Abstract
Objective
Behavioral therapies are first line treatments for preschoolers with ADHD. Studies support yoga as an intervention for school age children with ADHD; this study evaluated the effects of yoga in preschoolers on parent and teacher rated attention/challenging behaviors; attentional control (KiTAP); and heart rate variability (HRV).
Methods
This randomized waitlist-controlled trial tested a 6-week yoga intervention in preschoolers with ≥ 4 ADHD symptoms on the ADHD Rating Scale-IV Preschool Version. Group 1 (n=12) practiced yoga first; Group 2 (n=11) practiced yoga second. We collected data at four time points: baseline, T1 (6 wk), T2 (12 wk), follow-up (3 mo after T2).
Results
At baseline, there were no significant differences between Group 1 and 2 on any measure. At T1, Group 1 had faster reaction times on the KiTAP Go/No go task (p=.01, 95% CI: −371.1, −59.1, d=−1.7), fewer Distractibility errors of omission (p=.009, 95% CI: −14.2, −2.3, d=−1.5), but more commission errors (p=.02, 95% CI:1.4, 14.8, d=1.3) than Group 2. Children in Group 1 with more severe symptoms at baseline showed improvement at T1 not seen in Group 2 on parent-rated Strengths and Difficulties Questionnaire hyperactivity-inattention (β=−2.1, p=.04, 95% CI: −4.0, −0.1) and inattention on the ADHD Rating Scale (β=−4.4, p=.02, 95% CI: −7.9, −0.9). HRV measures did not differ between groups.
Conclusions
Yoga was associated with modest improvements on an objective measure of attention (KiTAP) and selective improvements on parent ratings. Yoga may be a promising treatment for ADHD symptoms in preschoolers.
Keywords: ADHD, Yoga, Preschool
INTRODUCTION
Attention Deficit Hyperactivity Disorder (ADHD) is a common and impairing neurodevelopmental disorder, occurring in up to 7% of children and adolescents1. Core symptoms include inattention, hyperactivity and impulsivity. ADHD is also associated with impaired self-regulation and decision making leading to negative educational outcomes1. ADHD symptoms often emerge in preschool age children and can be associated with similar behavioral, social, and cognitive impairments as seen in older children with ADHD1. These ADHD symptoms persist beyond preschool for 70-80% of children1. ADHD symptoms are associated with poor outcomes across the life span: academic and/or occupational difficulties, trouble maintaining friendships and other relationships, criminality, and substance use1. In preschool aged children, the American Academy of Pediatrics recommends evidence based behavioral therapy as first line treatment2. Common behavioral interventions include parent education, visual schedules, and classroom accommodations.
Exercise and mindfulness practices (e.g. meditation) may be beneficial for school age children with ADHD3,4. Aerobic exercise improves parent and/or teacher ratings of childhood ADHD symptoms, executive function, sustained attention, disruptive behaviors and response inhibition3. Emerging evidence suggests that physical exercise may be associated with more sustained improvements in ADHD than medications and/or behavioral interventions3. Physical exercise game instruction has also been successful in decreasing ADHD severity in preschoolers on parent and teacher rating scales5. An additional benefit of implementing these games at home included enhancement of parent-child relationships5.
Similar to benefits associated with exercise for ADHD, there is preliminary evidence of mindfulness training as a complementary form of therapy for ADHD. In school age children with ADHD, mindfulness training in conjunction with similar parent training resulted in decreased parent ratings of ADHD behaviors, increased mindful awareness in children, and decreased parenting stress and over-reactivity4. A review of mindfulness-based interventions in typical preschoolers described improved self-control via observer ratings and executive functioning performance after ten hours of Integrated Body-Mind Training6. Another study in typical preschoolers found improvements in teacher ratings of social competence and higher grades in social-emotional development after 12-weeks of mindfulness training7. Notably, baseline functioning moderated treatment effects – children with initially lower social competence and executive functioning demonstrated larger gains in social competence than controls7.
Yoga is a form of movement meditation that incorporates physical postures/poses, breathing practices, and meditation to hone self-regulation skills within the body and mind8. Yoga thus combines physical exercise and mindfulness. Prior studies evaluating the effects of yoga demonstrated promising results for school age children with ADHD, including improved parent and/or teacher rating scales9–12, and clinician completed rating scales13. Yoga improved attention via on-task attention10 and direct observations of “time on task”12. Parents who practiced yoga with their children reported better management of their own stress and improved parent-child relationships11. Promising evidence for the use of yoga with typically developing preschoolers is emerging. Significant gains in self-regulation, particularly for children with low baseline levels of self-regulation were found via direct assessment in children who received a yearlong daily school yoga intervention versus controls14.
Physiology may also be affected by yoga, such as vagal tone, which appears to improve in adults who practice yoga15. Heart rate variability (HRV), a measure of the beat-to-beat changes in heart rate, reflects the activity of the vagus nerve16. Degree of HRV is associated with physiologic resiliency, self-regulatory capacity and performance on tasks of executive function16. Compared to healthy controls, children with ADHD have higher mean heart rates and, unmedicated, have significantly lower HRV17.
The primary aims of this study were to explore the efficacy of practicing yoga for 6 weeks on behavioral symptoms, attentional control, and HRV. The secondary aim was to assess maintenance of the intervention effects over time. We hypothesized that participation in yoga for six weeks would lead to improvements in ADHD symptoms rated by parents and teachers, scores on attention tasks, and increases in HRV.
METHODS
Participants
Children 3 to 5 years of age with four or more ADHD symptoms rated by teachers or parents on the ADHD Rating Scale-IV Preschool Version18 (ADHD RS-IV Preschool Version) were recruited from a local urban, community-based preschool. We chose four or more symptoms as our cutoff to catch children at high-risk for ADHD, but did not require a diagnosis of ADHD, as it is often not diagnosed in preschoolers. Non-English-speaking children or those with a medical condition precluding them from safely participating in yoga were excluded. Recruitment included posting flyers at the preschool, and meeting with teachers and parents to discuss the study. This study was approved by the Institutional Review Board. Informed consent was obtained from the parents and teachers of the children enrolled.
