Abstract
Background:
Pneumoperitoneum and altered positioning 1in laparoscopic cholecystectomy predispose to alterations in cardiorespiratory physiology. We compared the effects of volume controlled, pressure controlled, and the newly introduced pressure controlled-volume guaranteed ventilation (PCV-VG) modes of ventilation on respiratory mechanics and oxygenation during laparoscopic cholecystectomy.
Materials and Methods:
Seventy-five physical status American Society of Anesthesiologists Classes I and II patients with normal lungs undergoing laparoscopic cholecystectomy were randomly allocated to receive volume controlled ventilation (VCV), pressure-controlled ventilation (PCV), or PCV-VG modes of ventilation during general anesthesia. In all modes of ventilation, the tidal volume was set at 8 mL/kg, and respiratory rate was set at 12 breaths/min with inspired oxygen of 0.4. After pneumoperitoneum, respiratory rate was adjusted to maintain an end-tidal carbon dioxide between 32 and 37 mm Hg. The peak airway pressures, compliance, the mean airway pressures, oxygen saturation, end tidal carbon dioxide and hemodynamics were recorded at the time of intubation (T1), 15 min after pneumoperitoneum (T2) and after desufflation (T3) and were compared. Arterial oxygen tension, arterial carbon dioxide tension at T2 and T3 were compared.
Results:
PCV-VG and PCV mode resulted in lower peak airway pressures than VCV (23.04 ± 3.43, 24.52 ± 2.79, and 27.24 ± 2.37 cm of water, respectively, P = 0.001). Compliance was better preserved in the pressure mediated modes than VCV (fall from baseline was 42%, 29%, and 30% in VCV, PCV, and PCV-VG). The arterial to end-tidal carbon dioxide gradient was lower in PCV-VG and PCV compared to VCV. No difference in oxygenation and hemodynamics were observed.
Conclusion:
PCV and PCV-VG modes are superior to VCV mode in providing adequate oxygenation at lower peak inspiratory pressures.
Keywords: Airway resistance, barotrauma, compliance, ventilator-induced lung injury, volutrauma
INTRODUCTION
Cholecystectomy is most commonly performed laparoscopically as it reduces the risk of postoperative pulmonary complications six-fold compared to open surgery.[1] However, the technique of laparoscopy involves significant cardiorespiratory adverse effects that should be balanced by safe anesthetic and ventilator management to profit the benefits without concerns of safety.[2] The effects are due to the creation of pneumoperitoneum and position changes incorporated to facilitate surgical access. The increase in intraabdominal pressure causes a cephalad shift of the diaphragm leading to decrease in lung compliance by 25%–40%[3] and a more marked increase in the airway pressure.[4] The head up position given during cholecystectomy causes a decrease in the airway pressure and increase in the thoracic compliance. However, it is minimal compared to the changes occurring due to the pneumoperitoneum. Although hypoxemia is rare,[5] there occur significant changes in airway pressures and compliance. The developments in our understanding of pressure-volume curves and recent demonstration of sheer stress injury following increased airway pressure have changed the whole concept of safe range of pressure and volume changes during laparoscopy, especially in the presence of underlying lung disease. Safer ventilation strategies such as use of lung protective modes, application of positive end-expiratory pressure, and recruitment methods are being studied and incorporated to mitigate laparoscopy-induced changes.[6]
Volume-controlled ventilation (VCV) mode is the most commonly used conventional mode in anesthesia. VCV follows a constant flow pattern to deliver a preset tidal volume in the preset inspiratory time, thus ensuring constant minute ventilation. This flow pattern generates high inspiratory pressure that can lead to shear stress injury, barotrauma and volutrauma to the alveoli[7] leading to micro atelectasis and inflammatory mediator release characteristic of ventilator-associated lung injury.
Pressure-controlled ventilation (PCV) mode came as an alternative mode in laparoscopic surgeries. PCV delivers tidal volume at a preset pressure and inspiratory time. The flow, unlike VCV, is decelerating. This flow pattern has a high initial rise followed by a decrease and helps to attain the tidal volume at lower peak inspiratory pressures, and oxygenation is also better due to the initial high flow rates. However, with changing lung compliance, the tidal volume delivered varies, and there is always a risk of hypoventilation or hyperventilation.
