Abstract
Background:
Several studies have been conducted in search of appropriate drugs to attenuate hemodynamic responses in laparoscopic cholecystectomy, but till date, no such study has been conducted on patients undergoing laparoscopic nephrectomy.
Aim:
The study was designed to assess the effect of esmolol and diltiazem infusions on hemodynamic changes during routine laparoscopic transperitoneal simple nephrectomy.
Settings and Design:
A prospective double-blinded randomized control trial.
Subjects and Methods:
A total of 120 nonhypertensive patients of the American Society of Anesthesiologists physical Status I and II aged 20–60 years about to undergo laparoscopic nephrectomy were enrolled for the study after obtaining Institute Ethical committee approval. The patients were randomly allocated to one of the three groups. Group I (control group) received 10 ml normal saline intravenously (i.v.) before induction of anesthesia, followed by continuous infusion 10–20 ml/h. Group II (esmolol group) received i.v. esmolol 1 mg/kg diluted in 10 ml similarly, followed by continuous infusion of 10–20 ml/h (5–10 μg/kg/min). Group III (diltiazem group) received i.v. diltiazem 0.2 mg/kg diluted in 10 ml before induction of anesthesia, followed by continuous infusion at 10–20 ml/h (0.08–1.25) μg/kg/min. After completion of surgery, all the infusions were stopped. Data recording were done for changes in hemodynamics throughout the surgery.
Statistical Analysis:
was done using Chi-square test for categorical data and one-way ANOVA for continuous data. Tukey (“honestly significant difference”) post hoc test was applied for intra- and inter-group comparison in cases where ANOVA was significant. P < 0.05 is considered statistically significant.
Results:
All hemodynamic data: Heart rate (HR), systolic, diastolic, and mean arterial pressure were observed to be significantly higher (P < 0.001) from baseline in control group at the time of creation of pneumoperitoneum, till 20 min thereafter. The values were comparable to baseline in both esmolol and diltiazem group. On intergroup comparison, the patients in esmolol group had significantly lower HR and blood pressures than in diltiazem group at the creation of pneumoperitoneum and at extubation (P < 0.05). Mean dose of esmolol and diltiazem used were 7.25 ± 1.33 μg/kg/min and 1.14 ± 0.77 μg/kg/min, respectively.
Conclusion:
Both esmolol and diltiazem infusion provide stable intraoperative hemodynamics and protection against stress response triggered by pneumoperitoneum in patients undergoing laparoscopic transperitoneal nephrectomy.
Keywords: Diltiazem, esmolol, laparoscopic nephrectomy
INTRODUCTION
The advancement of medical sciences has led us to an era of laparoscopic surgeries. Such surgeries though allow faster recovery, are associated with marked hemodynamic disturbances mainly attributed to the creation of pneumoperitoneum.[1] The nature of changes includes a decrease in cardiac output and increase in systemic vascular resistance due to increased abdominal pressures and release of catecholamines such as noradrenaline and adrenaline. This sympathetic surge initially leads to increase in heart rate (HR) and mean arterial pressure (MAP) which alters the hemodynamic of the body.[1,2] Many drugs have befriended anesthesiologists for attenuating responses during creation and maintenance of pneumoperitoneum.[3,4,5,6,7,8] All the studies to decrease stress response to pneumoperitoneum have been done in patients undergoing laparoscopic cholecystectomy or laparoscopic gynecological surgeries.[3,4,5,6,7,8] Laparoscopic urological procedures have now become a norm in most of the advanced medical centers. However, literature lacks prospective data on laparoscopic urological cases especially laparoscopic nephrectomies. This study aims to deal with the problem of increased hemodynamic responses to the creation of pneumoperitoneum in patients undergoing laparoscopic transperitoneal nephrectomy. Infusion of short-acting beta-blocker esmolol has been used previously for hemodynamic attenuation in laparoscopic cholecystectomy.[6,8] Taking the rationale from Conacher et al. that “Renal and upper urinary tract procedures have sufficient in common for laparoscopic cholecystectomy to be the model” we have used an infusion of esmolol in one group in the present study. In the second group, we have used infusion of a calcium channel blocker diltiazem. Intravenous diltiazem has been used previously to attenuate hemodynamic responses to tracheal intubation and extubation.[9,10] Diltiazem, however, has never been used to curb response of pneumoperitoneum. The present double-blind prospective randomized controlled study was designed to test the hypothesis that esmolol and diltiazem infusions blunt the sympathomimetic responses of pneumoperitoneum in comparison to control (normal saline) in patients undergoing laparoscopic transperitoneal simple nephrectomy. It also aims to compare the efficacy of these two drugs for the same purpose.