Design
We conducted a mixed-methods randomized waitlist-controlled trial of a 6-week home and school based children’s yoga intervention. Behavioral symptoms were evaluated using two parent and teacher rating scales: ADHD RS-IV Preschool Version18 and Strengths and Difficulties Questionnaire19 (SDQ). Attention was measured via computer based tasks using the KiTAP20. We used heart rate variability (HRV) as a physiologic index of self-regulation16. Qualitative data were also collected via questionnaires and focus groups and/or interviews with parents, teachers, and the yoga instructors after each six-week yoga intervention (not included here).
To maximize the frequency of yoga the intervention occurred at home and school. During the 1st six weeks, students in Group 1 practiced school yoga in a separate room from their classroom, and completed home yoga with parent encouragement using a yoga DVD featuring the same protocol. Group 2 (wait-list control) continued their regular classroom and home activities without exposure to yoga. During the 2nd six weeks, the groups switched. Based on teacher feedback after the first 6-week intervention, school yoga for Group 2 was moved into the classroom as part of their morning routine; home yoga practice was the same. Group 1 stopped receiving school yoga (aside from three students in one classroom where school yoga was taught for Group 2, however they were not included in the analysis for Time 2). See Figure, Supplemental Digital Content 1, for the study timeline.
Rating scales, KiTAP scores and HRV were collected on the children at four time points: Baseline, Time 1 (Group 1 completed yoga), Time 2 (Group 2 completed yoga), and Follow-up (3 months after Time 2). Please refer to Figure 1, a participant flowchart from randomization through Follow-up, for details. During each intervention period the yoga teachers completed Time on Task ratings for each student after school yoga classes. They also completed Yoga Fidelity Measures after each yoga class. While participating in the intervention, parents completed Daily Yoga Logs via email or hard copy to determine the frequency of yoga practice for each child. After each six-week yoga intervention parents and teachers completed Perception and Satisfaction questionnaires.
Figure 1.
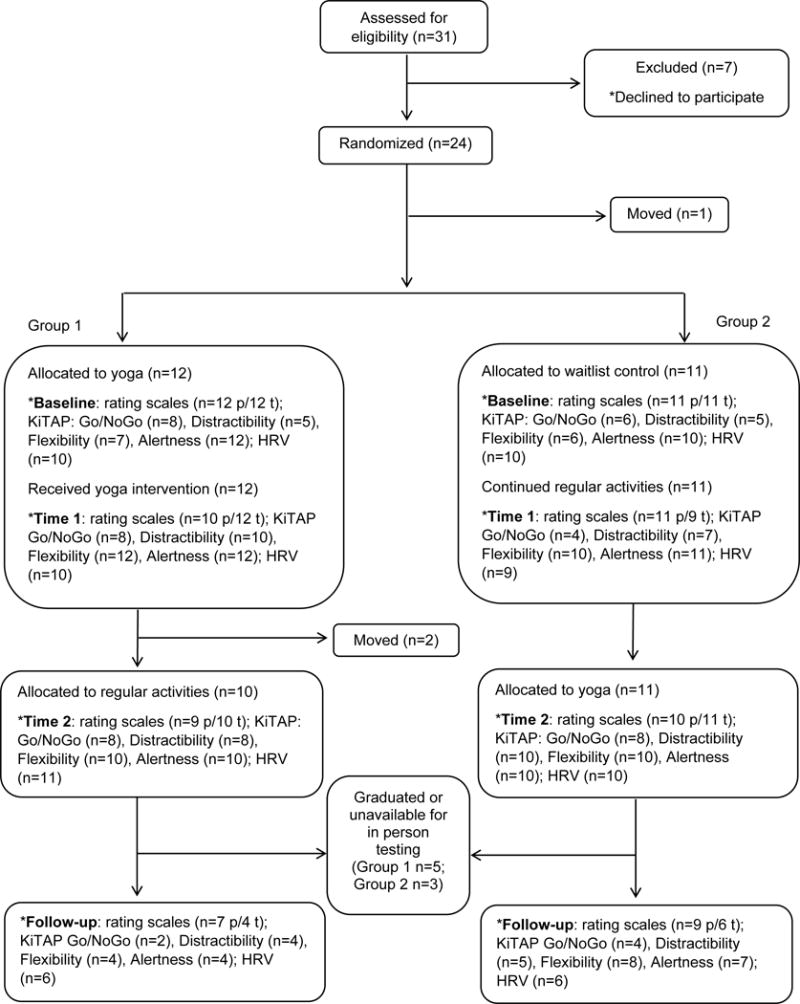
Participant flowchart of the study depicting both the number of children included in each group over the course of the study as well as the sample sizes (n) available for analysis of each outcome measure: parent (p) and teacher (t) rating scales, KiTAP subtests, and heart rate variability (HRV).
Intervention
School Yoga
Five months prior to starting the study two yoga instructors completed an intensive three-day training with Tiffany Gullberg, Owner and Founder of If I Was a Bird Yoga ™. Leading up to the study yoga teachers and assistants participated in monthly group practice sessions and more frequent home practice using yoga videos created for the study. During the study, thirty-minute group yoga sessions were held twice a week at the preschool, led by a trained children’s yoga instructors and 1-2 assistants, using a manualized curriculum from If I Was a Bird Yoga ™ (see Table, Supplemental Digital Content 2, for the protocol). The sequence of breathing exercises and poses was consistent over the six-week intervention. We created three themes (Ocean, Jungle, and Space Yoga Adventures) to help to keep the children engaged; each theme was implemented for two weeks.
During school yoga for Group 1 the children practiced away from the structure of their classroom. In this environment some children, especially those with significant hyperactive/impulsive symptoms, became disruptive (running, climbing, hitting), which resulted in being sent back to class to ensure the safety of the other children. Based on teacher feedback Group 2’s school yoga exercises were taught within the classroom setting along with typically developing peers, where classroom teachers and aides assisted in managing behaviors and enforcing rules.
Home Yoga
To maximize yoga practice parents were given a yoga DVD (also available online), featuring the same 30-minute yoga protocol themes. Home practice occurred on days the children did not practice at school. Children with persistent challenges participating in school yoga classes were asked to practice yoga daily at home, as some children complied better in more intimate settings.
Measures
Parent and Teacher Rating Scales
The ADHD RS-IV Preschool version includes 18 developmentally appropriate statements based on ADHD symptoms defined in DSM-IV-TR18. It includes Inattentive and Hyperactive/Impulsive subscales, and a total symptom scale. The scale screened and monitored response to the intervention.
