Abstract
Introduction
Staphylococcus aureus causes a diverse array of diseases, ranging from relatively harmless localized skin infections to life-threatening systemic conditions. It secretes toxins directly associated with particular disease symptoms.
Aim
To determine the prevalence of methicillin-resistant S. aureus (MRSA) and methicillin-susceptible S. aureus (MSSA) colonization among patients with atopic dermatitis and to assess the antimicrobial susceptibility to conventional antibiotics and selected antimicrobial peptides among toxin-producing strains and nonproducing strains.
Material and methods
One hundred patients with atopic dermatitis and 50 healthy people were microbiologically assessed for the carriage of S. aureus. Antimicrobial susceptibility tests were performed using the broth microdilution method for conventional antibiotics and antimicrobial peptides (CAMEL, Citropin 1.1, LL-37, Temporin A). Detection of genes lukS/lukF-PV, tst, sea-sed, eta and etb by multiplex PCR was performed.
Results
Staphylococcus aureus strains were isolated from the majority of patients, from either the skin (75%) or the anterior nares (73%). Among the conventional antibiotics tested, the highest rates of resistance were observed for ampicillin, daptomycin, lincomycin and erythromycin. Antimicrobial peptides did not show significant diversity in activity. Among MSSA strains greater differentiation of secreted toxins was observed (sec, eta, pvl, tsst, etb, seb), while in the group of MRSA strains secretion of 3 toxins (pvl, eta, seb) was noted.
Conclusions
Antimicrobial resistance continues to evolve. It is important to monitor S. aureus infections. The profile of toxins produced by S. aureus strains is an important consideration in the selection of an antimicrobial agent to treat infections.
Keywords: antimicrobial peptides, atopic dermatitis, polymerase chain reaction
Introduction
Atopic dermatitis (AD) is a common inflammatory skin disease with a chronic course. Patients suffering from AD show increased susceptibility to infections caused by viruses, bacteria or fungi and have an altered skin microflora. Studies have shown that 80 to 100% of patients with AD present nasal or skin colonization by Staphylococcus aureus, while the prevalence is 5 to 30% in healthy individuals [1]. A correlation between the severity of the eczema and colonization with S. aureus has been demonstrated, and it has been determined that bacterial colonization is an important factor aggravating skin lesions [2]. The pathogenicity of S. aureus is associated with the production of staphylococcal superantigens, which include toxic shock syndrome toxin-1 (TSST-1), staphylococcal enterotoxins (SEA, SEB, SEC, SED), exfoliative toxins (ETA and ETB), and leukocidin [3]. Superantigens are characterized by their capacity to stimulate a large number of T-cells. In contrast to conventional antigens, superantigens avoid intracellular processing and bind directly to the major histocompatibility complex (MHC) class II molecule, on the surface of the antigen processing cell, outside the antigen-binding groove [4]. Recently, an epidemic of community-acquired methicillin-resistant S. aureus (CA-MRSA) infections has emerged throughout the United States. These strains have an SCCmec (staphylococcal cassette chromosome mec) type IV cassette conferring resistance to methicillin, and 77% of them harbor genes for Panton Valentine leukocidin (PVL) [5, 6]. In addition, the prevalence of the genes for α-toxin and SEB is higher in CA-MRSA than in hospital-acquired MRSA (HA-MRSA), suggesting that strains circulating in the community are more virulent than hospital-associated strains [7]. The enhanced resistance of bacteria to conventional antibiotics is a serious problem in present day healthcare; thus the development of novel antimicrobial therapies, such as those based on various antimicrobial peptides (AMPs), seems to be advisable. The human body is equipped with more than 100 antimicrobial peptides that are an integral part of innate immunity [8]. They have broad antibacterial activity against Gram-positive and -negative bacteria and also show antifungal and antiviral activity. AMPs kill bacteria by permeating their membranes, and thus the lack of a specific molecular microbial target minimizes resistance development [9]. Currently, several peptides and peptide-based compounds are undergoing clinical trials [10]. Lesional skin of AD patients shows less expression of AMPs than would be predicted based on the inflammation and skin damage at this site [9]. Decreased expression of human β defensins (hBD-2 and hBD-3) in AD was also observed, and Th-2 cytokines IL-4 and IL-13 suppress hBD-2 and hBD-3 mRNA induction by tumor necrosis factor α (TNF-α) in keratinocytes [11]. Decreased expression of AMPs can explain the increased susceptibility of AD patients to skin infection.
Aim
The main purpose of this study was to assess the colonization of S. aureus in patients with AD. The isolated bacterial strains were analyzed for superantigen excretion and susceptibility to conventional antibiotics and selected AMPs (CAMEL, Citropin 1.1, LL-37, and Temporin A).
Material and methods
Patients and bacterial isolates
Patients were enrolled in our study during their visits in the Outpatient Clinic and hospitalization in the Department of Dermatology, Venereology and Allergology in Gdańsk (Medical University in Gdańsk) from August 2014 to August 2015. There was no selection of patients by sex or by severity of lesions. Atopic dermatitis was diagnosed following the criteria of Hanifin and Rajka, which include: pruritus, typical morphology and distribution of eczematous lesions, chronicity of the disease and personal or family history of atopy [12]. The study was approved by the local Research Ethics Board (approval number NKBBN/242-477/2014). Voluntary informed consent in written form was obtained from all participants. The exclusion criteria included: chronic dermatological condition with compromised skin barrier (e.g. psoriasis), diagnosis of any other chronic condition that increases the risk for MRSA colonization, oral or intravenous antibiotic treatment in the previous 4 weeks, treatment with topical antibiotics in the past 2 weeks, treatment with systemic corticosteroids or immunosuppressive drugs in the past 4 weeks, history of hospitalization, surgery, dialysis or residence in a long-term facility in the past year, indwelling catheter or a percutaneous device at the time of enrollment. Skin and nasal swabs collected from 100 patients with AD and 50 controls were used to investigate the presence of S. aureus. The control group consisted of patients without personal or family history of skin or allergic diseases who visited the Dermatological Outpatient Clinic for the dermatoscopic evaluation of moles. As a matter of fact, the CA-MRSA definition introduced in 2000 year by the Centers for Disease Control and Prevention (CDC) is described as a MRSA infection in a person who has none of the following established risk factors for MRSA infection: isolation of MRSA more than 48 h after hospital admission; history of hospitalization, surgery, dialysis or residence in a long-term care facility within one year of the MRSA culture date; the presence of an indwelling catheter or a percutaneous device at the time of culture; or previous isolation of MRSA [13].
