1. Introduction
Unicompartmental knee arthroplasty (UKA)is an increasingly popular surgical treatment for isolated medial compartment osteoarthritis (OA) of the knee [1]. Many distinct advantages of UKA compared to total knee arthroplasty (TKA) have been reported including lower perioperative morbidity [2,3], lower risk for infection [4], less blood loss [5], accelerated recovery [6,7] and improved range of motion [2,7]. A recent cost-effectiveness study demonstrated that medial UKA is preferable to TKA with decreased lifetime costs and improved quality of life in patients over 65 years of age [8].
In spite of these advantages, UKA may be an underutilized procedure [9,10]. This may be partially explained by concerns about short and long-term survivorship of UKA compared to TKA. Registry data demonstrated that ten-year survivorship of UKA (85 – 90%) is lower than TKA survivorship (95%) [11 – 13]. Recent literature also showed, however, that UKA performed in high-volume centers has a higher survivorship compared to low-volume UKA centers [14,15]. Several authors have shown that good results with UKA can be achieved by reporting a ten-year survivorship over 95% in high-volume UKA centers [16 – 19].
Recently, robotic-assisted surgery has been shown to reliably improve lower leg alignment [20–24], soft tissue balancing [25] and implant positioning [26–29] when compared to conventional UKA surgery. Since failure of UKA is commonly associated with technical errors of malalignment, instability and implant malpositioning [30–35], one would expect better results with robotic-assisted surgery; however early and long-term survivorship data of robotic-assisted UKA are lacking [36]. Therefore, the purpose of this multicenter study was to determine survivorship and patient satisfaction of robotic-assisted UKA at short-term follow-up.
2. Methods
2.1 Study design
In this prospective multicenter study, all patients were included who received a medial UKA with a fixed-bearing metal backed onlay tibial component between March 2009 and December 2011 (Figure 1). These patients represent the initial series of robotic-assisted MCK Medial Onlay UKAs (MAKO Surgical Corp., Ft. Lauderdale, FL, USA) performed by six surgeons, starting from the implant release date of March 2009. This corresponded to the release of the Robotic Arm Interactive Orthopedic (RIO) System (MAKO Surgical Corp., Ft. Lauderdale, FL, USA), a third generation robot-guided surgical instrument. Prior to this study, all surgeons participated in a knee course, in which the surgeons practiced robotic-assisted medial UKA on two to five cadaveric knees. Because half of the participating surgeons had previous robotic experience with UKA, this series included the robotic technology learning curve for three surgeons, and the implant learning curve for all six surgeons, both defined as the first 30 cases with the new technique and implant. The participating surgeons exhibited varying procedural volumes for robotic-assisted UKA during the study period, ranging from 4.6 to 15.8 procedures per month. The exact surgical indications for medial UKA were left to the discretion of the individual surgeons. This study was approved under the Western Institutional Review Board (WIRB) for all centers.
Fig. 1.

The MCK Medial Onlay UKA is shown with the femoral component, tibial component and the ultra-high-molecular-weight polyethylene (UHMWPE) insert.
2.2 Robot characteristics
Accuracy of the RIO system has previously been well characterized. Mechanical alignment with this system is accurate within 1.6° of the preoperative plan [37], soft tissue balancing is accurate within 0.53 mm of the preoperative plan at all flexion angles [25] and component positioning is accurate for the femoral component within 0.8 mm and 0.9° of the original plan and for the tibial component within 0.9 mm and 1.7° of the preoperative plan in all directions [28]. Robotic-assistant UKA surgery has been shown to be more accurate and reliable when compared to manual UKA surgery [26,29,36,38].
2.3 Data collection
In order to collect data on survivorship and patient satisfaction, a research coordinator contacted all patients by phone to complete a survey at a minimum of two years postoperatively. Patients were asked a series of questions to determine their implant survivorship and overall satisfaction with the function of their operated knee. The questions included a confirmation of the patient's surgeon and implant and whether they have had their implant removed, revised, or reoperated for any reason. If the patient answered yes, the patient was asked for the date and reason of revision or reoperation, and whether or not they returned to their original surgeon. If the patients answered no, the patient was asked to rate their overall satisfaction with their operated knee on the following five-level Likert scale: “very satisfied”, “satisfied”, “neutral”, “dissatisfied”, or “very dissatisfied”. Phone contact for each patient was attempted three times before they were considered lost to follow-up.
Patients were classified in different age groups (i.e. ≤ 59 years, 60 – 69 years, 70 – 79 years and ≥ 80 years) with age defined as age at time of surgery. Patients were also classified in different BMI groups according to the World Health Organization (i.e. normal weight (18.5 – 24.9), overweight (25.0 – 29.9), class I obesity (30.0 – 34.9) and class II-III obesity (≥35.0)). The annual revision rate was used to compare these different age and BMI groups. This parameter is defined as the “revision rate per 100 observed component years” and is calculated by dividing the number of failures by the total observed component years. This outcome corrects for different follow-up intervals and number of implants and therefore enables comparison between different groups or studies. This method is frequently used by other studies reporting UKA revision rates [39–42].