Pressure-controlled volume guaranteed ventilation (PCV-VG) mode is a new mode introduced recently in anesthesia workstations. PCV-VG features a user select tidal volume target that is autoregulated and pressure controlled.[8] The ventilator calculates the compliance of the lung and establishes the lowest possible pressure to deliver the target tidal volume. It has the characteristic decelerating flow pattern, thus incorporating the benefits of both VCV and PCV.[9]
Recently, few studies comparing the efficacy of PCV-VG over other modes on selected surgical cohorts have been published with varying results.
We hypothesize that the airway pressures are lesser with the PCV-VG mode compared to the conventional modes and the gas exchange, oxygenation, and lung compliance are also better in the PCV-VG mode of ventilation.
Aims and objectives
The aim of this study is to compare the effect of the three modes of ventilation on respiratory mechanics (airway pressure, gas exchange, and dynamic compliance) during laparoscopic cholecystectomy.
MATERIALS AND METHODS
The study was taken up after obtaining approval from the the Institutional Ethics Committee. (St Johns National Academy of Health Sciences, Institutional Ethics Committee, Study No-IEC Study Ref No 130/2015, Date of Approval-30/04/2015). All patients were informed, and a written consent for participation was obtained. The study was done over a period of 10 months.
All patients aged between 18 and 60 years belonging to physical status American Society of Anesthesiologists (ASA) Classes I and II undergoing laparoscopic cholecystectomy were included in this study. Patients with preexisting lung diseases, respiratory infections in the past 3 weeks, having a body mass index >25 and patients belonging to physical status ASA Classes III and IV were excluded from the study. In addition, patients in whom ventilator settings could not be stabilized within 30 min of pneumoperitoneum in the allocated modes and in whom surgery was converted to open procedure were excluded from the study.
Patients were randomly allocated to receive volume controlled, pressure controlled, or pressure controlled-volume guaranteed modes of ventilation. The randomization was done after patients consented for the study. Randomization was done by computer-generated numbering system. A standard general anesthesia technique was followed in all cases. Standard monitors included noninvasive blood pressure monitor, pulse oximeter, electrocardiogram, and capnogram. Anesthesia was induced with 2 mg/kg of propofol, 2 μg/kg of fentanyl, and 1 mg of midazolam intravenous. Endotracheal intubation was facilitated using 0.5 mg/kg of atracurium. Anesthesia was maintained with isoflurane, air oxygen mixture, and atracurium top-ups of 0.1 mg/kg. Muscle relaxation was maintained at <2 twitches in train of four (TOF) sequence using a TOF watch. At the end of the procedure, the neuromuscular block was reversed with Neostigmine 2.5 mg and glycopyrrolate 0.5 mg intravenous. The trachea was extubated when patient was fully awake with TOF ratio >0.9.
Ventilation was carried out using Datex Ohmeda Aisys CS2 workstation. In all three modes, patients were ventilated with a tidal volume of 8 mL/kg body weight, respiratory rate of 12 breaths/min, inspiratory to expiratory ratio of 0.5, inspired oxygen concentration of 0.4, and positive end-expiratory pressure of 5 cm of water. During insufflation of THE abdomen, the intra-abdominal pressure was maintained between 15 and 17 mmHg in all patients. After creating pneumoperitoneum, the respiratory rate was adjusted to achieve an end-tidal carbon dioxide (ETCO2) between 33 and 37 mm of Hg. Figure 1 shows the protocol followed to achieve the set ventilatory goals.
Figure 1.