Identification of S. aureus and MRSA strains
Preliminary identification and detection of S. aureus and MRSA strains was conducted using ChromID MRSA/ChromID S. aureus biplate (bioMérieux) for the simultaneous detection of S. aureus and methicillin-resistant S. aureus (MRSA).
Antimicrobial agents
Antimicrobial susceptibility tests for conventional antibiotics and antimicrobial peptides were performed on both, MSSA and MRSA strains. The conventional antibiotics tested included: ampicillin (Carl Roth GmbH), ciprofloxacin (Fluka), daptomycin (Sigma-Aldrich), erythromycin (Sigma-Aldrich), fusidic acid (Sigma-Aldrich), linezolid (Sigma-Aldrich), lincomycin (Sigma-Aldrich), mupirocin (Sigma-Aldrich), tetracycline (Sigma-Aldrich) and vancomycin (Sigma-Aldrich).
Antimicrobial peptides (AMPs) used in the study were: CAMEL (KWKLFKKIGAVLKVL-NH2), Citropin 1.1 (GLFDVIKKVASVIGGL-NH2), LL-37 (LLGDFFRKSKEKIGKEFKRIVQRIKDFLRNLVPRTES) and Temporin A (FLPLIGRVLSGIL-NH2). AMPs were synthesized manually by Fmoc chemistry on polystyrene resin modified by Rink Amide linker. Moreover, LL-37 was synthesized on Wang resin due to C-terminal carboxyl group. Deprotection of the Fmoc groups was carried out in 20 min using 20% piperidine in N, N-dimethylformamide (DMF). Then, the resin was washed with DMF and DCM (dichloromethane) and a chloranil test was performed. All amino acids were coupled using a mixture of DMF/DCM (1 : 1, v/v) in the presence of coupling agents such as 1-hydroxybenzotriazole (HOBt) and N, N-diisopropylcarbodiimide (DIC). The degree of acylation was monitored by the chloranil test. The peptides were cleaved from the resin with a mixture consisting of trifluoroacetic acid (TFA), water, triisopropylsilane (TIS) and phenol (92.5 : 2.5 : 2.5 : 2.5, v/v/v/v) as scavengers. In the next step, the peptide compounds were precipitated with cold diethyl ether and lyophilized. All crude products were purified by reversed-phase high-performance liquid chromatography (RP-HPLC) in a gradient of acetonitrile and water, both containing 0.1% TFA. Identity of the peptides was confirmed by mass spectrometry (ESI-MS).
Antimicrobial activity
Minimum inhibitory concentration (MIC) was determined by the broth microdilution method in Mueller Hinton broth according to the Clinical and Laboratory Standards Institute (CLSI) recommendations [14]. Assays for daptomycin were performed in medium supplemented with Ca2+ (50 mg/l). Polypropylene 96-well plates with bacteria at initial inoculums of 0.5 × 105 CFU/ml exposed to tested compounds were incubated for 18 h at 37°C. Minimum inhibitory concentration was taken as the lowest concentration of the compound at which visible growth of bacteria was not observed. The experiments were performed in triplicate. Research was conducted in the laboratory of the Department of Inorganic Chemistry, Medical University of Gdańsk.
Consideration of whether bacterial isolates are resistant or susceptible was conducted using interpretative criteria provided by CLSI [14].
DNA isolation
High molecular weight, bacterial genomic DNA was purified from lysates with Easy Genomic DNA Preparation (A&A Biotechnology, Poland) as described by Barski et al. [15]. Bacterial culture (1 ml) was centrifuged and suspended in 200 μl of 2% Triton X-100 in 2 M NaCl solution (Serva, Germany) and 2–5 μl of Lysostaphin (Sigma-Aldrich, USA) was added to make a final concentration of 25 μg/ml. The mixture was then incubated at 37°C for 30 min, 1 μl of proteinase K (Sigma, USA) was added and the mixture was incubated again at 65°C for 15 min. Subsequently, 400 μl of a chloroform gel (A&A Biotechnology, Poland) was added and the mixture was vortexed for 10 s (vortex, DHN, Poland). The white suspension obtained was centrifuged and the top phase shifted to a new tube. Finally, DNA was precipitated with isopropanol (Serva, Germany). DNA was dissolved in 100 μl of TE buffer (10 mM Tris pH 8.0; 1 mM EDTA; Sigma-Aldrich, USA), and its concentration was determined spectrophotometrically (DNA Calculator, Pharmacia). The DNA was stored at 20°C. Samples were diluted with sterile deionized water to a concentration of 5 ng/μl prior to amplification.
