Groot M, Hemmerlein K, Clark DO. Identifying Contextual and Emotional Factors to Explore Weight Disparities between Obese Black and White Women. Clinical medicine insights Women’s health. 2016;9(Suppl 1):85. doi: 10.4137/CMWH.S34687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stevens VJ, Obarzanek E, Cook NR, Lee IM, Appel LJ, Smith West D, et al. Long-term weight loss and changes in blood pressure: results of the Trials of Hypertension Prevention, phase II. Annals of internal medicine. 2001;134(1):1–11. doi: 10.7326/0003-4819-134-1-200101020-00007. [DOI] [PubMed] [Google Scholar]
- 16.Hamman RF, Wing RR, Edelstein SL, Lachin JM, Bray GA, Delahanty L, et al. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes care. 2006;29(9):2102–7. doi: 10.2337/dc06-0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Agboola S, Jethwani K, Lopez L, Searl M, O’Keefe S, Kvedar J. Text to move: a randomized controlled trial of a text-messaging program to improve physical activity behaviors in patients with type 2 diabetes mellitus. Journal of medical Internet research. 2016;18(11) doi: 10.2196/jmir.6439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kinnafick F-E, Thøgersen-Ntoumani C, Duda J. The effect of need supportive text messages on motivation and physical activity behaviour. Journal of behavioral medicine. 2016;39(4):574–86. doi: 10.1007/s10865-016-9722-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fischer HH, Fischer IP, Pereira RI, Furniss AL, Rozwadowski JM, Moore SL, et al. Text message support for weight loss in patients with prediabetes: a randomized clinical trial. Diabetes care. 2016;39(8):1364–70. doi: 10.2337/dc15-2137. [DOI] [PubMed] [Google Scholar]
- 20.Lin M, Mahmooth Z, Dedhia N, Frutchey R, Mercado CE, Epstein DH, et al. Tailored, interactive text messages for enhancing weight loss among African American adults: the TRIMM randomized controlled trial. The American journal of medicine. 2015;128(8):896–904. doi: 10.1016/j.amjmed.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 21.Shapiro JR, Koro T, Doran N, Thompson S, Sallis JF, Calfas K, et al. Text4Diet: a randomized controlled study using text messaging for weight loss behaviors. Preventive medicine. 2012;55(5):412–7. doi: 10.1016/j.ypmed.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 22.Clark DO, Frankel RM, Morgan DL, Ricketts G, Bair MJ, Nyland KA, et al. The meaning and significance of self-management among socioeconomically vulnerable older adults. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2008;63(5):S312–S9. doi: 10.1093/geronb/63.5.s312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.QuickFacts A. US Census Bureau; [accessed 22 May 2009]. 2010. Internet Website http://quickfacts census gov. [Google Scholar]
- 24.Keith NRXH, Weiner M, Clark DO. An RCT of Clinic, Community, and Video-Conference Behavior Change Counseling for Weight Loss in Urban Poor Adults. 2017 in preparation. [Google Scholar]
- 25.Wansink B. Mindless Eating: Why We Eat More Than We Think. New York, NY: Bantam Books; 2010. Reprint Edition ed. [Google Scholar]
- 26.Beyer H, Holtzblatt K. Contextual Design: A Customer-Centered Approach to Systems Designs (Morgan Kaufmann Series in Interactive Technologies) 1997. [Google Scholar]
- 27.Buxton B. Sketching user experiences: getting the design right and the right design. Morgan Kaufmann; 2010. [Google Scholar]
- 28.Nielsen J. Iterative user-interface design. Computer. 1993;26(11):32–41. [Google Scholar]
- 29.Rogers Y, Sharp H, Preece J. Interaction design: beyond human-computer interaction. John Wiley & Sons; 2011. [Google Scholar]
- 30.Snyder C. Paper prototyping: The fast and easy way to design and refine user interfaces. Morgan Kaufmann; 2003. [Google Scholar]
- 31.Iacucci G, Mäkelä A, Ranta M, Mäntylä M, editors. Proceedings COOP. 2000. Visualizing context, mobility and group interaction: role games to design product concepts for mobile communication. [Google Scholar]
- 32.Iacucci G, Kuutti K. Everyday life as a stage in creating and performing scenarios for wireless devices. Personal and Ubiquitous Computing. 2002;6(4):299–306. [Google Scholar]
