Abstract
Importance
Patients treated outside of their Medicare Shared Savings Program (MSSP) accountable care organization (ACO) likely benefit less from the ACO’s integration of care. Consequently, the MSSP’s open-network design may preclude ACOs from improving value in care.
Objectives
Quantify out-of-ACO care in a single urban ACO and examine associations between patient-level predictors and out-of-ACO expenditures.
Research Design
Secondary data analysis using Centers for Medicare and Medicaid ACO Program Claim and Claim Line Feed dataset (dates of service January 1, 2013–December 31, 2013). Two-part modeling was used to examine associations between patient-level predictors and likelihood and level of out-of-ACO expenditures.
Subjects
Patients were included if they were prospectively assigned to the MSSP in 2013. Patients were excluded if they declined to share data with the ACO, were not retrospectively confirmed to be in the ACO, or had missing data on covariates. Analytic sample included 11,922 patients.
Measures
Total out-of-ACO expenditures and out-of-ACO expenditures by place of service.
Results
Of total expenditures, 32.9% were paid to out-of-ACO providers, and 89.8% of beneficiaries had out-of-ACO expenditures. The presence of almost all medical comorbidities increased out-of-ACO expenditures ($800–$3000 per comorbidity) across the study population. Racial/ethnic minority groups spent between $1076 and $1422 less outside of the ACO than white patients, which was driven by less out-of-ACO outpatient office expenditures ($417–$517 less for each racial/ethnic minority group).
Conclusions
Out-of-ACO expenditures represented a significant portion of expenditures for the study population. Medically complex patients spent more outside of the ACO and represent an important population to study further.
Keywords: Accountable care, comorbidities, expenditures, medicare, ACO leakage, out-of-network care
The Accountable Care Organization (ACO) is a health care delivery innovation developed to improve value in health care. Conceptualized as a hybrid between traditional fee-for-service (FFS) reimbursement and managed care, ACOs preserve patient choice by maintaining an open network of providers, while incentivizing providers to manage quality and cost of care for a population of patients by tying reimbursement to performance. In practice, there is significant variation in the ACO designs proposed by both the Centers for Medicare and Medicaid Services (CMS) and commercial payers; ACOs vary with regard to reimbursement model, network design, services provided, and number and type of providers, facilities, and patients included in them.1
As part of the Affordable Care Act, CMS developed the Medicare Shared Savings Program (MSSP). The MSSP encourages the formation of Medicare ACOs as a mechanism for improving the value of care provided to Medicare FFS beneficiaries. Under this particular ACO design, CMS reimburses ACO providers on a FFS basis and maintains an open network of providers for patients, while encouraging reduction in expenditures and improved quality by allowing ACOs to earn back a portion of any savings they accrue at the end of the year.2 MSSP ACOs may include providers, hospitals, federally qualified health centers, rural health clinics, and critical access hospitals at the ACO’s discretion.
The MSSP emphasizes care coordination, population health management, and provider accountability as the keys to improving value in care.2 However, there is concern that the MSSP’s open-network design may require ACOs to develop and implement strategies to encourage patients to receive care from ACO providers as appropriate to derive the maximal benefit of care coordination.3,4 As patients treated outside of the ACO presumably benefit less from the ACO’s integration of providers, shared medical records, and reductions in waste and duplication, it may be challenging for ACOs to improve care and reduce costs for patients receiving high levels of out-of-ACO care. For example, to benefit financially, an ACO may potentially need to achieve twice the savings within its own network, if its patients are receiving half of their care outside of the ACO. This is of particular concern as many patients with the most to gain from care coordination efforts in terms of expenditure reduction and improved health (eg, patients with complex medical problems and social situations) have historically received the most fragmented care.5–7
Given the variation in ACO design and the flexibility in ACO network creation, strategic decisions around which facilities, providers, and patients to include in an ACO may significantly impact the performance of the ACO. Strategic considerations include the inclusion of hospital-based and/or community-based providers, postacute care facilities and providers, specialist providers, higher-performing providers with regard to cost and quality, etc. ACOs must also consider the services that will be provided within the ACO and the patients that will be included. These decisions will impact the degree to which ACO providers will encounter and be able to effectively manage care and costs for ACO patients.
How out-of-ACO care impacts the ACO’s ability to manage cost and quality may inform future innovations in CMS and commercial ACO models. In addition, for as long as open networks remain a key feature of the ACO, ACOs will likely need to develop approaches to manage out-of-ACO care through network design, provider-level incentives, patient assignment and attribution methodologies, and patient and provider engagement strategies. In developing these strategies, it is necessary to first understand the prevalence and predictors of out-of-ACO care.
To inform future ACO policy and management strategies, the objectives of this study are (1) to quantify out-of-ACO care in a single urban ACO during its first year of participation in the MSSP and (2) to examine associations between patient-level predictors and likelihood and level of out-of-ACO expenditures.
METHODS
Study Design and Study Population
The UCLA MSSP ACO is composed of 3 acute care hospitals with ~800 inpatient beds and over 100 ambulatory care sites. The ACO includes ~325 primary care physicians and ~1500 specialist physicians. UCLA participated in track 1 of the MSSP, which allowed the ACO the opportunity to earn shared savings without assuming downside risk.2
We conducted a retrospective secondary data analysis using the CMS ACO Program Claim and Claim Line Feed (CCLF) dataset, which includes services provided under Medicare Parts A, B, and D for patients assigned to the UCLA MSSP in 2013.
The 2013 MSSP regulations specify that CMS uses an initial prospective member assignment process followed by a confirmatory retrospective member assignment process to identify patients in a given MSSP ACO. As such, patients were included in the study if they were prospectively assigned to the UCLA MSSP at the beginning of 2013, agreed to share data with the ACO, and were retrospectively confirmed to be in the ACO at the end of 2013. Patients were assigned to the ACO as outlined in the MSSP Final Rule.2 Specifically, patients were prospectively assigned to the ACO for 2013 if they met assignment criteria based upon claims with dates of service October 1, 2011–September 30, 2012 processed as of December 07, 2012. Patients were retrospectively assigned to the ACO if they met assignment criteria based upon claims with dates of service January 1, 2013–December 31, 2013 processed as of March 28, 2014.
