Abstract
Background and Purpose
Deficiencies in stroke preparedness causes major delays to stroke thrombolysis, particularly among economically disadvantaged minorities. We evaluated the effectiveness of a stroke preparedness intervention delivered to preadolescent urban public school children on the stroke knowledge/preparedness of their parents.
Methods
We recruited 3,0704th through 6th graders and 1,144 parents from 22 schools into a cluster-randomized trial with schools randomized to the Hip Hop Stroke (HHS) intervention or attentional control (nutrition classes). HHS is a 3-hour culturally tailored, theory-based, multimedia stroke literacy intervention targeting school children, which systematically empowers children to share stroke information with parents. Our main outcome measures were stroke knowledge/preparedness of children and parents using validated surrogates.
Results
Among children, it was estimated that 1% (95% CI: 0-1%) of controls and 2% (95% CI: 1-4%, P=.09) of the intervention group demonstrated optimal stroke preparedness (perfect scores on the knowledge/preparedness test) at baseline, increasing to 57% (95% CI: 44-69%) immediately after the program in the intervention group compared to 1% (95% CI: 0-1%, P<.001) among controls. At 3-month follow-up, 24% (95% CI: 15-33%) of the intervention group retained optimal preparedness, compared to 2% (95% CI: 0-3%, P<.001) of controls.
Only 3% (95% CI: 2-4%) of parents in the intervention group could identify all four letters of the stroke FAST (Facial droop, Arm weakness, Speech disturbance, Time to call 911)acronym at baseline, increasing to 20% at immediate post-test (95% CI: 16-24%) and 17% at 3-months delayed post-test (95% CI: 13-21%, P=.0062), with no significant changes (3% identification)among controls. Four children, all in the intervention group, called 911 for real life stroke symptoms, in one case overruling a parent's wait-and-see approach.
Conclusions
Hip Hop Stroke is an effective, inter-generational model for increasing stroke preparedness among economically disadvantaged minorities.
Keywords: Stroke Treatment, Prehospital delays, Stroke education, Stroke awareness
Introduction
The nationwide Get-With-The-Guidelines stroke registry continues to demonstrate prehospital delays as the biggest rate-limiting step to improving acute stroke treatment in the United States1. Because of delays, only 25% of stroke patients arrive in the hospital within 3 hours1. Consequently, approximately 7% of ischemic stroke patients in the United States are treated with intravenous thrombolysis with tissue plasminogen activator (tPA)2, with lower rates of tPA use among Blacks compared to Whites.3
If all patients with known stroke symptom onset times called 911 immediately, one study showed a 24% increase in the rate of thrombolysis4. But efforts to improve stroke preparedness have focused on mass media campaigns that have been limited by the high costs of advertising, lack of cultural tailoring, low penetration into ethnic minority populations5 and outcome effects (calling 911 for stroke) that dissipate once the media campaign ends.6
Targeting the general public and not just individuals at risk for stroke is important because stroke patients call 911 for themselves approximately 4% of the time, while witnesses are responsible the rest of the time7. This is the rationale behind targeting large groups and why stroke education in schools is gaining traction as an alternative to mass media campaigns. Children are increasingly being raised by older parents or grandparents8 who may be at high risk for stroke: they may be able to serve as “transmission vectors” of stroke information into their households, and may be the only witnesses present during a stroke.
The primary aim of this study is to evaluate the effectiveness of a stroke education intervention delivered exclusively to preadolescent children on the stroke preparedness of children and of their parents (henceforth parents also refers to grandparents).
Hypothesis 1 (H1): There will be no differences in stroke preparedness at baseline between groups for parents and for children.
Hypothesis 2 (H2): Children in the intervention arm will demonstrate greater stroke preparedness immediately after and at three months following intervention as compared to those in the control arm.
Hypothesis 2a (H2a): Parents in the intervention arm will demonstrate greater stroke preparedness as well as stroke identification (FAST) immediately after and at three months following intervention as compared to those in the control arm.
Hypothesis 3 (H3): Compared to students in the control condition, children in the intervention arm will be more likely to communicate stroke information to their parents.
Hypothesis 4 (H4): In homes in which information is shared, parents in schools assigned to the intervention arm will demonstrate greater stroke preparedness, compared to their baseline knowledge, at 1-week and at 3-months follow-up, and compared to parents in the control arm.
Mediation analysis (H4M): Analyses to establish that the effect of the intervention on adult preparedness is mediated by improvement in children's knowledge.
Methods
Data supporting findings of this study are available from the corresponding author upon reasonable request.
