Abstract
Oxidative and electrophilic changes in cells are mainly coordinated by the KEAP1/NRF2 (Kelch-like erythroid-derived cap-n-collar homology- (ECH-) associated protein-1/nuclear factor (erythroid-derived 2)-like 2) axis. The physical interaction between these two proteins promotes the expression of several antioxidant defense genes in response to exogenous and endogenous insults. Recent studies demonstrated that KEAP1/NRF2 axis dysfunction is also strongly related to tumor progression and chemo- and radiotherapy resistance of cancer cells. In solid tumors, the KEAP1/NRF2 system is constitutively activated by the loss of KEAP1 or gain of NFE2L2 functions that leads to its nuclear accumulation and enhances the transcription of many cytoprotective genes. In addition to point mutations, epigenetic abnormalities, as aberrant promoter methylation, and microRNA (miRNA) and long noncoding RNA (lncRNA) deregulation were reported as emerging mechanisms of KEAP1/NRF2 axis modulation. This review will summarize the current knowledge about the epigenetic mechanisms that deregulate the KEAP1/NRF2 cascade in solid tumors and their potential usefulness as prognostic and predictive molecular markers.
1. Introduction
Oncogenes and tumor suppressor genes are deregulated in cancer and modify their expression through heterogeneous genetic and epigenetic modifications. All these alterations exert their effects on several cellular processes in which transient modifications of redox balance might occur, such as cell cycle and apoptosis. These transient cellular changes are mainly coordinated by the KEAP1/NRF2 (Kelch-like erythroid-derived cap-n-collar homology- (ECH-) associated protein-1/nuclear factor (erythroid-derived 2)-like 2) signaling pathway [1]. NRF2 is a transcription factor that acts as a master modulator of cellular defense against toxic and oxidative damage, mitochondrial physiology, differentiation, and stem cell maintenance [2–4]. In normal cell conditions, the NRF2 negative regulator KEAP1 forms an ubiquitin ligase complex with cullin 3 (CUL3) and ring-box 1 (RBX1) and targets NRF2 for proteolysis. Upon stress exposure, a specific pattern of KEAP1 cysteine modification arises. By consequence, the KEAP1 releases NRF2 which translocates into the nucleus, where it forms a heterodimeric complex with the small MAF proteins. This complex recognizes the enhancer sequences known as antioxidant response elements (AREs) located in the cytoprotective genes and activates their transcription [5]. Additionally, NRF2 can be subjected to a KEAP1-independent transcriptional and posttranslational regulation, with a consequent alteration of its cellular localization, protein degradation, and DNA-binding capability [6].
Deregulation of the KEAP1/NRF2 axis is actually considered a hallmark in cancer cells, since KEAP1 and NRF2 can modulate oncogenesis, cell proliferation, apoptosis, and tumor cell growth [7].
A decreased levels of KEAP1 protein were firstly reported to be linked to poor outcome in NSCLC patients treated with platinum-based neoadjuvant regimen and in the NSCLC group of patients with lymph node metastases [8, 9].
Actually, the main molecular events that lead to NRF2 abnormal nuclear accumulation in solid tumors can be generally divided into genetic and epigenetic alterations. The final effect is in any case the disruption of protein-protein interaction of the KEAP1/NRF2 crosstalk and its imbalance in expression levels, with a consequent upregulation of cellular detoxifying proteins.
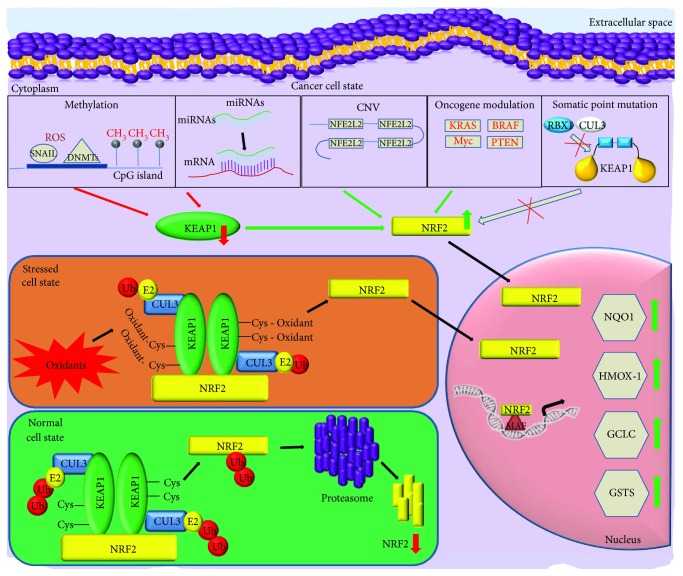
Genetic alterations were the first reported mechanisms of KEAP1/NRF2 axis deregulation. Biallelic changes of the tumor suppressor KEAP1 gene (by point mutations and loss of heterozygosity) were described for the first time in NSCLC [10] and, immediately after, in other several malignancies together with NFE2L2 mutations, the gene that codifies for the NRF2 protein [11]. More recently, the discovery of hypermethylation of the KEAP1 promoter and noncoding RNAs linked to cell-detoxifying network added a new important dimension in the complex regulation of the KEAP1/NRF2 system (Figure 1) [12].
Figure 1.
Overview of the main genetic and epigenetic modifications that lead to KEAP1-NFE2L2 impairment and constitutive NRF2 nuclear accumulation in cancer cells. NFE2L2 gene copy number variations (CNV), oncogene activity (KRAS, BRAF, MYC, and PTEN), DNA promoter methylation, and miRNAs contribute in a synergic manner to increase cancerous NRF2 activity as a result of reduction of KEAP1 mRNA or increase of NRF2 mRNA levels and/or protein expression. By contrast, somatic point gain-of-function mutations in NFE2L2 or in loss-of-function in KEAP1 promote the disruption of the interaction between KEAP1 and NRF2 and lead the increase of NRF2 protein quantity which translocates into the nucleus.
This minireview describes the recent updates about the deregulation mechanisms of the KEAP1/NRF2 pathway, with a particular focus on the epigenetic modulation of KEAP1 and NFE2L2 and their cellular significance and potential impact on cancer patient management.
2. The Genetic Deregulation of Keap1/Nrf2 Signaling and Its Translational Impact in Solid Tumors
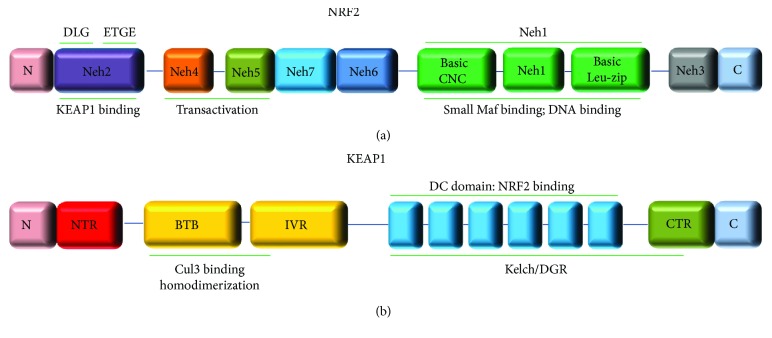
Among the genetic lesions that affect the KEAP1/NRF2 activity, point mutations are the most frequently investigated ones in solid tumors. They commonly occur in the exonic regions that codify for the KEAP1 and NRF2 interaction sites (the Kelch/DGR domain of KEAP1 and the Neh2 domain of NRF2) and induce a general failure of the ubiquitination process led by the KEAP1 (Figure 2).
Figure 2.
Domain architecture of the NRF2 (a) and KEAP1 (b) proteins. (a) NRF2 protein is divided into seven highly conserved domains, Neh1 to Neh7 (NRF2-ECH homology: Neh). The coordinates of NRF2 protein domains are shown as follows: Neh2 (16-89aa); Neh2 DLG motif (17-32aa), Neh2 ETGE motif (77-82aa), Neh4 (111-134aa), Neh5 (182-209aa), Neh7 (209-316aa), Neh6 (337-394aa), Neh1 (435-568aa), and Neh3 (569-605aa). (b) KEAP1 protein contains a number of functional domains including the N-terminal region (NTR; 1-60aa), broad complex, tramtrack and bric-a-brac (BTB; 61-179aa), the intervening linker domain (IVR; 180-314aa), the double glycine/Kelch domain harboring six Kelch-repeat domains (315-359aa; 361-410aa; 412-457aa; 459-504aa; 506-551aa; 553-598aa), and the C-terminal region (CTR; 599-624aa).
By consequence, the NRF2 escapes from proteasomal degradation and increases the ARE-target gene expression with an enhancement of the antioxidant defense system and chemo- and radioresistance of cancer cells [13, 14]. Moreover, since the KEAP1 is able to negatively modulate the BCL-2 and p62 degradation, the KEAP1 point mutations also lead to an accumulation of these proteins with a general deregulation of apoptosis, autophagy, and inflammation [15, 16].
Loss-of-function mutations of the human KEAP1 gene have been firstly reported in NSCLC with a prevalence of about 20–25%. These mutations were frequently observed in the lung papillary subtype and in TTF-1 negative lung adenocarcinoma [10, 17, 18]. Moreover, KEAP1 point mutations were identified in several human cancers such as gastric (11.1%), liver (2–8%), colorectal (7.8%), prostate (1.3%), gallbladder (30.7%), ovarian (37%), glioma (1.7%), head and neck (42%), and clear renal cell carcinoma (4.7%) [19–29]. More recently, Fernandez-Cuesta et al. and Derks reported KEAP1 genetic alterations as a new uncovered molecular hallmark of LCNEC (lung cancer neuroendocrine) with adenocarcinoma-like features [30, 31]. This last finding was also confirmed by a different group which reported a prevalence of KEAP1-NFE2L2 (31%) alterations in tumors with high neuroendocrine gene expression, mainly cooccurrent with gene mutations [4, 32, 33].
Gain-of-function NFE2L2 mutations are generally mutually exclusive with respect to KEAP1 mutations and are frequently located into the DLG or ETGE motifs. NFE2L2 point mutations were identified in several tumors with squamous histological features, such as esophageal, skin, lung, and laryngeal carcinomas. An increased NFE2L2 gene copy number was also described in lung squamous cell carcinoma. An increased NFE2L2 gene copy number was also described in lung squamous cell carcinoma. All of these mutations are generally missense changes that interfere with the KEAP1 ability to bind to NRF2, thus inducing an escape of NRF2 degradation without changing its gene functionality [34–37]. Somatic lesions linked to KEAP1/NRF2 axis deregulation were also reported in the CUL3 gene, the component of the E3 ligase complex KEAP1/CUL3/RBX1 that marks NRF2 for proteasomal degradation [7, 38]. Mutations in CUL3, together with those in NFE2L2, are frequent in hereditary type 2 papillary renal cell carcinoma (PRCC2). In squamous carcinoma of the head and neck, somatic lesions of CUL3/NFE2L2/KEAP1 have a prevalence of 64% and were associated with a lower patient overall survival (Tables 1 and 2) [25, 39–41].
Table 1.