In total, 19,179 beneficiaries were prospectively assigned to the ACO, and 17,591 (91.7%) agreed to share data with the ACO. Of those, 12,480 (70.9%) were retrospectively confirmed to be in the ACO and included in the study population. Patients with missing data (N = 558) were excluded from the analysis, so the final analytic sample included 11,922 patients (Fig. 1). The sample was stratified according to Reason for Medicare Eligibility into 2 sub-samples: age-eligible and non–age-eligible (ESRD-eligible and disability-eligible) beneficiaries.
FIGURE 1.
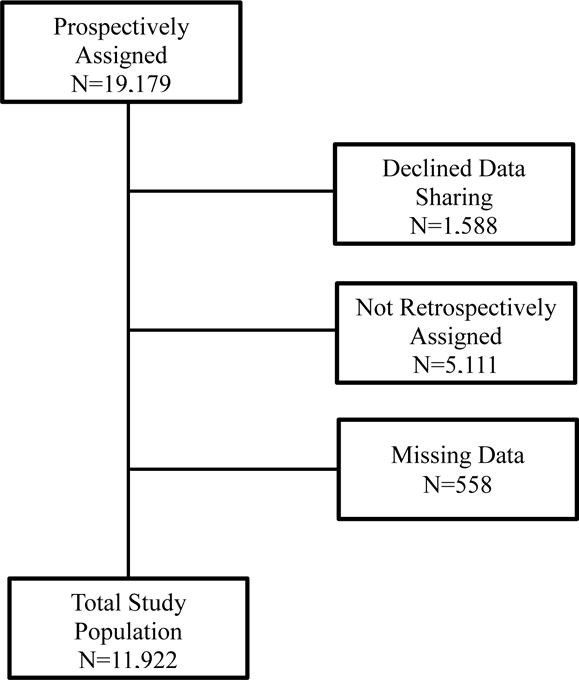
Flow Chart for Patients Meeting Inclusion and Exclusion Criteria
Main Outcome
To quantify out-of-ACO care, total overall expenditures and total out-of-ACO expenditures were calculated for each patient using Medicare paid amounts. Medicare Parts A, B, and D services delivered inside and outside of the ACO in CY 2013 were included. Expenditures for services with start and through dates in 2013 were included in their entirety. Expenditures for services that were partially provided in 2013 (eg, hospitalizations beginning in 2012 and ending in 2013) were prorated. In-ACO services were defined as services attributed to a billing provider with an NPI number or a facility with a tax-identification number registered with the UCLA MSSP in 2013. All other services were considered to be out-of-ACO.
Total out-of-ACO expenditures were calculated for all services combined as well as separately for services provided in various places of service, including inpatient setting, outpatient setting, long-term care facility, dialysis center, ambulatory surgery center, durable medical equipment, and prescription drugs. Total expenditures were calculated using Part A, B, and D paid claims. Inpatient, outpatient, long-term care, dialysis, and ambulatory surgery expenditures were calculated using Part A and B paid claims. Prescription drug expenditures were calculated using Part D paid claims. For further specificity, outpatient expenditures were further divided into outpatient office, emergency department, and outpatient other expenditure categories using only Part B paid claims.
Covariates
Predictor variables were selected based on their relevance and inclusion in the CMS ACO Program CCLF dataset. Covariates, as described in Table 1, included race/ethnicity (white, black, Latino, Asian, and other), age group (under 65, 65–74, 75–84, and 85 y or older), sex, individual medical comorbidities (hypertension, hyperlipidemia, coronary artery disease, mental health disease, dementia, osteoarthritis, rheumatoid arthritis, nonskin cancer, COPD, congestive heart failure, atrial fibrillation, ESRD, stroke, schizophrenia, and thyroid disorder), median income in patient’s residential zip code (based on 2010 US Census data) by quintile, travel distance from patient’s residential zip code to the ACO main campus (0–9, 10–19, 20–29, and 30+ miles), dual Medicaid-Medicare eligibility status, and employer-based supplemental insurance status.
Table 1.
Study MSSP Beneficiary Characteristics (N= 11922)
| Patient-Level Predictor | N | Percent |
|---|---|---|
| Race/Ethnicity (0.6% missing) | ||
| White | 8728 | 73.2% |
| Black | 1174 | 9.8% |
| Latino | 464 | 3.9% |
| Asian | 763 | 6.4% |
| Other | 793 | 6.7% |
| Age in years; (0.0% missing) | ||
| <65 | 1328 | 11.1% |
| 65-74 | 4545 | 38.1% |
| 75-84 | 3710 | 31.1% |
| 85+ | 2339 | 19.6% |
| Male Sex; N(%); (0.0% missing) | 4811 | 40.4% |
| Number of Medical Comorbidities; (0.0% missing) | ||
| 0 | 641 | 5.4% |
| 1 | 1725 | 14.5% |
| 2 | 2132 | 17.9% |
| 3 | 2127 | 17.8% |
| 4 | 1669 | 14.0% |
| 5+ | 3628 | 30.4% |
| Income in dollars; (3.7% missing) | ||
| Quintile 1 | 2585 | 21.7% |
| Quintile 2 | 2232 | 18.7% |
| Quintile 3 | 2416 | 20.3% |
| Quintile 4 | 2932 | 24.6% |
| Quintile 5 | 1757 | 14.7% |
| Distance in miles from residence to ACO; (0.3% missing) | ||
| 0-9 miles | 6632 | 55.6% |
| 10-19 miles | 3103 | 26.0% |
| 20-29 miles | 825 | 6.9% |
| 30+ miles | 1362 | 11.4% |
| Reason for Medicare Eligibility; (0.3% missing) | ||
| Aged | 10321 | 86.6% |
| ESRD | 134 | 1.1% |
| Disabled | 1467 | 12.3% |
| Medicare-Medicaid Dual-Eligible; (0.0% missing) | 2367 | 19.9% |
| Supplemental Commercial Insurance; (0.0% missing) | 320 | 2.7% |
Statistical Analyses
As our expenditure outcomes were generally limited-dependent variables with relatively large numbers of zero values (especially for expenditures by place of service) and skewed conditional distributions, we followed the Health Insurance Experiment methodology by using 2-part regression models to estimate patient-level predictors of out-of-ACO care.8 In the first part of the model, we identified patient-level predictors for having any out-of-ACO expenditures using a logit model of any out-of-ACO expenditures estimated using the full sample. In the second (conditional) part of the model, we identified predictors of the level of out-of-ACO expenditures among those that received any out-of-ACO care. This was done using a gamma model of expenditures estimated using the conditional sub-sample of patients with some out-of-ACO expenditures. Finally, estimates from both parts of the model were combined (by multiplying the predicted marginal probability of any out-of-ACO expenditures by the predicted level of out-of-ACO expenditures if any out-of-ACO care was used) to identify unconditional patient-level predictors of the level of out-of-ACO expenditures among the entire sample (out-of-ACO care users and nonusers).