The Strengths and Difficulties Questionnaire (SDQ) includes 25 developmentally appropriate statements divided into five subscales: Emotional Symptoms, Conduct Problems, Hyperactivity/Inattention, Peer Problems and Prosocial Behaviors19. There is a total difficulty score, and a prosocial scale score.
KiTAP Test of Attentional Performance for Children
The KiTAP20 is a computer administered child-friendly test with the theme of an enchanted castle. Four tasks (alertness, distractibility, flexibility, and go/no-go) are feasible to administer and reliable for a mental age of 3+ years, and are correlated with behavioral ratings of hyperactivity and attention21. We selected measures based on the manual or shown in previously published research to be reliable and valid21, including number of correct responses, total errors, omissions, and reaction times to correct responses. At each administration, the children were taught how to do each task, and given up to three practice tests. If more correct responses or equal numbers of correct responses and errors or omissions were achieved, the child completed the actual test, recorded by the computer. The test was considered invalid if the child persistently needed redirection to participate. At baseline, many children in both groups did not pass the practice tests or did not finish the actual test, resulting in insufficient data in either group to analyze at baseline. However, at subsequent times, sufficient numbers of children in both groups completed the full tests. Intermittent technical problems with the Go/No-Go task prevented the program from capturing data for some children: four at Baseline; seven at Time 1; three at Time 2; and five at Follow-up.
Heart rate variability (HRV)
The emWave® Coherence System by HeartMath measured HRV, using a photoplethysmography optical sensor placed on subjects’ earlobes. We used emWave to extract RR intervals and Kubios22 to analyze HRV data. Automated artifact correction was set at a threshold of 0.35 seconds. HRV indices of interest were the standard deviation of beat-to-beat intervals (SDNN), root mean square of successive differences (RMSSD), High Frequency (HF), and Low Frequency/High Frequency Ratio (LF/HF Ratio). Due to positive skew, HF HRV was log transformed prior to analyses. HRV was measured while the children listened to stories (resting condition) as well as during the KiTAP (an inhibitory control/attention task). The results presented will focus on HRV measured during the story.
Yoga Instructor Ratings
A 7 point Likert scale of Time on Task was rated by the yoga instructor and/or assistant for each student after school yoga classes (1=Never on task, 7=Always on task). At the end of each school yoga class they also completed Yoga Fidelity Measures based on the Yoga Study Protocol (see Table, Supplemental Digital Content 2, for the protocol) by crossing out poses or breathing exercises not completed.
Satisfaction and Perception Questionnaires
At the end of each six-week yoga intervention parents and teachers completed Satisfaction (Teacher 7/Parent 9 items) and Perception (Teacher 12/Parent 14 items) questionnaires. Some questions used semantic differential sliding scales between 0 - 100 (e.g., Not improved=0, and Greatly Improved=100); other questions were multiple choice.
Yoga Frequency
Parents completed Daily Yoga Logs via email or hard copy to determine the frequency of yoga practice for each child. The Daily Yoga Log included 1-2 multiple choice questions (Did your child practice yoga today? If not, what were the barriers to practicing?).
Statistical Analysis
Assuming pre/post correlations of 60%, our target sample size was 30 subjects per group to estimate treatment effects with margins of error of 0.41 standard deviations and provide 80% power (with 2-sided alpha=5%) to detect between-group effects as small as 0.59 standard deviations. However, we were only able to recruit 23 children (79% of the students eligible for the study). We were not able to expand the study to other preschools due to limitations in time and financial resources. With this sample size, assuming alpha=0.05 and a two-sided test, the minimum detectable difference with 82% power was 1.2 standard deviations. The primary assessment of treatment effects was estimated by comparing treatment and control groups on mean outcomes at Time 1 using analysis of covariance (ANCOVA) with the baseline values used as the covariate (when available). When the assumption of parallel groups was violated, an interaction between group and baseline values was included in the model. Secondary analyses included a within-group contrast to estimate the treatment effect in Group 2 (T2-T1) as well as an evaluation of treatment durability in Group 1 (follow-up – T1). If baseline data were unavailable (i.e., in analyses of the KiTAP), a t test was used to test differences between groups. Greek letters (e.g., β) are used to represent unstandardized model parameters. Feasibility and acceptability of the yoga intervention based on the Perceptions and Satisfaction questionnaires were analyzed using Wilcoxon rank sum tests. Data are presented as mean +/− standard deviation unless otherwise stated. Intention to treat analysis was implemented throughout. All analyses were conducted using SAS software, version 9.423 or R, version 3.2.224.
RESULTS
Demographics
A total of 23 students were recruited and randomized to Group 1 (yoga first; n=12) or Group 2 (waitlist control, yoga second; n=11). There were no differences between the groups based on their demographic data or baseline scores on the majority of outcome measures (Table 1). One child in Group 2 had autism spectrum disorder.
Table 1.
Demographic and baseline characteristics of the children and their parents by group.