Functionally investigated KEAP1 gene mutations in tumor tissues and cell lines.
| Cancer tissue or cell line types | Nucleotide change | Amino acid change | Mutation type/clinical prediction | Protein domain | Functional effects of KEAP1 mutant |
|---|---|---|---|---|---|
| Breast cell line and ductal carcinoma | c.68G>A | p.C23Y | Missense/pathogenic | NTR | Repression of NRF2-dependent transcription activity and ubiquitination defects |
| Lung AC, lung SCC | c.212G>T | p.R71L | Missense/pathogenic | BTB | Wild-type behavior |
| Stomach AC | c.246G>T | p.Q82H | Missense/pathogenic | BTB | Impaired effect on NRF2 pathway activation |
| EOC | c.319T>C | p.F107L | Missense/pathogenic | BTB | Enhance the NRF2 nuclear localization and its transcription activity |
| BUC, EOC | c.347G>C | p.R116P | Missense/pathogenic | BTB | Enhance the NRF2 nuclear localization and its transcription activity |
| Lung AC, lung SCC | c.463G>T | p.V155F | Missense/pathogenic | BTB | Enhance the binding of KEAP1 to NRF2 and facilitate NRF2 ubiquitination |
| EOC | c.475G>A | p.A159T | Missense/pathogenic | BTB | Enhance the NRF2 nuclear localization and its transcription activity |
| Lung AC, lung SCC | c.499G>T | p.V167F | Missense/pathogenic | BTB | Weakly affect the bind of KEAP1 to NRF2 without suppressing the NRF2 activity |
| BTC | c.543_544insC | p.S181fs∗11 | Frameshift/NS | IVR | Induce the loss of KEAP1 repression activity on NRF2 |
| HCC | c.548A>G | p.N183S | Missense/pathogenic | IVR | Induce an impaired binding of KEAP1 to the CUL3 ubiquitin ligase |
| Lung AC | c.556G>C | p.G186R | Missense/pathogenic | IVR | Induce an enhanced binding of KEAP1 to NRF2 and facilitate its ubiquitination without suppressing NRF2-mediated transcription |
| EOC | c.563C>T | p.A188V | Missense/pathogenic | IVR | Enhance activation of NRF2 pathway and an increase of its transcriptional activity and nuclear localization |
| Lung AC | c.599A>C | p.H200P | Missense/pathogenic | IVR | Wild-type behavior |
| Lung SCC | c.671C>A | p.S224Y | Missense/pathogenic | IVR | Wild-type behavior |
| Lung SCC | c.691C>G | p.L231V | Missense/pathogenic | IVR | Wild-type behavior |
| Stomach AC | c.698G>A | p.S233N | Missense/pathogenic | IVR | Induce an impaired binding of KEAP1 to the CUL3 ubiquitin ligase |
| CESC, colorectal AC | c.700C>T | p.R234W | Missense/pathogenic | IVR | Induce an impaired binding of KEAP1 to the CUL3 ubiquitin ligase |
| Lung AC | c.706G>C | p.D236H | Missense/pathogenic | IVR | Reduce KEAP1-mediated repression of NRF2 |
| Lung SCC, liver | c.706G>T | p.D236Y | Missense/pathogenic | IVR | Induce an impaired binding of KEAP1 to the CUL3 ubiquitin ligase |
| Lung AC | c.711delG | p.L237fs∗1 | Frameshift (stop codon)/NS | IVR | Reduce KEAP1-mediated repression of NRF2 |
| Lung AC | c.724G>A | p.E242K | Missense/pathogenic | IVR | Induce an impaired binding of KEAP1 to the CUL3 ubiquitin ligase |
| Lung SCC | c.728C>G | p.S243C | Missense/pathogenic | IVR | Induce an enhanced binding of KEAP1 to NRF2 and facilitate its ubiquitination without suppressing NRF2-mediated transcription |
| BUC, lung AC | c.730G>A | p.E244K | Missense/pathogenic | IVR | Induce an impaired binding of KEAP1 to the CUL3 ubiquitin ligase |
| BTC, stomach | c.746G>A | p.C249Y | Missense/pathogenic | IVR | Mutant KEAP1 fails to repress NRF2-dependent transactivation |
| Breast AC | c.767A>G | p.D256G | Missense/pathogenic | IVR | Induce an impaired binding of KEAP1 to the CUL3 ubiquitin ligase |
| PF | c.790G>A | p.V264I | Missense/pathogenic | IVR | Reduce KEAP1-mediated repression of NRF2 |
| Lung AC | c.814C>T | p.R272C | Missense/pathogenic | IVR | Reduce KEAP1-mediated repression of NRF2 (impaired Nrf2 degradation) |
| Stomach AC | c.838T>C | p.F280L | Missense/pathogenic | IVR | Induce an impaired binding of KEAP1 to the CUL3 ubiquitin ligase |
| Stomach AC | c.842T>C | p.L281P | Missense/pathogenic | IVR | Induce an impaired binding of KEAP1 to the CUL3 ubiquitin ligase |
| Lung AC, lung LCC | c.851A>T | p.Q284L | Missense/pathogenic | IVR | Reduce KEAP1-mediated repression of NRF2 |
| Stomach AC | c.863G>A | p.C288Y | Missense/pathogenic | IVR | Induce and impair binding of KEAP1 to NRF2 and facilitate NRF2 ubiquitination and its degradation |
| Lung AC, liver | c.880G>T | p.D294Y | Missense/pathogenic | IVR | Lead to deleterious effect on protein stability |
| Lung SCC | c.953C>T | p.P318L | Missense/pathogenic | KELCH1 | Wild-type behavior |
| Lung SCC | c.? | p.P318_fs | Frameshift/NS | KELCH1 | Impact on the KEAP1-NRF2 association and NRF2 degradation |
| EOC | c.1234C>T | p.P319S | Missense/NS | KELCH1 | Enhance activation of NRF2 pathway and an increase of its transcriptional activity and nuclear localization |
| Lung SCC | c.959G>A | p.R320Q | Missense/pathogenic | KELCH1 | Induce an enhanced binding of KEAP1 to NRF2 and facilitate its ubiquitination without suppressing NRF2-mediated transcription |
| Lung AC, lung SCC | c.965C>T | p.P322L | Missense/pathogenic | KELCH1 | Lead to deleterious effects on KEAP1 protein stability |
| Colorectal AC | c.989C>T | p.T330I | Missense/pathogenic | KELCH1 | Impair the KEAP1 binding to NRF2 through the KEAP1 DC pocket (lower affinity) |
| Lung AC | c.994G>T | p.G332C | Missense/pathogenic | KELCH1 | Induce an enhancement of the NRF2 activity |
| Gallbladder | c.996_996delC | p.G332fs∗67 | Frameshift/NS | KELCH1 | Lead a loss of NRF2 repression by KEAP1 |
| Lung AC | c.997G>T | p.G333C | Missense/pathogenic | KELCH1 | Induce misfolding effects and decrease the KEAP1 stability and capability to bind NRF2 |
| Lung | c.1001>T | p.Y334F | Missense/NS | KELCH1 | Disrupt the integrity of the Kelch domain of KEAP1 |
| HCC | c.1007G>A | p.R336Q | Missense/pathogenic | KELCH1 | Impair the KEAP1 binding to NRF2 through the KEAP1 DC pocket (lower affinity) |
| Gallbladder AC, breast AC | c.1013C>T | p.S338L | Missense/pathogenic | KELCH1 | Mutant KEAP1 fails to repress NRF2-dependent transactivation |
| HCC | c.1024C>A | p.L342M | Missense/pathogenic | KELCH1 | Impair the KEAP1 binding to NRF2 through the KEAP1 DC pocket (lower affinity) |
| Lung AC | c.1036InsT | p.S346_fs | Frameshift (stop codon)/pathogenic | KELCH1 | Lead to a premature termination and truncated KEAP1 protein |
| PF | c.1043insG | p.348_fs | Frameshift (stop codon)/NS | KELCH1 | Result in a frameshift and produce a truncated KEAP1 protein, with a lower KEAP1-mediated repression of NRF2 |
| Lung AC, stomach cell lines | c.1048G>A | p.G350S | Missense/NS | KELCH1 | Reduce KEAP1-mediated repression of NRF2 |
| Prostate | c.1069G>A | p.D357N | Missense/pathogenic | KELCH1 | Impair the KEAP1 binding to NRF2 through the KEAP1 DC pocket (lower affinity) |
| Colorectal AC | c.1075C>T | p.Q359X | Nonsense/pathogenic | KELCH1 | Impair the KEAP1 binding to NRF2 through the KEAP1 DC pocket (lower affinity) |
| Lung AC samples and cell lines | c.1090G>T | p.G364C | Missense/pathogenic | KELCH2 | Abolish the KEAP1-NRF2 interaction |
| Lung AC | c.GCC1098TTA | p.L367_fs | Frameshift/pathogenic | KELCH2 | Produce a truncated KEAP1 protein |
| Lung AC | c.1106T>C | p.V369A | Missense/pathogenic | KELCH2 | Lead to deleterious effects on KEAP1 protein stability |
| Gallbladder AC, HCC | c.1136G>A | p.G379D | Missense/pathogenic | KELCH2 | Mutant KEAP1 fails to repress NRF2-dependent transactivation. Induce a misfolding effects on the KEAP1 protein and decrease its ability to bind NRF2 |
| Lung AC | c.1238G>T | p.L413R | Missense/pathogenic | KELCH3 | Mutant KEAP1 fails to repress NRF2-dependent transactivation. Induce misfolding effects on the KEAP1 protein and decrease its ability to bind NRF2 |
| Lung AC | c.DelGG? | p.L413_fs | Frameshift (stop codon)/NS | KELCH3 | Reduce KEAP1-mediated repression of NRF2 |
| Lung AC | c.1243C>G | p.R415G | Missense/pathogenic | KELCH3 | Affect the ability of KEAP1 to repress NRF2 and lost the ability to bind and sequester NRF2 in the cytoplasm |
| Lung SCC, ESCC | c.1264G>A | p.D422N | Missense/pathogenic | KELCH3 | Enhance the binding of KEAP1 to NRF2 and facilitate NRF2 ubiquitination |
| Lung AC, lung SCC | c.1268G>T | p.G423V | Missense/pathogenic | KELCH3 | Enhance the binding of KEAP1 to NRF2 and facilitate NRF2 ubiquitination |
| Lung AC | c.1280C>T | p.A427V | Missense/pathogenic | KELCH3 | Reduce KEAP1-mediated NRF2 repression ability but Kelch domain should still be able to interact effectively with the ETGE and the DLG sites of NRF2 |
| Lung AC | c.1288G>T | p.G430C | Missense/pathogenic | KELCH3 | Induce a misfolding effect on the KEAP1 protein and decrease its ability to bind NRF2 and sequester NRF2 in the cytoplasm. |
| Lung AC cell line | c.1329T>G | p.Y443_fs | Frameshift (stop codon)/NS | KELCH3 | Reduce KEAP1-mediated repression of NRF2 |
| Lung AC | c.1370delG | p.L457fs∗1 | Frameshift (stop codon)/NS | KELCH3 | Result in a frameshift and produce a truncated KEAP1 protein, with a lower KEAP1-mediated repression of NRF2 |
| Lung AC | c.1396G>C | p.A466P | Missense/pathogenic | KELCH4 | Lead to deleterious effects on KEAP1 protein stability |
| Lung SCC | c.? | p.N469fs | Frameshift/NS | KELCH4 | Impact on the KEAP1-NRF2 association and the KEAP1 ability to suppress NRF2 |
| Lung AC, lung SCC, ESCC, UADT | c.1408C>T | p.R470C | Missense/pathogenic | KELCH4 | Exhibit enhanced binding to NRF2 and facilitate NRF2 ubiquitination |
| Lung LCC | c.1426G>A | p.G476R | Missense/NS | KELCH4 | Induce a misfolding effect on the KEAP1 protein and decrease its ability to bind NRF2 and sequester NRF2 in the cytoplasm. |
| Lung SCC | c.1438G>T | p.G480W | Missense/pathogenic | KELCH4 | Reduce the KEAP1-NRF2 binding |
| Lung AC | c.1448G>A | p.R483H | Missense/pathogenic | KELCH4 | Reduce the KEAP1-NRF2 binding |
| Lung AC | c.1477G>C | p.E493Q | Missense/pathogenic | KELCH4 | Induce an upregulation of the NRF2 activity |
| Lung SCC | c.1632G>T | p.W544C | Missense/pathogenic | KELCH5 | Reduce the KEAP1-NRF2 binding |
| Liver, lung AC | c.1661G>A | p.R554Q | Missense/pathogenic | KELCH6 | Reduce the KEAP1-NRF2 binding |
| Liver | c.1662G>A | p.W554X | Missense/pathogenic | KELCH6 | Decrease the NRF2 repression activity |
| PF | c.1663_1680del18 | p.S555_T560del | In frame/NS | KELCH6 | Reduce KEAP1-mediated repression of NRF2 |
| Lung AC | c.1709G>T | p.G570V | Missense/pathogenic | KELCH6 | Reduce the KEAP1-NRF2 binding |
| Lung AC | c.1772G>T | p.W591L | Missense/pathogenic | KELCH6 | Impair the KEAP1 binding to NRF2 through the KEAP1 DC pocket (lower affinity) |
| Colorectal AC | c.1816G>A | p.V606M | Missense/pathogenic | CTR | Induce an upregulation of the NRF2 activity |
| EOC | c.1831G>A | p.E611K | Missense/pathogenic | CTR | Enhance activation of NRF2 pathway and an increase of its transcriptional activity and nuclear localization |
Cosmic (Catalogue of Somatic Mutations in Cancer) database IP (http://cancer.sanger.ac.uk/cosmic/gene/analysis?ln=KEAP1#variants). AC: adenocarcinoma; BUC: bladder urothelial carcinoma; CESC: cervical squamous cell carcinoma; DC: C-terminal β-propeller domain; EOC: epithelial ovarian cancer; ESCC: esophageal squamous cell carcinoma; HCC: hepatocellular carcinoma; LCC: large cell carcinoma; PF: pleural fluid; SCC: squamous cell carcinoma; UADT: upper aerodigestive tract; NS: not specified.