This methodology was used to calculate 3 estimates for each individual. The estimates represent the mean differences between predictor variable categories in: (1) the predicted probability of having any out-of-ACO expenditures, (2) the predicted number of dollars spent outside of the ACO, conditional on having any out-of-ACO expenditures, and (3) the predicted number of dollars spent outside of the ACO averaged across the entire sample. Because we were most interested in the effect of covariates on out-of-ACO care across the entire population (unconditional results), we present only the predicted number of dollars spent outside of the ACO averaged across the entire sample. These results are displayed in Tables 2 and 3, where the values for the reference group indicate the predicted means, and the values for the nonreference groups indicate the marginal effects (the adjusted differences between that group and the reference group). We also provide the bootstrapped, bias-corrected 95% confidence intervals for the marginal effects. The predicted probabilities and results of the conditional analyses are included in Appendices A (Supplemental Digital Content 1, http://links.lww.com/MLR/B183) and B (Supplemental Digital Content 2, http://links.lww.com/MLR/B184).
Table 2.
Out-of-ACO Expenditures across All Beneficiaries (Unconditional Results) by Place of Service.
| All Care Settings | Inpatient | Outpatient Office | Emergency Department | |
|---|---|---|---|---|
| Out-of-ACO dollars spent, over entire sample (unconditional) | Out-of-ACO dollars spent, over entire sample (unconditional) | Out-of-ACO dollars spent, over entire sample (unconditional) | Out-of-ACO dollars spent, over entire sample (unconditional) | |
| Race/ethnicity | ||||
| Caucasian (reference)* | 5483 | 5122 | 1285 | 643 |
| (5307, 5660) | (4958, 5286) | (1370, 1399) | (610, 677) | |
| African American** | −1422 | 301 | −517 | 22 |
| (−2047, −644) | (−1416, 2244) | (−640, −385) | (−68, 138) | |
| Asian | −1076 | 115 | −437 | −25 |
| (−1714, −307) | (−1816, 3028) | (−563, −315) | (−127, 96) | |
| Latino | −207 | −530 | −436 | −37 |
| (−1337, 1144) | (−2220, 1497) | (−613, −246) | (−146, 96) | |
| Other Race/Ethnicity | −1304 | −1060 | −417 | −58 |
| (−1962, −522) | (−2654, 1078) | (−555, −258) | (−165, 38) | |
| Age (years) | ||||
| 65-74 (reference) | 5665 | 7262 | 1273 | 633 |
| (5482, 5847) | (7016, 7508) | (1259, 1288) | (598, 667) | |
| < 65 | 48 | 4581 | 148 | −96 |
| (−2391, 3341) | (39, 14812) | (−149, 523) | (−327, 129) | |
| 75-84 | −793 | −2635 | 18 | 15 |
| (−1288, −307) | (−4103, −1093) | (−84, 128) | (−60, 90) | |
| 85+ | −822 | −4182 | −102 | 96 |
| (−1494, −279) | (−5881, 2626) | (−236, 47) | (19, 190) | |
| Sex | ||||
| Male (reference) | 5361 | 5771 | 1240 | 672 |
| (5090, 5432) | (5587, 5955) | (1226, 1254) | (637, 706) | |
| Female | −166 | −1101 | 31 | −34 |
| (−650, 247) | (−2208, −92) | (−61, 125) | (−98, 17) | |
| Income (tens of thousands) | ||||
| Quintile 1 (reference) ($1235-$5750) | 4905 | 5129 | 1086 | 618 |
| (4745, 5066) | (4963, 5295) | (1073, 1098) | (587, 650) | |
| Quintile 2 ($5751-$6832) | 115 | −93 | 136 | −49 |
| (−558, 890) | (−1544, 1590) | (−6, 263) | (−122, 30) | |
| Quintile 3 ($6833-$7658) | 182 | −401 | 201 | 48 |
| (−501, 853) | (−1858, 1134) | (60, 343) | (−37, 135) | |
| Quintile 4 ($7659-$11379) | 584 | 155 | 233 | 84 |
| (−86, 1253) | (−1366, 1680) | (101, 379) | (3, 175) | |
| Quintile 5 ($11380-$18227) | 643 | 173 | 390 | 52 |
| (−67, 1416) | (−1590, 1921) | (207, 584) | (−29, 154) | |
| Distance (miles) | ||||
| 0-9 (reference) | 4950 | 4267 | 1268 | 652 |
| (4798, 5111) | (4131, 4403) | (1254, 1282) | (618, 685) | |
| 10-19 | 408 | 1118 | 66 | −19 |
| (−132, 1018) | (−99, 2264) | (−61, 217) | (−87, 52) | |
| 20-29 | −18 | 1294 | −89 | −65 |
| (−770, 837) | (−595, 3230) | (−260, 82) | (−164, 45) | |
| 30+ | 1296 | 3799 | −57 | −12 |
| (490, 2166) | (1803, 6083) | (−198, 95) | (−100, 74) | |
| Medicare Enrollment | ||||
| Aged (reference) | 4598 | 5454 | 1240 | 478 |
| (4476, 4721) | (5276, 5633) | (1226, 1254) | (466, 490) | |
| ESRD | 20690 | 727 | 1380 | 5152 |
| (12847, 34413) | (−2654, 5283) | (494, 2619) | (2713, 8783) | |
| Disability | 2475 | −1934 | 168 | 338 |
| (−252, 6848) | (−4147, 401) | (−107, 465) | (97, 773) | |
| Dual-eligible | ||||
