Abstract
Background:
The supraclavicular approach is considered to be the easiest and most effective approach to block the brachial plexus for upper limb surgeries. The classical approach using the anatomical landmark technique was associated with higher failure rates and complications. Ultrasonography (USG) guidance and peripheral nerve stimulator (PNS) have improved the success rates and safety margin.
Aims:
The aim of the present study is to compare USG with PNS in supraclavicular brachial plexus block for upper limb surgeries with respect to the onset of motor and sensory blockade, total duration of blockade, procedure time, and complications.
Settings and Design:
Prospective, randomized controlled study.
Subject and Methods:
Sixty patients aged above 18 years scheduled for elective upper limb surgery were randomly allocated into two groups. Group A patients received supraclavicular brachial plexus block under ultrasound guidance and in Group B patients, PNS was used. In both groups, local anesthetic mixture consisting of 15 ml of 0.5% bupivacaine and 10 ml of 2% lignocaine with 1:200,000 adrenaline were used.
Statistical Analysis:
Independent t-test used to compare mean between groups; Chi-square test for categorical variables.
Results:
The procedure time was shorter with USG (11.57 ± 2.75 min) compared to PNS (21.73 ± 4.84). The onset time of sensory block (12.83 ± 3.64 min vs. 16 ± 3.57 min) and onset of motor block (23 ± 4.27 min vs. 27 ± 3.85 min) were significantly shorter in Group A compared to Group B (P < 0.05). The duration of sensory block was significantly prolonged in Group A (8.00 ± 0.891 h) compared to Group B (7.25 ± 1.418 h). None of the patients in either groups developed any complications.
Conclusion:
The ultrasound-guided supraclavicular brachial plexus block can be done quicker, with a faster onset of sensory and motor block compared to nerve stimulator technique.
Keywords: Nerve stimulator, supraclavicular block, ultrasound
INTRODUCTION
The supraclavicular approach is considered the easiest and most effective approach to block the brachial plexus. The classical approach of using paresthesia to identify the nerve cluster using anatomical landmarks may be associated with a higher failure rate and injury to the nerves or vascular structures.[1]
The peripheral nerve stimulator (PNS) allows better localization of the brachial plexus by locating the nerves using a low-intensity electric current (up to 2.5 mA) for a short-duration (0.05–1 ms) with an insulated needle to obtain a defined response of muscle twitch or sensation and to inject local anesthetic solution in close proximity to the nerve.[2] This technique, however, did not reduce the risk of injury to surrounding structures.[3] The application of ultrasonography (USG) to localize the brachial plexus has revolutionized the field of regional anesthesia. However, the cost and the expertise required are the limiting factors.[4] This study was done to compare the above two techniques with respect to procedure time, block characteristics, and complication rate.
SUBJECT AND METHODS
After institutional ethical committee approval, sixty patients scheduled for elective upper limb surgery were included in the study.
Inclusion criteria
Age between 18 and 80 years, American Society of Anaesthesiologists (ASA) physical status Classification I to III.
Exclusion criteria
Refusal to participate, history of neurological diseases, coagulopathy and infection at the site of block, allergy to local anesthetics.
All patients underwent preanesthetic checkup on the day before surgery. Patients were premedicated with oral ranitidine 150 mg, metoclopramide 10 mg, and lorazepam 1 mg on the night before the procedure and 2 h before the surgery. Patients were shifted to operation theater on call and routine monitors such as electrocardiogram (ECG), noninvasive blood pressure, and pulse oximetry were applied. Intravenous cannulation was done on the nonoperating hand.
All patients were randomly allocated to either Group A (ultrasound) or Group B (nerve stimulator). The local anesthetic solution used was a mixture of 0.5% bupivacaine 15 ml and 10 ml of 2% lignocaine with 1:200,000 adrenaline to make a total volume of 25 ml.