Toxin gene detection by PCR technique
DNA amplification was carried out in a Perkin Elmer 2400 thermocycler (Norwalk, USA). Primers for enterotoxins (SEA, SEB, SEC and SED), TSST-1 and exfoliative toxins (ETA, ETB) were used as described previously [16, 17]. Primers used in PCR amplification of staphylococcal toxin genes are shown in Table 1. Bacterial DNA (50–100 ng) of S. aureus isolates was amplified in two sets of multiplex PCR. Set A contained 20 pmol (each) of sea, seb and sec primers and 40 pmol of sed primer, while set B contained 50 pmol of eta and 20 pmol (each) of etb and tst primers. Detection of the genes was performed in 50 μl/l of a mixture consisting of: 5 μl/l bacterial DNA (5 ng/μl), 5 μl/l 10× Reaction Buffer (100 mM Tris-HCl, pH 8.3; 500 mM KCl; 0.8% detergent) (MBI Fermentas Lithuania), primers sea, seb, sec, sed or eta, etb and tsst (Sigma-Proligo, USA), 200 μM (each) dNTP, 2 U of Taq DNA polymerase (MBI Fermentas Lithuania), 1.5 mM MgCl2. The volume of this mix was adjusted to 50 ml with sterile water. Multiplex primer set B included the same constituents as in set A except for the MgCl2 concentration (2.0 mM) and the primers, which were used at 50 pmol for eta and 20 pmol each for etb and tsst. DNA amplification was carried out in the automatic thermocycler GeneAmp PCR System 2400 (Perkin Elmer, USA) with the following thermal cycling profile: an initial denaturation at 94°C for 5 min was followed by 35 cycles of amplification (denaturation at 94°C for 2 min, annealing at 57°C for 2 min, and extension at 72°C for 1 min) and a final extension at 72°C for 7 min. The amplification of PVL genes (lukS/lukF-PV) was performed as described by Lina et al. [17]. The PCR products were analyzed on 4% agarose gel (Sigma, USA) in the presence of ethidium bromide and photographed under UV illumination. Detection of the PVL genes (lukS-PV/lukF-PV) was performed in 50 μl/l of mixture and 1 μl of primers PVL-1 and PVL-2 (100 mM). DNA amplification was carried out with the following thermal cycling profile: 30 cycles of amplification (30 s of denaturation at 94°C, 30 s of annealing at 55°C, and 1 min of extension at 72°C). The size of amplified fragments was compared with the position of a molecular weight marker (pUC19-DNA/MspI Marker 23; MBI Fermentas, Lithuania) and the reference strains. The negative control consisted of a mixture without the addition of bacterial DNA.
Table 1.
Primers used in PCR amplification of staphylococcal toxin genes
| Primer | Sequence of primers (5′–3′) | Size ofproduct [bp] |
|---|---|---|
| SEA1 | GGT TAT CAA TGT GCG GGT GG | 102 |
| SEA2 | CGG CAC TTT TTT CTC TTC GG | |
| SEB1 | GTA TGG TGG TGT AAC TGA GC | 164 |
| SEB2 | CCA AAT AGT GAC GAG TTA GG | |
| SEC1 | AGA TGA AGT AGT TGA TGT GTA TGG | 451 |
| SEC2 | CAC ACT TTT AGA ATC AAC CG | |
| SED1 | CCA ATA ATA GGA GAA AAT AAA AG | 287 |
| SED2 | ATT GGT ATT TTT TTT CGT TC | |
| TSST1-1 | ACC CCT GTT CCC TTA TCA TC | 326 |
| TSST1-2 | TTT TCA GTA TTT GTA ACG CC | |
| ETA-1 | GCA GGT GTT GAT TTA GCA TT | 93 |
| ETA-2 | AGA TGT CCC TAT TTT TGC TG | |
| ETB-1 | ACA AGC AAA AGA ATA CAG CG | 226 |
| ETB-2 | GTT TTT GGC TGC TTC TCT TG | |
| PVL-1 | ATC ATT AGG TAA AAT GTC TGG ACA TGA TCCA | 433 |
| PVL-2 | GCA TCA ACT GTA TTG GAT AGC AAA AGC |
Results
Patients and bacterial isolates
A total of 200 specimens were collected from 100 patients during the study. AD patients consisted of 55% males and 45% females, age 1 to 63 years, median: 22.3 ±15.6 years. Staphylococcus aureus was reported in 75 of 100 (75%) skin swabs and 73 of 100 nasal swabs (73%). Six (6%) of the 100 nasal swabs and 5 (5%) of the 100 skin swabs were positive for MRSA. A total of 100 specimens were collected from 50 healthy subjects in the control group. Seven of 50 (14%) nasal swabs and 2 of 50 skin swabs (4%) were positive for S. aureus. The MRSA colonization was not reported in the control group. Clinical characteristics are shown in Table 2.
Table 2.
Clinical characteristics of patients with atopic dermatitis and control group
| Parameter | Patients | Control | P-value |
|---|---|---|---|
| Total no. | 100 | 50 | 0.0001b |
| Children | 38 | 2 | |
| Adults | 62 | 48 | |
| Age [years] | 22.3 ±15.6 | 35.1 ±13.4 | 0.0001a |
| Sex (%): | |||
| Female | 45 | 50 | |
| Male | 55 | 50 | |
| Presence of SA (%): | 0.0001b | ||
| On the skin | 75 | 4 | |
| Anterior nares | 73 | 14 | |
| Presence of MRSA (%): | 11 | 0 | |
| CA-MRSA | 54.5% | 0 | |
| HA-MRSA | 45.5% | 0 | |
Mann-Whitney U test
χ2 test.