| No (reference) | 5562 | 5483 | 1303 | 624 |
| (5370, 5753) | (5300, 5665) | (1288, 1318) | (593, 656) | |
| Yes | −1318 | −1261 | −163 | 46 |
| (−1839, −738) | (−2595, −60) | (−276, −44) | (−19, 118) | |
| Employer-based Insurance | ||||
| No (reference) | 5261 | 5237 | 1287 | 641 |
| (5093, 5430) | (5070, 5403) | (1272, 1301) | (608, 674) | |
| Yes | −2107 | −3365 | −498 | −23 |
| (−2856, −1017) | (−4482, −1906) | (−717, −182) | (−161, 121) | |
| Hypertension | ||||
| No (reference) | 4112 | 4133 | 1194 | 558 |
| (3986, 4238) | (3992, 4274) | (1180, 1207) | (530, 586) | |
| Yes | 1396 | 1138 | 115 | 95 |
| (990, 1808) | (−228, 2212) | (18, 218) | (31, 160) | |
| Hyperlipidemia | ||||
| No (reference) | 5011 | 4967 | 1194 | 670 |
| (4850, 5171) | (4806, 5129) | (1181, 1208) | (636, 705) | |
| Yes | 294 | 200 | 148 | −44 |
| (−157, 712) | (−906, 1173) | (53, 247) | (−113, 9) | |
| Coronary Artery Disease | ||||
| No (reference) | 4505 | 4429 | 1219 | 599 |
| (4373, 4636 | (4292, 4565) | (1205, 1232) | (569, 628) | |
| Yes | 1955 | 1493 | 215 | 93 |
| (1360, 2586) | (415, 2507) | (100, 337) | (27, 166) | |
| Mental Health | ||||
| No (reference) | 4545 | 5012 | 1225 | 564 |
| (4408, 4676) | (4850, 5175) | (1212, 1239) | (536, 592) | |
| Yes | 2601 | 271 | 286 | 227 |
| (1902, 3244) | (−789, 1378) | (157, 430) | (169, 304) | |
| Dementia | ||||
| No (reference) | 4689 | 4712 | 1324 | 550 |
| (4553, 4825) | (4563, 4861) | (1309, 1339) | (523, 577) | |
| Yes | 3063 | 1965 | −449 | 415 |
| (2000, 4266) | (379, 3807) | (−568, −333) | (328, 536) | |
| Osteoarthritis | ||||
| No (reference) | 4210 | 4107 | 1134 | 605 |
| (4087, 4333) | (3976, 4237) | (1122, 1147) | (574, 636) | |
| Yes | 2376 | 2193 | 393 | 75 |
| (1888, 2845) | (1004, 3117) | (291, 484) | (21, 133) | |
| Rheumatoid Arthritis | ||||
| No (reference) | 5077 | 5148 | 1232 | 642 |
| (4915, 5239) | (4980, 5316) | (1219, 1246) | (609, 674) | |
| Yes | 2533 | −735 | 1010 | −29 |
| (1266, 3897) | (−2331, 1175) | (614, 1505) | (−133, 69) | |
| Cancer (non-skin) | ||||
| No (reference) | 4077 | 5011 | 968 | 607 |
| (3948, 4205) | (4847, 5176) | (958, 977) | (576, 639) | |
| Yes | 2583 | 187 | 721 | 76 |
| (2149, 3098) | (−747, 1193) | (619, 815) | (22, 133) | |
| COPD | ||||
| No (reference) | 4647 | 4462 | 1227 | 591 |
| (4505, 4788) | (4325, 4600) | (1214, 1241) | (560, 621) | |
| Yes | 2182 | 1909 | 234 | 165 |
| (1540, 2803) | (750, 2944) | (108, 375) | (101, 237) | |
| Congestive Health Failure | ||||
| No (reference) | 4723 | 4135 | 1291 | 578 |
| (4587, 4859) | (4020, 4250) | (1276, 1305) | (551, 606) | |
| Yes | 2000 | 3249 | −139 | 195 |
| (1183, 2999) | (1693, 4972) | (−381, 7) | (124, 268) | |
| Atrial Fibrillation | ||||
| No (reference) | 4766 | 4750 | 1226 | 599 |
| (4621, 4911) | (4597, 4902) | (1212, 1239) | (569, 630) | |
| Yes | 1231 | 803 | 197 | 101 |
| (717, 1768) | (−186, 1914) | (66, 319) | (44, 154) | |
| ESRD | ||||
| No (reference) | 4832 | 5125 | 1258 | 612 |
| (4692, 4972) | (4957, 5293) | (1243, 1272) | (582, 641) | |
| Yes | 1419 | −49 | 110 | 72 |
| (667, 2124) | (−1237, 1125) | (−48, 292) | (4, 142) | |
| Stroke | ||||
| No (reference) | 4522 | 4120 | 1206 | 575 |
| (4397, 4647) | (4000, 4240) | (1194, 1219) | (547, 603) | |
| Yes | 2564 | 3085 | 378 | 199 |
| (1853, 3271) | (1749, 4691) | (228, 564) | (136, 279) | |
| Peripheral Vascular Disease | ||||
| No (reference) | 4766 | 4882 | 1226 | 613 |
| (4626, 4906) | (4727, 5037) | (1213, 1239) | (583, 644) | |
| Yes | 1925 | 752 | 336 | 89 |
| (1210, 2689) | (−374, 2073) | (143, 596) | (23, 164) | |
| Diabetes | ||||
| No (reference) | 4821 | 4934 | 1223 | 621 |
| (4676, 4966) | (4776, 5093) | (1210, 1237) | (590, 651) | |
| Yes | 1170 | 457 | 211 | 47 |
| (643, 1744) | (−666, 1453) | (102, 331) | (−10, 107) | |
| Schizophrenia | ||||
| No (reference) | 5010 | 4863 | 1268 | 602 |
| (4855, 5165) | (4711, 5015) | (1253, 1282) | (572, 632) | |
| Yes | 2830 | 2907 | 131 | 418 |
| (1424, 4399 | (474, 5420) | (−117, 423) | (262, 632) | |
| Thyroid disorder | ||||
| No (reference) | 4956 | 4872 | 1234 | 617 |
| (4801, 5112) | (4714, 5030) | (1221, 1248) | (586, 648) | |
| Yes | 862 | 827 | 178 | 73 |
| (347, 1379) | (−271, 1962) | (51, 311) | (6, 151) |
Values for the reference group show the predicted probabilities and predicted means.