Design
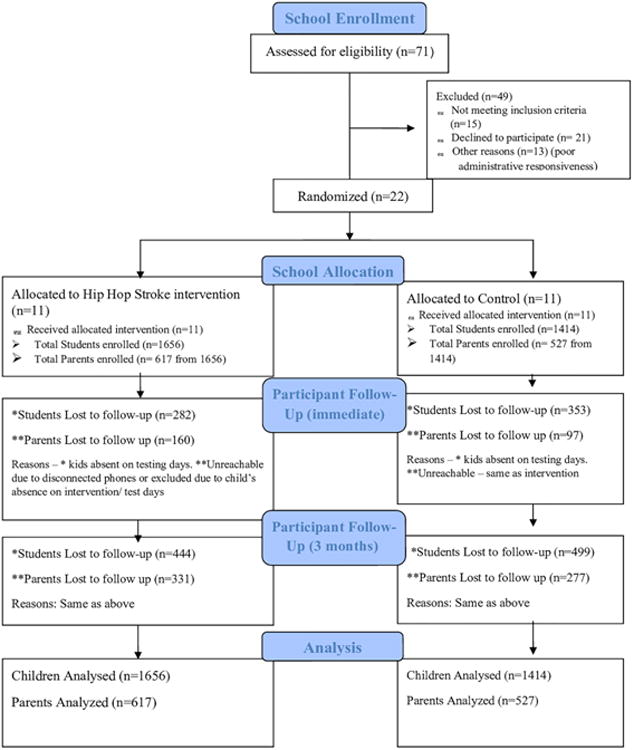
Children in 4th - 6th grades (aged 9-12 years) attending high need New York City (NYC) public schools and their parents were eligible for inclusion. Schools were randomized into either a stroke preparedness intervention (Hip Hop Stroke) or an attentional control (nutrition classes). Randomization occurred at the school level in a 1:1 ratio; written consent was obtained from parents for their child and themselves. Assent was obtained from each child. Details of enrollment and retention are shown in Figure 1. Further information on study procedures is available in a previous report9 and online supplement.
Figure 1.
Intervention
Hip Hop Stroke (HHS) is a culturally tailored intervention targeting urban minority children. Children undergo three, 1-hour modules separated by at least 24 hours (online supplement Table I). Theoretical models underpinning HHS are detailed in an earlier report.10 In brief, HHS is a modular, multi-media, school-based intervention that uses hip-hop music containing stroke lyrics, two synergistic 3.5 minute animated narrative cartoons, a “clotbuster” (thrombolytic) stroke video game, and a comic book (online supplement Figure I), to teach and motivate children to share stroke information with parents through homework activity that leverages an online HHS portal. No direct intervention is provided to parents. The children watch each cartoon three times (once per module)11. The cartoons teach recognition of the five “SUDDENS” stroke symptoms (sudden confusion or trouble speaking; unilateral numbness or weakness; trouble seeing; loss of balance, incoordination or dizziness; and severe headache with no known cause), the availability and benefit of time-dependent thrombolysis, lifestyle prevention measures, calling 911, and encourage children to share stroke information with parents.
Control Condition
The United States Department of Agriculture's (USDA) “My Pyramid” nutrition program constituted the attentional control program. This was adapted into three, 1-hour class modules to mirror the intervention and delivered by a trained facilitator.
Outcomes
Primary outcomes were child and parental stroke knowledge/preparedness. Parental outcomes were assessed with in-person surveys at baseline and by telephone during follow-up. Child outcomes were assessed in-person within classrooms. A secondary/exploratory outcome was the assessment of the occurrence and response to familial stroke-like symptoms after participating in study arms: whether 911 was called, and the child's role in facilitating stroke recognition or EMS activation. An independent stroke neurologist adjudicated the self-reported stroke event in a telephone interview.
Measures
1) A 7-item instrument was used to assess stroke knowledge/preparedness. This primary outcome measure was administered to children and parents. It included knowledge of the five SUDDENS symptoms, a question from the Stroke Action Test (STAT) evaluating intent to call 91112, and a distractor item - sudden chest pain - to facilitate comparison with the nationwide Behavioral Risk Factor Surveillance Survey (BRFSS)13. 2) A second outcome measure administered only to parents assessed as knowledge of the FAST acronym (Facial droop, Arm weakness, Speech disturbance, Time to call 911).14 This measure has been used to promote stroke identification and urgent action by mass media campaigns globally, identifies 88.8% of stroke/transient ischemic attack patients15, and has been associated with reduced prehospital delays to stroke care.16
Additional information about child-parental sharing was provided by a question asked of parents at post-test. “Did your child share any information from the program with you?”
We added a Self-Efficacy (SE) scale with subconstructs for stroke recognition, appropriate action in response to stroke symptoms, ability to describe a stroke event to a 911 operator, and ability to teach a friend or family member how to recognize a stroke.
Covariates
A 7-item composite of barriers to calling 911 (e.g. cost of ambulance and hospitalization) derived from focus groups on representative adults and literature review was included in the parent questionnaire as a covariate. Additionally, socio-demographic variables (Table 1), parental health literacy17, and parental stroke experience (presence of stroke in a family member, close relative or close friend with whom the parent has had contact) were assessed.
Table 1.