SUBJECTS AND METHODS
After approval from Institutional Ethical Committee and informed written consent from patients, 120 adult American Society of Anesthesiologists (ASA) physical status I and nonhypertensive ASA physical status II patients aged 20–60 years about to undergo laparoscopic transperitoneal nephrectomy for poorly functional kidney were included in the study.
Patients having hypertension, obesity, cardiovascular and pulmonary diseases, renal insufficiency were excluded from the study. Patient with known allergy to study drug or taking any beta blocker or calcium channel blocker were also not taken up. Before surgery, patients were divided randomly into three groups. A computer-generated random table was utilized for the purpose.
Group I (control group)
Received normal saline (10 ml) intravenously (i.v.) before induction of anesthesia, followed by continuous infusion 10–20 ml/h.
Group II (esmolol group)
Received i.v. esmolol 1 mg/kg diluted in 10 ml similarly, followed by continuous infusion of 10–20 ml/h (5–10 μg/kg/min).
Group III (diltiazem group)
Received i.v. diltiazem 0.2 mg/kg diluted in 10 ml before induction of anesthesia, followed by continuous infusion 10–20 ml/h (0.08–1.25 μg/kg/min).
On arrival to the operation room and initiation of standard monitoring of vitals all patients received injection midazolam 0.05 mg/kg i.v. The study drug was given as 10 ml bolus from an unlabeled syringe thus blinding the anesthesiologist delivering anesthesia to the patient. Anesthesia was induced with 2 mg/kg propofol and 1 mg/kg vecuronium was given i.v. to facilitate muscle relaxation. Laryngoscopy followed by endotracheal intubation with appropriate sized polyvinyl chloride cuffed tube was done. Infusion of the same unlabeled drug was started in a 50 ml syringe at the rate of 10–20 ml/h through infusion pump (Injectomat Agilia, Fresenius Kabi). Anesthesia was maintained with oxygen (40%) air mixture, isoflurane (to maintain end-tidal concentration of 1.0), and vecuronium bromide. Patients were positioned for the surgery; kidney position of the affected side was made. Pneumoperitoneum was created and intra-abdominal pressure was maintained between 10 and 12 mmHg. All patients were mechanically ventilated to maintain end-tidal CO2 between 36 and 39 mmHg. After completion of surgery and deflation of abdomen, the infusion of drugs was stopped. The patients were turned supine, neuromuscular blockade was reversed with injection neostigmine 0.05 mg/kg and injection glycopyrolate 0.01 mg/kg. After adequacy of spontaneous ventilation the trachea was extubated and patients were shifted to postoperative unit for further care.
Baseline hemodynamic parameters, namely, HR, systolic blood pressures (SBPs), diastolic blood pressures (DBP), and MAPs were recorded immediately after intubation and thereafter at 5 min interval till completion of surgery.
Hypotension defined by MAP <20% of baseline was dealt with bolus of 300 ml i.v. fluids and mephentermine 6 mg i.v. as and when required and the incidence noted. Hypertension as described by MAP >20% baseline was supposed to be dealt with infusion of nitroglycerine titrated accordingly. Bradycardia that is HR <50/min was supposed to be treated with 0.5 mg i.v. atropine.
Statistical analysis
The sample size as, calculated by power analysis, using a two-sample t-test, with a two-sided type I error of 5% (α = 0.05) and power at 80%, was 30 for each group. We enrolled 120 patients in total to account for dropouts that are conversion of surgery to open and protocol breach if any. All continuous data are presented as mean ± standard deviation. Comparison of hemodynamic variables is done by repeated measures of one-way ANOVA. Tukey (honestly significant difference) post hoc test is applied for intra- and inter-group comparison in cases where ANOVA is significant. Chi-square test is done for comparing categorical data. P < 0.05 is considered statistically significant. Statistical analysis is done using SPSS for windows version 16.0 (Chicago, SPSS Inc. 7).