| Child Demographics | Group 1 (n=12) | Group 2 (n=11) | p-value |
|---|---|---|---|
| Mean age in months ± SD | 52 ± 7 | 46 ± 10 | .14 |
| Male (raw count; %) | 8; 67 | 7; 64 | 1.00 ◆ |
| Not Hispanic (raw count; %) | 9; 90 | 7; 78 | .72 ◆ |
| Race (raw count; %) | 1.00 ◆ | ||
| Caucasian | 5; 42 | 5; 46 | |
| African American | 5; 42 | 4; 36 | |
| Asian | 0; 0 | 1; 9 | |
| Mixed | 1; 8 | 1; 9 | |
| Unknown | 1; 8 | 0; 0 | |
| Years preschool experience (raw count; %) | .58 ◆ | ||
| 1st year | 6; 55 | 8; 73 | |
| 2nd year | 2; 18 | 1; 9 | |
| 3rd year | 1; 9 | ||
| 4th year | 2; 18 | 0; 0 | |
| ADHD Diagnosis (raw count) | 1 | 1 | 1.00 |
| ADHD Medication (raw count) | 1 | 0 | 1.00 |
| Child Baseline Characteristics | |||
| SDQ – Parent rating (Mean ± SD)ˆ | |||
| Emotional Problems | 1.1 ± 0.8 | 3.0 ± 2.4 | .03 |
| Conduct Problems | 2.9 ± 1.8 | 3.5 ± 2.0 | .48 |
| Hyperactive-inattentive | 6.2 ± 2.5 | 4.5 ± 2.8 | .14 |
| Peer Problems | 1.5 ± 1.2 | 3.1 ± 2.9 | .13 |
| Prosocial | 7.4 ± 1.8 | 8.4 ± 1.8 | .22 |
| Total Score | 11.7 ± 4.4 | 14.1 ± 7.4 | .37 |
| SDQ – Teacher rating (Mean ± SD) | |||
| Emotional Problems | 0.6 ± 0.9 | 1.9 ± 2.0 | .07 |
| Conduct Problems | 4.1 ± 3.4 | 3.0 ± 3.7 | .47 |
| Hyperactive-inattentive | 7.0 ± 3.0 | 6.2 ±3.2 | .53 |
| Peer Problems | 1.8 ± 1.1 | 2.1 ± 2.5 | .76 |
| Prosocial | 5.8 ± 2.6 | 6.6 ± 1.6 | .39 |
| Total Score | 13.5 ± 5.4 | 13.2 ± 8.2 | .91 |
| ADHD – Parent rating (Mean ± SD)ˆ | |||
| Inattention | 8.4 ± 4.7 | 9.2 ± 4.8 | .70 |
| Hyperactivity | 13.3 ± 5.3 | 10.7 ± 5.7 | .28 |
| Total Score | 21.7 ± 9.1 | 19.9 ± 10.3 | .66 |
| ADHD – Teacher rating (Mean ± SD) | |||
| Inattention | 11.6 ± 6.8 | 11.9 ± 6.2 | .91 |
| Hyperactivity | 13.0 ± 8.7 | 12.5 ± 7.9 | .90 |
| Total Score | 24.6 ± 13.7 | 24.4 ± 12.4 | .98 |
| Heart rate variability (Mean ± SD) | (n=10) | (n=9) | |
| High frequency (ln) | 7.9 ± 0.8 | 7.5 ± 1.3 | .44 |
| RMSSD | 101.1 ± 24.6 | 90.8 ± 29.0 | .41 |
| SDNN | 97.4 ± 38.3 | 86.9 ± 45.6 | .59 |
| LF/HF ratio | 1.9 ± 1.7 | 1.5 ± 1.2 | .63 |
| Parent Demographics | |||
| Parent Age (raw count; %) | 1.00 ◆ | ||
| 18-24 years | 1; 8 | 1; 9 | |
| 25-34 years | 5; 42 | 4; 36 | |
| 35-44 years | 5; 42 | 6; 55 | |
| 45-54 years | 1; 8 | 0; 0 | |
| Parent Education (raw count; %) | 1.00 ◆ | ||
| High School or less | 3; 27 | 4; 36 | |
| Secondary education | 8; 73 | 7; 64 | |
| SES (raw count; %) | 1.00 ◆ | ||
| Preschool grant/voucher | 6; 55 | 6; 55 | |
| Tuition paying | 5; 46 | 5; 46 | |
| Caregivers in home (raw count; %) | 1.00 ◆ | ||
| One | 3; 33 | 3; 27 | |
| Two or more | 6; 67 | 8; 73 |
Note: Baseline KiTAP values are not included as there was not enough data to analyze meaningfully. One individual in Group 1 was American Indian/African American and one individual in Group 2 was Asian/African American.
Key:
Missing for one participant in Group 2; SDQ = Strengths and Difficulties Questionnaire; ADHD = ADHD Rating Scale-IV Preschool Version; RMSSD = root mean square of successive differences; SDNN = standard deviation of beat-to-beat intervals; LF/HF = low frequency/high frequency;
Fisher Exact Test.
Parent/Teacher Rating Scales
At baseline, there were no significant differences between the groups for parent-rated or teacher-rated scores on the ADHD Rating Scale-IV (ADHD RS-IV) Preschool Version. On the baseline Strengths and Difficulties Questionnaire (SDQ) subscales, Group 2 had significantly higher parent-rated Emotional problems (95% CI: −3.6, −0.2). Significant time effects were observed for the parent-rated SDQ total score (F=5.8, p=.008), teacher-rated SDQ conduct scale (F=4.9, p=.02), and teacher-rated inattention on the ADHD RS-IV (F=4.8, p=.02), but not for the other outcomes (F=0.2-2.9). Similarly, significant time by group interactions were observed for the parent-rated SDQ hyperactive-inattentive scale (F=5.2, p=.01), teacher-rated SDQ conduct scale (F=6.2, p=.007), teacher-rated SDQ prosocial scale (F=10.3, p<.001, and parent-rated inattention on the ADHD RS-IV (F=6.8, p=.004), but not for the other outcomes (F=0.3-2.5).
At Time 1, differences in mean rating scale scores between the groups depended on baseline scores for the parent-rated SDQ hyperactive-inattentive scale and inattention on the ADHD RS-IV. Particularly, children with parent-rated SDQ hyperactive-inattentive scale scores of 8.5 at baseline in Group 1 had 2 point lower ratings, on average, at Time 1 than similar children in Group 2 (β=−2.1, SE=1.0, p=.04, 95% CI: −4.0, −0.1). Similarly, children in Group 1 with baseline ADHD inattention score ratings of 17 had 4 point lower ratings at Time 1 than similar children in Group 2 (β=−4.4, SE=1.7, p=.02, 95% CI: −7.9, 0.9) (Figure 2). The total scores on both scales and the other subscales did not differ between the groups at Time 1.
Figure 2.