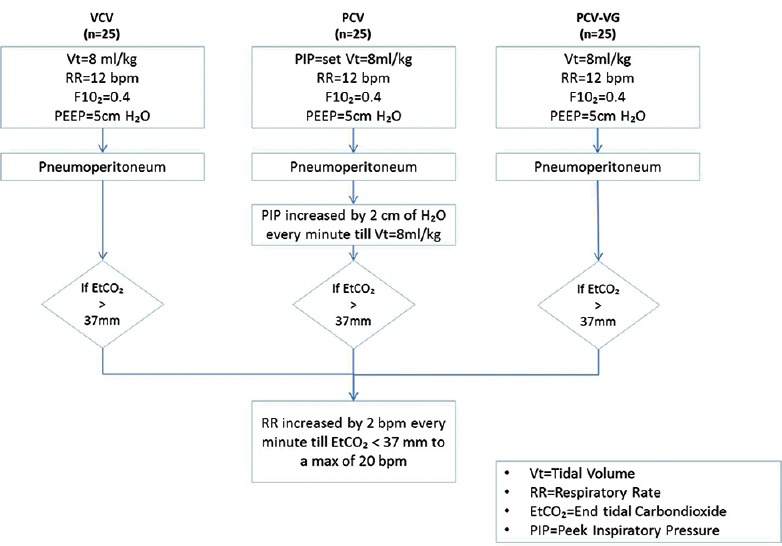
Flow chart-ventilatory settings
Measurements
Tidal volume, respiratory rate, peak and mean airway pressures (Pmean), dynamic compliance, oxygen saturation, end-tidal and arterial carbon dioxide levels, mean arterial pressures, and heart rate were recorded at the time of intubation (T1), 15 min after pneumoperitoneum (T2) and after desufflation (T3) and were compared between the three modes. Arterial oxygen tension (PaO2), arterial carbon dioxide tension (PaCO2) at T2 and T3 were measured and compared between the three modes.
Statistical methods
Sample size
A pilot study on nine patients was done. A difference in peak airway pressures (Ppeaks) of 5 cm H2O was observed. Considering an alpha error of 5% and beta error of 85%, the calculated sample size was 75 (n = 25 in each group). Descriptive and inferential statistical analysis has been carried out in the present study.
Results on continuous measurements are presented on mean ± standard deviation (minimum–maximum), and results on categorical measurements are presented in number (%). The significance is assessed at 5% level of significance. All the variables were tested for normality by Sapiro–Wilks test and proved to follow the normality (P > 0.05). Homoscedasticity was tested all the study variables using Levens test and proved to accept the homogeneity of variance (P > 0.05).
The Statistical software, namely, The Statistical softwares SAS9.2 (SAS Inc.NC, USA), SPSS.15 (IBM SPSS Statistics, Somers NY, USA)were used for analysis of data. Analysis of variance has been used to find the significance of study parameters between three or more groups of patients, post hoc Tukey (two-tailed, independent) has been used to find the significance of study parameters on continuous scale between two groups (Intergroup analysis) on metric parameters. Chi-square/Fisher's exact test has been used to find the significance of study parameters on categorical scale between two or more groups.
RESULTS
Seventy-five patients were enrolled in the study. Each group had 25 patients each. None of the patients had any ventilation-related issues intraoperatively to be excluded from the study.
The mean age, weight, and sex distribution of the patients were similar in all three groups. The mean duration of surgery was also similar in all the three groups studied [Table 1].
Table 1.
Demographic characteristics
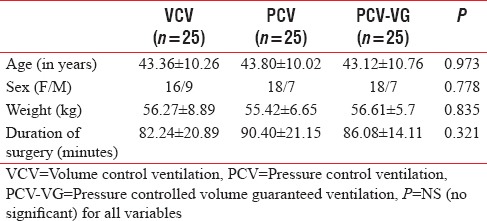
There were no significant differences in the hemodynamic parameters (Heart rate and blood pressure) between the three groups at all periods of the study [Table 1].
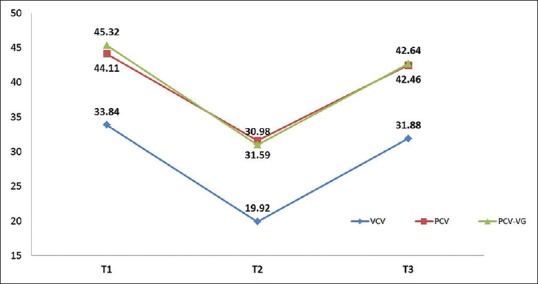
Among the respiratory parameters, tidal volume and respiratory rates were also comparable between the three groups before and after the creation of pneumoperitoneum [Table 2]. Despite similar values of Pmean, Ppeak was significantly high in VCV group at T1, T2, and T3 as compared to PCV-VG and PCV groups as depicted in Figure 2.