RESULTS
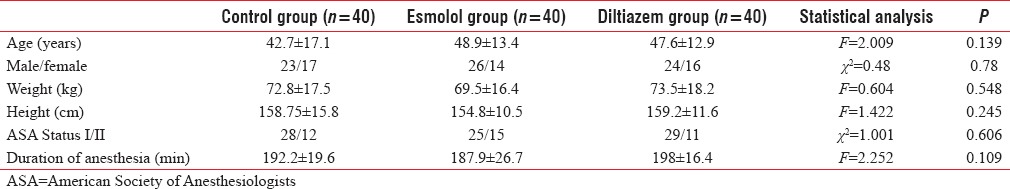
A total of 120 patients were enrolled for the study and randomly divided into three groups. There was no dropouts that is none of the surgeries had to be converted to open procedure. Data from all 120 patients were analyzed. There was no significant difference between the three groups in respect to age, male and female ratio, weight and height, physical status of patients, and duration of surgery [Table 1]. The average infusion rates of esmolol and diltiazem were 7.25 ± 1.33 μg/kg/min and 1.14 ± 0.77 μg/kg/min, respectively.
Table 1.
Patient characteristics and duration of anesthesia
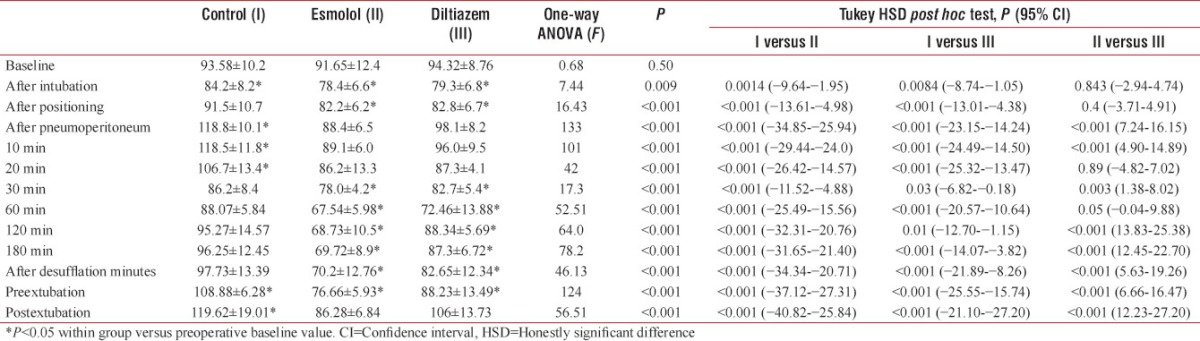
The increase in HR [Table 2] as compared to baseline in response to pneumoperitoneum was significantly higher in control as compared to both esmolol and diltiazem group (P < 0.001) and it remained high till 20 min of creation of pneumoperitoneum after which it settled to be similar to baseline rising again at extubation. The HR as compared to baseline remained stable in both esmolol and diltiazem group during and after creation of pneumoperitoneum. It was observed to be statistically lower than baseline at several points in both the study drugs. On intergroup comparison, the HR was significantly lower in esmolol and diltiazem group as compared to control right after induction but the higher attenuating effect of esmolol in comparison to diltiazem was seen significantly after the establishment of pneumoperitoneum. Thereafter, HR remained significantly lower in esmolol group than diltiazem and control throughout the duration of anesthesia (P < 0.001).
Table 2.