Group A
Ultrasound-guided supraclavicular block was performed using a Sonosite Ultrasound machine with a 4 cm linear transducer with a frequency of 5–10 MHz. The needle from a 18G cannula was attached to a 10 cm extension for drug injection. The patients were placed in a supine position with a shoulder roll under the patient, and the head turned away from the side to be blocked, and the arm was held downward to depress the clavicle. The ultrasound probe was placed in a sterile plastic sheath and placed in an oblique plane in the supraclavicular region. The brachial plexus was identified as a honeycombed hyper and hypoechoic structure lateral to subclavian artery above first rib and pleura. After skin infiltration with 2% lignocaine, an 18G needle attached to a three-way extension was introduced through the skin. Once the needle was visualized on the screen, it was slowly advanced into the sheath of the brachial plexus, with the subclavian artery as the landmark. Under vision, 2 ml of saline was injected to observe the spread. When the spread was satisfactory, after negative aspiration, the local anesthetic solution was injected into the brachial plexus sheath under vision in at least two different needle positions around the subclavian artery.
Group B
In this group, the positive electrode from the PNS is attached to an ECG lead and placed in the ipsilateral shoulder, and the negative electrode is attached to a 20G insulated needle. After skin preparation, the subclavian artery was palpated in the supraclavicular region and skin was infiltrated with 2% lignocaine immediately lateral to the artery. The point of needle entrance was about one inch lateral to the insertion of the sternocleidomastoid on the clavicle. The needle was inserted through the skin in a downward and inward direction with the PNS set to deliver 1.5–2.5 mA current at 1 Hz frequency and 0.1 ms of pulse duration. The needle was slowly advanced until the upper trunk was identified by a muscle twitch of the shoulder muscles. At this point, the orientation of the needle was changed to advance it caudally under the palpating finger, with a slight posterior angle. This strategy directs the needle from the vicinity of the upper trunk (shoulder twitch) to the front of the medial trunk (biceps, triceps, and pectoralis twitch) on its way to the lower trunk (fingers twitch). The goal of this block was to bring the tip of the needle in the proximity of the lower trunk, which is manifested by a twitch of the fingers in either flexion or extension. Once the finger twitch was obtained, the current was gradually reduced to 0.5 mA and then the local anesthetic solution was injected after negative aspiration.
The time interval between the first needle insertion and its removal at the end of the block is taken as the procedure time. Sensory evaluation for pain and touch was done for the entire cutaneous innervation of upper limb, i.e., musculocutaneous, radial, ulnar, median, medial cutaneous nerves of arm and forearm and intercostobrachial nerve. The sensory block in each dermatome was evaluated using the following scale.
2 - normal sensation
1 - hypoesthesia
0 - no sensation felt.
The time from the removal of block needle to the time when a score of zero has been achieved was taken as onset time of sensory block for each nerve.
Motor block was assessed after 5, 10, 15, 20 and 30 min after injection of the drug according to modified Bromage scale for upper extremities.[5] Flexion, extension, abduction, adduction was checked at the elbow, wrist, and fingers. The time from the removal of block needle to the time when modified Bromage grade of zero has been achieved was taken as onset time of motor block.
Modified Bromage grade to assess upper limb motor weakness:
Grade 0: Normal motor function with full extension of elbow, wrist, and fingers
Grade 1: Ability to flex and extend wrist and fingers
Grade 2: Ability to flex and extend only fingers
Grade 3: Complete motor block with the inability to move elbow, wrist, and finger.
During the surgery, mild sedation (intravenous Midazolam 1–2 mg) was administered. In case of insufficient analgesia, supplementation was given with intravenous fentanyl 1 mcg/kg. If the patient still had pain, then general anesthesia was given, and the block was considered failed. All patients were monitored postoperatively in the postanesthesia care unit for 1 h and thereafter discharged to their ward. The following were also noted.
The need for intraoperative supplementary systemic medication
Conversion to general anesthesia (block failure)
Adverse effects (defined as vessel puncture, newly observed cardiac dysrhythmias, seizure, transcutaneous oxygen saturation lower than 90%, Horner's syndrome, signs of local anesthetic toxicity, and pneumothorax) were recorded.
Postoperative pain at the surgical site was assessed using a 10-point visual analog scale (0 = no pain and 10 = worst imaginable pain), and a score of more than 3 was taken as the endpoint for the duration of the block. Patients were evaluated 24 h after the block for complications such as persisting paresthesia and pneumothorax.