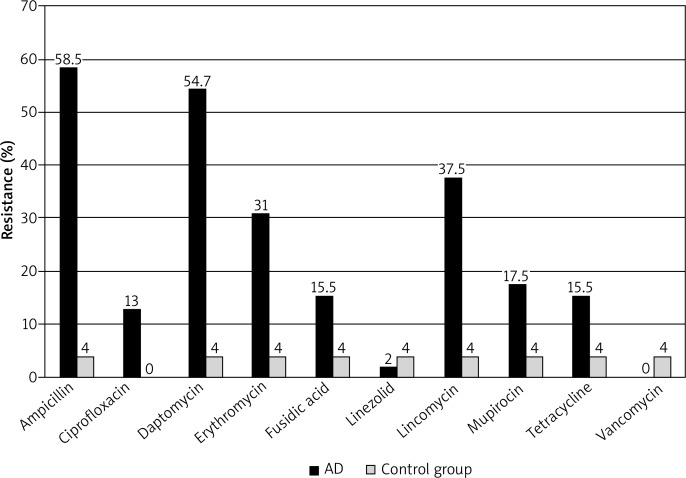
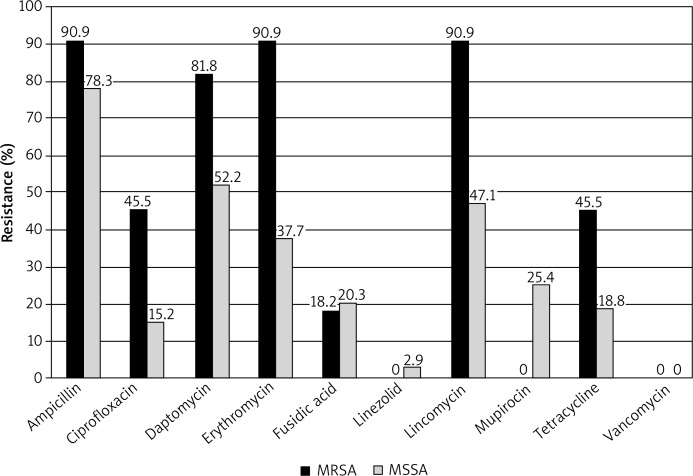
Antibiotic sensitivity pattern of S. aureus
The conventional antibiotics used in the study exhibited diverse activities against clinical isolates of S. aureus. The vancomycin MIC values were the lowest among the tested antibiotics and varied between 0.125 and 8 μg/ml. The minimal inhibitory concentrations for 90% of isolates (MIC 90) were the lowest for ciprofloxacin and vancomycin. The highest MIC 90 were noted for erythromycin, lincomycin, mupirocin and tetracycline among patients with AD. Similar results were obtained for the control group; see Table 3. Among the conventional antibiotics tested, the highest rates of resistance were observed for ampicillin (58.5%), daptomycin (54.7%), lincomycin (37.5%) and erythromycin (31.0%). The following percentages of resistant strains were noted for: mupirocin 17.5%, tetracycline 15.5%, ciprofloxacin 13.0%. In the control group strains resistant to ampicillin (4%), daptomycin (4%), erythromycin (2%), fusidic acid (1%), lincomycin (3%), and tetracycline (1%) were noted. All strains in the control group were sensitive to ciprofloxacin, linezolid, mupirocin and vancomycin. The antimicrobial resistance patterns (%) of S. aureus in patients with atopic dermatitis and the control group are shown in Figure 1. For the antibiotics ciprofloxacin, erythromycin, lincomycin, and tetracycline, the percentage of resistant strains was significantly higher in the MRSA group than the MSSA group (Figure 2). Antimicrobial peptides (CAMEL, Citropin 1.1, LL-37 Temporin A) did not show significant diversity in activity, depending on the tested strain. The concentrations that inhibited growth of S. aureus strains were several times higher as compared to those of vancomycin, ciprofloxacin, fusidic acid and linezolid.
Table 3.
Minimal inhibitory concentration values of Staphylococcus aureus strains isolated from atopic dermatitis (AD) patients and control group
| Agents | MIC [μg/ml] | P-value | |||||
|---|---|---|---|---|---|---|---|
| Patients with AD | Control group | ||||||
| Range | MIC 50 | MIC 90 | Range | MIC 50 | MIC 90 | ||
| Ampicillin | 0.125–32 | 2 | 16 | 0.25–32 | 16 | 32 | 0.125584 |
| Ciprofloxacin | 0.125–>512 | 0.5 | 2 | 0.125–1 | 0.25 | 1 | 0.2214 |
| Daptomycin | 0.125–4 | 2 | 4 | 1–2 | 2 | 2 | 0.6965 |
| Erythromycin | 0.125–>512 | 0.5 | > 512 | 0.125–>512 | 1 | > 512 | 0.7188 |
| Fusidic acid | 0.312–32 | 0.125 | 8 | 0.125–16 | 1 | 16 | 0.0242 |
| Linezolid | 0.25–32 | 1 | 4 | 1–4 | 2 | 4 | 0.125059 |
| Lincomycin | 0.25–>512 | 1 | 64 | 0.25–>512 | 0.5 | > 512 | 0.25239 |
| Mupirocin | 0.125–>512 | 0.5 | > 512 | 0.125–32 | 0.25 | 32 | 0.25257 |
| Tetracycline | 0.125–64 | 0.5 | 32 | 0.125–32 | 0.5 | 32 | 0.8630 |
| Vancomycin | 0.125–8 | 0.5 | 2 | 0.25–1 | 1 | 1 | 0.8069 |
MIC 50 – MIC for 50% of isolates. MIC 90 – MIC for 90% of isolates. Significant differences between groups determined with Mann-Whitney U test.
Figure 1.
Antimicrobial resistance patterns (%) of S. aureus in patients with atopic dermatitis and control group
Figure 2.
Antimicrobial resistance patterns (%) of S. aureus in patients with atopic dermatitis among methicillin-resistant S. aureus (MRSA) and methicillin-susceptible S. aureus (MSSA) strains
Amplification of eta, etb sea, seb, sec, sed, tst and pvl genes
Among tested strains, 17 were positive for eta, 5 for etb, 3 for seb and 21 for sec. Seven strains were found to be tsst positive, and 16 contained the pvl gene. None were positive for sea or sed. Among MSSA strains greater differentiation of secreted toxins was observed (in order of frequency: sec, eta, pvl, tsst, etb, seb), while in the group of MRSA strains secretion of 3 toxins (pvl, eta, seb) was noted. Secretion of at least one toxin was observed among MSSA strains in 4 and MRSA strains in 4 cases. Prevalence (%) of staphylococcal toxin genes among tested strains is shown in Table 4. Considering the susceptibility profile, a difference between superantigen positive and negative strains in the group of conventional antibiotics was not noted, except for erythromycin, fusidic acid and mupirocin. Also, we did not find that strains producing tested superantigens were less susceptible to AMPs than nonproducing ones (Table 5).
Table 4.
Prevalence (%) of staphylococcal toxin genes among tested strains
| Gene | MSSA (n = 148) | MRSA (n = 11) |
|---|---|---|
| eta | 12.8% (19) | 9.09% |
| etb | 4.7% (7) | 0% |
| pvl | 10.1% (15) | 27.27% |
| sea | 0% (0) | 0% |
| seb | 2.7% (4) | 9.09% |
| sec | 15.5% (23) | 0% |
| sed | 0% (0) | 0% |
| tsst | 6.1% (9) | 0% |
Table 5.