- 33.Iacucci G, Iacucci C, Kuutti K, editors. Proceedings of the second Nordic conference on Human-computer interaction. ACM; 2002. Imagining and experiencing in design, the role of performances. [Google Scholar]
- 34.Kuutti K, Iacucci G, Iacucci C, editors. Acting to know: improving creativity in the design of mobile services by using performances; Proceedings of the 4th conference on Creativity & cognition; 2002; ACM; [Google Scholar]
- 35.Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- 36.Kahneman D, Krueger AB, Schkade DA, Schwarz N, Stone AA. A survey method for characterizing daily life experience: the day reconstruction method. Science. 2004;306(5702):1776–80. doi: 10.1126/science.1103572. [DOI] [PubMed] [Google Scholar]
- 37.Marteau TM, Hollands GJ, Fletcher PC. Changing human behavior to prevent disease: the importance of targeting automatic processes. Science. 2012;337(6101):1492–5. doi: 10.1126/science.1226918. [DOI] [PubMed] [Google Scholar]
- 38.Fogg BJ, editor. A behavior model for persuasive design. Proceedings of the 4th international Conference on Persuasive Technology; 2009; ACM; [Google Scholar]
- 39.Wansink B. Mindless Eating: Why We Eat More Than We Think. New York, NY: Bantam Books; 2006. [Google Scholar]
- 40.Kremers SP, Eves FF, Andersen RE. Environmental changes to promote physical activity and healthy dietary behavior. J Environ Public Health. 2012;2012:470858. doi: 10.1155/2012/470858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Papies EK. Goal Priming in Dieters: Recent Insights and Applications. Curr Obes Rep. 2012;1(2):99–105. doi: 10.1007/s13679-012-0009-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hofman W, van Koningsbruggen GM, Stroebe W, Ramanathan S, Aarts H. As pleasure unfolds. Psychol Sci. 2010;21(12):1863–70. doi: 10.1177/0956797610389186. [DOI] [PubMed] [Google Scholar]
- 43.Whitlock EP, Orleans CT, Pender N, Allan J. Evaluating primary care behavioral counseling interventions: an evidence-based approach. American journal of preventive medicine. 2002;22(4):267–84. doi: 10.1016/s0749-3797(02)00415-4. [DOI] [PubMed] [Google Scholar]
- 44.Bennett HD, Coleman EA, Parry C, Bodenheimer T, Chen EH. Health coaching for patients with chronic illness. Fam Pract Manag. 2010;17(5):24–9. [PubMed] [Google Scholar]
- 45.Rothman RL, Housam R, Weiss H, Davis D, Gregory R, Gebretsadik T, et al. Patient understanding of food labels: the role of literacy and numeracy. American journal of preventive medicine. 2006;31(5):391–8. doi: 10.1016/j.amepre.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 46.Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3(6):514–22. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Blumberg SJ, Bialostosky K, Hamilton WL, Briefel RR. The effectiveness of a short form of the Household Food Security Scale. Am J Public Health. 1999;89(8):1231–4. doi: 10.2105/ajph.89.8.1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Morgan JF, Reid F, Lacey JH. The SCOFF questionnaire: assessment of a new screening tool for eating disorders. Bmj. 1999;319(7223):1467–8. doi: 10.1136/bmj.319.7223.1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stewart JC, Zielke DJ, Hawkins MA, Williams DR, Carnethon MR, Knox SS, et al. Depressive symptom clusters and 5-year incidence of coronary artery calcification: the coronary artery risk development in young adults study. Circulation. 2012;126(4):410–7. doi: 10.1161/CIRCULATIONAHA.112.094946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.de Vries RA, Truong KP, Kwint S, Drossaert CH, Evers V, editors. Crowd-Designed Motivation: Motivational messages for exercise adherence based on behavior change theory; Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems; 2016; ACM; [Google Scholar]
- 51.de Vries RA, Zaga C, Bayer F, et al. Experts Get Me Started, Peers Keep Me Going: Comparing Crowdversus Expert-Designed Motivational Text Messages for Exercise Behavior Change. EAI International Conference on Pervasive Computing Technologies for Healthcare; ACM; 2017. [Google Scholar]
- 52.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–9. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]