Statistical analysis
Statistical analyses were performed using SPSS version 16.0 (SPSS Inc., Chicago, IL, USA). Data were expressed in mean and standard deviation for continuous variables, numbers, and percentage for categorical variables. Independent t-test was used to compare the mean between the groups and Chi-square test used for categorical variables. P < 0.05 is considered statistically significant.
RESULTS
The mean age, weight, gender, and ASA physical state classification of the patients in both groups were comparable, and the P value between the groups was <0.05, i.e., statistically insignificant. The mean heart rate, systolic, and diastolic blood pressure were comparable between the groups.
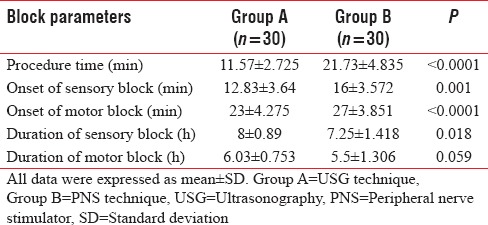
The mean procedure time was 11.57 ± 2.725 min in Group A compared to 21.73 ± 4.835 min in Group B, which was statistically significant (P < 0.0001). The mean onset time of sensory block (score 0) was 16 ± 3.572 min in Group B and 12.83 ± 3.64 min in Group A, which was statistically significant (P = 0.001). The mean onset time of motor block was 27 ± 3.851 min in Group B and 23 ± 4.275 min in Group A and was statistically significant (P < 0.0001).
As shown in Table 1, the mean duration of sensory block was significantly higher in Group A compared to Group B (8 ± 0.89 min vs. 7.25 ± 1.418 min). However, there was no significant difference in the mean duration of the motor block between the two groups. There was also no significant difference in the requirement of intravenous fentanyl supplementation. None of the patients in either groups developed any adverse effects such as arterial puncture, nerve injury, pneumothorax, and local anesthetic toxicity. In Group B, out of 30 patients, only five required analgesic supplementation with intravenous fentanyl compared to Group B, though this was not statistically significant. None of the patients in either groups required conversion to general anesthesia.
Table 1.
Block parameters
DISCUSSION
Supraclavicular block is one of the most commonly practiced approaches for brachial plexus block since it provides consistent and predictable anesthesia of the entire upper extremity. In 1962 Greenblatt and Denson pioneered the use of peripheral nerve stimulation technique to locate the peripheral nerves.[6] Since the last few decades, nerve stimulator was considered the gold standard for performing the peripheral nerve blocks. la Grange et al. in 1978 reported the use of Doppler USG in performing supraclavicular block by identifying subclavian vessels.[7] The use of USG helps in identifying the brachial plexus and to guide the needle thereby minimizing the risk of injury to the nearby structures. This study was done to compare the above two techniques for performing supraclavicular block with respect to efficiency and complication rate.
In our study, the mean procedure time was significantly shorter in Group A than Group B (11.57 ± 2.75 min vs. 21.73 ± 4.835 min, respectively) similar to Singh et al., who observed significantly shorter procedure time in USG group compared to PNS group during supraclavicular block (8.14 vs. 10.63 min, respectively).[8] Similarly, Williams et al. and Ratnawat et al. found a significantly shorter time to perform the block with USG than the PNS.[9,10] However, Duncan et al. observed a comparable procedural time with the above two techniques.[11] The procedure time was greater in the nerve stimulator group because of the variability in the relationship between the surface anatomy and nerve location whereas use of USG may minimize this variation. Furthermore, PNS technique took a longer time since the initial response was seen at the shoulder and then the needle position had to be adjusted slightly posteriorly to get finger twitches. With USG guidance, positioning, and any repositioning of the needle is performed under direct vision whereas in the PNS technique, landmark technique is used to locate the plexus requiring repeated needle pricks and needle repositioning ultimately leading to longer procedure time.