Baseline parent demographics (n=1144).
| Total N=1144 | Control N=527 | Intervention N=617 | |||||
|---|---|---|---|---|---|---|---|
| n | % | N | % | N | % | ||
| Age | 25 or younger | 22 | 1.9 | 8 | 1.5 | 14 | 2.2 |
| 26-35 | 399 | 34.9 | 200 | 38.0 | 199 | 32.3 | |
| 36-45 | 469 | 41.0 | 191 | 36.2 | 278 | 45.1 | |
| 46-55 | 190 | 16.6 | 98 | 18.6 | 92 | 14.9 | |
| 55 and older | 48 | 4.2 | 23 | 4.3 | 25 | 4.1 | |
| No response, data missing | 16 | 1.4 | 7 | 1.3 | 9 | 1.5 | |
| Gender | Male | 176 | 15.4 | 91 | 17.3 | 85 | 13.8 |
| Female | 963 | 84.2 | 435 | 82.5 | 528 | 85.6 | |
| No response, data missing | 5 | 0.4 | 1 | 0.2 | 4 | 0.6 | |
| Ethnicity | Black or African American | 837 | 73.2 | 414 | 78.6 | 423 | 68.6 |
| White | 63 | 5.5 | 18 | 3.4 | 45 | 7.3 | |
| Non-Black Hispanic | 55 | 4.8 | 24 | 4.6 | 31 | 5.0 | |
| Asian Pacific Islander | 53 | 4.6 | 4 | .8 | 49 | 7.9 | |
| Other | 23 | 2.0 | 14 | 2.7 | 9 | 1.5 | |
| No response, data missing | 113 | 9.9 | 53 | 10.0 | 60 | 9.7 | |
| Hispanic | Yes | 154 | 13.5 | 72 | 13.7 | 82 | 13.3 |
| No | 706 | 61.7 | 268 | 50.9 | 438 | 71.0 | |
| No response, data missing | 284 | 24.9 | 187 | 35.4 | 97 | 15.7 | |
| Highest level of education | Less than HS | 114 | 9.0 | 49 | 8.7 | 65 | 9.2 |
| Completed HS | 300 | 26.2 | 136 | 25.8 | 164 | 26.6 | |
| Some college/Associate's degree | 336 | 29.3 | 170 | 32.2 | 166 | 26.9 | |
| Completed Bachelor's degree | 227 | 19.8 | 95 | 18.0 | 132 | 21.4 | |
| Graduate/advanced degree (or some work toward it) | 110 | 9.6 | 47 | 8.9 | 63 | 10.2 | |
| No response, data missing | 57 | 5.0 | 30 | 5.7 | 27 | 4.4 | |
Data Analysis
For the stroke preparedness instrument, internal consistency reliability estimates, including Cronbach's alpha and McDonalds omega total were calculated. Additionally, the explained common variance (ECV), an estimate of dimensionality derived from a factor analysis model was computed. Psychometric analyses were conducted using the psych package in R18. Alpha, McDonald's omega total, and ECV were computed using tetrachoric correlations for binary data. Observed means and standard errors were computed using SPSS complex samples19.
Analysis of longitudinal data was performed on an intention to treat basis and adjusted for clustering of subjects within schools using SAS PROC Mixed20 for continuous outcomes and SAS PROC Glimmix for binary outcomes. The statistical tests were based on trajectories (slopes) estimated from observed data points over three waves of data (pre, immediate post, and 3-month delayed post-tests). Significance tests were two-tailed, and the alpha level was set at 0.05 for each primary outcome. The end points entered into the models when treated as continuous variables did not require prior transformation, based on graphical inspection of the distribution of the outcome and of the residuals from the models. Adjusted means (s.e.) of the end points during follow-up were estimated as follows. Power terms were added if a non-linear model provided a better fit. The stroke preparedness measure evidenced a non-linear trajectory; thus, a quadratic (group*test2) term was included to model the non-linearity. A significant quadratic term indicates differences between treatment groups, with one of the groups exhibiting a U-shaped distribution of the outcome over time. Group heterogeneity in cluster and residual variances also required modeling. Sensitivity analyses were conducted using the same methodology described above including participants that completed at least two tests (n=2,789 for the students and n=887 for the parents).
The best covariance structure was selected based on examination of the Akaike Information Criterion21 and Schwarz's Bayesian Information Criterion22. An unstructured covariance structure was observed to be superior, and was thus used in all analyses.
Power calculations were performed for the group and method with the most stringent requirements. Power calculations were performed for endpoint analyses, treating the outcome as binary (100% correct vs. <100%) on the knowledge/preparedness and FAST literacy tests (see online supplement for details). Power was greater than 0.90 for the child preparedness test and the parent FAST test, but the study was underpowered for the parent preparedness test (treated as binary), given the observed effect sizes (shown below).
The potential mediating effect of child knowledge on parent knowledge was also evaluated through the assessment of p-values for the mediating path coefficients. Details of the analyses are in the online supplement. Finally, the effect of the child sharing information about the program with parents was evaluated using a mixed model evaluating the continuous version of the parental stroke knowledge/preparedness and FAST composite outcomes. An interaction term was used to examine whether shared information resulted in larger effects.
Ethics Review approval was obtained from the New York City Department of Education's Institutional Review Board and Columbia University's Institutional Review Board.
Results
Reliability of measures
Data on the psychometric properties of measures used can be found in the online supplement.