Table 2.
Functional investigated NFE2L2 gene mutations in tumor tissues and cell lines.
| Cancer tissue or cell line types | Nucleotide change | Amino acid change | Mutation type/clinical prediction | Protein domain | Functional effects of NFE2L2 mutant |
|---|---|---|---|---|---|
| HCC | c.68T>G | p.L23R | Missense/pathogenic | Neh2 DLG | Disrupt the intramolecular interactions for KEAP1-DLGex binding and are associated with the strongest increase of NRF2 activity |
| PRCC, ESCC | c.70T>C | p.W24R | Missense/pathogenic | Neh2 DLG | NFE2L2 mutant with gain-of-function activity, which is partly resistant to KEAP1-mediated inhibition |
| Lung SCC, SCLC, ESCC | c.72G>C | p.W24C | Missense/pathogenic | Neh2 DLG | Affect the binding to the KEAP1 dimer and inhibit the KEAP1-mediated degradation of NRF2 and a stronger increase of the NRF2 activity |
| ESCC | c.76C>G | p.Q26E | Missense/pathogenic | Neh2 DLG | NFE2L2 mutant with gain-of-function activity, which is partly resistant to KEAP1-mediated inhibition |
| Lung SCC | c.77A>T | p.Q26L | Missense/pathogenic | Neh2 DLG | Only present in TCGA report |
| Lung SCC | c.77A>C | p.Q26P | Missense/pathogenic | Neh2 DLG | Only present in TCGA report |
| HCC | c.78A>C | p.Q26H | Missense/pathogenic | Neh2 DLG | Lead to an activation of NRF2 signaling |
| Lung SCC | c.79G>C | p.D27H | Missense/pathogenic | Neh2 DLG | Only present in TCGA report |
| ESCC | c.79G>T | p.D27Y | Missense/pathogenic | Neh2 DLG | Block proper KEAP1-NRF2 binding and inhibit the KEAP1-mediated degradation of NRF2 |
| Lung SCC, ESCC | c.83T>C | p.I28T | Missense/pathogenic | Neh2 DLG | Lead to weaker KEAP1-binding DLG region and inhibit the KEAP1-mediated degradation of NRF2 |
| HCC, lung AC, SCC-UADT | c.85G>C | p.D29H | Missense/pathogenic | Neh2 DLG | Lead and increase NRF2 levels |
| Lung SCC | c.85G>A | p.D29N | Missense/pathogenic | Neh2 DLG | Inhibit the KEAP1-mediated degradation of NRF2, resulting in a stabilization and a nuclear accumulation of NRF2 |
| Cervix SCC, PRCC, lung AC, lung SCC | c.85G>T | p.D29Y | Missense/pathogenic | Neh2 DLG | Lead to a constitutive activation of NRF2 at E3 ligase recognition sites |
| HCC, lung SCC, ESCC, SCC-UADT | c.86A>G | p.D29G | Missense/pathogenic | Neh2 DLG | Lead to weaker KEAP1-binding DLG region and inhibit the KEAP1-mediated degradation of NRF2 |
| ccRCC | c.86A>T | p.D29V | Missense/pathogenic | Neh2 DLG | Lead to a constitutive activation of NRF2 at E3 ligase recognition sites |
| Liver, lung SCC, ESCC, skin, SCC-UADT | c.88C>T | p.L30F | Missense/pathogenic | Neh2 DLG | Affect the binding ability of NRF2 to the KEAP1 dimer with a lower NRF2 ubiquitination and an enhancement of its transcriptional activity into the nucleus |
| EEA | c.89T>G | p.L30R | Missense/pathogenic | Neh2 DLG | Disrupt the KEAP1/NRF2 interaction due to lack of binding of NRF2 to Kelch domain of KEAP1 |
| Central nervous system | c.91G>A | p.G31R | Missense/pathogenic | Neh2 DLG | Gain-of-function mutation with an increased NRF2 stabilization |
| ccRCC, lung SCC, ESCC, skin SCC | c.92G>C | p.G31A | Missense/pathogenic | Neh2 DLG | NFE2L2 mutant with a gain-of-function activity, which is partly resistant to KEAP1-mediated inhibition |
| ESCC | c.92G>A | p.G31E | Missense/pathogenic | Neh2 DLG | Affect the binding ability of NRF2 to interact with the Kelch domain of KEAP1 |
| SCC-UADT, skin SCC | c.93_95delAGT | p.V32del | In frame/NS | Neh2 DLG | Lead to weaker KEAP1-binding DLG region and inhibit the KEAP1-mediated degradation of NRF2 |
| HCC | c.95T>A | p.V32E | Missense/pathogenic | Neh2 DLG | Mutational target that leads to its aberrant activation |
| Lung SCC | c.95T>G | p.V32G | Missense/pathogenic | Neh2 DLG | Lead to weaker KEAP1-binding DLG region and inhibit the KEAP1-mediated degradation of NRF2 |
| EEA, lung SCC | c.100C>G | p.R34G | Missense/pathogenic | Neh2 | Inhibit the KEAP1-mediated degradation of NRF2, resulting in an increase of its stabilization and nuclear accumulation |
| Lung SCC, ESCC | c.101G>C | p.R34P | Missense/pathogenic | Neh2 | Lead to a constitutive activation of NRF2 at E3 ligase recognition sites |
| Cervix SCC, lung SCC, ESCC, SCC-UADT | c.101G>A | p.R34Q | Missense/pathogenic | Neh2 | Lead to weaker KEAP1-binding DLG region and inhibit the KEAP1-mediated degradation of NRF2 |
| PRCC | c.105_107delAGT | p.V36del | In frame/NS | Neh2 | NFE2L2 mutant is insensitive to KEAP1-mediated degradation (NFE2L2 mutant is stable even with ectopic expression of KEAP1 occurs) |
| ESCC, UADT | c.225A>C | p.Q75H | Missense/pathogenic | Neh2 | Impair two-site substrate of KEAP1 recognition and inhibit the KEAP1-mediated degradation of NRF2 |
| SCC-UADT | c.229G>A | p.D77N | Missense/pathogenic | Neh2 ETGE | Block the KEAP1-NRF2 binding and inhibit the KEAP1-mediated degradation of NRF2 |
| Liver | c.229G>T | p.D77Y | Missense/pathogenic | Neh2 ETGE | Affect the NRF2 binding to Kelch domain surface of the KEAP1 |
| Lung SCC | c.230A>C | p.D77A | Missense/pathogenic | Neh2 ETGE | Block the KEAP1-NRF2 binding and inhibit the KEAP1-mediated degradation of NRF2 |
| HCC, lung SCC, ESCC | c.230A>G | p.D77G | Missense/pathogenic | Neh2 ETGE | NFE2L2 mutant with a gain-of-function activity, partly resistant to the KEAP1-mediated inhibition |
| Lung SCC,ESCC | c.230A>T | p.D77V | Missense/pathogenic | Neh2 ETGE | Compromise the association of NRF2 with KEAP1-DC and inhibit the KEAP1-mediated degradation of NRF2 |
| ESCC | c.232G>A | p.E78K | Missense/pathogenic | Neh2 ETGE | NFE2L2 mutant with gain-of-function activity, which is partly resistant to the KEAP1-mediated inhibition |
| Lung SCC, ESCC | c.235G>A | p.E79K | Missense/pathogenic | Neh2 ETGE | Reduce the ability of NRF2 to interact with KEAP1 and inhibit the KEAP1-mediated degradation of NRF2, thus promoting the nuclear localization and transcriptional activity of NRF2 |
| Cervix SCC, lung AC, lung SCC, SCC-UADT | c.235G>C | p.E79Q | Missense/pathogenic | Neh2 ETGE | Compromise the association of NRF2 with KEAP1-DC and inhibit the KEAP1-mediated degradation of NRF2 |
| HCC, SCC-UADT | c.236A>G | p.E79G | Missense/pathogenic | Neh2 ETGE | Block the KEAP1-NRF2 binding and inhibit the KEAP1-mediated degradation of NRF2 |
| HCC, ESCC | c.238A>C | p.T80P | Missense/pathogenic | Neh2 ETGE | NFE2L2 mutant with a gain-of-function activity, partly resistant to the KEAP1-mediated inhibition |
| HCC, UADT | c.239C>T | p.T80I | Missense/pathogenic | Neh2 ETGE | Impair the two-site substrate recognition of KEAP1 and inhibit KEAP1-mediated degradation of NRF2 |
| Lung SCC | c.239C>G | p.T80R | Missense/pathogenic | Neh2 ETGE | Reduce the ability of NRF2 to interact with KEAP1 |
| PRCC, lung SCC, ESCC | c.239C>A | p.T80K | Missense/pathogenic | Neh2 ETGE | Compromise the association of NRF2 with KEAP1-DC. Also inhibit KEAP1-mediated degradation of NRF2 and promote nuclear localization and transcriptional activity of NRF2 |
| HCC, lung SCC | c.241G>A | p.G81S | Missense/pathogenic | Neh2 ETGE | NFE2L2 mutant with gain-of-function activity, with an increased NRF2 stabilization due to alteration of the binding ability to KEAP1 |
| Breast, lung AC, lung SCC, ESCC | c.242G>A | p.G81D | Missense/pathogenic | Neh2 ETGE | NFE2L2 mutant with a gain-of-function activity, partly resistant to the KEAP1-mediated inhibition |
| HCC, lung SCC, ESCC | c.242G>T | p.G81V | Missense/pathogenic | Neh2 ETGE | Block the KEAP1-NRF2 binding and inhibit the KEAP1-mediated degradation of NRF2 |
| HCC, lung AC, lung SCC, ESCC | c.244G>C | p.E82Q | Missense/pathogenic | Neh2 ETGE | Block the KEAP1-NRF2 binding and inhibit the KEAP1-mediated degradation of NRF2 |
| PRCC, HCC, lung SCC, UADT | c.245A>G | p.E82G | Missense/pathogenic | Neh2 ETGE | Stabilize NRF2 by disrupting its ability to bind KEAP1 although the NRF2 transcriptional activity remains unchanged |
| ESCC | c.245A>T | p.E82V | Missense/pathogenic | Neh2 ETGE | Affect the repressive activity of KEAP1 on NRF2 signaling |
| HCC, lung AC, ESCC | c.246A>C | p.E82D | Missense/pathogenic | Neh2 ETGE | Impair the two-site substrate recognition of KEAP1 and inhibit KEAP1-mediated degradation of NRF2 |
Cosmic (Catalogue of Somatic Mutations in Cancer) database IP (http://cancer.sanger.ac.uk/cosmic/gene/analysis?ln=NFE2L2#variants). AC: adenocarcinoma; ccRCC: clear cell renal cell carcinoma; DC: C-terminal β-propeller domain; DLGex: extended DLG motif; EEA: endometrioid endometrial adenocarcinoma; ESCC: esophageal squamous cell carcinoma; HCC: hepatocellular carcinoma; PRCC: papillary renal cell carcinoma; SCC: squamous cell carcinoma; SCLC: small cell lung cancer; UADT: upper aerodigestive tract; NS: not specified.