The mean onset time for sensory and motor block was found to be significantly shorter in Group A (12.83 ± 3.640 min and 23 ± 4.275 min, respectively) when compared to Group B (16 ± 3.572 min and 27 ± 3.851 min, respectively). This is similar to the study done by Ratnawat et al. in which the mean onset time of sensory and motor block was significantly shorter in USG group (6.46 ± 1.02 min and 8.10 ± 1.02 min, respectively) compared to the PNS group (7.68 ± 1.33 min and 9.94 ± 1.28 min, respectively).[10] However, our findings were in contrary to the study done by Duncan et al., in which the onset time of sensory and motor block was comparable between the USG and PNS groups.[11]
The mean duration of sensory block was significantly prolonged in Group A (8.00 ± 0.891 h) compared to Group B (7.25 ± 1.418 h). However, the mean duration of motor block was comparable in both the groups (P = 0.059). Ratnawat et al. observed a significantly prolonged duration of sensory and motor block in USG group (8.13 ± 1.63 h and 7.13 ± 1.63 h respectively) than the PNS group (6.14 ± 2.36 h and 5.14 ± 2.36 h, respectively) with 30 ml of 0.5% ropivacaine solution.[10] Singh et al. also observed a prolonged block with USG. Our findings are in contrary with Duncan et al., in which both the USG and PNS groups had comparable mean duration of sensory and motor with 1:1 mixture of 0.5% bupivacaine and 2% lignocaine with 1:200,000 adrenaline.[11] The sonographic imaging-guided supraclavicular block helps in assessing the size, depth, and exact location along with the anatomy of the adjacent structures. USG assists in exact placement of the needle and helps in depositing the local anesthetic in the accurate site and also helps in visualizing the spread of the drug. This, in turn, hastens the onset of the block and may explain the prolonged duration of block seen in our study.
In our study, five out of thirty patients in Group B required supplementation of analgesia with intravenous Fentanyl, whereas none of the patients in Group A required supplementation. After applying Fisher's exact t-test, this was not found to be statistically significant (P = 0.052). None of the patients in both the groups required conversion to general anesthesia, and hence there were no failure of blocks in both groups. Singh et al. have observed that out of 102 patients, 45 out of 50 (90%) patients had developed successful block with USG, compared to 38 of 52 (73.1%) in Group PNS requiring additional nerve blocks (P = 0.028).[8] Duncan et al. and Williams et al. observed a comparable rate of the successful block with both the groups though there were block failures with both USG and PNS in these studies.[9,11] Jeon and Kim observed that success rates were 93.7% and 75.0% when a distal response and proximal response were noted, respectively, using a PNS for supraclavicular block.[12] In our study, we elicited both proximal and distal muscle response in the PNS group, which may explain the absence of block failures in the PNS group.
There was no incidence of complications such as arterial puncture, pneumothorax and nerve injury in both groups in our study similar to Duncan et al. Singh et al. reported seven vascular punctures in the PNS group, while only one in the USG group during check aspiration.[11] Several studies have shown nil or lesser incidence of complications with the use of USG as it helps in direct visualization of the needle with relation to the cervical pleura thereby avoiding the puncture of pleura and development of pneumothorax.[13,14,15]
One of the limitations of this study is the small sample size of only 60 patients. A multicentric study with a large sample size will give a better picture of the incidence of complications such as arterial puncture and pneumothorax. The number of needle pricks and needle readjustments which will be helpful in assessing patient discomfort and satisfaction were not recorded in our study.