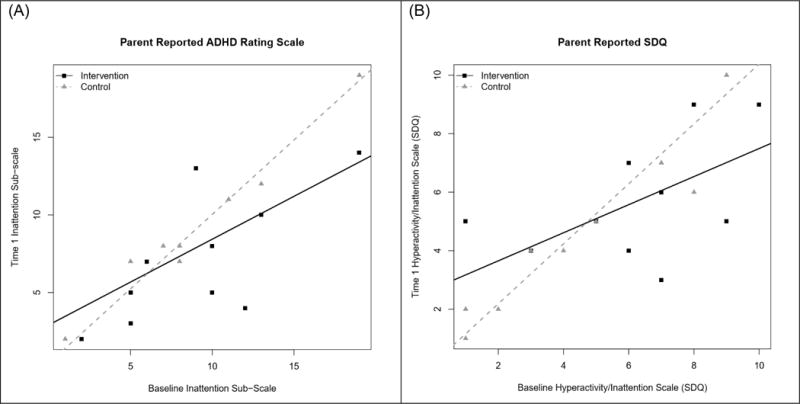
Parent reported behaviors on the Inattention sub-scale of the (A) ADHD Rating Scale IV Preschool version and (B) Hyperactivity/Inattention sub-scale of the Strengths and Difficulties Scales at baseline and Time 1.
Within Group 2, parent-rated SDQ total scores (β=−2.5, SE=0.7, p=.002, 95% CI: −4.0, 1.0) decreased after the yoga intervention (Time 2 – Time 1). However, scores on the parent-rated ADHD RS-IV hyperactivity subscale increased after yoga (β=2.2, SE=0.9, p=.03, 95% CI: 0.3, 4.1) in Group 2. There were no other differences observed in Group 2 after the intervention.
In Group 1, improvements noted for children with a baseline parent-rated SDQ hyperactive-inattentive score of 8.5 at Time 1 continued at the follow-up, with scores another 1.5 points lower, on average (β=−1.5, SE=0.4, p<.001, 95% CI: −2.2, −0.7). Although no effects of the yoga intervention were observed at Time 1 on the teacher-rated prosocial SDQ subscale, scores were higher (better on this scale) in Group 1 at follow-up than at Time 1 (β=1.3, SE=0.4, p=.003, 95% CI: 0.5, 2.1). No other differences were observed between follow-up and Time 1.
KiTAP Tasks of Attention
At Time 1, comparisons between Group 1 and 2 showed that Group 1 had faster reaction times for correct responses on the Go/No-Go subtest (t(12)=−3.0, p=.01, 95% CI: −371.1, −59.1, d=−1.7). The comparisons for the other subtests at Time 1 were not significantly different between the groups: Flexibility (t(20)=−2.0, p=.06, 95% CI: −1123.1, 12.8, d=−0.9), Alertness (t(21)=−2.0, p=.06, 95% CI: −509.1, 13.9, d=−0.9), Distractibility subtests (t(15)=−2.0, p=.07, 95% CI: −398.4, 15.1, d=−1.0). Group 1 also had fewer Distractibility omission errors at Time 1 (t(15)=−3.0, p=.009, 95% CI: −14.2, −2.3, d=−1.5), but also committed significantly more commission errors on the Distractibility subtest (t(15)=2.6, p=.02, 95% CI: 1.4, 14.8, d=1.3). Significant differences on commission errors were not found on other subtests. (Figure 3). No differences were found for variability of reaction times on the Alertness subtest or errors on the Flexibility subtest, ps > .58. Covarying for age or ADHD severity did not affect the significance of these results.
Figure 3.
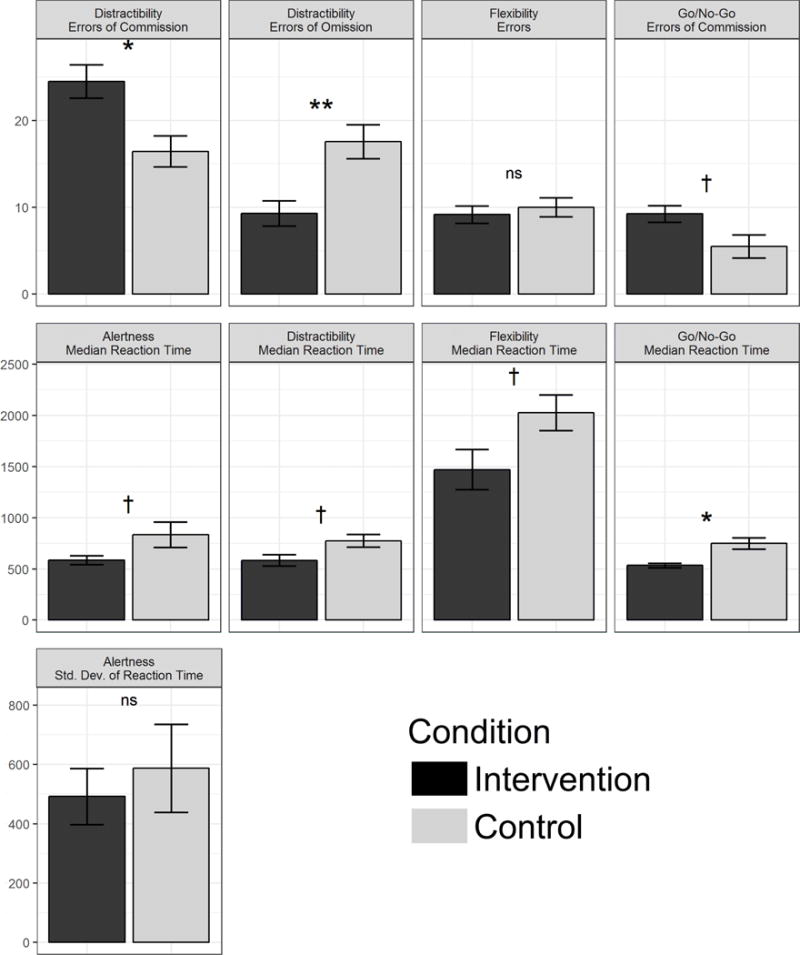
KiTAP performance at Time 1 (post-intervention for Group 1) significantly or marginally differed on numerous tests. For symmetry, Go/No-Go errors of omission were omitted from this figure; differences between groups on this task outcome were far from significant, p = .894.
Note: †p < .10, *p < .05, **p < .01, ns = nonsignificant.