Dysfunction of the KEAP1/NRF2 axis by genetic mutations is gradually becoming a milestone to understand cancer development, progression, and resistance to conventional and biological treatments [42]. It is now well known that loss-of-function mutations of the KEAP1 gene or gain-of-function mutations in NFE2L2 enhance the resistance of cancer cells to anticancer drugs, such as etoposide and carboplatin, and it is associated with poor outcome of platinum-based advanced NSCLC patients [43]. Nuclear accumulation of NRF2 was also correlated with a poor survival of lung SqCC and pancreatic adenocarcinomas and a worse progression free survival (PFS) in patients treated with surgery only [44–47]. Aberrant NRF2 activation due to KEAP1 alterations is also reported as one of the molecular mechanisms of chemoresistance of gallbladder cancer under 5-FU-based regimen and of colorectal cancer under demethylase and methyltransferase treatments [20, 48, 49].
Jeong and coworkers suggested a new role for KEAP1 and NFE2L2 mutations in radiotherapy resistance of NSCLC patients and in identifying patients who might benefit from radiation dose escalation [50]. Knockdown experiments reported that radiochemosensitization was led by CDK20 that competes with NRF2 for KEAP1 binding and induces nuclear translocation of NRF2 and the enhancement of its transcriptional activity. This ultimately results in proliferation defects and provides new insights into the cellular response to NRF2-mediated DNA damage [51].
An interesting link between the KEAP1/NRF2 axis and target therapies was recently reported. Cell proliferation in cancer was demonstrated to be cross-regulated by KEAP1/NRF2 and EGFR signaling. Moreover, cells expressing oncogenic allele of KRAS are able to activate NRF2 via the MAPK pathway in mouse embryonic fibroblasts [52, 53]. In the same way, the loss of KEAP1 by the CRISPR-Cas9 system cooperates with the tumor mutational landscape in modulating the response to BRAF, MEK, EGFR, and ALK inhibition and in allowing cancer cells to increase their ability to resist to treatments and proliferate [54]. KRAS activity confers in NSCLC chemoresistance also by upregulating NRF2 through the link with TPA response element (TRE) located in exon 1 of the NFE2L2. In the same context of resistance to target therapy, it is possible that NFE2L2 mutations can contribute to survival under crizotinib treatment and can allow the cells to acquire additional resistance mutations over time. In line with these hypotheses, Krall et al. recently identified a hotspot mutation in NFE2L2 in a patient with acquired resistance to ALK inhibitors that could exert a synergic effect with a secondary ALK mutation in the resistance to second-generation ALK inhibitors [55].
Recent additional studies in this field gave the first hint of the prognostic role of single-nucleotide polymorphisms (SNPs) of the KEAP1 gene in breast cancer without inducing any evident and detectable variations of the protein structure or conformation. More specifically, five tagging SNPs (rs34197572, rs9676881, rs1048290, rs11085735, and rs8113472) located in the KEAP1 were genotyped and appeared to be in allelic linkage disequilibrium (LD) with each other. This finding suggests the existence of a haplotype block at the KEAP1 gene locus that might correlate with specific clinical features of cancer patients [56]. The two SNPs rs9676881 and rs1048290 resulted to be significantly associated with a shorter PFS survival in invasive breast cancer patients. The main hypothesis is that they reside into cell type-specific regulatory elements that modulate the binding capability of critical transcriptional factors, which in turn change target gene expression. Thus, it might explain the observed correlation with the high KEAP1 protein expression levels and the high cytoplasmic localization of NRF2 in breast tissues [57]. The SNP rs1048290 is located in the DGR domain, so it may affect the maintenance of physiological levels of NRF2.
Tumor susceptibility SNPs might be also associated with specific miRNA/lncRNA binding regions [58, 59]. The SNP rs1048290 was found in LD with the SNP rs9676881, which is located in a putative enhancer region, few bases downstream of the 3′-untraslated region (3′-UTR) of the KEAP1 gene and 410 bp from the miR-200a binding site. By consequence, it is clear to suppose that a LD may exist with these silent variations and the specific miRNA binding site. However, the role of KEAP1 SNPs in predicting patient survival remains controversial. The two SNPs rs9676881 and rs1048290 appeared to be the most interesting ones and resulted to be significantly associated with a shorter PFS survival in both invasive and ER-positive tamoxifen-treated invasive breast cancer patients [60].
3. The Aberrant Methylation of the Keap1-Nrf2 Axis and Its Translational Impact in Solid Tumors
Gene promoter hypermethylation at the specific CpGs and chromatin remodeling are two of the main epigenetic events that can modulate gene expression by spatial interfering with the ability to work with the transcriptional machinery.
Epigenetic mechanisms are clearly implicated in the complex regulation of the KEAP1/NRF2 axis and are actually considered the most frequent mechanisms of KEAP1 silencing in solid tumors [61]. The first hypothesis of an epigenetic dysregulation of the KEAP1 gene comes from the intriguing observation that the KEAP1 mutations were not frequent enough to justify alone the frequency of aberrant NRF2 nuclear accumulation reported in lung tumor cells [8]. All the scientific findings on the hypermethylation of the KEAP1 promoter and its effects on the KEAP1/NRF2 pathway are summarized in Table 3. The first report in this field was in human NSCLC and prostate DU-145 cancer cell lines. The promoter CpGs affected by this phenomenon are grouped into one island located at the P1 region of KEAP1, near the transcriptional start site [62–64]. The KEAP1 promoter hypermethylation was described in neoplastic tissues of patients affected by glioma, breast cancer (51%), and primary NSCLC (47%). In lung cancer, the presence of epigenetic abnormalities in the KEAP1 gene plus its point mutations/LOH matched with the prevalence of NRF2 nuclear accumulation in NSCLC tissues and was associated with an increased risk of lung cancer progression in surgically resected patients [65–67]. In clear renal cell carcinoma (ccRCC), the epigenetic modulation of KEAP1 was shown to be the leading mechanism of KEAP1 deregulation (48.6%), thus supporting a driver role of the KEAP1/NRF2 axis in renal cancer. TCGA (The Cancer Genome Atlas) concomitant data analysis suggested that KEAP1 hypermethylation is able to strongly predict patient survival [68]. In primary breast cancers and preinvasive lesions, an aberrant KEAP1 promoter methylation was seen to be more recurrent in ER-positive, HER2-negative than in triple-negative breast cancers and was hypothesized to be a prognostic marker since a higher mortality risk in triple-negative patients was predicted. Moreover, KEAP1 promoter silencing by methylation was also predictive of a lower risk of tumor relapse in patients treated with sequential therapy of anthracyclines and cyclophosphamide followed by taxanes [67]. Gliomas are the second tumor described by our group to have a promoter hypermethylation. In these tumors, it was reported that KEAP1 epigenetic modifications were associated with poor prognosis and contribute to the prediction of the disease progression of patients subjected to radiotherapy and temozolomide treatment [65]. The role of KEAP1/NRF2 in radiation has been also elucidated in A549 lung adenocarcinoma cell line under DNMT inhibitor genistein treatment. The pharmacological demethylation of the KEAP1 CpG promoter islands was demonstrated to induce an increase in transcript levels and a consequent overexpression of NRF2, GSS, and HO-1 [69].
Table 3.
Effect of KEAP1/NRF2 expression by promoter methylation in human cancers (tissues and cell lines) and correlation with clinical patients' outcomes.
| Molecular target | Cancer model | Methylation status | Functional effects | Clinical outcome | Refs |
|---|---|---|---|---|---|
| NRF2 | Prostate cancer cell line (LNCaP) and tissues (n = 27) | Hypermethylation | ↓ NRF2 mRNA ↓ HO-1 mRNA and protein ↓ NQO1 mRNA and protein |
Increment of Gleason score from normal to advanced stage prostate cancer | [121] |
| Human colon cancer cells (SNU-C5) | Hypomethylation | ↑ NRF2 mRNA ↑ HO-1 mRNA and protein |
NA | [59, 60] | |
|
| |||||
| KEAP1 | Lung cancer cell lines (SPC-A1, A549, and NCI-H460) and tissues (n = 5) | Hypermethylation | ↓ KEAP1 mRNA ↑ NRF2 protein ↑ HO-1 mRNA and protein ↑ GSH mRNA and protein |
NA | [48,116, 122] |
| NSCLC tissues (n = 47) | Hypermethylation | ↓ KEAP1 mRNA | Worst prognosis associated to KEAP1 double alterations | [52] | |
| Malignant gliomas (n = 86) | Hypermethylation | ↓ KEAP1 mRNA | Lowest risk to progress in patients treated with radiotherapy and temozolomide | [51] | |
| Primary breast cancers (n = 102) and preinvasive breast lesions (n = 14) | Hypermethylation | ↓ KEAP1 mRNA | Worse prognosis in triple-negative phenotype and reduced risk of relapse in patients treated with EC/D chemotherapy | [53] | |
| Human colorectal cancer cell lines (n = 10) and tissues (n = 40) | Hypermethylation | ↓ KEAP1 mRNA ↑ NRF2 protein ↑ NQO1 mRNA ↑ AKR1C1 mRNA |
NA | [55] | |
| Prostate cancer cell DU-145 | Hypermethylation | ↓ KEAP1 mRNA ↑ NRF2 mRNA ↑ NQO1 mRNA ↑ HO-1 mRNA ↑ GCLC mRNA |
NA | [49] | |
| ccRCC tissues (n = 37) TCGA dataset (n = 481) |
Hypermethylation | ↓ KEAP1 mRNA | Worse overall survival (OS) and association with increased of tumor grading | [54] | |
AKR1C1: aldo-keto reductase family 1 member C1; ccRCC: clear renal cell carcinoma; GCLC: glutamate-cysteine ligase catalytic subunit; GSH: glutathione; HO-1: heme oxygenase-1; KEAP1: Kelch-like ECH-associated protein 1; NQO1: NAD(P)H-quinone oxidoreductase 1; NRF2: nuclear factor erythroid 2-related factor 2; NSCLC: non-small-cell lung cancer; NA: not applicable.
Aberrant KEAP1 methylation was also reported in 53% of colorectal cancer and head and neck cancer tissues (29.3%) and was also linked to the worse prognosis of these tumors [70, 71]. In pancreatic cancer cell lines, the suppression of KEAP1 protein was demonstrated to be correlated with UHRF1, a scaffold protein for DNA methyltransferase DNMT1 [72].
A possible role of epigenetic variations in the modulation of NRF2 expression is less investigated. Li and colleagues showed that a low methyltransferase EZH2 expression correlates both lung cancer cell lines and tissues with an elevated expression of NRF2, NQO1 (NAD(P)H-quinone oxidoreductase 1), and HO-1 (heme oxygenase 1). Since the EZH2 is involved in the establishment and/or maintenance of chromatin architecture and histone methylation, its downstream effect was attributed to a decrease in the trimethylation of lysine 27 on histone H3 (H3K27Me3) in the NFE2L2 promoter region [73]. Recently, Kang and colleagues focused on the causative relationship between NRF2 expression and its epigenetic alterations, especially in the context of DNA methylation at cytosines and histone methylation status during 5-fluorouracil- (5-FU-) induced oxidative stress in colon cancer cells. They found that elevated reactive oxygen species (ROS) level induced by 5-FU activates TET (ten-eleven translocation) DNA demethylases and produces a hypomethylation of the NFE2L2 promoter with consequent activation of NRF2 translation. This, in turn, upregulates the expression of the antioxidant enzymes and generates the resistance to 5-FU in cancer cells [48, 49].
4. MicroRNAs Directly Targeting the Keap1/Nrf2 Pathway
An intriguing epigenetic way of KEAP1/NRF2 pathway deregulation in tumor cells comes from miRNAs that act in cancer as oncogenes or tumor suppressors [74]. miRNAs are proximately 22 nucleotide single-stranded noncoding RNA molecules which regulate gene expression at posttranscriptional levels by binding to the 3′-untranslated regions (UTRs) of specific mRNAs. They generally affect the translation or stability of mRNA molecules through the interaction of specific mRNAs with complementary base pairing.