Values for the non-reference groups show the marginal effects (the adjusted differences between that group and the reference group).
Table 3.
Out-of-ACO Expenditures for Age-Eligible and Non-Age-Eligible Beneficiaries.
| Non-Age-Eligible Population | Age-Eligible Population | |
|---|---|---|
| Out-of-ACO dollars spent, over entire sample (unconditional results) | Out-of-ACO dollars spent, over entire sample (unconditional results) | |
| Race/ethnicity | ||
| Caucasian (reference)* | 8301 | 4899.685 |
| (7589, 9014) | (4769, 5031) | |
| African American** | −831 | −1365 |
| (−3014, 1120) | (−1987, −501) | |
| Asian | −2397 | −966 |
| (−5529, −19) | (−1576, −222) | |
| Latino | 226 | −193 |
| (−2148, 3030) | (−1637, 1643) | |
| Other Race/Ethnicity | 348 | −1216 |
| (−3516, 5293) | (−1788, −522) | |
| Sex | ||
| Male (reference) | 8303 | 4664 |
| (7592,9014) | (4534, 4794) | |
| Female | −423 | −49 |
| (−2493, 958) | (−467, 336) | |
| Income (tens of thousands) | ||
| Quintile 1 (reference) | 7141 | 4530 |
| (6511, 7772) | (4404, 4656) | |
| Quintile 2 | 1841 | −194 |
| (−451, 6534) | (−877, 446) | |
| Quintile 3 | 1055 | 41 |
| (−966, 4220) | (−724, 710) | |
| Quintile 4 | 1848 | 399 |
| (−89, 5441) | (−298, 1026) | |
| Quintile 5 | 3862 | 428 |
| (−387, 14421) | (−293, 1162) | |
| Distance (miles) | ||
| 0-9 (reference) | 6969 | 4489 |
| (6380, 7557) | (4364, 4614) | |
| 10-19 | 1647 | 285 |
| (−95, 5372) | (−238, 801) | |
| 20-29 | 13 | 101 |
| (−2087, 2582) | (−657, 995) | |
| 30+ | 3176 | 1196 |
| (972, 7994) | (419, 2067) | |
| Dual-eligible | ||
| No (reference) | 9775 | 4860 |
| (8922, 10627) | (4723, 4997) | |
| Yes | −2756 | −1061 |
| (−5788, −1017) | (−1566, −488) | |
| Employer-based Insurance | ||
| No (reference) | 8131 | 4733 |
| (7433, 8830) | (4603, 4863) | |
| Yes | −3011 | −1876 |
| (−6431, 29) | (−2565, −837) | |
| Hypertension | ||
| No (reference) | 4507 | 3992 |
| (4187, 4827) | (3885, 4098) | |
| Yes | 5230 | 860 |
| (3605, 7903) | (496, 1247) | |
| Hyperlipidemia | ||
| No (reference) | 9022 | 4364 |
| (8215, 9829) | (4247, 4482) | |
| Yes | −1666 | 487 |
| (−5099, 55) | (98, 859) | |
| Coronary Artery Disease | ||
| No (reference) | 7044 | 4114 |
| (6490, 7597) | (4012, 4216) | |
| Yes | 3416 | 1556 |
| (−32, 8278) | (1077, 2062) | |
| Mental Health | ||
| No (reference) | 6231 | 4188 |
| (5713, 6749) | (4088, 4289) | |
| Yes | 6124 | 2084 |
| (3771, 9455) | (1443, 2674) | |
| Dementia | ||
| No (reference) | 4187 | |
| (4087, 4287) | ||
| Yes | 2674 | |
| (1829, 3780) | ||
| Osteoarthritis | ||
| No (reference) | 7346 | 3731 |
| (6732, 7959) | (3639, 3823) | |
| Yes | 2263 | 2158 |
| (564, 4403) | (1739, 2582) | |
| Rheumatoid Arthritis | ||
| No (reference) | 7944 | 4571 |
| (7258,8630) | (4448,4695) | |
| Yes | 1389 | 2519 |
| (−1537, 5849) | (1343,4040) | |
| Cancer (non-skin) | ||
| No (reference) | 6856 | 3586 |
| (6294, 7417) | (3494, 3678) | |
| Yes | 3649 | 2329 |
| (1674, 7279) | (1901, 2751) | |
| COPD | ||
| No (reference) | 7322 | 4195 |
| (6697, 7947) | (4090, 4301) | |
| Yes | 2740 | 1912 |
| (465, 5961) | (1289, 2517) | |
| Congestive Health Failure | ||
| No (reference) | 7311 | 4237 |
| (6732, 7890) | (4137, 4337) | |
| Yes | 3234 | 1871 |
| (131, 7643) | (1017, 2850) | |
| Atrial Fibrillation | ||
| No (reference) | 7421 | 4293 |
| (6808, 8035) | (4183, 4403) | |
| Yes | 2121 | 1062 |
| (−79, 4905) | (549, 1562) | |
| ESRD | ||
| No (reference) | 5573 | 4379 |
| (5207, 5939) | (4268, 4490) | |
| Yes | 8511 | 1454 |
| (5009, 12697) | (751, 2147) | |
| Stroke | ||
| No (reference) | 6945 | 4082 |
| (6413,7477) | (3985, 4178) | |
| Yes | 5600 | 2219 |
| (2674, 9940) | (1589, 2928) | |
| Peripheral Vascular Disease | ||
| No (reference) | 7401 | 4289 |
| (6810, 7992) | (4182, 4397) | |
| Yes | 2874 | 1778 |
| (−159, 6846) | (1061, 2551) | |
| Diabetes | ||
| No (reference) | 6978 | 4406 |
| (6403, 7553) | (4289, 4523) | |
| Yes | 2536 | 970 |