Attrition
Overall, 3,0704th – 6th graders in 22 schools and 1,144 of their parents were enrolled. The primary analyses were intent-to-treat, and therefore all children and parents enrolled were analyzed (Figure 1). In sensitivity analyses,2,789 children (90.87%) and 887 parents (77.5%) who completed at least two tests were included in the analyses. A parent was considered as “followed” if they completed the pre-test and at least one post-test. There were 257 parents with no follow-up tests and 887 parents with at least one follow-up test. There were no significant differences between those parents who were followed or not.
Children (H1, H2)
There was no significant difference in baseline tests between the intervention and control groups (H1) regardless of whether stroke preparedness was analyzed as a binary variable (perfect score on the knowledge/preparedness test) or as a continuous measure. Model-based means from the analyses of the binary outcomes (H2) for children were similar to the observed means (see Table 2). The model based means were: 1% (95% CI: 0-1%) in the control and 2% (95% CI: 1-4%, P=0.09) in the intervention group demonstrated optimal stroke preparedness (perfect scores) at baseline, increasing to 57% (95% CI: 44-69%) immediately after the program in the intervention as contrasted with 1% (95% CI: 0-1%, P<0.001) in the control. At 3-month follow-up, 24% (95% CI: 15-33%) of the intervention retained optimal preparedness, compared to 2% (95% CI: 0-3%, P<0.001) in the control. Treated as a continuous measure, examined over three time-points, the intervention group evidenced significantly greater gains in preparedness relative to controls (P<0.0001). Self-Efficacy across all subconstructs increased significantly (P<0.0001) relative to the control group.
Table 2. Child based stroke knowledge/preparedness over the course of the study (n=3070).
| Continuous (Knowledge/preparedness score) | Binary (1=Answered all questions correctly) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | Std. Err. | p-value | Estimate | Std. Err. | p-value | ||||||
| Intercept | 3.4581 | 0.1265 | <0.0001 | -4.7356 | 0.3659 | <0.0001 | |||||
| Intervention | 2.7135 | 0.1736 | <0.0001 | 4.9983 | 0.4470 | <0.0001 | |||||
| Test | 0.1721 | 0.0304 | <0.0001 | 0.5074 | 0.1407 | 0.0003 | |||||
| Intervention by test | 0.9298 | 0.0400 | <0.0001 | 0.7870 | 0.1671 | <0.0001 | |||||
| Quadratic test | -0.0973 | 0.0513 | 0.0579 | 0.0890 | 0.2659 | 0.7380 | |||||
| Intervention by quadratic test | -1.5871 | 0.0659 | <0.0001 | -2.7903 | 0.2863 | <0.0001 | |||||
| Control | Intervention | Control | Intervention | ||||||||
| N | Mean | Std. Err. | N | Mean | Std. Err. | Mean | Std. Err. | Mean | Std. Err. | ||
| Pre-Test | Observed | 1414 | 3.16 | (0.17) | 1656 | 3.38 | (0.09) | 0.01 | (0.01) | 0.02 | (0.01) |
| Model Based | 1414 | 3.19 | (0.12) | 1656 | 3.39 | (0.12) | 0.01 | (0.00) | 0.02 | (0.01) | |
| Immediate Post-Test | Observed | 1061 | 3.37 | (0.14) | 1374 | 6.18 | (0.07) | 0.01 | (0.01) | 0.56 | (0.03) |
| Model Based | 1061 | 3.46 | (0.13) | 1374 | 6.17 | (0.12) | 0.01 | (0.00) | 0.57 | (0.06) | |
| 3-Month follow-up | Observed | 915 | 3.47 | (0.14) | 1212 | 5.59 | (0.13) | 0.03 | (0.01) | 0.24 | (0.04) |
| Model Based | 915 | 3.53 | (0.13) | 1212 | 5.59 | (0.12) | 0.02 | (0.01) | 0.24 | (0.05) | |
Non-linear models predicting stroke preparedness, adjusted for clustering within school and heterogeneity in group and residual variances.
Sensitivity analysis for children's data including respondents with at least 2 waves of data was conducted using a mixed model approach that was the same as that of the intent to treat analysis (the covariance structure was unstructured, with heterogeneous group variances, and school treated as a random effect). A total of 281 cases were excluded (102 in the intervention group and 179 in the control group). The estimates were similar to those from the intent-to-treat analyses for both continuous and binary outcomes. For example, for the continuous outcome, the estimates of the fixed effects for the intent-to-treat and at least 2 wave analyses respectively are as follows. Intercept: 3.46 vs 3.45, intervention group: 2.71 vs 2.72, test: 0.17 vs 0.19, intervention group by test: 0.93 vs 0.91, intervention group by quadratic test: -1.59 vs -1.57, all with a p-value <0.0001 (online supplemental Table II).
Parents Knowledge/Preparedness (H1, H2a)
There were no significant differences in stroke preparedness between control and intervention groups at baseline (H1). Model based means from the analyses of the binary outcome (H2a) showed that 17% (95% CI: 13-20%) of parents in the control and 19% (95% CI: 16-23%) in the intervention group demonstrated optimal stroke preparedness, and this increased to 29% (95% CI: 24-34%) immediately after the program in the intervention group as contrasted with 21% (95% CI: 17-25%) in controls. However, endpoint differences were less (21% in controls and 24% in the intervention; P=0.0892). The observed and model based means were similar. Treated as a continuous knowledge measure, and examined over the three time-points, the intervention group evidenced significantly greater gains in preparedness relative to the controls (P=0.0012). The model-based mean differences were two points on a 7 point scale. Thus the effect was an average of 3.5/7 (50% correct) vs. 5.6/7 (80%), a significant and clinically important difference.