Minimal inhibitory concentration of Staphylococcus aureus strains isolated from atopic dermatitis (AD) patients
| Agents | MIC [μg/ml] | |||||
|---|---|---|---|---|---|---|
| Superantigen positive Staphylococcus aureus (n = 52) | Superantigen negative Staphylococcus aureus (n = 48) | |||||
| MIC 50 | MIC 90 | Range | MIC 50 | MIC 90 | Range | |
| Ampicillin | 1 | 8 | 0.125–32 | 8 | 16 | 0.125–32 |
| Ciprofloxacin | 0.5 | 2 | 0.625–>512 | 0.25 | 2 | 0.0625–>512 |
| Daptomycin | 2 | 2 | 0.125–4 | 2 | 4 | 0.0625–4 |
| Erythromycin | 0.5 | > 512 | 0.125–>512 | 0.5 | 256 | 0.0625–>512 |
| Fusidic acid | 0.125 | 8 | 0.0625–32 | 0.125 | 4 | 0.0312–32 |
| Linezolid | 1 | 2 | 0.5–4 | 1 | 4 | 0.25–4 |
| Lincomycin | 1 | 16 | 0.25–>512 | 1 | 64 | 0.25–>512 |
| Mupirocin | 0.5 | > 512 | 0.0625–>512 | 0.25 | 512 | 0.0625–>512 |
| Tetracycline | 0.25 | 32 | 0.0625–32 | 0.5 | 32 | 0.0625–32 |
| Vancomycin | 0.5 | 1 | 0.125–2 | 1 | 2 | 0.125–2 |
| CAMEL | 4 | 8 | 1–8 | 4 | 4 | 2–128 |
| Citropin 1.1 | 16 | 16 | 1–64 | 16 | 32 | 1–128 |
| LL-37 | 64 | 256 | 2–>512 | 128 | > 512 | 2–>512 |
| Temporin A | 8 | 16 | 2–64 | 8 | 32 | 4–32 |
MIC 50 – MIC values for 50% of isolates. MIC 90 – MIC values for 90% of isolates.
Discussion
Epidemiology of S. aureus and MRSA strains in AD
Studies worldwide suggest that the prevalence of MRSA in the population with AD varies from 0 to 30.8% [18–20]. In the USA, where CA-MRSA is now the most common pathogen cultured from patients with skin and soft-tissue infections in emergency departments, the colonization rate of AD patients is as high as 18.3% [21]. CA-MRSA strains are responsible for severe infections, including toxic shock, necrotizing fasciitis, and necrotizing pneumonia. These strains have a unique mecA cassette (type IV) [22] and have greater antibiotic susceptibility than the HA-MRSA strains [23]. Staphylococcus aureus strains were isolated from the majority of our patients, either from the skin (75%) or the anterior nares (73%). In the present study, 6 (6%) of 100 nasal swabs and 5 (5%) of 100 skin swabs were positive for MRSA (55% CA-MRSA, 45% HA-MRSA). Compared with the HA-MRSA strains, CA-MRSA strains also have a higher prevalence of toxin genes, including the enterotoxins, TSST-1, and PVL [24]. Due to the insufficient number of strains, such a relationship in the present study was not observed.
Antibiotic resistance
Several studies concerning the effect of antimicrobial treatment on S. aureus colonization and the severity of inflammation have given conflicting results. In open or double-blind placebo-controlled trials, topical or systemic antibiotics were able to reduce colonization density and led to a partial improvement of skin lesion [25–27]. In addition, some authors reported that topical steroids in combination with antibiotic treatment can cause the elimination of S. aureus from the skin in some patients with AD [28]. On the other hand, treatment with oral antibiotics did not lead to a significant improvement of AD in two double-blind placebo-controlled studies [29, 30]. There are reports suggesting that treatment with antibiotics can temporarily reduce bacterial colonization and improve AD severity. However, these benefits last no longer than 3 months [31]. Antibacterials effective against S. aureus include azithromycin, cefuroxime axetil, clarithromycin and erythromycin [32], while CA-MRSA eradication by clindamycin, fusidic acid, trimethoprim-sulfamethoxazole and intranasal mupirocin can be effective. In our study a high rate of resistance to conventional antibiotics was noted. Thirty-one percent of isolated strains were resistant to erythromycin and 15.5% to tetracycline. Our results are comparable with those of Kędzierska et al. and Hoeger [33, 34]. In the above-mentioned studies the rate of resistance to erythromycin was respectively 14% and 18%. The increasing resistance to macrolides may suggest that erythromycin no longer should be applied in this indication. In the present study strains resistant to fusidic acid (FA) were also noted. The resistance rate of FA was as high as 15.5%. High rates of fusidic acid (FA)-resistant Staphylococcus aureus (FRSA) in patients with skin disease have been previously attributed to high usage of topical FA. The resistance rate of fusidic acid is nearly 10% in the general population and 50% in dermatological patients [35]. Shah et al. reported that 50% of S. aureus isolates among dermatological patients were resistant to fusidic acid [32]. These data reveal that a high rate of resistance may reveal that fusidic acid should be used in treatment of skin infections only for short periods of time in order to prevent further resistance development. There are reports suggesting that short-term use of topical FA for atopic dermatitis has no influence on increasing FRSA [36]. In the present study 17.5% of isolated strains were resistant to mupirocin, which is comparable with other report [37]. Although studies have reported resistance to the newer antimicrobial agents such as linezolid and vancomycin [38], in the present study none of the isolates were resistant to these antibiotics.
