Abstract
Introduction:
This study compares the efficacy in terms of pain relief and complications of intra-articular Botulinum toxin-A (BoNT-A) with intra-articular Triamcinolone versus Triamcinolone alone in the treatment of osteoarthritic knee pain of severe grade. If effective, BoNT-A may help in reducing the long term adverse effects due to prolonged analgesic consumption and reduce/delay requirement of knee replacement surgeries.
Materials and Methods:
In this prospective study, 30 patients of either sex, aged between 40 to 60 years with physical status ASA classes I or II suffering from knee joint osteoarthritis with knee pain and functional impairment were divided into 2 groups: The OA patients which received Botulinum toxin-A with Triamcinolone (Group A) & OA patients which received only Triamcinolone (Group B). Only patients with advanced OA of the knee; radiographically verified with a Joint space <2 mm were included. The efficacy of pain relief in the 2 groups were compared using Visual analog score (VAS) and Oxford knee Score and followed upto 6 months.
Results and Conclusions:
On comparing the VAS Score during the follow up period, there was a significant difference between groups A and B upto 3 months. During post treatment follow up, there was significant difference in pain relief as measured by the Oxford Knee score from 4 weeks to 6 months, where Group A patients fared much better in terms of pain relief than group B with a highly significant value of P =<0.001 during the time period of 6 weeks to 6 months. The study shows that the use intra-articular Botulinum toxin-A with steroid is far superior to intra-articular steroid alone in terms of pain relief as well as functional outcome.
Keywords: Botulinum toxin-A, intra-articular steroid, osteoarthritis
INTRODUCTION
Osteoarthritis (OA) is the most common joint disorder worldwide. Approximately 11% of people older than 64 years have symptomatic knee OA.[1] The third National Health and Nutrition Examination Survey revealed that more than 21% of 6596 respondents at least 60 years of age have significant knee pain on most days and concluded that although radiographic confirmation would be needed, OA was the most likely cause of the majority of this pain.[2]
Symptoms of knee OA include pain and reduced function as well as swelling, morning stiffness lasting <30 min, joint enlargement, deformity, grinding, clicking, and joint instability or buckling. Signs include muscle atrophy, weakness, joint effusion, crepitus, bony tenderness and enlargement, altered gait, limitation of motion, deformity, and instability. Radiographs are characterized by marginal osteophytes, joint space narrowing, malalignment, subchondral sclerosis, and subchondral cyst formation.[3] Pain and reduced function impact the quality of life of people with knee OA, and the symptoms may be exacerbated by trauma, obesity, and psychological factors.
Pain is the most prominent symptom of OA and most often is the reason patients seek medical help. The most often involved joint in OA is the knee joint. Osteoarthritic pain is amenable to a wide modality of treatment such as nonsteroidal anti-inflammatory drugs (NSAIDS) and other analgesics as well as intra-articular treatment with local anesthetics, steroids, hyaluronidase, etc. Corticosteroid injections have been used successfully in a number of conditions, with OA the most common and best studied. Botulinum toxin type A (BoNT-A) is a new therapeutic option for treatment for refractory OA knee joint pain. BoNT-A is a presynaptic neuromuscular blocking agent that triggers chemical denervation by temporarily suppressing secretion of acetylcholine at motor nerve endings; therefore, BoNT-A injections are useful for diseases with increased involuntary muscle activity or tension.[4] Intraarticular BoNT-A injections are an effective and safe treatment for chronic joint pain disorders.[5] There are studies which suggest that BoNT-A may be a therapeutic option for patients with knee OA pain to maintain function and decrease pain when intra-articular corticosteroids and other first- and second-line therapies have failed or are not an option.[6]
The objective of this study is to compare the efficacy in terms of pain relief and complications of intra-articular BoNT-A with intra-articular triamcinolone in the treatment of osteoarthritic knee pain. If proven as an effective treatment modality, then BoNT-A may help in reducing the long-term adverse effects due to prolonged analgesic consumption and reduce/delay requirement of knee replacement surgeries. Fragile patients unfit for knee replacement surgery may get an alternate option.