| (514, 5430) | (463, 1458) | |
| Schizophrenia | ||
| No (reference) | 7317 | 4608 |
| (6687,7948) | (4485, 4731) | |
| Yes | 7896 | 1102 |
| (4137, 14183) | (−111, 2548) | |
| Thyroid disorder | ||
| No (reference) | 7899 | 4439 |
| (7220, 8579) | (4321, 4557) | |
| Yes | 579 | 876 |
| (−1340, 2540) | (410, 1400) |
Values for the reference group show the predicted probabilities and predicted means.
Values for the non-reference groups show the marginal effects (the adjusted differences between that group and the reference group).
This study was approved by the University of California-Los Angeles Institutional Review Board (IRB # 14-000482). Statistical analyses were done using STATA 13.
RESULTS
Descriptive statistics for the study population are shown in Table 1. The sample is predominantly white (73.2%) and female (59.6%). On average, beneficiaries in the study population are 74.6 (SD = 11.9) years of age, suffer from 3.6 (SD = 2.5) medical comorbidities, live in zip codes with a median annual income of $81,097 (SD = $32,340), and live 16.0 miles (SD = 31.3) from the ACO main campus. A significant portion of the population aged into the Medicare program (86.6%). A minority of beneficiaries is also eligible for Medicaid enrollment (19.9%) or additionally enrolled in an employer-based supplemental insurance plan (2.7%).
We quantified total and out-of-ACO expenditures across the population and by place of service, and these results are shown in Table 4. Mean total expenditures per beneficiary for the analytic sample was $14,481 (SD = $30,011). Across the population, 32.9% ($56,877,716) of total expenditures (Parts A, B, and D) were paid to providers outside of the ACO. Considering Part A and B expenditures, 25.9% ($16,731,305) of inpatient expenditures, 37.0% ($21,928,657) of outpatient expenditures, 35.1% ($9,400,648) of long-term care expenditures, 49.3% ($1,662,271) of dialysis expenditures, 92.4% (1,378,660) of ambulatory surgery expenditures, and 27.3% ($4,053,738) of durable medical equipment expenditures were paid to providers outside of the ACO. In addition, 35.6% ($4,675,391) of Part D prescription drug expenditures were attributed to out-of-ACO providers. Considering only Part B outpatient expenditures, 45.3% ($15,017,395) of outpatient office expenditures, 87.5% ($2,621,689) of emergency department expenditures, and all ($106,866) of outpatient other expenditures were paid to providers outside of the ACO. In total, 89.8% of beneficiaries had some out-of-ACO expenditures.
Table 4.
Total and Out-of-ACO Expenditures across Study Beneficiaries
| N | Mean Expenditures per Beneficiary | SD | Percent Out- of-ACO Expenditures | |
|---|---|---|---|---|
| Total Expenditures (Part A, B, D) | 11,922 | $ 14,481 | $ 30,011 | 32.9% |
| Inpatient (Part A & B) | 3,278 | $ 19,719 | $ 35,833 | 25.9% |
| Outpatient (Part A & B) | 11,916 | $ 4,967 | $ 9,834 | 37.0% |
| Outpatient Office (Part B only) | 11,906 | $ 2,786 | $ 5,872 | 45.3% |
| Emergency Department (Part B only) | 3,859 | $ 777 | $ 3,199 | 87.5% |
| Outpatient Other (Part B only) | 2,387 | $ 45 | $ 45 | 100.0% |
| Long-term Care (Part A & B) | 2,317 | $ 11,543 | $ 17,820 | 35.1% |
| Dialysis (Part A & B) | 319 | $ 10,567 | $ 15,352 | 49.3% |
| Ambulatory Surgery Center (Part A & B) | 1,332 | $ 1,120 | $ 1,459 | 92.4% |
| Other (Part A & B) | 3,239 | $ 1,252 | $ 6,253 | 27.3% |
| Prescription Drug (Part D) | 8,726 | $ 1,507 | $ 3,207 | 35.6% |
Table 2 compares predictors of out-of-ACO care for the entire study population across the 3 places of service we felt were most clinically meaningful: inpatient, outpatient office, and emergency department. In general, we found that our covariates were not significant predictors of out-of-ACO expenditures in long-term care facilities, hemodialysis centers, ambulatory surgery centers, durable medical equipment, or outpatient other settings due to the reduced analytic sample sizes, and these results are not displayed.