Table 2.
Respiratory and hemodynamic parameters by mode of ventilation
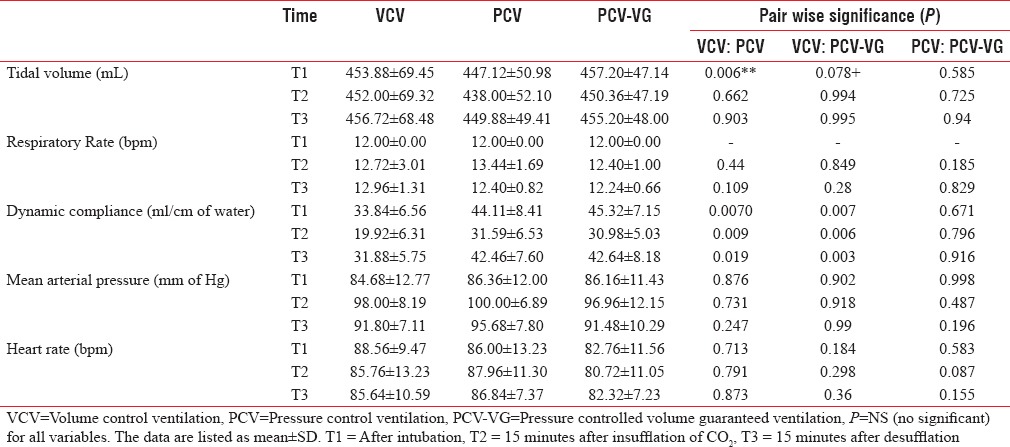
Figure 2.
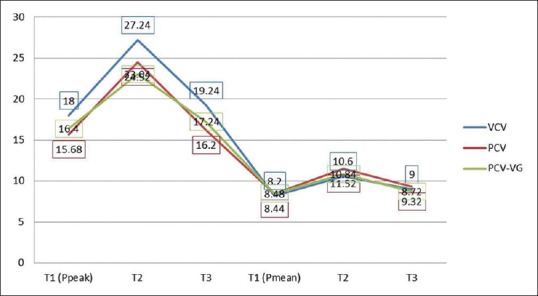
Peak and mean pressures by modes of ventilation. VCV=Volume control ventilation, PCV=Pressure control ventilation, PCV-VG=Pressure-Controlled volume guaranteed ventilation. The data are listed as mean ± standard deviation. T1-After Intubation, T2-15 Min after insufflation of Co2, T3-15 min after desufflation
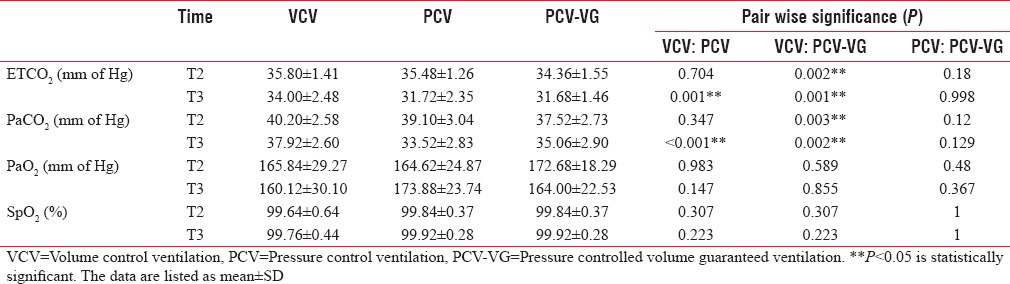
The dynamic compliance which is inversely related to the peak pressures was better preserved in the PCV and PCV-VG modes than VCV.
After the creation of pneumoperitoneum, the dynamic compliance decreased in all the groups [Figure 3]. However, the fall from baseline was lesser in the pressure-mediated modes (42% fall in VCV group compared to 29 and 30% in PCV and PCV-VG, respectively).
Figure 3.