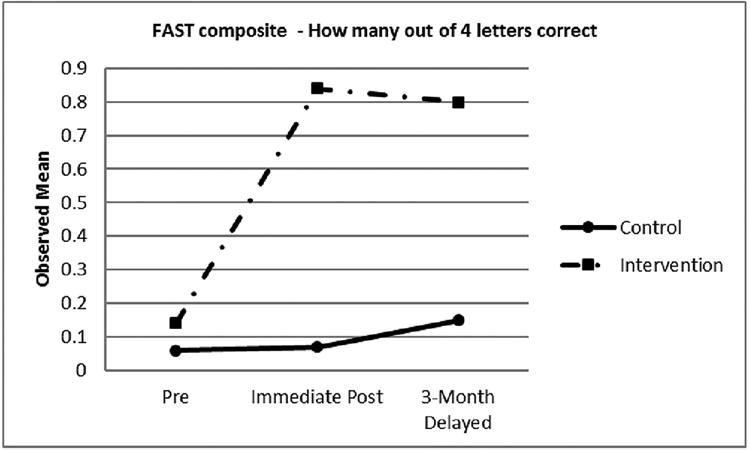
Parents FAST literacy (H2a)
Model based means for the binary FAST outcome (H2a) showed that only 3% (95% CI: 2-4%) of parents in the intervention could identify all letters of the FAST acronym at baseline but this increased to 20% at immediate post-test (95% CI: 16-24%) and 17% at the 3-months delayed post-test (H2: 95% CI: 13-21%, P=0.0062), while no significant changes were observed in controls (see Table 3 and Figure 2). The observed and model based means were similar.
Table 3. Parent based stroke knowledge/preparedness over the course of the study (n=1144).
| Stroke Knowledge/preparedness | FAST Stroke Identification composite | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Continuous | Binary (1=Answered all questions correctly) |
Continuous | Binary (1=Answered all questions correctly) |
||||||||||||||||
| Estimate | Std. Err. | p-value | Estimate | Std. Err. | p-value | Estimate | Std. Err. | p-value | Estimate | Std. Err. | p-value | ||||||||
| Intercept | 5.5321 | 0.0642 | <0.0001 | -1.3130 | 0.1448 | <0.0001 | 0.0699 | 0.0236 | 0.0077 | -4.2877 | 0.4216 | <0.0001 | |||||||
| Intervention | 0.3254 | 0.0854 | 0.0001 | 0.4277 | 0.1962 | 0.0293 | 0.7636 | 0.0763 | <0.0001 | 2.8931 | 0.4376 | <0.0001 | |||||||
| Test | 0.1465 | 0.0340 | <0.0001 | 0.1602 | 0.0759 | 0.0349 | 0.0437 | 0.0189 | 0.0209 | 0.5126 | 0.2718 | 0.0595 | |||||||
| Intervention by test | -0.0296 | 0.0462 | 0.7792 | -0.0312 | 0.1037 | 0.7632 | 0.2802 | 0.0467 | <0.0001 | 0.4522 | 0.3023 | 0.1348 | |||||||
| Quadratic test | -0.0135 | 0.0494 | 0.7844 | -0.1425 | 0.1130 | 0.2074 | 0.0322 | 0.0227 | 0.1554 | 0.1521 | 0.4449 | 0.7326 | |||||||
| Intervention by quadratic test | -0.2200 | 0.0680 | 0.0012 | -0.2613 | 0.1537 | 0.0892 | -0.4027 | 0.0705 | <0.0001 | -1.2975 | 0.4739 | 0.0062 | |||||||
| Control | Intervention | Control | Intervention | Control | Intervention | Control | Intervention | ||||||||||||
| N | Mean | Std. Err. | N | Mean | Std. Err. | Mean | Std. Err. | Mean | Std. Err. | Mean | Std. Err. | Mean | Std. Err. | Mean | Std. Err. | Mean | Std. Err. | ||
| Pre-Test | Observed | 527 | 5.37 | (0.06) | 617 | 5.50 | (0.09) | 0.17 | (0.02) | 0.20 | (0.02) | 0.06 | (0.02) | 0.14 | (0.04) | 0.01 | (0.01) | 0.03 | (0.01) |
| Model Based | 527 | 5.37 | (0.06) | 617 | 5.49 | (0.06) | 0.17 | (0.02) | 0.19 | (0.02) | 0.06 | (0.02) | 0.14 | (0.03) | 0.01 | (0.00) | 0.03 | (0.01) | |
| Immediate Post-Test | Observed | 430 | 5.55 | (0.05) | 457 | 5.88 | (0.06) | 0.21 | (0.02) | 0.30 | (0.03) | 0.07 | (0.02) | 0.84 | (0.08) | 0.01 | (0.01) | 0.20 | (0.02) |
| Model Based | 430 | 5.53 | (0.06) | 457 | 5.86 | (0.06) | 0.21 | (0.02) | 0.29 | (0.02) | 0.07 | (0.02) | 0.83 | (0.07) | 0.01 | (0.01) | 0.20 | (0.02) | |
| 3-Month follow-up | Observed | 250 | 5.70 | (0.06) | 286 | 5.78 | (0.05) | 0.23 | (0.03) | 0.26 | (0.03) | 0.15 | (0.04) | 0.80 | (0.07) | 0.03 | (0.01) | 0.17 | (0.02) |
| Model Based | 250 | 5.67 | (0.07) | 286 | 5.76 | (0.06) | 0.21 | (0.03) | 0.24 | (0.03) | 0.15 | (0.04) | 0.79 | (0.08) | 0.03 | (0.01) | 0.17 | (0.02) | |
Non-linear models predicting stroke preparedness, adjusted for clustering within school and heterogeneity in group and residual variances.