Across the entire study population, black, Asian, and Latino patients spent less outside of the ACO than whites. Compared with whites, who spent $5483 outside of the ACO, blacks spent $1422 less, Asians spent $1076 less, and patients of other race/ethnicity spent $1304 less outside of the ACO. These differences in out-of-ACO expenditures were largely driven by less out-of-ACO outpatient office expenditures.
With regard to age, patients aged 75–84 years spent $793 less and patients aged 85+ years spent $822 less than patients aged 65–74 years who spent $5665 outside of the ACO. These reductions in out-of-ACO expenditures for older patients were driven by inpatient expenditures. Across the entire study population, there was no difference in out-of-ACO expenditures according to sex; however, females spent $1101 less on inpatient out-of-ACO expenditures than men.
Across the entire study population, there was no difference in out-of-ACO expenditures according to income; however, higher income was associated with slightly higher outpatient office out-of-ACO expenditures. With regard to distance of the patient’s residence to the primary ACO facility, patients living 30+ miles from the ACO spent $1296 more outside of the ACO than those living 0–9 miles from the ACO who spent $4950 outside of the ACO. This was driven by $3799 in higher inpatient out-of-ACO expenditures for those living 30+ miles from the ACO.
With regard to reason for Medicare enrollment, patients with ESRD spent $20,690 more outside of the ACO than patients who aged into Medicare who spent $4598 outside of the ACO. This increase in expenditures was driven by emergency department expenditures ($5152) and outpatient office expenditures ($1380). Across the entire study population, dual-eligible patients spent $1318 less than non–dual-eligible patients who spent $5562 outside of the ACO. Dual-eligible patients spent $1261 less on inpatient out-of-ACO services and $163 less on outpatient office out-of-ACO services. Patients with employer-based supplemental insurance spent $2107 less outside of the ACO than those without it who spent $5261 outside of the ACO. This reduction in out-of-ACO expenditures was driven by a reduction of $3365 in inpatient out-of-ACO expenditures and $498 in outpatient office out-of-ACO expenditures.
Across the entire study population, all medical comorbidities, with the exception of hyperlipidemia, were associated with increased out-of-ACO expenditures ($862–$3063 per comorbidity). Increased out-of-ACO expenditures were driven by inpatient out-of-ACO expenditures for coronary artery disease, dementia, osteoarthritis, COPD, congestive heart failure, stroke, and schizophrenia. Increased out-of-ACO expenditures were driven by outpatient office out-of-ACO expenditures for hypertension, hyperlipidemia, mental health disorder, rheumatoid arthritis, nonskin cancer, atrial fibrillation, peripheral vascular disease, diabetes, and thyroid disorder. Increased out-of-ACO expenditures were driven by emergency department out-of-ACO expenditures for ESRD.
Table 3 compares predictors of out-of-ACO care for the age-eligible and non–age-eligible subsamples. With regard to race/ethnicity, patients of racial/ethnic minority groups in the age-eligible sample spent less outside of the ACO than white patients. White patients spent $4900 outside of the ACO. Black patients spent $1365 less, Asian patients spent $966 less, and patients of other race/ethnicity spent $1216 less than white patients outside of the ACO. In the non–age-eligible sample, only Asian patients spent $2397 less than white patients who spent $8301 outside of the ACO.
There was no significant difference in out-of-ACO expenditures between men and women or with regard to income. With regard to distance from the patient’s residence to primary ACO facility, patients living 30+ miles from the ACO spent $1196 more in the age-eligible subsample and $3176 more in the non–age-eligible subsample than those living 0–9 miles from the ACO. Dual-eligible patients spent $1061 less than non–dual-eligible patients in the age-eligible subsample and $2756 less in the non–age-eligible subsample. Patients with employer-based supplemental insurance spent $1876 less in the age-eligible sample. There was no difference in out-of-ACO spending with regard to supplemental insurance in the non–age-eligible sample, though the sample size was small.
With regard to medical comorbidities in the age-eligible subsample, all comorbidities, except schizophrenia, were associated with greater out-of-ACO expenditures. The marginal increase in expenditures for each comorbidity ranged from $487 for hyperlipidemia to $2519 for rheumatoid arthritis. In the non–age-eligible sample, several comorbidities were associated with greater out-of-ACO expenditures. Marginal increases in expenditures per comorbidity were markedly higher for the non–age-eligible subsample and ranged from $2263 for osteoarthritis to $8511 for ESRD.
DISCUSSION
Out-of-ACO expenditures represented a significant portion of total expenditures for the UCLA MSSP population in both the age-eligible and non–age-eligible subsamples and across place of service. Substantial overall rates of out-of-ACO care agree with findings reported in an earlier study.3 That over a third of dollars spent on the UCLA MSSP population were paid to providers outside of the ACO creates an important challenge for the ACO in increasing value and achieving shared savings. Specifically, for the UCLA MSSP (and likely other similar ACOs), earning shared savings requires that the ACO achieve a 2% reduction in total expenditures while only controlling two thirds of rendered services.
Beyond the sheer volume of services delivered outside of the ACO, it may be even more concerning that more medically complex patients received care outside of the ACO. In general, we found that out-of-ACO expenditures were driven by medical comorbidities. We also found that patients enrolled in Medicare due to ESRD had higher out-of-ACO expenditures. Patients with more medical comorbidities may be receiving care from more providers and in more care settings and have increased opportunity to receive care outside of the ACO. Previous studies demonstrate that sicker, more complex patients experience the most benefit from care coordination with regard to lower total cost of care and reduced inpatient and ED utilization.9–11 In addition, care coordination for the ESRD population has been shown to significantly improve outcomes and control costs in multiple ESRD demonstration projects.12 Higher levels of out-of-ACO care for these high-risk patients exacerbate the challenge in managing their care.