Change scores for Group 2 (Time 2 – Time 1) were not significantly different. However, controlling for age at baseline led to some significant results. Specifically, there were significant improvements in Go/No-Go reaction times (β=−113.7, SE=47.0, p=.04, 95% CI: −223.9, −3.5). Comparisons on the Alertness subtest were not significantly different for reaction times (β=−148.4, SE=71.7, p=.07, 95% CI: −311.4, 14.5) or variability of reaction times (β=−215.7, SE=102.9, p=.06, 95% CI: −442.0, 10.6). Controlling for ADHD severity at baseline did not reveal significant improvements in Go/No-Go reaction time (β=−109.5, SE=47.6, p=.06, 95% CI: −222.0, 3.1), Alertness reaction time (β=−139.9, SE=70.1, p=.08, 95% CI: −297.5, 17.7), or Alertness variability in reaction times (β=−225.6, SE=104.9, p=.06, 95% CI: −458.2, 6.9).
We had insufficient data from Group 1 at follow-up to make any comparisons with confidence.
Heart Rate Variability (HRV)
At baseline there were no significant differences in HRV between Group 1 and Group 2 (ts < 0.84, ps > .41). At Time 1 (Fs < 1.84, ps > .19) and Follow-up (Fs < 0.59, ps > .43), none of the HRV measures we assessed significantly differed between groups, controlling for each respective measure at baseline. Similarly, within Group 2 after the yoga intervention (Time 2 – Time 1) none of the HRV measures we assessed significantly differed.
Yoga Instructor Ratings
Time on Task
Mean Time on Task ratings for Group 1 (3.9 ± 1.8) were similar to Group 2 (3.8 ± 1.2) indicating that on average students were rated as being “occasionally on task” during school yoga. Over the course of the intervention, mean Time on Task ratings remained stable in both groups (β=−0.02, p=.6, 95% CI: −0.08, 0.04). When considering ADHD symptoms, defined as the average of parent and teacher ADHD RS-IV ratings, children with higher symptoms on the total score or the hyperactive/impulsive and inattention subscales had lower Time on Task ratings initially (p<.05). Children with higher symptoms improved slightly over time, although this improvement was not statistically significant (see Figure, Supplemental Digital Content 3, for graphs). Children with symptom scores one standard deviation below the mean (low symptoms), declined in Time on Task over the course of the intervention (total ADHD rating: β=−0.08, p=.007, 95% CI=−0.15, −0.02; hyperactive/impulsive: β=−0.07, p=.006, 95% CI= −0.13, −0.02; inattention: β=−0.08, p=.01, 95% CI=−0.14, −0.02). Children with mean symptoms remained stable over time.
Fidelity
Each part of the school yoga classes were completed with rates of 63 -100%. The poses missed most often in both groups included: bird-dog, chair, airplane, and happy baby pose.
Satisfaction and Perception Questionnaires
Parent satisfaction and perception ratings were not significantly different between the groups. Many parents were satisfied with behavior changes they noticed after yoga (Group 1: 80 ± 23; Group 2: 67 ± 30), and felt learning yoga helped their children learn self-calming skills (Group 1: 85 ± 23 vs Group 2: 82 ± 20). Overall parent satisfaction with the program was promising (Group 1: 75 ± 39 vs Group 2: 72 ± 30), and most would recommend the program to others (Group 1: 74 ± 43 vs Group 2: 78 ± 32). In both groups, most parents did not perceive changes in their children’s appetite, sleeping patterns, mood and ability to handle transitions. Most parents also did not perceive changes in their stress level or parent-child relationships.
Teacher satisfaction and perception ratings were also not significantly different between the groups: behavioral improvements (Group 1: 28 ± 31 vs Group 2: 59 ± 25; p=0.10), teacher-student relationships (Group 1: 61 ± 16 vs Group 2: 64 ± 23), overall satisfaction with yoga (Group 1: 50 ± 22 vs Group 2: 78 ± 22; p=0.15). After each intervention teachers rated that they would recommend the program to others at similar rates (Group 1: 73 ± 22 vs Group 2: 78 ± 22).
Yoga Frequency
There were 42 possible days to practice yoga during each intervention period. Overall the children in both groups practiced yoga about 50% of the possible days (mean days of practice: Group 1: 25 ± 14; Group 2: 20 ± 8), which averaged to 3-4 days of yoga per week. None of the parents reported continuing to practice home yoga after their intervention period ended.
DISCUSSION
In our study, yoga led to modest improvements on selective parent ratings of ADHD symptoms and an objective measure of attention, but not our physiological measure (heart rate variability). Parent ratings of inattentive symptoms on the ADHD Rating Scale-IV (ADHD RS-IV) Preschool Version and hyperactive-inattentive symptoms on the Strengths and Difficulties Questionnaire (SDQ) were significantly improved on average after yoga for children with high baseline scores. These results raise questions regarding which type of ADHD symptoms respond best to yoga. Published theories about the underlying mechanisms of yoga draw connections between yoga and increases in mind-body awareness that lead to improvements in attention25. Thus, inattentive symptoms may selectively decrease after practicing yoga, as seen in our study for children with higher baseline inattention symptoms. However, it is important to note that teacher’s ratings of inattentive symptoms did not significantly improve after practicing yoga. This may be because teachers are trying to manage a busy classroom and are less likely to notice inattentive symptoms, as these symptoms are generally not disruptive. This is likely the same reason that children with predominantly inattentive symptoms are diagnosed with ADHD at school age26, once inattention begins to affect academic achievement. These results also suggest that children with more significant symptoms at baseline and/or children with inattentive symptoms show more dramatic improvements after practicing yoga. These finding are consistent with the study of yoga in typically developing preschoolers which found that children with less self-regulation skills benefited most from yoga14. At follow-up parents did not report continued yoga practice, however children in Group 1 with higher baseline scores had continued improvements, on average, on parent ratings of SDQ hyperactive-inattentive scores, indicating that practicing yoga may have some lasting benefits. This is consistent with finding from the MTA Study regarding behavioral therapies27. They found when behavioral therapies for ADHD are discontinued ADHD symptoms remain stable due to generalization of the practices learned, whereas when ADHD medications are discontinued symptoms generally worsen but do not return to baseline27.
Using the KiTAP, an objective measure of attention, we found that children in Group 1 displayed improved attention with significantly better reaction times on correct responses for the Go/No-Go task and fewer omissions on the Distractibility task after the intervention than children in the waitlist condition. Unexpectedly, at Time 1, Group 1 showed higher impulsivity after yoga with significantly more commission errors on the Distractibility task. Thus, although children evidenced improved sustained attention after the intervention, they also evidenced greater impulsivity on this computerized measure. We were not able to account for baseline scores on the KiTAP due to insufficient data, however we feel that these findings are still notable, and support our hypothesis that yoga improves attention. The scores on the KiTAP tasks align with the parent ratings, although were not limited to children with more severe ADHD symptoms.