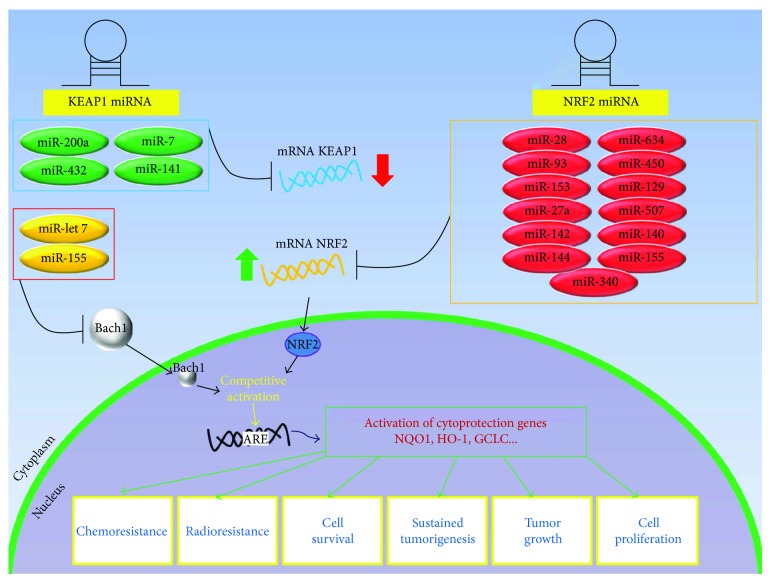
Two different blocks of miRNAs can be distinguished in the context of posttranscriptional regulation of the KEAP1/NRF2 pathway (Table 4) [75]. The first group includes the miRNAs that directly target NFE2L2 and usually negatively regulate the KEAP1/NRF2 pathway by decreasing the NRF2 protein levels. The second one comprises those miRNAs that directly interact with KEAP1 and indirectly influence the NRF2 signaling. In addition, a lot of miRNAs are reported to indirectly modulate the ARE-mediated redox signaling through their interaction with additional factors located in the crossing points of the NRF2 network (Figure 3). All of these interactions are complex and still remain to be fully elucidated. So we focalized our attention on the main findings concerning NRF2 and KEAP1.
Table 4.
Main miRNAs interacting with KEAP1 and NRF2 and downstream effects observed in cancer cells.
| Target | miRNA ID | Functional validations | |||
|---|---|---|---|---|---|
| Downstream effects | Cancer model | Methods | Refs | ||
| NRF2 | ↑ hsa-miR-28 | ↓ NRF2 | Human breast cancer cells | Luciferase assay, qRT-PCR, WB, and coimmunoprecipitation | [76] |
| ↓ hsa-miR-155 | ↑ NRF2, ↑ HO-1, ↑ GSH, ↑ NO, ↑ SOD, ↑ colony formation, ↑ arsenite resistance |
Human bronchiolar epithelial cells | Mimic and miRNA inhibitor transfection, qRT-PCR, WB, measurements of ROS and enzymatic activity, cell cycle, cell migration, and colony formation assays | [78] | |
| ↑ hsa-miR-144 | ↓ NRF2, ↓ GSH, ↓ cell viability, ↑ apoptosis, ↓ 5-FU resistance |
Leukemia cells, human hepatocellular cancer cells, neuroblastoma cells |
Luciferase reporter assay, cell viability assay, ROS and enzymatic activity measurements, qRT-PCR, WB | [82] | |
| MicroRNA microarray analysis, luciferase reporter assay, qRT-PCR, WB, ELISA | [83] | ||||
| Luciferase reporter assay, drug sensitivity assay, qRT-PCR, WB | [84] | ||||
| ↓ hsa-miR-93 | ↑ NRF2, ↑ mammosphere formation, ↓ apoptosis, ↑ DNA damage |
Rat breast cancer cells | siRNA (small interfering RNA) transfection, qRT-PCR, WB, clonogenic cell survival assay, mammosphere formation assay, cell migration, and cell apoptosis assays | [85] | |
| ↑ hsa-miR-153 | ↓ NRF2, ↓ GCLC, ↓ GSR, ↓ cell migration, ↓ cell invasion |
Neuroblastoma cells, breast cancer cells, oral squamous cell carcinoma | miRNA mimic and inhibitor transfection, cell proliferation assay and colony forming assays, cell migration analysis, cell cycle analysis, measurement of ROS and enzymatic activity, qRT-PCR, WB | [87] | |
| MicroRNA microarray analysis, luciferase reporter assay, qRT-PCR, WB, cell migration, and invasion assays | [88] | ||||
| ↑ hsa-miR-27 ↑ hsa-miR 142 | ↓ NRF2, ↓ GCLC, ↓ GSR | Neuroblastoma cells | Transient transfection, WB, qRT-PCR, measurement of ROS, and enzymatic activity | [86] | |
| ↑ hsa-miR-340 | ↓ NRF2, ↓ cisplatin resistance |
Esophageal cancer cells | MicroRNA microarray analysis, luciferase reporter assay, drug sensitivity assay, qRT-PCR, WB | [89] | |
| ↑ hsa-miR-507 ↑ hsa-miR-634 ↑ hsa-miR-450 ↑ hsa-miR-129 |
↓ NRF2, ↓ ME1, ↓ cell growth, ↓ cisplatin resistance |
Esophageal cancer cells | Measurement of ROS, qRT-PCR, WB, siRNA, drug sensitivity assays | [90, 91] | |
|
| |||||
| KEAP1 | ↑ hsa-miR-141 | ↓ KEAP1, ↑ NRF2, ↑ HO-1, ↓ apoptosis, ↑ cisplatin resistance, ↑ 5-FU resistance |
Ovarian cancer cells, hepatocellular carcinoma | MicroRNA microarrays analysis, luciferase reporter assay, qRT-PCR, WB, apoptosis assay | [92] |
| MicroRNA microarray analysis, miRNA mimic and inhibitor transfection, luciferase reporter assay, qRT-PCR, WB, cell viability assay, apoptosis assay, drug sensitivity assay | [93] | ||||
| ↑ hsa-miR-200 | ↓ KEAP1, ↑ NRF2 | Breast cancer cells, esophageal cancer cells | Luciferase reporter assay, qRT-PCR, mRNA stability assay, WB, ChIP, anchorage-independent cell growth assay, IHC | [60] | |
| Transfection reporter assay, qRT-PCR, ChIP | [95] | ||||
| ↑ hsa-miR-7 | ↓ KEAP1, ↑ NRF2, ↑ GSH | Neuroblastoma cells | Cell viability assay, LC-MS/MS, qRT-PCR, WB, enzymatic activity measurements | [96] | |
| ↑ hsa-miR-432 | ↓ KEAP1, ↑ NRF2, ↑ chemoresistance |
Esophageal cancer cells | CRISPR/Cas9 system, cell survival assay, siRNAs, luciferase reporter assay, qRT-PCR, WB, mRNA stability assay, ChIP | [98] | |
GCLC: glutamate-cysteine ligase catalytic subunit; GSH: glutathione; GSR: glutathione reductase; HO-1: heme oxygenase-1; KEAP1: Kelch-like ECH-associated protein 1; ME1: malic enzyme 1; NO: nitric oxide; NRF2: nuclear factor erythroid 2-related factor 2; SOD: superoxide dismutase; 5-FU: 5-fluorouracil; WB: Western blot; FC: flow cytometry; IHC: immunohistochemistry; LC-MS/MS: liquid chromatography tandem mass spectrometry; MTT: (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide) assay; qRT-PCR: quantitative real-time PCR.
Figure 3.
Left and right panels show how miRNA modifications may contribute to down and upregulate the KEAP1/NRF2 signaling in cancer. Representative scheme on the left side summarizes a group of miRNAs that directly target KEAP1 mRNA and indirectly impact on the transcriptional activity of the NRF2 into the nucleus. Other miRNAs modulate BACH1, a transcription factor that competes with NRF2 leading to the link at the antioxidant response element (ARE) of detoxifying genes. The schematic model on the right side depicts those miRNAs that directly target NFE2L2 and impact on the general mRNA and protein levels of NRF2 and, by consequence, on the activation of detoxification NRF2 target genes with a great impact on chemo- and radioresistance, survival, growth, and proliferation of tumor cells.
Several miRNAs predicted to target the KEAP1/NRF2 axis were identified by bioinformatic analysis of miRNA databases [76]. Some of these were experimentally proven to directly target and repress the NRF2 activity. The negative effects on the NRF2 expression by miR-28 were firstly documented in MCF-7 breast cancer cells [77]. A similar activity was described for miR-155 in 16-HBE human bronchiolar epithelial cells under arsenite treatment, together with an observed upregulation of glutathione (GSH), nitric oxide (NO), and superoxide dismutase (SOD) [78]. The increased expression of miR-155 correlates with radiation-induced severe fibrosis in a murine skin model [79], similar to miR-140, whose deficiency increased activation of TGF-β1 signaling, inflammation, and myofibroblast differentiation in fibrotic lung tissue after radiation treatment [80, 81]. Among functionally validated miRNAs that regulate NRF2, miR-144 recently emerged as having a central role in the modulation of cellular stress response in blood malignancies and solid tumors. In K562 cell line and primary erythroid progenitor cells, it was seen that increased levels of miR-144 were associated with reduced NRF2 levels in HbSS reticulocytes. By contrast, inhibition of miR-144-3p in human leukemia HL-60 cells reduced cell viability and prompted apoptosis by interfering with NRF2 activity. In hepatocellular carcinoma cell lines, miR-144 overexpression was reversely correlated with an enhancement of 5-fluorouracil- (5-FU-) induced cytotoxicity and apoptosis and with GSH biosynthesis in neuroblastoma SH-SY5Y cells via NRF2 [82–84].
A direct effect of miR-93 on nuclear accumulation of NRF2 was well described by Singh et al. using a rat model of breast carcinogenesis. A significant reduction in carcinogenesis-associated phenotypes such as mammosphere development, antiapoptosis, and DNA damage was observed [85].
In silico analysis and in vitro studies on different sets of tumor cell lines recently provided more additional insights into the role of KEAP1/NRF2 axis modulation by miRNAs. In SH-SY5Y neuroblastoma cells, the 3′-UTR of NFE2L2 is targeted by miR-153, miR27a, and miR-142-5p, with a consequent decrease in Gclc glutamate-cysteine ligase (GCLC) and glutathione-disulfide reductase (GSR) expression levels [86]. The functional impact of miR-153-3p/NRF2 interaction was firstly reported in breast cancer cell lines and recently highlighted by microarray studies in oral squamous cell carcinoma cell lines and tissues. Low expression levels of miR-153-3p significantly correlate with tumor cell migration and invasion [87, 88]. In the same histological pattern of esophageal cell carcinoma, miR-340 was shown to directly modulate the NRF2 expression levels, thus interfering with the chemoresistance phenotype under cisplatin treatment [89]. Finally, miR-507, miR-634, miR-450a, and miR-129-5p appeared to negatively modulate the NRF2 activity by targeting both the NFE2L2 and ME1 transcripts, a well-known target of NRF2 [90]. In NSCLC A549 cells, this group of miRNAs exerts a synergic effect in increasing sensitivity of cell growth suppression under cisplatin treatment [91].
By looking at the KEAP1 regulation side, miR-141 was the first reported miRNA to target KEAP1 by binding to its 3′-UTR sequence site in ovarian carcinoma cell lines [92]. The upregulation of miR-141 expression decreases the 5-FU-mediated effects and apoptosis in hepatocellular carcinoma cell lines by inducing nuclear translocation of NRF2 and activation of HO-1 gene transcription [93]. A direct inhibition effect of miR-200a on KEAP1 was elucidated in human MDA-MB-231 and Hs578T breast and esophageal squamous cell carcinoma cells under methylseleninic acid (MSA) treatment. MSA acts as a chemopreventive agent that is able to induce miR-200a expression and inhibits KEAP1 through the Krüpple-like factor 4 (KLF4) [60, 94, 95]. Interesting results came from the investigation by Hartikainen et al. In their work, SNP rs1048290 has been found in LD with SNP rs9676881, which is located in a putative enhancer region, few bases downstream of the 3′-untranslated region (3′-UTR) of the KEAP1 gene, the specific target region of miR-200a [56]. More recently, a direct action of miR-7 on KEAP1 expression was described in the human neuroblastoma cells. By targeting the 3′-UTR of KEAP1 mRNA, miR-7 enhances the nuclear localization of NRF2 and induces an increased expression of HO-1 and glutamate-cysteine ligase modifier subunit (GCLM). The control of cell survival under stress by miR-7 was amplified by the observed variation of intracellular hydroperoxide levels and increases in the reduced form of glutathione levels [83, 96]. A similar effect was described for miR-196 in human hepatoma cells against hepatitis C virus infection [97]. The CRISPR/Cas9 system was used to prove the direct binding to the coding region of KEAP1 by miR-432-3p in the esophageal squamous cell carcinoma (ESCC). In this tumor, miR-432-3p overexpression correlates with a downregulation of the KEAP1 expression, thus inducing a decrease in the sensitivity of tumor cells to cisplatin and other chemotherapy drugs [98].