CONCLUSION
We observed shorter procedure time, faster onset time of sensory and motor block with USG guided supraclavicular block. In addition, the duration of sensory block was significantly more with the USG technique compared to the PNS technique. There was no incidence of complications such as arterial puncture, nerve injury and pneumothorax with both the techniques. We conclude USG-guided supraclavicular block to be significantly better in terms of procedure time and block characteristics during upper limb surgeries compared to the nerve stimulator technique. Furthermore, nerve stimulator can be safely used in situ ations when USG machine availability is limited. Further studies with large sample size are required to assess and compare the incidence of complications with these techniques.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Carty S, Nicholls B. Ultrasound-guided regional anaesthesia. Continuing Education in Anaesthesia Critical Care & Pain. 2007;1:20–4. [Google Scholar]
- 2.Fanelli G, Casati A, Garancini P, Torri G. Nerve stimulator and multiple injection technique for upper and lower limb blockade: Failure rate, patient acceptance, and neurologic complications. Study Group on Regional Anesthesia. Anesth Analg. 1999;88:847–52. doi: 10.1097/00000539-199904000-00031. [DOI] [PubMed] [Google Scholar]
- 3.Brown DL, Cahill DR, Bridenbaugh LD. Supraclavicular nerve block: Anatomic analysis of a method to prevent pneumothorax. Anesth Analg. 1993;76:530–4. doi: 10.1213/00000539-199303000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Chan VW, Perlas A, Rawson R, Odukoya O. Ultrasound-guided supraclavicular brachial plexus block. Anesth Analg. 2003;97:1514–7. doi: 10.1213/01.ANE.0000062519.61520.14. [DOI] [PubMed] [Google Scholar]
- 5.Gaumann D, Forster A, Griessen M, Habre W, Poinsot O, Della Santa D, et al. Comparison between clonidine and epinephrine admixture to lidocaine in brachial plexus block. Anesth Analg. 1992;75:69–74. doi: 10.1213/00000539-199207000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Greenblatt GM, Denson JS. Needle nerve stimulatorlocator: Nerve blocks with a new instrument for locating nerves. Anesth Analg. 1962;41:599–602. [PubMed] [Google Scholar]
- 7.la Grange P, Foster PA, Pretorius LK. Application of the Doppler ultrasound bloodflow detector in supraclavicular brachial plexus block. Br J Anaesth. 1978;50:965–7. doi: 10.1093/bja/50.9.965. [DOI] [PubMed] [Google Scholar]
- 8.Singh S, Goyal R, Upadhyay KK, Sethi N, Sharma RM, Sharma A, et al. An evaluation of brachial plexus block using a nerve stimulator versus ultrasound guidance: A randomized controlled trial. J Anaesthesiol Clin Pharmacol. 2015;31:370–4. doi: 10.4103/0970-9185.161675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williams SR, Chouinard P, Arcand G, Harris P, Ruel M, Boudreault D, et al. Ultrasound guidance speeds execution and improves the quality of supraclavicular block. Anesth Analg. 2003;97:1518–23. doi: 10.1213/01.ANE.0000086730.09173.CA. [DOI] [PubMed] [Google Scholar]
- 10.Ratnawat A, Bhati FS, Khatri C, Srinivasan B, Sangwan P, Chouhan DS. Comparative study between nerve stimulator guided technique and ultrasound guided technique of supraclavicular nerve block for upper limb surgery. Int J Res Med Sci. 2016;4:2101–6. [Google Scholar]
- 11.Duncan M, Shetti AN, Tripathy DK, Roshansingh D, Krishnaveni N. A comparative study of nerve stimulator versus ultrasound-guided supraclavicular brachial plexus block. Anesth Essays Res. 2013;7:359–64. doi: 10.4103/0259-1162.123235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jeon DG, Kim WI. Comparison of a supraclavicular block showing upper arm twitching response with a supraclavicular block showing wrist or finger twitching response. Korean J Anesthesiol. 2010;58:464–7. doi: 10.4097/kjae.2010.58.5.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rupera KB, Khara BN, Shah VR, Parikh BK. Supra-clavicular brachial plexus block: Ultra-sonography guided technique offer advantage over peripheral nerve stimulator guided technique. Natl J Med Res. 2013;3:241–4. [Google Scholar]
- 14.Yuan JM, Yang XH, Fu SK, Yuan CQ, Chen K, Li JY, et al. Ultrasound guidance for brachial plexus block decreases the incidence of complete hemi-diaphragmatic paresis or vascular punctures and improves success rate of brachial plexus nerve block compared with peripheral nerve stimulator in adults. Chin Med J (Engl) 2012;125:1811–6. [PubMed] [Google Scholar]
- 15.Kapral S, Krafft P, Eibenberger K, Fitzgerald R, Gosch M, Weinstabl C, et al. Ultrasound-guided supraclavicular approach for regional anesthesia of the brachial plexus. Anesth Analg. 1994;78:507–13. doi: 10.1213/00000539-199403000-00016. [DOI] [PubMed] [Google Scholar]