Dynamic compliance in different modes of ventilation. VCV=Volume control ventilation, PCV=Pressure control ventilation, PCV-VG=Pressure-controlled volume guaranteed ventilation. The data are listed as mean ± standard deviation. T1-after intubation, T2-15 min after insufflation of CO2, T3-15 min after desufflation
The arterial blood gas analysis showed that the arterial oxygen levels after pneumoperitoneum and after desufflation in all three modes of ventilation were comparable [Table 3].
Table 3.
Ventilation and Oxygenation parameters by mode of ventilation
The arterial to end-tidal carbon dioxide gradient which represents the amount of dead space ventilation was lower in PCV and PCV-VG compared to VCV mode after pneumoperitoneum (T2) and desufflation (T3). The P = 0.02 between VCV and PCV-VG at T2 and 0.001 between VCV and PCV and 0.001 between VCV and PCV-VG at T3. The gradient was comparable with no significant statistical difference between the pressure-mediated modes. Although the difference in ETCO2 and PaCO2 between PCV and PCV-VG modes was not statistically significant, the values were lower in PCV-VG group [Figure 4].
Figure 4.
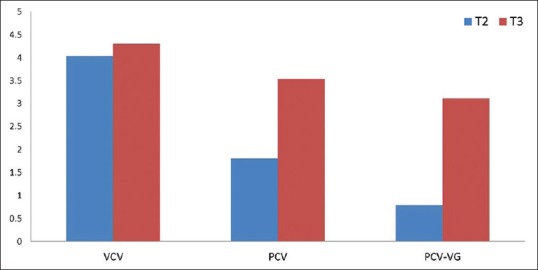
Arterial carbon dioxide tension-end tidal carbon dioxide gradient by modes of ventilation. VCV=Volume control ventilation, PCV=Pressure control ventilation, PCV-VG=Pressure-controlled volume guaranteed ventilation. The data are listed as mean. T2-15 min after insufflation of CO2, T3-15 min after desufflation
DISCUSSION
Under anesthesia, delivery of mechanical ventilation should result in adequate gas exchange with minimum lung injury and lowest possible degree of hemodynamic impairment. This study comparing VCV, PCV, PCV-VG modes of ventilation using a set algorithm has shown a difference in the airway pressures in favor of PCV-VG and PCV modes as per our hypothesis. However, the oxygenation has remained similar in all modes.
The principle observation in our study was that the Ppeak was significantly lower in the pressure-mediated modes (PCV and PCV-VG) compared to the volume-controlled mode at all periods of study. No significant difference was observed in the peak pressures between PCV and the PCV-VG mode.
The inflating pressures during mechanical ventilation are of great clinical significance as high pressures predispose to the development of barotrauma.
Barotrauma is a condition wherein high inflating pressures predispose the alveoli to rupture causing extra-alveolar air seepage and pulmonary interstitial emphysema.[10] This results in pneumothorax, pneumomediastinum, and cardiorespiratory failure. Eisner et al.[11] have found that high Ppeaks is the major risk factor for early barotrauma in patients with lung injury.
The airway pressures in our study were within the normal range in all three modes. Although a plateau pressure of <30 cm of water is considered acceptable, so far no safe pressure limits have been proposed. Hence, lower pressures with the pressure-mediated modes imply better lung protection offering more advantage in patients with lower lung compliances.
The inspiratory flow pattern in the PCV and PCV-VG modes is decelerating type with a high initial flow rate as against a constant flow pattern in the volume-controlled mode. The high initial flow rate inflates the compliant alveoli and during the decelerating phase of flow, the noncompliant alveoli with higher time constants are ventilated without over inflation of the other units thus delivering the same tidal volume at a lower airway pressure.
Our study was conducted on patients with no underlying lung pathology. We postulated that the effects of the different modes on the laparoscopic physiology are better appreciated in healthy patients. The complex alveolar pathology in restrictive and obstructive lung diseases and its interaction with the laparoscopy-induced changes are absent in our patients, and hence, the direct effects of the modes are better appreciated.