A lot of miRNAs were also reported to regulate the KEAP1/NRF2 pathway independently from the KEAP1 or NRF2 activity. The let-7 family modulates the DICER expression and represents the first example of cancer regulation by miRNA in humans [99]. Not less importantly, let-7 showed to inhibit the expression of several oncogenes involved in cellular proliferation, such as RAS (rat sarcoma), MYC (avian myelocytomatosis viral oncogene homolog), and HMGA2 (high-mobility group AT-hook 2) [100, 101]. The miRNAs let-7b and let-7c were firstly demonstrated to negatively modulate the expression of BACH1 in the liver, a transcription factor that works in association with the small MAF proteins in a dominant condition in respect of NRF2 [102, 103]. By consequence, the repression of BACH1 induces an upregulation of HO-1 expression via NRF2 transcription [104].
5. Long Noncoding RNAs Linked to the Keap1/Nrf2 Pathway
Long noncoding RNAs (lncRNAs) are non-protein-coding transcripts longer than 200 nucleotides which are expressed in a sense, antisense, or bidirectional manner. Different to protein-coding genes, they show a high density of DNA methylation around their transcription start sites, independent of their expression status [105]. A growing number of evidences elucidated the role of lncRNAs in the initiation, progression, and stem cell pluripotency of cancer cells [106]. Little is known about the role of lncRNAs in the modulation of the detoxification processes of cells.
The most recent findings are those related to smoke and cancer-associated lncRNA 1 (SCAL1) and lncRNA regulator of reprogramming (ROR). The SCAL1 is the first characterized long noncoding RNA activated by NRF2 and is considered one of the downstream mediators of NRF2-induced oxidative stress protection in airway epithelial cells. Under stress induced by cigarette smoke, the SCAL1 expression increases in lung cancer cell lines and appears to be directly correlated with NFE2L2 mutations [107]. In human bronchial epithelial cells, a knockdown gene approach revealed that NRF2 can regulate the expression level of SCAL1 by binding to the nuclear factor erythroid-derived 2 (NF-E2) motif located in the promoter region of its gene [108]. Conversely to SCAL1, Zhang and colleagues proved that in breast cells, NRF2 controls the ROR lncRNA expression by binding two different NRF2 response elements flanking the ROR promoter region. NFE2L2 knockdown leads to the overexpression of lncRNA ROR in mammary embryonic stem cells [109].
6. Concluding Remarks
Significant advances have been made in these last years to understand the regulation mechanisms of the KEAP1/NRF2 system. However, although KEAP1/NRF2 dysfunction is now well known to confer resistance to chemo- and radiotherapy, the KEAP1-NFE2L2 mutational status assessment is not used to make treatment decisions in lung cancer yet. Moreover, molecular profiling of these two proteins in pretreated and resistant tumor samples will help to elucidate if the loss of KEAP1 or the gain of NFE2L2 may be clinically relevant mechanisms of acquired and intrinsic resistance to therapies in lung cancer and other solid tumors or not. A general limitation to clarify these issues remains and consists of a lack of available rebiopsy tissue specimens.
From an epigenetic point of view, the effects produced by KEAP1 hypermethylation on the KEAP1/NRF2 signaling in cancer remain partially understood. Firstly, it is natural to wonder what the real role of P1 CpG island methylation is and if the methylation status of KEAP1 exclusively affects its expression or could additionally interfere with the ability to bind to NRF2 in promoting tumor progression and resistance to therapies. According to these observations, it would be of great interest to determine if in tumors with different origins there are similar or different methylation CpG density patterns at the P1 region and if demethylation of the KEAP1 promoter in neoplastic tissues could really suppress tumor progression and enhance resistance to therapies.
Given that posttranscriptional modifications play important roles in regulating the stability and translation of mRNAs, more studies on the regulation of the KEAP1/NRF2 pathway by miRNAs will corroborate their key roles in clinical practice. However, this approach will require a greater knowledge of how drug treatment influences miRNA expression and how miRNA expression could influence the multifaced KEAP1/NRF2 network.
Acknowledgments
This work was supported by the Italian Ministry of Health (Ricerca Corrente, RC1703LO41 to L.A. Muscarella) by “5 × 1000” voluntary contributions to Casa Sollievo della Sofferenza and AIRC/MFAG Grant 12983 (to L.A. Muscarella).
Conflicts of Interest
The authors declare that they have no competing financial interests.
References
- 1.Taguchi K., Yamamoto M. The KEAP1-NRF2 system in cancer. Frontiers in Oncology. 2017;7:p. 85. doi: 10.3389/fonc.2017.00085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Itoh K., Ye P., Matsumiya T., Tanji K., Ozaki T. Emerging functional cross-talk between the Keap1-Nrf2 system and mitochondria. Journal of Clinical Biochemistry and Nutrition. 2015;56(2):91–97. doi: 10.3164/jcbn.14-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hawkins K. E., Joy S., Delhove J. M. K. M., et al. NRF2 orchestrates the metabolic shift during induced pluripotent stem cell reprogramming. Cell Reports. 2016;14(8):1883–1891. doi: 10.1016/j.celrep.2016.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sparaneo A., Fabrizio F. P., Muscarella L. A. Nrf2 and notch signaling in lung cancer: near the crossroad. Oxidative Medicine and Cellular Longevity. 2016;2016:17. doi: 10.1155/2016/7316492.7316492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mcmahon M., Itoh K., Yamamoto M., Hayes J. D. Keap1-dependent proteasomal degradation of transcription factor Nrf2 contributes to the negative regulation of antioxidant response element-driven gene expression. The Journal of Biological Chemistry. 2003;278(24):21592–21600. doi: 10.1074/jbc.M300931200. [DOI] [PubMed] [Google Scholar]
- 6.Bryan H. K., Olayanju A., Goldring C. E., Park B. K. The Nrf2 cell defence pathway: Keap1-dependent and -independent mechanisms of regulation. Biochemical Pharmacology. 2013;85(6):705–717. doi: 10.1016/j.bcp.2012.11.016. [DOI] [PubMed] [Google Scholar]
- 7.Taguchi K., Motohashi H., Yamamoto M. Molecular mechanisms of the Keap1-Nrf2 pathway in stress response and cancer evolution. Genes to Cells. 2011;16(2):123–140. doi: 10.1111/j.1365-2443.2010.01473.x. [DOI] [PubMed] [Google Scholar]
- 8.Solis L. M., Behrens C., Dong W., et al. Nrf2 and Keap1 abnormalities in non-small cell lung carcinoma and association with clinicopathologic features. Clinical Cancer Research. 2010;16(14):3743–3753. doi: 10.1158/1078-0432.CCR-09-3352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chien M. H., Lee W. J., Hsieh F. K., et al. Keap1-Nrf2 interaction suppresses cell motility in lung adenocarcinomas by targeting the S100P protein. Clinical Cancer Research. 2015;21(20):4719–4732. doi: 10.1158/1078-0432.CCR-14-2880. [DOI] [PubMed] [Google Scholar]
- 10.Singh A., Misra V., Thimmulappa R. K., et al. Dysfunctional KEAP1-NRF2 interaction in non-small-cell lung cancer. PLoS Medicine. 2006;3(10, article e420) doi: 10.1371/journal.pmed.0030420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hayes J. D., Mcmahon M. NRF2 and KEAP1 mutations: permanent activation of an adaptive response in cancer. Trends in Biochemical Sciences. 2009;34(4):176–188. doi: 10.1016/j.tibs.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 12.Guo D., Wu B., Yan J., Li X., Sun H., Zhou D. A possible gene silencing mechanism: hypermethylation of the Keap1 promoter abrogates binding of the transcription factor Sp1 in lung cancer cells. Biochemical and Biophysical Research Communications. 2012;428(1):80–85. doi: 10.1016/j.bbrc.2012.10.010. [DOI] [PubMed] [Google Scholar]
- 13.Mitsuishi Y., Motohashi H., Yamamoto M. The Keap1-Nrf2 system in cancers: stress response and anabolic metabolism. Frontiers in Oncology. 2012;2:p. 200. doi: 10.3389/fonc.2012.00200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Padmanabhan B., Tong K. I., Ohta T., et al. Structural basis for defects of Keap1 activity provoked by its point mutations in lung cancer. Molecular Cell. 2006;21(5):689–700. doi: 10.1016/j.molcel.2006.01.013. [DOI] [PubMed] [Google Scholar]
- 15.Tian H., Zhang B., Di J., et al. Keap1: one stone kills three birds Nrf2, IKKβ and Bcl-2/Bcl-xL. Cancer Letters. 2012;325(1):26–34. doi: 10.1016/j.canlet.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 16.Lebovitz C. B., Robertson A. G., Goya R., et al. Cross-cancer profiling of molecular alterations within the human autophagy interaction network. Autophagy. 2015;11(9):1668–1687. doi: 10.1080/15548627.2015.1067362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cardnell R. J. G., Behrens C., Diao L., et al. An integrated molecular analysis of lung adenocarcinomas identifies potential therapeutic targets among TTF1-negative tumors, including DNA repair proteins and Nrf2. Clinical Cancer Research. 2015;21(15):3480–3491. doi: 10.1158/1078-0432.CCR-14-3286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li Q. K., Singh A., Biswal S., Askin F., Gabrielson E. KEAP1 gene mutations and NRF2 activation are common in pulmonary papillary adenocarcinoma. Journal of Human Genetics. 2011;56(3):230–234. doi: 10.1038/jhg.2010.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yoo N. J., Kim H. R., Kim Y. R., An C. H., Lee S. H. Somatic mutations of the KEAP1 gene in common solid cancers. Histopathology. 2012;60(6):943–952. doi: 10.1111/j.1365-2559.2012.04178.x. [DOI] [PubMed] [Google Scholar]
- 20.Shibata T., Kokubu A., Gotoh M., et al. Genetic alteration of Keap1 confers constitutive Nrf2 activation and resistance to chemotherapy in gallbladder cancer. Gastroenterology. 2008;135(4):1358–1368.e4. doi: 10.1053/j.gastro.2008.06.082. [DOI] [PubMed] [Google Scholar]
- 21.Konstantinopoulos P. A., Spentzos D., Fountzilas E., et al. Keap1 mutations and Nrf2 pathway activation in epithelial ovarian cancer. Cancer Research. 2011;71(15):5081–5089. doi: 10.1158/0008-5472.CAN-10-4668. [DOI] [PubMed] [Google Scholar]
- 22.Kanamori M., Higa T., Sonoda Y., et al. Activation of the NRF2 pathway and its impact on the prognosis of anaplastic glioma patients. Neuro-Oncology. 2015;17(4):555–565. doi: 10.1093/neuonc/nou282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nioi P., Nguyen T. A mutation of Keap1 found in breast cancer impairs its ability to repress Nrf2 activity. Biochemical and Biophysical Research Communications. 2007;362(4):816–821. doi: 10.1016/j.bbrc.2007.08.051. [DOI] [PubMed] [Google Scholar]
- 24.Sjoblom T., Jones S., Wood L. D., et al. The consensus coding sequences of human breast and colorectal cancers. Science. 2006;314(5797):268–274. doi: 10.1126/science.1133427. [DOI] [PubMed] [Google Scholar]