Antimicrobial peptides
AMPs seemed to be promising candidates to meet the demand for new classes of anti-infectives with novel mechanism of action. Daptomycin, a lipopeptide antibiotic widely used in the treatment of systemic and life-threatening infections caused by Gram-positive organisms including S. aureus, was approved in 2003. Unfortunately, therapeutic failures, relatively uncommon, have been reported [39]. Thus far, the mechanisms underlying daptomycin resistance (DAPR) in S. aureus have focused on point mutations in genes involved in phospholipid biosynthesis, particularly mprF, which codes for lysyl-phosphatidylglycerol (L-PG) synthetase, cls2, which codes for cardiolipin synthase, and pgsA, which codes for CDP-diacylglycerol-glycerol-3-phosphate-3-phosphatidyltransferase [40]. We found 54.8% isolates resistant to daptomycin. The susceptibility breakpoint for daptomycin was considered as < 1 μg/ml for staphylococci as recommended by the CLSI. Reduced susceptibility to vancomycin has been reported to be associated with reduced susceptibility to daptomycin. Diederen et al. reported 7 of the 17 vancomycin intermediate S. aureus (VISA) isolates to have a daptomycin minimum inhibitory concentration (MIC) of 2 μg/ml and one isolate to have MIC 4 μg/ml [41]. However, such an association was not seen in our study. The observation mentioned above suggests that frequent practice of using daptomycin when vancomycin therapy appears to be failing may be the wrong strategy. Recent data have shown “cross-resistance” between DAP and cationic host defense peptides (HDPs) from neutrophils and platelets in S. aureus isolates obtained from patients failing DAP therapy. Similar to many endogenous HDPs, daptomycin contains a significant peptide moiety that can be positively charged by calcium decoration during in vivo use. Therefore, one potential driver of such HDP-daptomycin cross-resistance phenotypes may be the capacity of innate HDPs to impact organisms before daptomycin therapy, facilitating increased daptomycin MICs on subsequent daptomycin exposure [42, 43]. Since many of the strains in the present study were isolated from skin infection, it is quite possible to exhibit the daptomycin non-susceptibility during therapy because daptomycin exhibits cross resistance to other cationic host defense peptides. The other antimicrobial peptides (CAMEL, Citropin 1.1, Temporin A) did not show significant diversity in activity LL-37, depending on the tested strain. The concentrations that inhibited growth of SA strains were higher than those of vancomycin, ciprofloxacin, fusidic acid and linezolid.
Virulence factors
Staphylococcus aureus produces numerous virulence factors, including exotoxins such as exfoliatins, Panton-Valentine leukocidin (PVL), superantigens including enterotoxins (SEA-SED), and toxic shock syndrome toxin-1 (TSST-1), that correspond well with our findings (52% of strains excreted tested superantigens). Of the more than 20 staphylococcal enterotoxins, SEA and SEB are the best characterized and are also regarded as superantigens because of their ability to bind to class II MHC molecules on antigen-presenting cells and stimulate large populations of T cells that share variable regions on the β chain of the T cell receptor. The result of this massive T cell activation is a cytokine bolus leading to acute toxic shock [44, 45]. The research regarding the appearance of the enterotoxin genes among the strains of S. aureus prove that about half of them have the enterotoxin genes [46]; however, the enterotoxin gene A (sea) dominates and about 25% of them have the tsst gene [16]. In the present study 2.7% were positive for seb and 15.5% for sec and none were positive for sea or sed. Panton-Valentine leukocidin is a cytotoxin that causes leukocyte destruction and tissue necrosis by damage of host defense cells membranes and erythrocytes by the synergistic action of 2 non-associated classes of secretory proteins. The PVL gene has been detected in S. aureus strains associated with community-acquired, severe, necrotizing pneumonia and furunculosis [17]. It is produced by fewer than 5% of S. aureus strains [46]. Strains isolated from primary necrotic infections involving the dermis, such as furuncles, harbored the PVL genes in 86–93% of cases [17, 47]. In contrast, superficial, non-necrotic processes such as impetigo and folliculitis were not associated with PVL-harboring S. aureus [48]. In the present study 10.1% of MSSA and 27.27% MRSA strains secreted PVL. Among MSSA strains greater differentiation of secreted toxins was observed (sec, eta, pvl, tsst, etb, seb), while in the group of MRSA strains secretion of 3 toxins (pvl, eta, seb) was noted. The purpose of the study was to investigate whether the superantigen positive S. aureus strains are more resistant to conventional antibiotics. The effect on toxin production is an important consideration in the selection of an antimicrobial agent to treat staphylococcal infections. Considering the susceptibility profile, a difference between superantigen positive and negative strains in the group of conventional antibiotics was noted for erythromycin, fusidic acid and mupirocin. An alarming observation is the higher resistance of those strains to macrolides which could not only kill bacteria and diminish the rate of colonization but also can suppress the production of superantigen [48]. We did not find that strains producing the tested superantigens were less susceptible to AMPs than nonproducing ones.
Conclusions
Strains of Staphylococcus aureus present a significant clinical chalange because of their rising prevalence of antimicrobial resistance. Methicillin-resistant S. aureus (MRSA) infections have become a general occurrence in hospitals, and the situation is worrying, since the pathogen is resistant to many antibiotics, including daptomycin and vancomycin, which was considered as the last resort for treatment of MRSA infections. AMPs seemed to be promising candidates to meet the demand for new classes of anti-infectives with a distinctive mechanism of action. Unfortunately, therapeutic failures have been reported, which correspond well with our findings (54.7% of strains resistant to daptomycin). The effect on toxin production is an important consideration in the selection of an antimicrobial agent to treat staphylococcal infections.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Petry V, Bessa GR, Poziomczyck CS, et al. Bacterial skin colonization and infections in patients with atopic dermatitis. An Bras Dermatol. 2012;87:729–34. doi: 10.1590/s0365-05962012000500010. [DOI] [PubMed] [Google Scholar]