MATERIALS AND METHODS
This was a prospective study in which thirty patients of either sex suffering from knee pain due to advanced OA, with physical status American Society of Anesthesiologists Classes I or II, refractory to NSAIDs were included on the basis of diagnosis made by plain X-ray knee joint anteroposterior (AP) and lateral (LAT) view defined as joint space less than 2 mm. It was further confirmed by a dry tap on joint aspiration. Patients with rheumatoid arthritis, trauma, or any other comorbidity were excluded.
All patients included in the study were evaluated clinically by taking a detailed history and physical examination. Other than X-Ray (AP and LAT VIEW) of knee joint, all patients underwent routine blood investigations such as complete blood picture and rheumatoid factor titre.
After explaining the procedure and taking informed consent, patients were randomly allocated in any of the following groups:
Group A: BoNT-A with Triamcinolone
Group B: Triamcinolone alone.
Procedure
Procedure site infiltrated with local anesthetic agent
Fluoroscopically guided 20-G 10 cm needle was inserted using the triangle technique described by Lockman, and synovial fluid is aspirated
A dry tap meant advanced OA, and then, the patient was selected for any of the above-mentioned technique, i.e., BoNT-A(100 IU) with Triamcinolone or Triamcinolone (40 IU) alone
Intraoperatively and during postoperative period patients’ vitals were monitored including heart rate, noninvasive blood pressure, and oxygen saturation
The patients were followed for immediate and long-term relief of pain (subjective/objective) using visual analog scale (VAS) score, and functional improvement using Oxford knee score, at an interval of day 1, 2 weeks, 4 weeks, 6 weeks, 3 months, and 6 months.
RESULTS
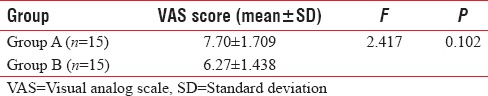
The age and sex distribution in both groups were comparable [Tables 1 and 2]. Table 3 shows there was no significant difference in the baseline Oxford knee scores in both groups (P = 0.426). Table 4 shows there was no significant difference in the baseline visual analog scores in both groups (P = 0.102).
Table 1.
Age distribution
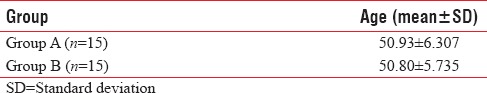
Table 2.
Sex distribution (P=0.678)
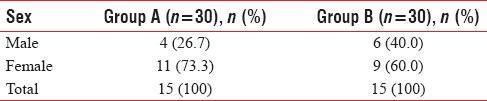
Table 3.
Oxford knee score (baseline)
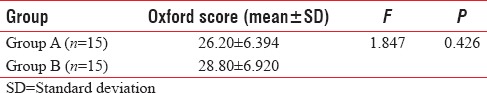
Table 4.
Visual analog scale score (baseline)
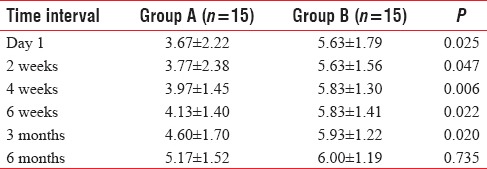
During posttreatment follow-up of the patients, it was seen that there was no significant difference in pain relief as measured by the Oxford Knee score up to 2 weeks (P = 0.09). From 4 weeks to 6 months, Group A patients fared much better in terms of pain relief than Group B with a highly significant value of P ≤ 0.001 from 6 weeks to 6 months [Table 5]. On comparing VAS scores, there was a significant difference between the two groups up to 3 months [Table 6].
Table 5.
Comparison of oxford knee score in all three groups at different time interval
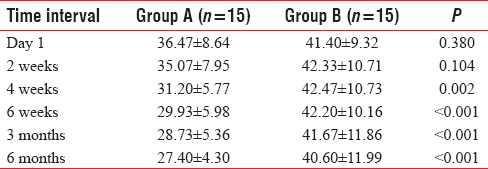
Table 6.