Interestingly, we found that patients from racial/ethnic minority groups spent less outside of the ACO than white patients. This was particularly true for age-eligible patients and for care provided in the outpatient office setting. One hypothesis for this is that lower rates of out-of-ACO care among minority groups suggest that they place greater trust in familiar providers.13
Despite evidence demonstrating significant out-of-ACO expenditures, identifying whether and how ACOs should reduce out-of-ACO care is not entirely straightforward, as the financial and quality incentives built into the MSSP are complex. On one hand, MSSP ACOs are incentivized to retain the care of patients within the ACO to increase reimbursement and to maximize care coordination efforts for its patients. On the other hand, given the potential for shared savings, ACOs may be also incentivized to refer patients outside of the ACO if they believe patients can receive lower-cost or higher-quality care at an outside facility. This point is particularly important for ACOs that operate near capacity. In addition, allowing patients the ability to seek the highest-quality care, wherever it can be provided, is an important political cornerstone of the MSSP model. As a result of these mixed incentives, a more nuanced understanding of exactly why patients receive care outside of the ACO is needed.
On the basis of these initial findings, it is not possible to describe the impact of out-of-ACO care on health outcomes or total health care expenditures. Future work to explore these associations will be important in understanding how necessary it is to devise strategies and policies to reduce out-of-ACO care.
The methods described in this study can be used as a starting point in identifying various causes of out-of-ACO care. However, it is important to remember that these analyses are from a single large urban ACO, and we do not have the needed data or design to compare the association of various ACO features with the amount of out-of-ACO care. Associations drawn from claims data may provide hypotheses that can be further explored with patients and providers through interviews or focus groups. For example, claims analysis may demonstrate an association between illness burden and out-of-ACO care. However, upon surveying patients and providers, it may be revealed that out-of-ACO is occurring because the ACO does not provide all necessary specialty services for certain medical conditions; alternatively, it may be revealed that out-of-ACO care is occurring because the ACO has poor parking/access to facilities for patients or because patients are unaware that they are enrolled in an ACO. The implications of each of these findings are different and whether and how to respond to leakage will differ as a result.
In conclusion, out-of-ACO care is a byproduct of the ACO’s open-network model and represents approximately a third of total health care expenditures for patients in the UCLA MSSP. Patients who receive the most care outside of the ACO represent groups that have historically received more fragmented care and may benefit most from care coordination. Future studies should examine how higher rates of out-of-ACO care affect total cost of care and health outcomes to determine to what degree the MSSP’s open-network structure impedes its ability to improve value in care.
Supplementary Material
Acknowledgments
C.M.M. received financial support from the University of California at Los Angeles (UCLA), Resource Centers for Minority Aging Research Center for Health Improvement of Minority Elderly under National Institutes of Health (NIH)/NIA Grant P30-AG021684, and from NIH/National Center for Advancing Translational Sciences UCLA Clinical and Translational Science Institute Grant UL1TR000124. C.M.M. holds the Barbara A. Levey and Gerald S. Levey Endowed Chair in Medicine, which partially supported her work.
Footnotes
An abstract related to this work was presented as a poster at the Society of General Internal Medicine Annual Meeting, April 22–25, 2013.
The authors declare no conflict of interest.
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Website, www.lww-medicalcare.com.
References
- 1.Shortell SM, Wu FM, Lewis VA, et al. A taxonomy of accountable care organizations for policy and practice. Health Serv Res. 2014;49:1883–1899. doi: 10.1111/1475-6773.12234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Medicare and Medicaid Services. Medicare Shared Savings Program final rule. Federal Register. 2011 Available at: http://www.commonwealthfund.org/~/media/Files/Publications/Other/2011/ZezzasummaryfinalruleMedicaresharedsavingsv2.pdf Accessed April 4, 2015.
- 3.McWilliams JM, Chernew ME, Dalton JB, et al. Outpatient care patterns and organizational accountability in Medicare. JAMA Intern Med. 2014;174:938–945. doi: 10.1001/jamainternmed.2014.1073. [DOI] [PubMed] [Google Scholar]
- 4.Sinaiko AD, Rosenthal MB. Patients’ role in accountable care organizations. N Engl J Med. 2010;363:2583–2585. doi: 10.1056/NEJMp1011927. [DOI] [PubMed] [Google Scholar]
- 5.McWilliams JM, Landon BE, Chernew ME. Changes in health care spending and quality for Medicare beneficiaries associated with a commercial ACO contract. JAMA. 2013;310:829–836. doi: 10.1001/jama.2013.276302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nissenson AR, Collins AJ, Dickmeyer J, et al. Evaluation of disease-state management of dialysis patients. Am J Kidney Dis. 2001;37:938–944. doi: 10.1016/s0272-6386(05)80009-5. [DOI] [PubMed] [Google Scholar]
- 7.Morrow R, Halbach JL, Hopkins C, et al. A family practice model of health care for homeless people: collaboration with family nurse practitioners. Fam Med. 1992;24:312–316. [PubMed] [Google Scholar]
- 8.Duan N, Manning WG, Morris CN, et al. A comparison of alternative models for the demand for medical care. J Bus Econ Stat. 1983;1:115–126. [Google Scholar]
- 9.Flottemesch TJ, Anderson LH, Solberg LI, et al. Patient-centered medical home cost reductions limited to complex patients. Am J Manag Care. 2012;18:677–686. [PubMed] [Google Scholar]
- 10.Higgins S, Chawla R, Colombo C, et al. Medical homes and cost and utilization among high-risk patients. Am J Manag Care. 2014;20:e61–e71. [PubMed] [Google Scholar]
- 11.Tuso P, Watson HL, Garofalo-Wright L, et al. Complex case conferences associated with reduced hospital admissions for high-risk patients with multiple comorbidities. Perm J. 2014;18:38–42. doi: 10.7812/TPP/13-062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen RA, Scott S, Mattern WD, et al. The case for disease management in chronic kidney disease. Dis Manag. 2006;9:86–92. doi: 10.1089/dis.2006.9.86. [DOI] [PubMed] [Google Scholar]
- 13.Kahn KL. Health care for black and poor hospitalized Medicare patients. JAMA. 1994;271:1169. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