Similar studies comparing the three modes of ventilation among various surgical cohorts showed varying results. Leopoldo et al.[12] in their study randomized 41 patients undergoing laparoscopic cholecystectomy to receive VCV, PCV, and PCV-VG modes of ventilation (n = 13) and found no difference in the peak pressure generated in the three modes.
However, in a study by Dion et al.,[13] 20 obese patients undergoing laparoscopic sleeve gastrectomy received VCV, PCV, and PCV-VG modes in a random sequence and the authors found the peak pressures were significantly lower in the pressure modes (PCV and PCV-VG) compared to the volume controlled mode similar to our observations.
Boules and Ghobrial[14] and Song et al.[15] studied the effects of PCV-VG and VCV on various parameters, including respiratory mechanics and hemodynamics during one-lung ventilation (OLV). Results were similar to our study showing that Ppeak was significantly lower in PCV-VG compared to VCV in all stages of the study (P < 0.050). In addition, the Pmean showed lower values in the PCV-VG group. They indicated that PCV-VG provided lower airway pressures compared to VCV.
Cadi et al.[16] randomly allocated 36 patients to receive PCV or VCV modes of ventilation in patients undergoing bariatric surgery and found that the peak pressures were lower in PCV group. No significant change in mean pressures was noted.
A review by Aldenkortt et al.[17] assessed 13 studies comparing PCV and VCV modes that included 500 obese patients. They concluded that there was no significant difference in airway pressures between the two groups.
The Pmeans which reflect the alveolar pressure were comparable in the three modes of ventilation in all times of the study. Our results were consistent with the findings of other similar studies.[12,13,15,16,17] Our patient cohort being healthy with no underlying diseases, the alveolar pressures remained unaffected.
Dynamic compliance of the lung is inversely related to the Ppeaks. An increase in Ppeak after pneumoperitoneunl results in fall in the lung compliance. In our study also, the compliance decreased on the creation of pneumoperitoneum in all the three modes of ventilation. In fact, the compliance measured at all time periods (T1, T2, and T3) was better in PCV and PCV-VG modes than VCV mode. In addition, the percentage fall in compliance after creation of pneumoperitoneum was lesser in their pressure-mediated modes (29% and 30% in PCV and PCV-VG vs. 42% in VCV mode). It has been demonstrated that the dynamic compliance falls by 25%–40% after pneumoperitoneum. A 42% decrease in VCV mode has significant effects in the development of pulmonary complications, especially in patients with preexisting diseases.
Oxygenation was well maintained in all the three groups of patients throughout the surgery. The PaO2 and SpO2 were comparable between the three groups. Oxygenation depends on the FiO2, alveolar ventilation, and intrapulmonary shunts. The inspired oxygen concentration in our study was constant, and alveolar ventilation was uncompromised (mean pressures were normal). We inferred that the ventilation-perfusion mismatch which is expected to be higher with anesthesia, and pneumoperitoneum has not been significant in our patients to impair oxygenation. Our finding has been consistent with many studies conducted on ventilation-perfusion changes during laparoscopy. Strang et al.[18] studied the ventilation and perfusion distribution in pigs following pneumoperitoneum and inferred that perfusion was also redistributed from the atelectatic area to the compliant units, and there was better V/Q match. This was attributed to effective hypoxic vasoconstriction secondary to pneumoperitoneum.
Andersson et al.[19] conducted a similar study on V/Q distribution using MIGET scan in humans and showed similar finding explaining why oxygenation is by and large well preserved in healthy adults. However, Cadi et al.[16] and Gupta et al.[20] in their studies found that oxygenation was better maintained in the PCV than VCV in obese patient undergoing bariatric surgeries. Boules et al.[14] in their study comparing PCV-VG with conventional modes for OLV found better oxygenation in the PCV-VG mode. The difference in their results and ours could be attributed to the difference in the patient profiles in both the studies.