Figure 2.
Self-efficacy increased significantly across all subconstructs (P<.0001; not shown) relative to controls.
Sensitivity analysis for parental knowledge/preparedness data using respondents with at least 2 waves of data was conducted using a mixed model approach that was the same as that of the intent to treat analysis (the covariance structure was unstructured, with heterogeneous group variances, and school treated as a random effect). A total of 257 cases were excluded (160 in the intervention group and 97 in the control group). The estimates were similar to those from the intent-to-treat analyses for both continuous and binary outcomes. For example, for the continuous outcome, the estimates of the fixed effects for the intent-to-treat and at least 2 wave analyses, respectively are as follows. Intercept: 5.53 vs 5.55, intervention group: 0.33 vs 0.33, test: 0.15 vs 0.14, intervention group by quadratic test: -0.22 vs -0.21, all with p-values <0.002 (online supplemental Table III).
Covariates
Although 61% of parents reported stroke experience at both pre-test and post-test, we found no association between this and stroke preparedness. Additionally, health literacy and barriers to calling 911 were not associated significantly with stroke preparedness.
Sharing and Mediation
There was an intervention effect for information sharing (H3). The results (adjusted for clustering) were that among the control group, 42% reported sharing information as contrasted with 81% of the intervention group (P<0.0001). Over time, parental stroke preparedness scores in the intervention group whose children shared stroke information (H4) with them showed greater increase than intervention parents whose children did not share stroke information (stroke preparedness items, P=0.0183; FAST composite, P=0.0019; data not shown). The model-based means for the parental preparedness test for the intervention group whose children shared information increased from 5.60 to 5.96, as contrasted with those who shared information in the control group (5.52 to 5.68). The comparable data for the FAST were 0.20 to 1.11 (intervention) and 0.07 to 0.10 (control).
We found no significant mediation effect (H4M) of child stroke preparedness scores and prevention knowledge on parental stroke preparedness scores and prevention knowledge (online supplement Figure II).
Stroke Events (secondary aim)
We performed a total of 315 stroke event interviews on parents (200 intervention and 115 control) over a three-year follow-up period. We found 27 (8.6%) self-reported stroke events affecting a family member, with 18 in the intervention (9%) and 9 in the control group (8%). EMS activation occurred in 14/18 cases (77%) in the intervention group and 6/9 (66%) cases in the control group. Due to the low number of events, we were unable to draw meaningful conclusions from these data. However, four children, all in the intervention group, called 911 for stroke events, in one case overruling a parent's wait-and-see approach.
Discussion
This randomized controlled trial of a school-based stroke education program showed significant and relatively large gains in stroke preparedness for both parents and children that were sustained over at least three months. Using our definition of optimal stroke knowledge/preparedness (perfect scores), it was estimated that 24% of school children aged 9-12 years exposed to the HHS intervention as contrasted with 2% of those who were not exposed became and remained stroke prepared at 3 months. HHS children demonstrated high self-efficacy for stroke recognition, calling 911, describing stroke event to a 911 operator, and teaching their parents about stroke. Although we did not find a mediation effect between children's stroke preparedness scores and their parent's stroke preparedness scores, parents of children who shared stroke information with them showed greater increase in stroke preparedness over time than parents whose children did not share stroke information, supporting our “transmission vector” hypothesis. Overall, parents showed an increase in stroke knowledge/preparedness at immediate post-intervention, followed by a decline toward pretest values after three months, which nonetheless remained greater for the intervention than control parents. Although greater missing data at three months was observed for the parents (53.15%) in contrast to children (30.72%), non-linear models for average change over time were significant in the direction of significantly greater estimated stroke knowledge/preparedness in both intervention groups relative to the control group. Moreover, significant gains in FAST literacy were observed among parents in the intervention group, and this persisted at three months. Translated into real-world gains in stroke preparedness, for every 100 parents whose children are exposed to the HHS intervention, 14 additional parents will pass the FAST literacy test with a perfect score.