Analysis of heart rate
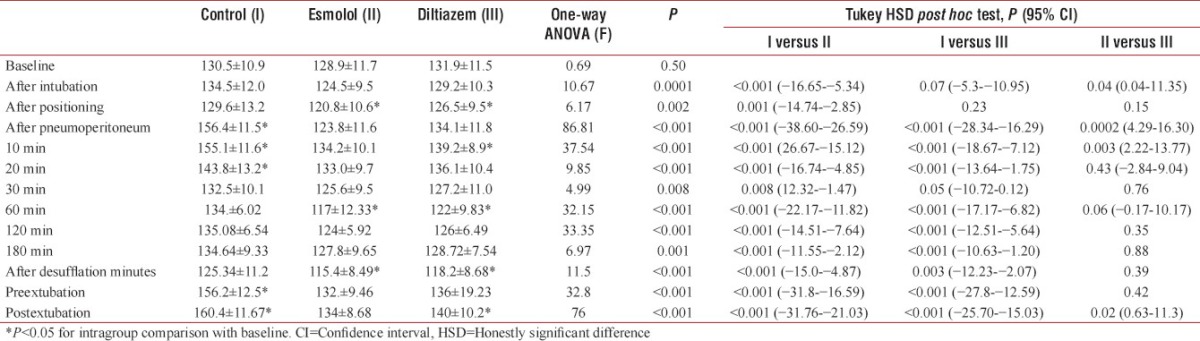
The changes observed in SBP at different time intervals between control and study groups are [Table 3]: The SBP was statistically and clinically significantly higher in the study group as compared to baseline on intragroup comparison at creation of pneumoperitoneum and then settled in next 20 min to rise again before extubation. It was statistically lower in esmolol group as compared to baseline and higher at some time points in diltiazem group, but these changes were not clinically significant. In comparison to control group attenuation of SBP was significantly greater in both esmolol and diltiazem group (P < 0.001) at intubation, creation of pneumoperitoneum and throughout the surgery. Esmolol group, however, showed a significantly better attenuation of SBPs compared to diltiazem group, P < 0.001 at laryngoscopy, pneumoperitoneum, and extubation. Rest of the period of surgery did not show any significant difference between SBPs in both groups receiving drugs.
Table 3.
Analysis of systolic blood pressure
The DBP [Table 4] remained similar in all the groups till after intubation. However, at the time of positioning, creation of pneumoperitoneum and thereafter the diastolic pressures remained significantly lower (P < 0.01) in esmolol group as compared to control. The diltiazem group also was seen to have significantly lower DBPs than control at creation of pneumoperitoneum and occasionally thereafter. By the time of extubation, however, the diastolic pressures were similar with control group. The esmolol group was seen to have significantly lower DBPs as compared to diltiazem at pneumoperitoneum creation, desufflation and the response continued till after extubation. The MAP [Figure 1] mimicked the DBPs trend with significantly lower values in esmolol group in comparison to control from positioning of patient till extubation of trachea. Diltiazem group had lower MAP than control at pneumoperitoneum creation, and at extubation (P < 0.05). A comparison between esmolol and diltiazem showed significiantly greater hemodynamic attenuation in esmolol group during highly stressful conditions such as pneumoperitoneum creation and extubation. Rest of the duration of surgery also showed lower hemodynamic values in esmolol group as compared to diltiazem. On intragroup comparison with baseline values both DBPs and MAPs were found to be significantly raised in control group at creation of pneumoperitoneum. The values settled after 20 min of pneumoperitoneum creation but rose again by the end of surgery and at extubation. The blood pressure values, however, remained fairly maintained in both esmolol and diltiazem groups when compared to baseline. There were statistically lower and higher values than baseline as seen in Tables 2 and 4 at different time points of surgery but they were not clinically relevant.
Table 4.
Analysis of diastolic blood pressure
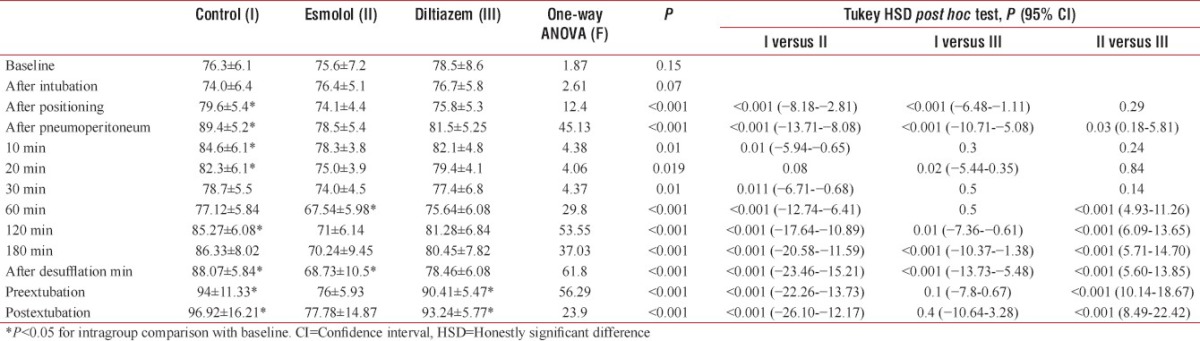
Figure 1.