When we controlled for age, Group 2 also evidenced faster reaction times on correct responses for the Go/NoGo task after yoga. Limited data were available to analyze for both groups at follow up due to preschool graduation or changes in preschool.
None of the measures of HRV displayed significant differences between groups at baseline, Time 1, or within Group 2 at Time 2, which could be related to our small sample size and short intervention period.
On average, both groups were rated as being “occasionally on task” for school yoga sessions over the six weeks. The poses most often missed in both groups required significant balance and coordination. In future studies these poses could be excluded or taught gradually, allowing time to build the balance and coordination required.
Based on the parent and teacher satisfaction questionnaires, both parents and teachers were satisfied with the intervention. Change in location of school yoga introduced variation in instruction between groups, although the yoga itself did not change. This variation did not lead to significantly different ratings of satisfaction, but teachers verbalized to us that the school yoga worked better within the classroom, which may be helpful for planning future research in the preschool setting.
The findings of our study are similar to the findings of Jensen and Kenny (2004) who performed a randomized control crossover study of the effects of yoga in school age boys with ADHD and found improvements on the parent rating scales but not teacher rating scales9. Harrison (2004) also found improvements on parent ratings, but did not include teacher ratings in their study11, and Haffner et al (2006) found improvements on parent but not teacher ratings10. Mehta et al (2012) found improvements on both parent and teacher ratings28. Causes proposed for the non-significant teacher rating scales included use of ADHD medication during the school day and changes in the teachers who completed the rating scales during the study9; however, most children in our study were not taking ADHD medications. Importantly, over the course of our study there were some changes in teachers who completed rating scales, which may have contributed to not finding differences in teacher ratings.
We had several limitations and challenges in this pilot study, which included a smaller sample size than desired based on power calculations, short intervention period, missing data due to unreturned or incomplete rating scales, inability of some children to complete the full tests for some KiTAP tasks, refusal of some children to wear the emWave ® to measure HRV, the change in location of school yoga between groups, and changes in teachers rating the participant’s behavior. Many mindfulness and yoga interventions lack randomized assignment, statistical power, active control groups, and holistic measurement approaches29. The strength of our study is its randomized design. Moreover, by including parent and teacher reports of children’s behavior, clinical assessments and a physiological index of self-regulation, as well as qualitative data documenting the perceived changes and feasibility of the yoga intervention, our study is one of the first in the field to contribute to a holistic measurement approach.
In conclusion, our study suggests yoga practice improves parent ratings of inattention and combined symptoms for a subset of children with higher ADHD symptoms at baseline, but not for the group overall, or for teacher ratings. We also found that yoga improved reaction times and decreased omission errors on some tasks of attention which are less subjective than parent/teacher rating scales, and is a promising sign of the impact of yoga on improved attention. We did not see significant changes in HRV after yoga, although our study was underpowered and of short duration. Importantly, we learned that yoga was feasible and well-liked by parents and teachers. This study adds to the growing body of literature suggesting yoga as an intervention to address attentional symptoms in ADHD, while also including suggestions to guide future yoga studies in this age group. Larger studies with an active control condition are needed to evaluate if subgroups with higher baseline ratings or symptom subtypes respond better to yoga. As more evidence supporting the use of yoga for children with ADHD symptoms is gathered yoga may be considered an additional intervention to improve attention.
Supplementary Material
Supplemental Digital Content 1. docx
Figure: Study Timeline. Mixed-methods randomized waitlist controlled trial. The quantitative measures were done at baseline, Time 1 (6 weeks), Time 2 (12 weeks), and follow-up (3 months after Time 2). The qualitative measures were done after each group completed their six-week yoga intervention.
Supplemental Digital Content 2. docx
Table: Yoga Study Protocol. The protocol was adapted from the If I Was a Bird Yoga ™ sequence for use in this study.
Supplemental Digital Content 3. docx
Figure: Yoga teacher rated Time on Task over the course of the 6-week intervention, by group in relation to ADHD symptoms severity on the ADHD Rating Scale IV Preschool Version. In each plot, three lines are presented for average symptoms (solid), low symptoms defined as one standard deviation below the mean (dashed) and high symptoms defined as one standard deviation above the mean (dotted).
Acknowledgments
We would like to thank the families, teachers and staff from Triumph Center for Early Childhood Education who participated in this study, as well as the time and dedication of the yoga instructors, assistants and volunteers who helped with this study. We are also grateful for donations from the Brodovsky Family Foundation, R. Robert & Suzanne W. Hansen Endowment Fund, and yoga mats from Manduka ®.