- 25.Martinez V. D., Vucic E. A., Thu K. L., Pikor L. A., Lam S., Lam W. L. Disruption of KEAP1/CUL3/RBX1 E3-ubiquitin ligase complex components by multiple genetic mechanisms: association with poor prognosis in head and neck cancer. Head & Neck. 2015;37(5):727–734. doi: 10.1002/hed.23663. [DOI] [PubMed] [Google Scholar]
- 26.Sato Y., Yoshizato T., Shiraishi Y., et al. Integrated molecular analysis of clear-cell renal cell carcinoma. Nature Genetics. 2013;45(8):860–867. doi: 10.1038/ng.2699. [DOI] [PubMed] [Google Scholar]
- 27.Eichenmüller M., Trippel F., Kreuder M., et al. The genomic landscape of hepatoblastoma and their progenies with HCC-like features. Journal of Hepatology. 2014;61(6):1312–1320. doi: 10.1016/j.jhep.2014.08.009. [DOI] [PubMed] [Google Scholar]
- 28.Schulze K., Imbeaud S., Letouzé E., et al. Exome sequencing of hepatocellular carcinomas identifies new mutational signatures and potential therapeutic targets. Nature Genetics. 2015;47(5):505–511. doi: 10.1038/ng.3252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zucman-Rossi J., Villanueva A., Nault J. C., Llovet J. M. Genetic landscape and biomarkers of hepatocellular carcinoma. Gastroenterology. 2015;149(5):1226–1239.e4. doi: 10.1053/j.gastro.2015.05.061. [DOI] [PubMed] [Google Scholar]
- 30.Fernandez-Cuesta L., Peifer M., Lu X., et al. Abstract 1531: crossentity mutation analysis of lung neuroendocrine tumors sheds light into their molecular origin and identifies new therapeutic targets. Cancer Research. 2014;74(19):p. 1531. doi: 10.1158/1538-7445.AM2014-1531. [DOI] [Google Scholar]
- 31.Derks J. Genetic subtypes of large cell neuroendocrine carcinoma (LCNEC) to predict response to chemotherapy. Journal of Clinical Oncology. 2017;35(Supplement 15):9061–9061. [Google Scholar]
- 32.George J., Lim J. S., Jang S. J., et al. Comprehensive genomic profiles of small cell lung cancer. Nature. 2015;524(7563):47–53. doi: 10.1038/nature14664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ball D. W. Achaete-scute homolog-1 and notch in lung neuroendocrine development and cancer. Cancer Letters. 2004;204(2):159–169. doi: 10.1016/S0304-3835(03)00452-X. [DOI] [PubMed] [Google Scholar]
- 34.The Cancer Genome Atlas Research Network. Comprehensive genomic characterization of squamous cell lung cancers. Nature. 2012;489(7417):519–525. doi: 10.1038/nature11404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sasaki H. Increased NRF2 gene (NFE2L2) copy number correlates with mutations in lung squamous cell carcinomas. Molecular Medicine Reports. 2012;6(2):391–394. doi: 10.3892/mmr.2012.921. [DOI] [PubMed] [Google Scholar]
- 36.Kim Y. R., Oh J. E., Kim M. S., et al. Oncogenic NRF2 mutations in squamous cell carcinomas of oesophagus and skin. The Journal of Pathology. 2010;220(4):446–451. doi: 10.1002/path.2653. [DOI] [PubMed] [Google Scholar]
- 37.Goldstein L. D., Lee J., Gnad F., et al. Recurrent loss of NFE2L2 exon 2 is a mechanism for Nrf2 pathway activation in human cancers. Cell Reports. 2016;16(10):2605–2617. doi: 10.1016/j.celrep.2016.08.010. [DOI] [PubMed] [Google Scholar]
- 38.Zhang D. D., Lo S. C., Sun Z., Habib G. M., Lieberman M. W., Hannink M. Ubiquitination of Keap1, a BTB-Kelch substrate adaptor protein for Cul3, targets Keap1 for degradation by a proteasome-independent pathway. The Journal of Biological Chemistry. 2005;280(34):30091–30099. doi: 10.1074/jbc.M501279200. [DOI] [PubMed] [Google Scholar]
- 39.Kovac M., Navas C., Horswell S., et al. Recurrent chromosomal gains and heterogeneous driver mutations characterise papillary renal cancer evolution. Nature Communications. 2015;6(1):p. 6336. doi: 10.1038/ncomms7336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ooi A., Wong J.-C., Petillo D., et al. An antioxidant response phenotype shared between hereditary and sporadic type 2 papillary renal cell carcinoma. Cancer Cell. 2011;20(4):511–523. doi: 10.1016/j.ccr.2011.08.024. [DOI] [PubMed] [Google Scholar]
- 41.Ooi A., Dykema K., Ansari A., et al. CUL3 and NRF2 mutations confer an NRF2 activation phenotype in a sporadic form of papillary renal cell carcinoma. Cancer Research. 2013;73(7):2044–2051. doi: 10.1158/0008-5472.CAN-12-3227. [DOI] [PubMed] [Google Scholar]
- 42.Menegon S., Columbano A., Giordano S. The dual roles of NRF2 in cancer. Trends in Molecular Medicine. 2016;22(7):578–593. doi: 10.1016/j.molmed.2016.05.002. [DOI] [PubMed] [Google Scholar]
- 43.Wang X. J., Hayes J. D., Wolf C. R. Generation of a stable antioxidant response element-driven reporter gene cell line and its use to show redox-dependent activation of nrf2 by cancer chemotherapeutic agents. Cancer Research. 2006;66(22):10983–10994. doi: 10.1158/0008-5472.CAN-06-2298. [DOI] [PubMed] [Google Scholar]
- 44.Yang H., Wang W., Zhang Y., et al. The role of NF-E2-related factor 2 in predicting chemoresistance and prognosis in advanced non-small-cell lung cancer. Clinical Lung Cancer. 2011;12(3):166–171. doi: 10.1016/j.cllc.2011.03.012. [DOI] [PubMed] [Google Scholar]
- 45.Cescon D. W., She D., Sakashita S., et al. NRF2 pathway activation and adjuvant chemotherapy benefit in lung squamous cell carcinoma. Clinical Cancer Research. 2015;21(11):2499–2505. doi: 10.1158/1078-0432.CCR-14-2206. [DOI] [PubMed] [Google Scholar]
- 46.Isohookana J., Haapasaari K. M., Soini Y., Karihtala P. Keap1 expression has independent prognostic value in pancreatic adenocarcinomas. Diagnostic Pathology. 2015;10(1):p. 28. doi: 10.1186/s13000-015-0258-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lister A., Nedjadi T., Kitteringham N. R., et al. Nrf2 is overexpressed in pancreatic cancer: implications for cell proliferation and therapy. Molecular Cancer. 2011;10(1):p. 37. doi: 10.1186/1476-4598-10-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kang K. A., Piao M. J., Kim K. C., et al. Epigenetic modification of Nrf2 in 5-fluorouracil-resistant colon cancer cells: involvement of TET-dependent DNA demethylation. Cell Death & Disease. 2014;5(4, article e1183) doi: 10.1038/cddis.2014.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kang K. A., Piao M. J., Ryu Y. S., et al. Interaction of DNA demethylase and histone methyltransferase upregulates Nrf2 in 5-fluorouracil-resistant colon cancer cells. Oncotarget. 2016;7(26):40594–40620. doi: 10.18632/oncotarget.9745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jeong Y., Hoang N. T., Lovejoy A., et al. Role of KEAP1/NRF2 and TP53 mutations in lung squamous cell carcinoma development and radiation resistance. Cancer Discovery. 2017;7(1):86–101. doi: 10.1158/2159-8290.CD-16-0127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang Q., Ma J., Lu Y., et al. CDK20 interacts with KEAP1 to activate NRF2 and promotes radiochemoresistance in lung cancer cells. Oncogene. 2014;36(37):5321–5330. doi: 10.1038/onc.2017.161. [DOI] [PubMed] [Google Scholar]
- 52.Denicola G. M., Karreth F. A., Humpton T. J., et al. Oncogene-induced Nrf2 transcription promotes ROS detoxification and tumorigenesis. Nature. 2011;475(7354):106–109. doi: 10.1038/nature10189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yamadori T., Ishii Y., Homma S., et al. Molecular mechanisms for the regulation of Nrf2-mediated cell proliferation in non-small-cell lung cancers. Oncogene. 2012;31(45):4768–4777. doi: 10.1038/onc.2011.628. [DOI] [PubMed] [Google Scholar]
- 54.Huang Y., Li W., Su Z.-Y., Kong A.-N. T. The complexity of the Nrf2 pathway: beyond the antioxidant response. The Journal of Nutritional Biochemistry. 2015;26(12):1401–1413. doi: 10.1016/j.jnutbio.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Krall E. B., Wang B., Munoz D. M., et al. KEAP1 loss modulates sensitivity to kinase targeted therapy in lung cancer. eLife. 2017;6, article e18970 doi: 10.7554/eLife.18970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hartikainen J. M., Tengström M., Winqvist R., et al. KEAP1 genetic polymorphisms associate with breast cancer risk and survival outcomes. Clinical Cancer Research. 2015;21(7):1591–1601. doi: 10.1158/1078-0432.CCR-14-1887. [DOI] [PubMed] [Google Scholar]
- 57.Muscarella L. A., Fazio V. M. Keap1/Nrf2 impairing revised: are we missing the single nucleotide polymorphisms? Journal of Thoracic Disease. 2016;8(12):E1752–E1754. doi: 10.21037/jtd.2016.12.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nicoloso M. S., Sun H., Spizzo R., et al. Single-nucleotide polymorphisms inside microRNA target sites influence tumor susceptibility. Cancer Research. 2010;70(7):2789–2798. doi: 10.1158/0008-5472.CAN-09-3541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhao N., Han J. G., Shyu C. R., Korkin D. Determining effects of non-synonymous SNPs on protein-protein interactions using supervised and semi-supervised learning. PLoS Computational Biology. 2014;10(5, article e1003592) doi: 10.1371/journal.pcbi.1003592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Eades G., Yang M., Yao Y., Zhang Y., Zhou Q. miR-200a regulates Nrf2 activation by targeting Keap1 mRNA in breast cancer cells. The Journal of Biological Chemistry. 2011;286(47):40725–40733. doi: 10.1074/jbc.M111.275495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Copple I. M. The Keap1-Nrf2 cell defense pathway – a promising therapeutic target? Advances in Pharmacology. 2016;63:43–79. doi: 10.1016/B978-0-12-398339-8.00002-1. [DOI] [PubMed] [Google Scholar]
- 62.Wang R., An J., Ji F., Jiao H., Sun H., Zhou D. Hypermethylation of the Keap1 gene in human lung cancer cell lines and lung cancer tissues. Biochemical and Biophysical Research Communications. 2008;373(1):151–154. doi: 10.1016/j.bbrc.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 63.Zhang P., Singh A., Yegnasubramanian S., et al. Loss of Kelch-like ECH-associated protein 1 function in prostate cancer cells causes chemoresistance and radioresistance and promotes tumor growth. Molecular Cancer Therapeutics. 2010;9(2):336–346. doi: 10.1158/1535-7163.MCT-09-0589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Khor T. O., Fuentes F., Shu L., et al. Epigenetic DNA methylation of antioxidative stress regulator NRF2 in human prostate cancer. Cancer Prevention Research. 2014;7(12):1186–1197. doi: 10.1158/1940-6207.CAPR-14-0127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Muscarella L. A., Barbano R., D’Angelo V., et al. Regulation of KEAP1 expression by promoter methylation in malignant gliomas and association with patient’s outcome. Epigenetics. 2011;6(3):317–325. doi: 10.4161/epi.6.3.14408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Muscarella L. A., Parrella P., D’Alessandro V., et al. Frequent epigenetics inactivation of KEAP1 gene in non-small cell lung cancer. Epigenetics. 2011;6(6):710–719. doi: 10.4161/epi.6.6.15773. [DOI] [PubMed] [Google Scholar]