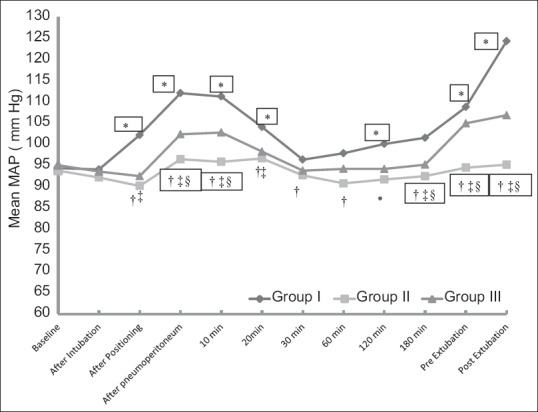
Trend of mean arterial pressure. *P < 0.05 for intragroup comparison with baseline. †P < 0.05 for intergroup comparison between I and II. ‡P < 0.05 for intergroup comparison between I and III. §P < 0.05 for intergroup comparison between II and III
Bradycardia with hypotension requiring atropine bolus was seen in one case in esmolol group (2.5%). Two patients in control group (5%) required nitroglycerine infusion for control of hypertension on pneumoperitoneum creation. The drug however was tapered off over the next 30 min in both the cases. No other complications were noted.
DISCUSSION
The present prospective double-blinded randomized control study conducted in patients undergoing laparoscopic nephrectomy observed that their hemodynamic parameters at creation of pneumoperitoneum increased significantly from baseline when no drugs were used to control the same. The changes however were observed only for initial 20 min on insufflations of gas in the abdomen, after which an adaptation was seen to occur. The initial rise in vitals followed by adaptation to pneumoperitoneum seen in patients undergoing laparoscopic nephrectomies has previously been hinted by Conacher et al.[11] Although the rise in hemodynamic is only for the initial period in operation it may be deleterious in patients with previous cardiac ailments, elderly and hypertensive patients. The parameters of patients in the esmolol and diltiazem group remained fairly comparable to baseline especially during stressful times such as initiation of abdominal insufflations and pre- and post-extubation. The blood pressures dipped significantly lower than baseline at certain times in patients receiving esmolol infusions but the mean pressure were never low enough to be clinically significant.
In lack of data form laparoscopic nephrectomy surgeries, we had to rely on data available on laparoscopic cholecytectomy. Joris et al.[12] found an increase of 35% in MAP, an increase of 65% in systemic vascular resistance, 90% increase in pulmonary vascular resistance, and cardiac output was seen to decrease by 20% in patients undergoing laparoscopic cholecytectomy after carbon dioxide insufflations at intraabdominal pressures of 15 mmHg. Various pharmacologic interventions such as nitroglycerine,[13] magnesium sulfate,[4] clonidine,[5,8] dexmedetomidine,[3,6,7] and propofol[3] infusions have been used with varying success to attenuate hemodynamic disturbances created by pneumoperitoneum. Esmolol hydrochloride: an ultra-short acting beta-adrenergic receptor blocking agent has also been used effectively for the same purpose.[6] It decreases sympathetic outflow, thereby causing a fall in blood pressures and HR. It also causes a fall in Noradrenaline level. Ibrahim et al.[8] had used esmolol in dose of 1.5 mg/kg and then continued with infusion of 10 μg/kg/min to effectively attenuate all hemodynamic responses to creation and maintenance of pneumoperitoneum. Srivastava et al.[6] had used 1 mg/kg of esmolol as bolus followed by infusion at rate of 0.5 mg/kg/h that comes up to an infusion of 8.33 μg/kg/min. They found this dose inadequate to maintain both HR and blood pressures comparable to baseline on creation and maintenance of pneumoperitoneum however the vitals remained in a range lower than that in saline control group. Our study used the same bolus as Srivastava et al. and an average infusion rate of 7.5 ± 5.3 μg/kg/min was seen to effectively maintain vitals on gas insufflations in abdomen and henceforth. This effectiveness of a lower dose of esmolol may be attributed to the fact that both the above studies were done in laparoscopic cholecystectomy whereas our surgery was conducted in patients undergoing laparoscopic nephrectomy.