Comparison of visual analog scale score in all three groups at different time interval
DISCUSSION
This study was aimed to evaluate and compare the efficacy of newer modality of pain relief in advanced OA of knee joint namely intra-articular BoNT with the current standard intra-articular steroid injection. The patients in the two groups were statistically similar with reference to site of pain, joint swelling, restriction of movement, and intensity of pain before the procedure. Baseline Oxford Knee score and VAS score were similar in both groups with no significant difference between them. Pain relief as observed by VAS score was significantly better in patients receiving intra-articular BoNT as compared to intra-articular steroids (P < 0.05). The onset of pain relief in patients receiving intra-articular botulinum group was seen after 2 weeks and persisted for 6 months which is similar to the observations made by Singh et al. who reported 42%–100% pain reduction in OA patients receiving intra-articular BoNT-A which lasted up to 12 months.[7] However, this long-lasting effect may be because of the repeated injections (one to three times) given to the patients in their series, whereas in this study only a single injection was given.
An insignificant pain relief was observed in the intra-articular steroid group based on VAS score while BoNT group showed significant pain relief up to 3 months. The functional improvement as observed by Oxford knee score was definitely better in intra-articular BoNT group as compared to intra-articular steroid group (P < 0.002) but only after 4 weeks. At 6-month interval, a highly significant improvement was seen in intra-articular BoNT group when compared to intra-articular steroid group (P < 0.001). It is clearly evident from these observations that functional improvement was significantly better in intra-articular BoNT group. Similar observations were made by Boon et al. who reported statistically significant functional improvement in patients receiving intra-articular BoNT.[8]
CONCLUSIONS
From the study, we conclude that pain relief as well as functional improvement with intra-articular BoNT is better and long-lasting in comparison to intra-articular corticosteroid but is of delayed onset.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Manek NJ, Lane NE. Osteoarthritis: Current concepts in diagnosis and management. Am Fam Physician. 2000;61:1795–804. [PubMed] [Google Scholar]
- 2.Andersen RE, Crespo CJ, Ling SM, Bathon JM, Bartlett SJ. Prevalence of significant knee pain among older Americans: Results from the Third National Health and Nutrition Examination Survey. J Am Geriatr Soc. 1999;47:1435–8. doi: 10.1111/j.1532-5415.1999.tb01563.x. [DOI] [PubMed] [Google Scholar]
- 3.Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage. 2007;15(Suppl A):A1–56. doi: 10.1016/j.joca.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 4.Lew MF. Review of the FDA-approved uses of botulinum toxins, including data suggesting efficacy in pain reduction. Clin J Pain. 2002;18:S142–6. doi: 10.1097/00002508-200211001-00005. [DOI] [PubMed] [Google Scholar]
- 5.Mahowald ML, Singh JA, Dykstra D. Long term effects of intra-articular botulinum toxin A for refractory joint pain. Neurotox Res. 2006;9:179–88. doi: 10.1007/BF03033937. [DOI] [PubMed] [Google Scholar]
- 6.Recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. American College of Rheumatology Subcommittee on Osteoarthritis Guidelines. Arthritis Rheum. 2000;43:1905–15. doi: 10.1002/1529-0131(200009)43:9<1905::AID-ANR1>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 7.Singh JA, Mahowald ML, Kushnaryov A, Goelz E, Dykstra D. Repeat injections of intra-articular botulinum toxin a for the treatment of chronic arthritis joint pain. J Clin Rheumatol. 2009;15:35–8. doi: 10.1097/RHU.0b013e3181953b14. [DOI] [PubMed] [Google Scholar]
- 8.Boon AJ, Smith J, Dahm DL, Sorenson EJ, Larson DR, Fitz-Gibbon PD, et al. Efficacy of intra-articular botulinum toxin type A in painful knee osteoarthritis: A pilot study. PM R. 2010;2:268–76. doi: 10.1016/j.pmrj.2010.02.011. [DOI] [PubMed] [Google Scholar]