- 2.Gong JQ, Lin L, Lin T, et al. Skin colonization by Staphylococcus aureus in patients with eczema and atopic dermatitis and relevant combined topical therapy: a double-blind multicentre randomized controlled trial. Br J Dermatol. 2006;155:680–7. doi: 10.1111/j.1365-2133.2006.07410.x. [DOI] [PubMed] [Google Scholar]
- 3.Iandolo JJ. Genetic analysis of extracellular toxins of Staphylococcus aureus. Annu Rev Microbiol. 1989;43:375–402. doi: 10.1146/annurev.mi.43.100189.002111. [DOI] [PubMed] [Google Scholar]
- 4.Marrack P, Kappler J. The staphylococcal enterotoxins and their relatives. Science. 1990;248:705–11. doi: 10.1126/science.2185544. [DOI] [PubMed] [Google Scholar]
- 5.Naimi TS, LeDell KH, Como-Sabetti K, et al. Comparison of community- and health care-associated methicillin-resistant Staphylococcus aureus infection. JAMA. 2003;290:2976–84. doi: 10.1001/jama.290.22.2976. [DOI] [PubMed] [Google Scholar]
- 6.Błażewicz I, Jaśkiewicz M, Piechowicz L, et al. Increasing rate of daptomycin non-susceptible strains of Staphylococcus aureus in patients with atopic dermatitis. Adv Dermatol Allergol. 2017;34:547–52. doi: 10.5114/ada.2017.72460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cosgrove SE, Sakoulas G, Perencevich EN, et al. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis. 2003;36:53–9. doi: 10.1086/345476. [DOI] [PubMed] [Google Scholar]
- 8.Marcinkiewicz M, Majewski S. The role of antimicrobial peptides in chronic inflammatory skin diseases. Adv Dermatol Allergol. 2016;33:6–12. doi: 10.5114/pdia.2015.48066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zanetti M. Cathelicidins, multifunctional peptides of the innate immunity. J Leukoc Biol. 2004;75:39–48. doi: 10.1189/jlb.0403147. [DOI] [PubMed] [Google Scholar]
- 10.Reddy KV, Yedery RD, Aranha C. Antimicrobial peptides: premises and promises. Int J Antimicrob Agents. 2004;24:536–47. doi: 10.1016/j.ijantimicag.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 11.Ong PY, Ohtake T, Brandt C, et al. Endogenous antimicrobial peptides and skin infections in atopic dermatitis. N Engl J Med. 2002;347:1151–60. doi: 10.1056/NEJMoa021481. [DOI] [PubMed] [Google Scholar]
- 12.Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol Suppl (Stockh) 1980;92:44–7. [Google Scholar]
- 13.Morrison MA, Hageman JC, Klevens RM. Case definition for community-associated methicillin-resistant Staphylococcus aureus. J Hosp Infect. 2006;62:241.. doi: 10.1016/j.jhin.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 14.Wayne PA. M100-S21: Performance standards for antimicrobial susceptibility testing. 2012. USA: Clinical and Laboratory Standards Institute (CLSI) p. 32. 21st Informational Supplement. [Google Scholar]
- 15.Barski P, Piechowicz L, Galiński J, et al. Rapid assay for detection of methicillin-resistant Staphylococcus aureus using multiplex PCR. Mol Cell Probes. 1996;10:471–5. doi: 10.1006/mcpr.1996.0066. [DOI] [PubMed] [Google Scholar]
- 16.Mehrotra M, Wang G, Johnson WM. Multiplex PCR for detection of genes for Staphylococcus aureus enterotoxins, exfoliative toxins, toxic shock syndrome toxin 1, and methicillin resistance. J Clin Microbiol. 2000;38:1032–5. doi: 10.1128/jcm.38.3.1032-1035.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lina G, Piémont Y, Godail-Gamot F, et al. Involvement of Panton-Valentine leukocidin-producing Staphylococcus aureus in primary skin infections and pneumonia. Clin Infect Dis. 1999;29:1128–32. doi: 10.1086/313461. [DOI] [PubMed] [Google Scholar]
- 18.Balma-Mena A, Lara-Corrales I, Zeller J, et al. Colonization with community-acquired methicillin-resistant Staphylococcus aureus in children with atopic dermatitis: a cross-sectional study. Int J Dermatol. 2011;50:682–8. doi: 10.1111/j.1365-4632.2010.04751.x. [DOI] [PubMed] [Google Scholar]
- 19.Breuer K, Haussler S, Kapp A, et al. Staphylococcus aureus: colonizing features and influence of an antibacterial treatment in adults with atopic dermatitis. Br J Dermatol. 2002;147:55–61. doi: 10.1046/j.1365-2133.2002.04872.x. [DOI] [PubMed] [Google Scholar]
- 20.Jappe U, Schnuch A, Uter W. Frequency of sensitization to antimicrobials in patients with atopic eczema compared with nonatopic individuals: analysis of multicentre surveillance data, 1995-1999. Br J Dermatol. 2003;149:87–93. doi: 10.1046/j.1365-2133.2003.05290.x. [DOI] [PubMed] [Google Scholar]
- 21.Chung HJ, Jeon HS, Sung H, et al. Epidemiological characteristics of methicillin-resistant Staphylococcus aureus isolates from children with eczematous atopic dermatitis lesions. J Clin Microbiol. 2008;46:991–5. doi: 10.1128/JCM.00698-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mongkolrattanothai K, Boyle S, Kahana MD, et al. Severe Staphylococcus aureus infections caused by clonally related community-acquired methicillin-susceptible and methicillin-resistant isolates. Clin Infect Dis. 2003;37:1050–8. doi: 10.1086/378277. [DOI] [PubMed] [Google Scholar]
- 23.Okuma K, Iwakawa K, Turnidge JD, et al. Dissemination of new methicillin-resistant Staphylococcus aureus clones in the community. J Clin Microbiol. 2002;40:4289–94. doi: 10.1128/JCM.40.11.4289-4294.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gillet Y, Issartel B, Vanhems P, et al. Association between Staphylococcus aureus strains carrying gene for Panton-Valentine leukocidin and highly lethal necrotising pneumonia in young immunocompetent patients. Lancet. 2002;359:753–9. doi: 10.1016/S0140-6736(02)07877-7. [DOI] [PubMed] [Google Scholar]