Diltiazem, a calcium channel blocker, was the second drug used in the present study to curb sympathetic response to pneumoperitoneum. Diltiazem in usual clinical doses is known to decrease total peripheral resistance producing a consistent fall in blood pressure. It has modest direct negative inotropic action.[9] Intravenous diltiazem has been used previously to curb sympathetic stimulation on laryngoscopy, intubation, and extubation without exhibiting any side effects.[9,10,14] It has also been used to produce hypotension in patients undergoing total hip arthroplasty.[15] The drug however has never been used to attenuate response to pneumoperitoneum in laparoscopic surgeries. For curbing hemodynamic responses of intubation or extubation the dose used was 0.2 mg/kg given as a single bolus dose 2–3 min before the stimulus.[9,10,14] We used the same dose as bolus before induction of anesthesia in our patients. Since we were studying the effect of diltiazem on hemodynamics throughout the surgery so an infusion of diltiazem was required. Diltiazem has been used safely at rate of 0.1 μg/kg/min in patients undergoing off-pump coronary artery bypass surgery.[16] Hence, the infusion range decided in our study was 0.08–1.25 μg/kg/min and average infusion turned out to be at rate of 1.14 ± 0.77 μg/kg/min. In our study, diltiazem infusion was seen to curb hemodynamic responses to pneumoperitoneum effectively as compared to saline but was not as effective as esmolol in maintaining vitals at stimulating time points in surgery such as insufflations and extubation. Since there are no previous data available on the use of diltiazem for laparoscopic surgeries, a comparison of effects of this drug in our study with other studies is not possible. This is also one of the strengths of this study that the use of diltiazem infusion for curbing sympathetic response to insufflations of gas in abdomen is shown for the first time. Other strengths of the study are that attenuation of hemodynamic responses to creation of pneumoperitoneum in laparoscopic nephrectomies has been studied for the first time. Furthermore, the effects of two sympatholytic drugs esmolol and diltiazem have been compared directly for the first time.
The limitations of this study, however, are that only the hemodynamic parameters were recorded and the study period was intraoperative. The effect of drugs on the requirement of fentanyl or other anesthetics was not accessed and no follow-up of patients in postoperative period for prolonged effect of drugs was done. Nevertheless, the study does prove that intravenous infusion of diltiazem can be added to the list of drugs used to achieve hemodynamic stability in laparoscopic surgeries.
Maintaining of renal perfusion pressure of remaining single kidney is necessary for patients undergoing nephrectomies.[11] This renal perfusion pressure in turn is directly dependent on MAP and therefore maintaining MAP is important for patients undergoing nephrectomies. A balanced attenuation of blood pressures by diltiazem infusion may be of benefit over esmolol, but further studies measuring postoperative renal functions are required to comment anything definite in this regard.
The present study concludes that similar to laparoscopic cholecystectomy the vital parameters of patients undergoing laparoscopic nephrectomies also rise significantly in early intraoperative period synchronizing with time of insufflations of gas in abdomen. Both diltiazem and esmolol infusions can be used effectively to curb this sympathetic response.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Öztürk T. Shamsa A, editor. Risks associated with laparoscopic surgery. Advanced Laparoscopy. InTech. 2011. [Last accessed on 2017 Nov 08]. Available from: http://www.intechopen.com/books/advancedlaparoscopy/risks-associatedwith-laparoscopic-surgery .