Beside these cognitive effects, four intervention children called 911 for real-life stroke occurrences among family members. These cases, combined with an additional two cases reported in our pilot studies23, although few in number (n = 6), show that our intervention not only improves stroke preparedness of children, it can also translate into behavior change. We note that in our collective experience at a major New York City stroke center, it is highly unusual for preadolescent children to be a family leader in making decisions to call 911 for a recognized stroke.
One systematic literature review of school-based stroke interventions included 12 studies, which provided data on 3,312 children and 612 parents24. The authors found a single RCT (the second RCT reported was an interim analysis of the same study), which enrolled older children in 6th, 7th, and 8th grades25. Unfortunately, this study did not analyze parental data due to low parental participation (17% or 77/462 parents completed testing). The systematic review also found a lack of data supporting the ability of stroke-educated children to recognize and respond appropriately to stroke in the real world, and in their ability to transfer stroke knowledge to the parents24. A subsequent school-based RCT involved an intervention delivered to 8th graders (adolescents) by a neurologist in the form of a stroke lecture26. Encouragingly, the authors provided evidence supporting the ability of these children to transfer stroke information to parents, although psychometric data on their stroke knowledge instrument was not presented. The current trial, which to the best of our knowledge is the largest of its kind to date, targets preadolescent children through Lay Health Facilitators equipped with culturally tailored multimedia that can be accessed for free online. It may therefore represent a more scalable approach.
Limitations
We had significant parental attrition over time with similar dropout rates in both arms, but maintained statistical power for the FAST outcome due to our large sample size. Sensitivity analyses examining only those respondents with at least two waves of data yielded estimates very close to those found in the primary intent-to-treat analyses of all respondents. These challenges reflect the practical problems of parental recruitment and retention in school-based studies; especially those targeting schools within economically disadvantaged communities. We did track and model gains in parental stroke preparedness relative to child engagement in family stroke preparedness conversations, however the exact “dose” of each child's engagement cannot be determined. Regarding stroke events, we were severely underpowered to detect meaningful differences, although this was a secondary outcome. Notwithstanding, our observations suggest that stroke-educated children aged 9-12 years can recognize stroke and appropriately call 911 in the real world.
Conclusion
Children may be underutilized conduits for reaching economically disadvantaged ethnic minorities with critical stroke information. Hip Hop Stroke may represent an effective intergenerational alternative to mass media campaigns and may be used to support annual public stroke education requirements for stroke center certification in the United States.
Supplementary Material
Acknowledgments
Authors thank Luisa Chan, Janhavi Mallaiah, Alexandra Desorbo Quinn, Monique Hedmann, Mindy Hecht, Adrian Harris, Amparo Abel-Bey, and Madeleine Gordillo for research coordination; Rachel Shelton and Lisa Metsch for their help with conceptual framework development; Morgan Metsch for data collection efforts; Doug E Fresh and Artie Green for song development; and Bill Davis and Ian James for cartoon development.
Sources of Funding: Authors were supported by the National Institute of Neurological Disorders and Stroke 1R01NS067443-01A1 (PI: Olajide Williams)
Footnotes
Clinical Trial Registration: https://clinicaltrials.gov/ct2/show/NCT01497886
Disclosures: Authors have no conflicts of interests to disclose
References
- 1.Tong D, Reeves MJ, Hernandez AF, et al. Times from symptom onset to hospital arrival in the Get with the Guidelines--Stroke Program 2002 to 2009: temporal trends and implications. Stroke. 2012;43:1912–1917. doi: 10.1161/STROKEAHA.111.644963. [DOI] [PubMed] [Google Scholar]
- 2.Schwamm LH, Ali SF, Reeves MJ, et al. Temporal trends in patient characteristics and treatment with intravenous thrombolysis among acute ischemic stroke patients at Get With The Guidelines-Stroke hospitals. Circulation Cardiovascular quality and outcomes. 2013;6:543–549. doi: 10.1161/CIRCOUTCOMES.111.000303. [DOI] [PubMed] [Google Scholar]
- 3.Schwamm LH, Reeves MJ, Pan W, et al. Race/ethnicity, quality of care, and outcomes in ischemic stroke. Circulation. 2010;121:1492–1501. doi: 10.1161/CIRCULATIONAHA.109.881490. [DOI] [PubMed] [Google Scholar]
- 4.Investigators CASPR. Prioritizing interventions to improve rates of thrombolysis for ischemic stroke. Neurology. 2005;64:654–659. doi: 10.1212/01.WNL.0000151850.39648.51. [DOI] [PubMed] [Google Scholar]