Footnotes
Conflicts of Interest: None declared by any of the authors
References
- 1.Barkley RA. Attention-Deficit Hyperactivity Disorder. Fourth. New York, NY: The Guilford Press; 2015. [Google Scholar]
- 2.Wolraich M, Brown L, Brown RT, et al. ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128(5):1007–1022. doi: 10.1542/peds.2011-2654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berwid OG, Halperin JM. Emerging support for a role of exercise in attention-deficit/hyperactivity disorder intervention planning. Curr Psychiatry Rep. 2012;14(5):543–551. doi: 10.1007/s11920-012-0297-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van der Oord S, Bogels SM, Peijnenburg D. The effectiveness of mindfulness training for children with ADHD and mindful parenting for their parents. J Child Family Stud. 2012;21(1):139–147. doi: 10.1007/s10826-011-9457-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Halperin JM, Marks DJ, Bedard AC, et al. Training executive, attention, and motor skills: a proof-of-concept study in preschool children With ADHD. J Atten Disord. 2013;17(8):711–721. doi: 10.1177/1087054711435681. [DOI] [PubMed] [Google Scholar]
- 6.Tang YY, Yang L, Leve LD, et al. Improving executive function and its neurobiological mechanisms through a mindfulness-based intervention: advances within the field of developmental neuroscience. Child Dev Perspect. 2012;6(4):361–366. doi: 10.1111/j.1750-8606.2012.00250.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Flook L, Goldberg SB, Pinger L, et al. Promoting prosocial behavior and self-regulatory skills in preschool children through a mindfulness-based kindness curriculum. Dev Psychol. 2015;51(1):44–51. doi: 10.1037/a0038256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gard T, Noggle JJ, Park CL, et al. Potential self-regulatory mechanisms of yoga for psychological health. Front Hum Neurosci. 2014;8:770. doi: 10.3389/fnhum.2014.00770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jensen PS, Kenny DT. The effects of yoga on the attention and behavior of boys with attention-deficit/hyperactivity disorder (ADHD) J Atten Disord. 2004;7(4):205–216. doi: 10.1177/108705470400700403. [DOI] [PubMed] [Google Scholar]
- 10.Haffner J, Roos J, Goldstein N, et al. The effectiveness of body-oriented methods of therapy in the treatment of attention-deficit hyperactivity disorder (ADHD): results of a controlled pilot study. Z Kinder Jugendpsychiatr und Psychother. 2006;34(1):37–47. doi: 10.1024/1422-4917.34.1.37. [DOI] [PubMed] [Google Scholar]
- 11.Harrison LJ. Sahaja yoga meditation as a family treatment programme for children with attention deficit-hyperactivity disorder. Clin Child Psychol Psychiatry. 2004;9(4):479–497. [Google Scholar]
- 12.Peck HL, Kehle TJ, Bray MA, et al. Yoga as an intervention for children with attention problems. School Psychol Review. 2005;34(3):415. [Google Scholar]
- 13.Hariprasad VR, Arasappa R, Varambally S, et al. Feasibility and efficacy of yoga as an add-on intervention in attention deficit-hyperactivity disorder: an exploratory study. Indian J Psychiatry. 2013;55(Suppl 3):S379–384. doi: 10.4103/0019-5545.116317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Razza RA, Bergen-Cico D, Raymond K. Enhancing preschoolers’ self-regulation via mindful yoga. J Child Family Stud. 2015;24(2):372–385. [Google Scholar]
- 15.Balasubramaniam M, Telles S, Doraiswamy PM. Yoga on our minds: a systematic review of yoga for neuropsychiatric disorders. Front Psychiatry. 2012;3:117. doi: 10.3389/fpsyt.2012.00117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCraty Rollin, Shaffer Fred. Heart rate variability: new perspectives on physiological mechanisms, assessment of self-regulatory capacity, and health risk. Glob Adv Health Med. 2015;4(1):46–61. doi: 10.7453/gahmj.2014.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buchhorn R, Conzelmann A, Willaschek C, et al. Heart rate variability and methylphenidate in children with ADHD. Atten Defic Hyperact Disord. 2012;4(2):85–91. doi: 10.1007/s12402-012-0072-8. [DOI] [PubMed] [Google Scholar]
- 18.McGoey KE, DuPaul GJ, Haley E, et al. Parent and teacher ratings of attention/deficit/hyperactivity disorder in preschool: the ADHD rating scale-IV preschool version. J Psychopathology Behavioral Assessment. 2007;29(4):269–276. [Google Scholar]
- 19.Bourdon KH, Goodman R, Rae DS, et al. The strengths and difficulties questionnaire: U.S. normative data and psychometric properties. J Am Acad Child Adolesc Psychiatry. 2005;44(6):557–564. doi: 10.1097/01.chi.0000159157.57075.c8. [DOI] [PubMed] [Google Scholar]
- 20.Testbatterie zur Aufmerksamkeitsprüfung für Kinder (KITAP) [computer program] Herzogenrath, Germany: Psytest; 2002. [Google Scholar]
- 21.Knox A, Schneider A, Abucayan F, et al. Feasibility, reliability, and clinical validity of the test of attentional performance for children (KiTAP) in fragile X syndrome (FXS) J Neurodev Disord. 2012;4(1):2. doi: 10.1186/1866-1955-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tarvainen MP, Niskanen JP, Lipponen JA, et al. Kubios HRV–heart rate variability analysis software. Comput Methods Programs Biomed. 2014;113(1):210–220. doi: 10.1016/j.cmpb.2013.07.024. [DOI] [PubMed] [Google Scholar]
- 23.SAS [computer program]. Version 9.4. Cary, NC: SAS Institute Inc; 2002–2012. [Google Scholar]
- 24.R [computer program]. Version 3.2.2. Vienna Austria: Team RC R: A language and environment for statistical computing. R Foundation for Statistical Computing; 2015. [Google Scholar]
- 25.Butzer B, Bury D, Telles S, et al. Implementing yoga within the school curriculum: a scientific rationale for improving social-emotional learning and positive student outcomes. J Children’s Services. 2016;11(1):3–24. [Google Scholar]
- 26.Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics. 2012;9(3):490–499. doi: 10.1007/s13311-012-0135-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Group MC. National institute of mental health multimodal treatment study of ADHD follow-up: changes in effectiveness and growth after the end of treatment. Pediatrics. 2004;113(4):762–769. doi: 10.1542/peds.113.4.762. [DOI] [PubMed] [Google Scholar]
- 28.Mehta S, Shah D, Shah K, et al. Peer-mediated multimodal intervention program for the treatment of children with ADHD in India: one-year followup. ISRN Pediatr. 2012;2012:419168. doi: 10.5402/2012/419168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Greenberg MT, Harris AR. Nurturing mindfulness in children and youth: Current state of research. Child Dev Perspect. 2012;6(2):161–166. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1. docx
Figure: Study Timeline. Mixed-methods randomized waitlist controlled trial. The quantitative measures were done at baseline, Time 1 (6 weeks), Time 2 (12 weeks), and follow-up (3 months after Time 2). The qualitative measures were done after each group completed their six-week yoga intervention.
Supplemental Digital Content 2. docx
Table: Yoga Study Protocol. The protocol was adapted from the If I Was a Bird Yoga ™ sequence for use in this study.
Supplemental Digital Content 3. docx
Figure: Yoga teacher rated Time on Task over the course of the 6-week intervention, by group in relation to ADHD symptoms severity on the ADHD Rating Scale IV Preschool Version. In each plot, three lines are presented for average symptoms (solid), low symptoms defined as one standard deviation below the mean (dashed) and high symptoms defined as one standard deviation above the mean (dotted).