- 25.Brockow K, Grabenhorst P, Abeck D, et al. Effect of gentian violet, corticosteroid and tar preparations in Staphylococcus aureus-colonized atopic eczema. Dermatology. 1999;199:231–6. doi: 10.1159/000018253. [DOI] [PubMed] [Google Scholar]
- 26.Luber H, Amornsiripanitch S, Lucky AW. Mupirocin and the eradication of Staphylococcus aureus in atopic dermatitis. Arch Dermatol. 1988;124:853–4. [PubMed] [Google Scholar]
- 27.White MI, Noble WC. Consequences of colonization and infection by Staphylococcus aureus in atopic dermatitis. Clin Exp Dermatol. 1986;11:34–40. doi: 10.1111/j.1365-2230.1986.tb00421.x. [DOI] [PubMed] [Google Scholar]
- 28.Dhar S. Should topical antibacterials be routinely combined with topical steroids in the treatment of atopic dermatitis? Indian J Dermatol Venereol Leprol. 2005;71:71–2. doi: 10.4103/0378-6323.13987. [DOI] [PubMed] [Google Scholar]
- 29.Boguniewicz M, Sampson H, Leung SB, et al. Effects of cefuroxime axetil on Staphylococcus aureus colonization and superantigen production in atopic dermatitis. J Allergy Clin Immunol. 2001;108:651–2. doi: 10.1067/mai.2001.118598. [DOI] [PubMed] [Google Scholar]
- 30.Ewing CI, Ashcroft C, Gibbs AC, et al. Flucloxacillin in the treatment of atopic dermatitis. Br J Dermatol. 1998;138:1022–9. doi: 10.1046/j.1365-2133.1998.02271.x. [DOI] [PubMed] [Google Scholar]
- 31.Gilani SJ, Gonzalez M, Hussain I, et al. Staphylococcus aureus re-colonization in atopic dermatitis: beyond the skin. Clin Exp Dermatol. 2005;30:10–3. doi: 10.1111/j.1365-2230.2004.01679.x. [DOI] [PubMed] [Google Scholar]
- 32.Shah M, Mohanraj M. High levels of fusidic acid-resistant Staphylococcus aureus in dermatology patients. Br J Dermatol. 2003;148:1018–20. doi: 10.1046/j.1365-2133.2003.05291.x. [DOI] [PubMed] [Google Scholar]
- 33.Kędzierska A, Kapińska-Mrowiecka M, Czubak-Macugowska M, et al. Susceptibility testing and resistance phenotype detection in Staphylococcus aureus strains isolated from patients with atopic dermatitis, with apparent and recurrent skin colonization. Br J Dermatol. 2008;159:1290–9. doi: 10.1111/j.1365-2133.2008.08817.x. [DOI] [PubMed] [Google Scholar]
- 34.Hoeger PH. Antimicrobial susceptibility of skin-colonizing S. aureus strains in children with atopic dermatitis. Pediatr Allergy Immunol. 2004;15:474–7. doi: 10.1111/j.1399-3038.2004.00182.x. [DOI] [PubMed] [Google Scholar]
- 35.Mitra A, Mohanraj M, Shah M. High levels of fusidic acid-resistant Staphylococcus aureus despite restrictions on antibiotic use. Clin Exp Dermatol. 2009;34:136–9. doi: 10.1111/j.1365-2230.2008.02790.x. [DOI] [PubMed] [Google Scholar]
- 36.Ravenscroft JC, Layton AM, Eady EA, et al. Short-term effects of topical fusidic acid or mupirocin on the prevalence of fusidic acid resistant (FusR) Staphylococcus aureus in atopic eczema. Br J Dermatol. 2003;148:1010–7. doi: 10.1046/j.1365-2133.2003.05292.x. [DOI] [PubMed] [Google Scholar]
- 37.Kaur DC, Chate SS. Study of antibiotic resistance pattern in methicillin resistant Staphylococcus aureus with special reference to newer antibiotic. J Glob Infect Dis. 2015;7:78–8. doi: 10.4103/0974-777X.157245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Damaceno Q, Nicoli JR, Oliveira A. Variability of cutaneous and nasal population levels between patients colonized and infected by multidrug-resistant bacteria in two Brazilian intensive care units. SAGE Open Med. 2015;3:2050312114566668. doi: 10.1177/2050312114566668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fowler VG, Jr, Boucher HW, Corey GR, et al. Daptomycin versus standard therapy for bacteremia and endocarditis caused by Staphylococcus aureus. N Engl J Med. 2006;355:653–65. doi: 10.1056/NEJMoa053783. [DOI] [PubMed] [Google Scholar]
- 40.Peleg AY, Miyakis S, Ward DV, et al. Whole genome characterization of the mechanisms of daptomycin resistance in clinical and laboratory derived isolates of Staphylococcus aureus. PLoS One. 2012;7:e28316. doi: 10.1371/journal.pone.0028316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Diederen BM, Duijn IV, Willemse P, et al. In vitro activity of daptomycin against methicillin resistant Staphylococcus aureus including heterogeneously glycopeptide resistant strains. Antimicrob Agents Chemother. 2006;50:3189–91. doi: 10.1128/AAC.00526-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mishra NN, Bayer AS, Moise PA, et al. Reduced susceptibility to host-defense cationic peptides and daptomycin coemerge in methicillin-resistant Staphylococcus aureus from daptomycin-naive bacteremic patients. J Infect Dis. 2012;206:1160–7. doi: 10.1093/infdis/jis482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mishra NN, Yang SJ, Chen L, et al. Emergence of daptomycin resistance in daptomycin-naïve rabbits with methicillin-resistant Staphylococcus aureus prosthetic joint infection is associated with resistance to host defense cationic peptides and mprF polymorphisms. PLoS One. 2013;8:e71151. doi: 10.1371/journal.pone.0071151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bukowski M, Wladyka B, Dubin G. Exfoliative toxins of Staphylococcus aureus. Toxins (Basel) 2010;2:1148–65. doi: 10.3390/toxins2051148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Melconian AK, Brun Y, Fleurette J. Enterotoxin production, phage typing and serotyping of Staphylococcus aureus strains isolated from clinical materials and food. J Hyg (Lond) 1983;91:235–42. doi: 10.1017/s0022172400060241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Prevost G, Couppie P, Prevost P, et al. Epidemiological data on Staphylococcus aureus strains producing synergohymenotropic toxins. J Med Microbiol. 1995;42:237–45. doi: 10.1099/00222615-42-4-237. [DOI] [PubMed] [Google Scholar]
- 47.Couppie P, Cribier B, Prévost G. Leukocidin from Staphylococcus aureus and cutaneous infections: an epidemiologic study. Arch Dermatol. 1994;130:1208–9. doi: 10.1001/archderm.130.9.1208. [DOI] [PubMed] [Google Scholar]
- 48.Adachi Y, Akamatsu H, Horio T. The effect of antibiotics on the production of superantigen from Staphylococcus aureus isolated from atopic dermatitis. J Dermatol Sci. 2002;28:76–83. doi: 10.1016/s0923-1811(01)00143-8. [DOI] [PubMed] [Google Scholar]