The next significant observation in our study was that the ETCO2 and PaCO2 were significantly lower in PCV and PCV-VG group during the period of pneumoperitoneum and after desufflation. In healthy patients, the ETCO2 reflects truly the arterial levels. The arterial to end-tidal gradient is usually 2–5 mm of mercury. In our study, the gradient was well within the normal range at all periods of study. However, it was significantly lower in the PCV-VG group compared to VCV during the period of pneumoperitoneum (3.12 ± 1.64 mm Hg vs. 4.3 ± 2.3 mm Hg) and after desufflation (1.8 ± 1.2 vs. 4.04 ± 2.02 mm Hg). This implies a significant reduction in the alveolar dead space thereby improving gas exchange and preventing respiratory acidosis. It becomes clinically advantageous in obese patients and patients subjected to pneumoperitoneum for a longer duration.
What is new in the study is that though the advantages of PCV over VCV in maintaining lung dynamics has been proved beyond ambiguity, this mode is still not popular in the anesthesia settings due to the inconsistency in the tidal volume delivered in a setting of changing compliance as in laparoscopy. The newer PCV-VG mode which beholds the advantage of delivering a consistent tidal volume in a decelerating flow pattern can be used as a standard ventilatory mode of choice in surgeries involving changes in respiratory dynamics.
The limitations of our study are that the results are from a single-hospital study and are done on patients subjected to one particular type of surgery. More complex surgical manipulations as in robotic surgeries may potentially alter the results of the study. In addition, our study being conducted in patients with normal lungs and studies on patients with underlying lung diseases subjected to such surgeries may also differ from our study results.
CONCLUSION
It can be stated that in patients undergoing laparoscopic cholecystectomy the pressure-controlled modes PCV and PCV-VG deliver the targeted tidal volume at significantly lower airway pressures compared to VCV. In addition, the PaCO2 and ETCO2 gradient were better with PCV and PCV-VG. No differences in oxygenation and hemodynamics were noted between the modes of ventilation. Despite no difference between PCV and PCV-VG modes, the PCV-VG mode is more users-friendly and requires fewer adjustments than PCV with variations in compliance and resistance intraoperatively. However, further studies are required to support our results.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Approval for this study was granted by the Institutional Ethics Committee. For this, a formal written informed consent was taken from all the participants.
REFERENCES
- 1.Cunningham AJ, Brull SJ. Laparoscopic cholecystectomy: Anesthetic implications. Anesth Analg. 1993;76:1120–33. doi: 10.1213/00000539-199305000-00035. [DOI] [PubMed] [Google Scholar]
- 2.Holohan TV. Laparoscopic cholecystectomy. Lancet. 1991;338:801–3. doi: 10.1016/0140-6736(91)90678-i. [DOI] [PubMed] [Google Scholar]
- 3.Gutt CN, Oniu T, Mehrabi A, Schemmer P, Kashfi A, Kraus T, et al. Circulatory and respiratory complications of carbon dioxide insufflation. Dig Surg. 2004;21:95–105. doi: 10.1159/000077038. [DOI] [PubMed] [Google Scholar]
- 4.Rash R, Risk M. Influence of pneumo peritoneum and patient positions on respiratory system compliance. J Clin Anesth. 2001;13L:361–3. doi: 10.1016/s0952-8180(01)00286-0. [DOI] [PubMed] [Google Scholar]
- 5.Haydon GH, Dillon J, Simpson KJ, Thomas H, Hayes PC. Hypoxemia during diagnostic laparoscopy: A prospective study. Gastrointest Endosc. 1996;44:124–8. doi: 10.1016/s0016-5107(96)70128-1. [DOI] [PubMed] [Google Scholar]
- 6.Nichols D, Haranath S. Pressure control ventilation. Crit Care Clin. 2007;23:183–99. doi: 10.1016/j.ccc.2006.12.005. viii-ix. [DOI] [PubMed] [Google Scholar]
- 7.Maeda Y, Fujino Y, Uchiyama A, Matsuura N, Mashimo T, Nishimura M. Effects of peak inspiratory flow on development of ventilator-induced lung injury in rabbits. Anesthesiology. 2004;101:722–8. doi: 10.1097/00000542-200409000-00021. [DOI] [PubMed] [Google Scholar]
- 8.Keszler M. Volume-targeted ventilation. Early Hum Dev. 2006;82:811–8. doi: 10.1016/j.earlhumdev.2006.09.008. [DOI] [PubMed] [Google Scholar]
- 9.Keszler M, Abubakar K. Volume guarantee: Stability of tidal volume and incidence of hypocarbia. Pediatr Pulmonol. 2004;38:240–5. doi: 10.1002/ppul.20063. [DOI] [PubMed] [Google Scholar]
- 10.Hoo GW. Barotrauma and mechanical ventilation. E medicine. [Last accessed on 2016 Apr]. Available from: http://www.Medscape.com/article/296625-overview#a2 .