- 2.Midgley S, Tolley DA. Anaesthesia for Laparoscopic Surgery in Urology. Eur Urol Suppl. 2006;4:241–5. [Google Scholar]
- 3.Bhutia MP, Rai A. Attenuation of haemodynamic parameters in response to pneumoperitoneum during laparoscopic cholecystectomy: A Randomized controlled trial comparing infusions of propofol and dexmedetomidine. J Clin Diagn Res. 2017;11:UC01–4. doi: 10.7860/JCDR/2017/26239.9810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dar SA, Gupta DD, Deopujari RC, Gomes P. Effect of magnesium sulphate on attenuation of hemodynamic stress responses during laparoscopic abdominal surgeries. J Anesth Clin Res. 2015;6:12. [Google Scholar]
- 5.Tripathi DC, Shah KS, Dubey SR, Doshi SM, Raval PV. Hemodynamic stress response during laparoscopic cholecystectomy: Effect of two different doses of intravenous clonidine premedication. J Anaesthesiol Clin Pharmacol. 2011;27:475–80. doi: 10.4103/0970-9185.86586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Srivastava VK, Nagle V, Agrawal S, Kumar D, Verma A, Kedia S, et al. Comparative evaluation of dexmedetomidine and esmolol on hemodynamic responses during laparoscopic cholecystectomy. J Clin Diagn Res. 2015;9:UC01–5. doi: 10.7860/JCDR/2015/11607.5674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ghodki PS, Thombre SK, Sardesai SP, Harnagle KD. Dexmedetomidine as an anesthetic adjuvant in laparoscopic surgery: An observational study using entropy monitoring. J Anaesthesiol Clin Pharmacol. 2012;28:334–8. doi: 10.4103/0970-9185.98329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ibrahim AN, Kamal MM, Lotfy A. Comparative study of clonidine versus esmolol on hemodynamic responses during laparoscopic cholecystectomy. Egyp J Anaesth. 2016;32:37–44. [Google Scholar]
- 9.Mondal M, Kumar MD, Sapui S. Evaluation of efficacy of intravenous diltiazem, lignocaine and combination of both in attenuating the cardiovascular responses to laryngoscopy and endotracheal intubation in normotensive patients. Sch J Appl Med Sci. 2017;5:1719–22. [Google Scholar]
- 10.Thanvi A, Tak ML, Naithani U. Comparison of diltiazem and lignocaine in attenuating hemodynamic responses during extubation in patients undergoing laparoscopic cholecystectomy. Int J Health Sci Res. 2016;6:82–9. [Google Scholar]
- 11.Conacher ID, Soomro NA, Rix D. Anaesthesia for laparoscopic urological surgery. Br J Anaesth. 2004;93:859–64. doi: 10.1093/bja/aeh274. [DOI] [PubMed] [Google Scholar]
- 12.Joris JL, Noirot DP, Legrand MJ, Jacquet NJ, Lamy ML. Hemodynamic changes during laparoscopic cholecystectomy. Anesth Analg. 1993;76:1067–71. doi: 10.1213/00000539-199305000-00027. [DOI] [PubMed] [Google Scholar]
- 13.Feig BW, Berger DH, Dougherty TB, Dupuis JF, Hsi B, Hickey RC, et al. Pharmacologic intervention can reestablish baseline hemodynamic parameters during laparoscopy. Surgery. 1994;116:733–9. [PubMed] [Google Scholar]
- 14.Mohan K, Rupa M. Attenuation of cardiovascular responses to laryngoscopy and intubation by diltiazem and lignocaine: A comparative study. Int J Med Res Health Sci. 2013;2:557–63. [Google Scholar]
- 15.Bernard JM, Pinaud M, Carteau S, Hubert C, Souron R. Hypotensive actions of diltiazem and nitroprusside compared during fentanyl anaesthesia for total hip arthroplasty. Can Anaesth Soc J. 1986;33:308–14. doi: 10.1007/BF03010742. [DOI] [PubMed] [Google Scholar]
- 16.Hegde A, Amaria T, Mandke A, Mandke NV. Comparative study of perioperative infusion of diltiazem and nicorandil on myocardial protection during OPCAB surgery. Ann Card Anaesth. 2005;8:49–54. [PubMed] [Google Scholar]