- 5.Robinson TG, Reid A, Haunton VJ, Wilson A, Naylor AR. The face arm speech test: does it encourage rapid recognition of important stroke warning symptoms? Emergency medicine journal : EMJ. 2013;30:467–471. doi: 10.1136/emermed-2012-201471. [DOI] [PubMed] [Google Scholar]
- 6.Rasura M, Baldereschi M, Di Carlo A, et al. Effectiveness of public stroke educational interventions: a review. European journal of neurology. 2014;21:11–20. doi: 10.1111/ene.12266. [DOI] [PubMed] [Google Scholar]
- 7.Wein TH, Staub L, Felberg R, Hickenbottom SL, Chan W, Grotta JC, et al. Activation of emergency medical services for acute stroke in a nonurban population: the T.L.L. Temple Foundation Stroke Project. Stroke. 2000;31:1925–1928. doi: 10.1161/01.str.31.8.1925. [DOI] [PubMed] [Google Scholar]
- 8.Hayslip B, Kaminski PL. Grandparents raising their grandchildren: a review of the literature and suggestions for practice. The Gerontologist. 2005;45:262–269. doi: 10.1093/geront/45.2.262. [DOI] [PubMed] [Google Scholar]
- 9.Williams O, Leighton-Herrmann E, DeSorbo A, Hecht M, Hedmann M, Huq S, Gerin W, Chinchilli V, Ogedegbe G, Noble J. Hip Hop Stroke: Study Protocol for a Randomized Controlled Trial to Address Stroke Literacy. Journal of clinical trials. 2015;5:242. doi: 10.4172/2167-0870.1000242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Williams O, Leighton-Herrmann E, Hecht MF, DeSorbo AL, Gerin W, et al. Child-mediated Health Communication: A Conceptual Framework for Increasing Stroke Literacy in Hard to Reach Populations. Journal of Health Disparities Research and Practice. 2016;9 [Google Scholar]
- 11.Krugman HE. Why Three Exposures May Be Enough. Journal of Advertising Research. 1972;12:11–14. [Google Scholar]
- 12.Billings-Gagliardi S, Mazor KM. Development and validation of the stroke action test. Stroke. 2005;36:1035–1039. doi: 10.1161/01.STR.0000162716.82295.ac. [DOI] [PubMed] [Google Scholar]
- 13.Greenlund KJ, Neff LJ, Zheng ZJ, Keenan NL, Giles WH, et al. Low public recognition of major stroke symptoms. American journal of preventive medicine. 2003;25:315–319. doi: 10.1016/s0749-3797(03)00206-x. [DOI] [PubMed] [Google Scholar]
- 14.Kothari RU, Pancioli A, Liu T, Brott T, Broderick J. Cincinnati Prehospital Stroke Scale: reproducibility and validity. Annals of emergency medicine. 1999;33:373–378. doi: 10.1016/s0196-0644(99)70299-4. [DOI] [PubMed] [Google Scholar]
- 15.Kleindorfer DO, Miller R, Moomaw CJ, Alwell K, Broderick JP, Khoury J, et al. Designing a message for public education regarding stroke: does FAST capture enough stroke? Stroke. 2007;38 doi: 10.1161/STROKEAHA.107.484329. [DOI] [PubMed] [Google Scholar]
- 16.Wolters FJ, Paul NL, Li L, Rothwell PM, Oxford Vascular S. Sustained impact of UK FAST-test public education on response to stroke: a population-based time-series study. International journal of stroke : official journal of the International Stroke Society. 2015;10:1108–1114. doi: 10.1111/ijs.12484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the newest vital sign. Annals of family medicine. 2005 Nov-Dec;3:514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Revelle W. Psych: Procedures for Psychological, Psychometric and Personality Research; R package version 1.7.8. Northwestern University; Evanston, IL, USA: 2017. [Google Scholar]
- 19.SPSS: IBM Corp. Version 23.0. Armonk, NY: IBM Corp; Released 2013. IBM SPSS Statistics for Windows. [Google Scholar]
- 20.SAS Institute Inc. SAS Version 9.4. Cary, NC: SAS Institue Inc; 2012. [Google Scholar]
- 21.Sullivan LM. Repeated measures Circulation. 2008;117:1238–1243. doi: 10.1161/CIRCULATIONAHA.107.654350. [DOI] [PubMed] [Google Scholar]
- 22.Schwarz G. Estimating the Dimensions of a Model. The Annals of Statistics. 1978;6:461–464. [Google Scholar]
- 23.Williams O, Noble JM. ‘Hip-hop’ stroke: a stroke educational program for elementary school children living in a high-risk community. Stroke. 2008;39:2809–2816. doi: 10.1161/STROKEAHA.107.513143. [DOI] [PubMed] [Google Scholar]
- 24.Beal CC, Flander SA, Bader SG. Can Children Reduce Delayed Hospital Arrival for Ischemic Stroke?: A Systematic Review of School-Based Stroke Education. Journal of Neuroscience Nursing. 2016;48:E2–E13. doi: 10.1097/JNN.0000000000000202. [DOI] [PubMed] [Google Scholar]
- 25.Morgenstern LB, Gonzales NR, Maddox KE, et al. A randomized, controlled trial to teach middle school children to recognize stroke and call 911: the kids identifying and defeating stroke project. Stroke Nov. 2007;38:2972–2978. doi: 10.1161/STROKEAHA.107.490078. [DOI] [PubMed] [Google Scholar]
- 26.Marto JP, Borbinha C, Filipe R, Calado S, Viana-Baptista M. Impact of stroke education on middle school students and their parents: A cluster randomized trial. International journal of stroke : official journal of the International Stroke Society. 2017;12:401–411. doi: 10.1177/1747493016677980. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