- 11.Eisner MD, Thompson BT, Schoenfeld D, Anzueto A, Matthay MA Acute Respiratory Distress Syndrome Network. Airway pressures and early barotrauma in patients with acute lung injury and acute respiratory distress syndrome. Am J Respir Crit Care Med. 2002;165:978–82. doi: 10.1164/ajrccm.165.7.2109059. [DOI] [PubMed] [Google Scholar]
- 12.Leopoldo E, Zaccaro F, Niño C, Manrique F, Benítez D, Mantilla H. Comparison of Volume Control Ventilation (VCV), Pressure Control Ventilation (PCV) and Pressure Control Ventilation-volume Guarantee (PCV-VG) in Patients Undergone Laparoscopic Cholecystectomy; A1129. [Last accessed on 2016 May]. Available from: htttp://www.asaabstracts.com/strands/asaabstracts/abstractlist.htm?index=18 .
- 13.Dion JM, McKee C, Tobias JD, Sohner P, Herz D, Teich S, et al. Ventilation during laparoscopic-assisted bariatric surgery: Volume-controlled, pressure-controlled or volume-guaranteed pressure-regulated modes. Int J Clin Exp Med. 2014;7:2242–7. [PMC free article] [PubMed] [Google Scholar]
- 14.Boules NS, Ghobrial HZ. Efficiency of a newly introduced mode pressure controlled volume guaranteed mode in thoracic surgery with one lung ventilation. Egypt J Anaesth. 2011;27:113–9. [Google Scholar]
- 15.Song SY, Jung JY, Cho MS, Kim JH, Ryu TH, Kim BI. Volume-controlled versus pressure-controlled ventilation-volume guaranteed mode during one-lung ventilation. Korean J Anesthesiol. 2014;67:258–63. doi: 10.4097/kjae.2014.67.4.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cadi P, Guenoun T, Journois D, Chevallier JM, Diehl JL, Safran D. Pressure-controlled ventilation improves oxygenation during laparoscopic obesity surgery compared with volume-controlled ventilation. Br J Anaesth. 2008;100:709–16. doi: 10.1093/bja/aen067. [DOI] [PubMed] [Google Scholar]
- 17.Aldenkortt M, Lysakowski C, Elia N, Brochard L, Tramèr MR. Ventilation strategies in obese patients undergoing surgery: A quantitative systematic review and meta-analysis. Br J Anaesth. 2012;109:493–502. doi: 10.1093/bja/aes338. [DOI] [PubMed] [Google Scholar]
- 18.Strang CM, Fredén F, Maripuu E, Hachenberg T, Hedenstierna G. Ventilation-perfusion distributions and gas exchange during carbon dioxide-pneumoperitoneum in a porcine model. Br J Anaesth. 2010;105:691–7. doi: 10.1093/bja/aeq211. [DOI] [PubMed] [Google Scholar]
- 19.Andersson L, Lagerstrand L, Thörne A, Sollevi A, Brodin LA, Odeberg-Wernerman S. Effect of CO(2) pneumoperitoneum on ventilation-perfusion relationships during laparoscopic cholecystectomy. Acta Anaesthesiol Scand. 2002;46:552–60. doi: 10.1034/j.1399-6576.2002.460513.x. [DOI] [PubMed] [Google Scholar]
- 20.Gupta SD, Kundu SB, Ghose T, Maji S, Mitra K, Mukherjee M, et al. A comparison between volume-controlled ventilation and pressure-controlled ventilation in providing better oxygenation in obese patients undergoing laparoscopic cholecystectomy. Indian J Anaesth. 2012;56:276–82. doi: 10.4103/0019-5049.98777. [DOI] [PMC free article] [PubMed] [Google Scholar]