- 67.Barbano R., Muscarella L. A., Pasculli B., et al. Aberrant Keap1 methylation in breast cancer and association with clinicopathological features. Epigenetics. 2013;8(1):105–112. doi: 10.4161/epi.23319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fabrizio F. P., Costantini M., Copetti M., et al. Keap1/Nrf2 pathway in kidney cancer: frequent methylation of KEAP1 gene promoter in clear renal cell carcinoma. Oncotarget. 2017;8(7):11187–11198. doi: 10.18632/oncotarget.14492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Liu X., Sun C., Liu B., et al. Genistein mediates the selective radiosensitizing effect in NSCLC A549 cells via inhibiting methylation of the keap1 gene promoter region. Oncotarget. 2016;7(19):27267–27279. doi: 10.18632/oncotarget.8403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hanada N., Takahata T., Zhou Q., et al. Methylation of the KEAP1 gene promoter region in human colorectal cancer. BMC Cancer. 2012;12(1):p. 66. doi: 10.1186/1471-2407-12-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jazirehi A. R., Wenn P. B., Arle D. Is there a decrease in Keap1 RNA expression in colorectal cancer cells, and is this decrease in expression due to hypermethylation? Epigenomics. 2012;4(3):253–254. [PubMed] [Google Scholar]
- 72.Abu-Alainin W., Gana T., Liloglou T., et al. UHRF1 regulation of the Keap1-Nrf2 pathway in pancreatic cancer contributes to oncogenesis. The Journal of Pathology. 2016;238(3):423–433. doi: 10.1002/path.4665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Li Z., Xu L., Tang N., et al. The polycomb group protein EZH2 inhibits lung cancer cell growth by repressing the transcription factor Nrf2. FEBS Letters. 2014;588(17):3000–3007. doi: 10.1016/j.febslet.2014.05.057. [DOI] [PubMed] [Google Scholar]
- 74.Berindan-Neagoe I., Monroig Pdel C., Pasculli B., Calin G. A. MicroRNAome genome: a treasure for cancer diagnosis and therapy. CA: A Cancer Journal for Clinicians. 2014;64(5):311–336. doi: 10.3322/caac.21244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ayers D., Baron B., Hunter T. miRNA influences in NRF2 pathway interactions within cancer models. Journal of Nucleic Acids. 2015;2015:6. doi: 10.1155/2015/143636.143636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Papp D., Lenti K., Módos D., et al. The NRF2-related interactome and regulome contain multifunctional proteins and fine-tuned autoregulatory loops. FEBS Letters. 2012;586(13):1795–1802. doi: 10.1016/j.febslet.2012.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yang M., Yao Y., Eades G., Zhang Y., Zhou Q. MiR-28 regulates Nrf2 expression through a Keap1-independent mechanism. Breast Cancer Research and Treatment. 2011;129(3):983–991. doi: 10.1007/s10549-011-1604-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chen C., Jiang X., Gu S., Zhang Z. MicroRNA-155 regulates arsenite-induced malignant transformation by targeting Nrf2-mediated oxidative damage in human bronchial epithelial cells. Toxicology Letters. 2017;278:38–47. doi: 10.1016/j.toxlet.2017.07.215. [DOI] [PubMed] [Google Scholar]
- 79.Pottier N., Maurin T., Chevalier B., et al. Identification of keratinocyte growth factor as a target of microRNA-155 in lung fibroblasts: implication in epithelial-mesenchymal interactions. PLoS One. 2009;4(8, article e6718) doi: 10.1371/journal.pone.0006718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Duru N., Gernapudi R., Zhang Y., et al. NRF2/miR-140 signaling confers radioprotection to human lung fibroblasts. Cancer Letters. 2015;369(1):184–191. doi: 10.1016/j.canlet.2015.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Duru N., Zhang Y., Gernapudi R., et al. Loss of miR-140 is a key risk factor for radiation-induced lung fibrosis through reprogramming fibroblasts and macrophages. Scientific Reports. 2017;6(1, article 39572) doi: 10.1038/srep39572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhou C., Zhao L., Zheng J., et al. MicroRNA-144 modulates oxidative stress tolerance in SH-SY5Y cells by regulating nuclear factor erythroid 2-related factor 2-glutathione axis. Neuroscience Letters. 2016;655:21–27. doi: 10.1016/j.neulet.2017.06.045. [DOI] [PubMed] [Google Scholar]
- 83.Sun X., Liu D., Xue Y., Hu X. Enforced miR-144-3p expression as a non-invasive biomarker for the acute myeloid leukemia patients mainly by targeting NRF2. Clinical Laboratory. 2017;63(4):679–687. doi: 10.7754/Clin.Lab.2016.161116. [DOI] [PubMed] [Google Scholar]
- 84.Zhou S., Ye W., Zhang Y., et al. miR-144 reverses chemoresistance of hepatocellular carcinoma cell lines by targeting Nrf2-dependent antioxidant pathway. American Journal of Translational Research. 2010;8(7):2992–3002. [PMC free article] [PubMed] [Google Scholar]
- 85.Singh B., Ronghe A. M., Chatterjee A., Bhat N. K., Bhat H. K. MicroRNA-93 regulates NRF2 expression and is associated with breast carcinogenesis. Carcinogenesis. 2013;34(5):1165–1172. doi: 10.1093/carcin/bgt026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Narasimhan M., Patel D., Vedpathak D., Rathinam M., Henderson G., Mahimainathan L. Identification of novel microRNAs in post-transcriptional control of Nrf2 expression and redox homeostasis in neuronal, SH-SY5Y cells. PLoS One. 2012;7(12, article e51111) doi: 10.1371/journal.pone.0051111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wang B., Teng Y., Liu Q. MicroRNA-153 regulates NRF2 expression and is associated with breast carcinogenesis. Clinical Laboratory. 2016;62(1-2):39–47. doi: 10.7754/clin.lab.2015.150518. [DOI] [PubMed] [Google Scholar]
- 88.Jing Y., Xu B. Decreased expression of miR-153-3p in oral squamous cell carcinoma contributes to cell migration and invasion. International Journal of Clinical and Experimental Pathology. 2017;10(5):6117–6129. [Google Scholar]
- 89.Shi L., Chen Z. G., Wu L. L., et al. miR-340 reverses cisplatin resistance of hepatocellular carcinoma cell lines by targeting Nrf2-dependent antioxidant pathway. Asian Pacific Journal of Cancer Prevention. 2014;15(23):10439–10444. doi: 10.7314/apjcp.2014.15.23.10439. [DOI] [PubMed] [Google Scholar]
- 90.Qaisiya M., Coda Zabetta C. D., Bellarosa C., Tiribelli C. Bilirubin mediated oxidative stress involves antioxidant response activation via Nrf2 pathway. Cellular Signalling. 2014;26(3):512–520. doi: 10.1016/j.cellsig.2013.11.029. [DOI] [PubMed] [Google Scholar]
- 91.Yamamoto S., Inoue J., Kawano T., Kozaki K., Omura K., Inazawa J. The impact of miRNA-based molecular diagnostics and treatment of NRF2-stabilized tumors. Molecular Cancer Research. 2014;12(1):58–68. doi: 10.1158/1541-7786.MCR-13-0246-T. [DOI] [PubMed] [Google Scholar]
- 92.Van Jaarsveld M. T. M., Helleman J., Boersma A. W. M., et al. miR-141 regulates KEAP1 and modulates cisplatin sensitivity in ovarian cancer cells. Oncogene. 2013;32(36):4284–4293. doi: 10.1038/onc.2012.433. [DOI] [PubMed] [Google Scholar]
- 93.Shi L., Wu L., Chen Z., et al. MiR-141 activates Nrf2-dependent antioxidant pathway via down-regulating the expression of Keap1 conferring the resistance of hepatocellular carcinoma cells to 5-fluorouracil. Cellular Physiology and Biochemistry. 2015;35(6):2333–2348. doi: 10.1159/000374036. [DOI] [PubMed] [Google Scholar]
- 94.Eades G., Yao Y., Yang M., Zhang Y., Chumsri S., Zhou Q. miR-200a regulates SIRT1 expression and epithelial to mesenchymal transition (EMT)-like transformation in mammary epithelial cells. The Journal of Biological Chemistry. 2011;286(29):25992–26002. doi: 10.1074/jbc.M111.229401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Liu M., Hu C., Xu Q., et al. Methylseleninic acid activates Keap1/Nrf2 pathway via up-regulating miR-200a in human oesophageal squamous cell carcinoma cells. Bioscience Reports. 2015;35(5, article e00256) doi: 10.1042/BSR20150092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kabaria S., Choi D. C., Chaudhuri A. D., Jain M. R., Li H., Junn E. MicroRNA-7 activates Nrf2 pathway by targeting Keap1 expression. Free Radical Biology & Medicine. 2015;89:548–556. doi: 10.1016/j.freeradbiomed.2015.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hou W., Tian Q., Zheng J., Bonkovsky H. L. MicroRNA-196 represses Bach1 protein and hepatitis C virus gene expression in human hepatoma cells expressing hepatitis C viral proteins. Hepatology. 2010;51(5):1494–1504. doi: 10.1002/hep.23401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Akdemir B., Nakajima Y., Inazawa J., Inoue J. miR-432 induces NRF2 stabilization by directly targeting KEAP1. Molecular Cancer Research. 2017;15(11):1570–1578. doi: 10.1158/1541-7786.MCR-17-0232. [DOI] [PubMed] [Google Scholar]
- 99.Tokumaru S., Suzuki M., Yamada H., Nagino M., Takahashi T. let-7 regulates Dicer expression and constitutes a negative feedback loop. Carcinogenesis. 2008;29(11):2073–2077. doi: 10.1093/carcin/bgn187. [DOI] [PubMed] [Google Scholar]
- 100.Johnson C. D., Esquela-Kerscher A., Stefani G., et al. The let-7 microRNA represses cell proliferation pathways in human cells. Cancer Research. 2007;67(16):7713–7722. doi: 10.1158/0008-5472.CAN-07-1083. [DOI] [PubMed] [Google Scholar]
- 101.Johnson S. M., Grosshans H., Shingara J., et al. RAS is regulated by the let-7 microRNA family. Cell. 2005;120(5):635–647. doi: 10.1016/j.cell.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 102.Reichard J. F., Motz G. T., Puga A. Heme oxygenase-1 induction by NRF2 requires inactivation of the transcriptional repressor BACH1. Nucleic Acids Research. 2007;35(21):7074–7086. doi: 10.1093/nar/gkm638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Li S., Chen T., Zhong Z., Wang Y., Li Y., Zhao X. microRNA-155 silencing inhibits proliferation and migration and induces apoptosis by upregulating BACH1 in renal cancer cells. Molecular Medicine Reports. 2012;5(4):949–954. doi: 10.3892/mmr.2012.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hou W., Tian Q., Steuerwald N. M., Schrum L. W., Bonkovsky H. L. The let-7 microRNA enhances heme oxygenase-1 by suppressing Bach1 and attenuates oxidant injury in human hepatocytes. Biochimica et Biophysica Acta (BBA) - Gene Regulatory Mechanisms. 2012;1819(11-12):1113–1122. doi: 10.1016/j.bbagrm.2012.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sati S., Ghosh S., Jain V., Scaria V., Sengupta S. Genome-wide analysis reveals distinct patterns of epigenetic features in long non-coding RNA loci. Nucleic Acids Research. 2012;40(20):10018–10031. doi: 10.1093/nar/gks776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Moran V. A., Perera R. J., Khalil A. M. Emerging functional and mechanistic paradigms of mammalian long non-coding RNAs. Nucleic Acids Research. 2012;40(14):6391–6400. doi: 10.1093/nar/gks296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.White N. M., Cabanski C. R., Silva-Fisher J. M., Dang H. X., Govindan R., Maher C. A. Transcriptome sequencing reveals altered long intergenic non-coding RNAs in lung cancer. Genome Biology. 2014;15(8):p. 429. doi: 10.1186/s13059-014-0429-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Thai P., Statt S., Chen C. H., Liang E., Campbell C., Wu R. Characterization of a novel long noncoding RNA, SCAL1, induced by cigarette smoke and elevated in lung cancer cell lines. American Journal of Respiratory Cell and Molecular Biology. 2013;49(2):204–211. doi: 10.1165/rcmb.2013-0159RC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Zhang Y., Xia J., Li Q., et al. NRF2/long noncoding RNA ROR signaling regulates mammary stem cell expansion and protects against estrogen genotoxicity. The Journal of Biological Chemistry. 2014;289(45):31310–31318. doi: 10.1074/jbc.M114.604868. [DOI] [PMC free article] [PubMed] [Google Scholar]