2.4 Statistical Analysis
All statistical analyses were performed using SAS Software for Windows 9.3 (SAS Institute Inc., Cary, NC, USA). In order to assess robotic-assisted UKA survivorship, revision for any reason was determined. Additionally, a “worst-case” analysis was performed whereby all patients who declined to participate in the follow-up survey considered as revision, which has been reported in orthopedic studies [17,43]. Survivorship from surgery to revision was calculated and graphed according to the Kaplan-Meier method and reported with 95% confidence interval (CI) [44]. The log-rank test was then used to compare survivorship between surgeons. Independent t-tests were used to assess the learning curve of all surgeons by comparing revision rate in the first 30 cases to revision rate in the remaining cases. To our best knowledge, no statistical method can be used to assess differences in annual revision rate as stated by other studies [39,40,42,45]. All tests were two-sided and a p-value of <0.05 was used to determine statistical significance.
3. Results
A total of 1007 consecutive patients (1135 knees) underwent robotic-assisted medial UKA surgery. Thirty-five patients declined study participation, 15 patients were deceased, and 160 patients were lost to follow-up (i.e. could not be contacted). A total of 797 patients (909 knees) were successfully enrolled in the study, yielding an 80% follow-up rate. A total of 443 males (56%) and 352 females (44%) were included (gender was missing in two patients). Of all patients, 685 patients (86%) received unilateral UKA while 112 patients (14%) received bilateral UKA. Average age (± SD) at surgery was 69.1 ± 9.5 years (range: 39 – 93 years) and the average BMI was 29.4 ± 4.9 (range: 19 – 48; BMI was missing in 18 patients). Average follow-up was 29.6 months (range: 22 – 52 months).
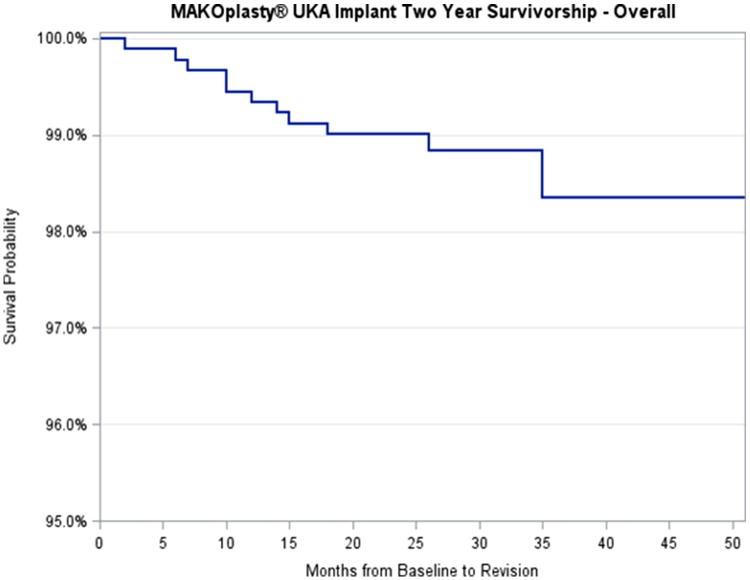
Eleven revisions (3 males, 8 females) were reported in 909 knees, which resulted in a survivorship of 98.8% (95% CI: 97.8% – 99.3%) at mean follow-up of 2.5 years (Figure 2). The annual revision rate was 0.49 revisions per year (Table 1). Fifteen patients reported reoperations in which no original implant component was removed. Worst-case scenario analysis (with patients who declined to participate considered as failure) revealed a survivorship of 96.0% (95% CI: 94.7% – 97.0%). Modes of failures were unexplained pain in five patients (45%), aseptic loosening in three patients (27%), infection in one patient (9%), tibial subsidence in one patient (9%) and OA progression in one patient (9%). Reasons for reoperation included soft tissue tears and cement debridement but were not further specified.
Fig. 2.
The Kaplan-Meier curve shows the survivorship of this cohort of 909 UKAs.
Table 1. Revisions per 100 observed years (annual revision rate) in different age groups.
| Age group | Mean Age | Number of UKA | Mean follow-up (months) | Number of Revisions | Total Observed years | Annual Revision Rate |
|---|---|---|---|---|---|---|
| ≤ 59 years | 54.3 | 154 | 29.2 | 4 | 374.5 | 1.07 |
| 60 - 69 | 65.3 | 323 | 29.1 | 3 | 784.4 | 0.38 |
| 70 - 79 | 74.7 | 303 | 30.2 | 3 | 761.8 | 0.39 |
| ≥ 80 years | 83.1 | 129 | 29.9 | 1 | 321.9 | 0.31 |
|
| ||||||
| Total | 69.1 | 909 | 29.6 | 11 | 2242.2 | 0.49 |
UKA indicates unicompartmental knee arthroplasty.
When comparing annual revision rates in different age groups, it was found that patients older than 80 years had the lowest annual revision rate (0.31), while patients younger than 60 years had the highest annual revision rate (1.07) (Table 1). When comparing annual revision rate in different BMI groups, the highest revision rate was found in patients with an BMI above 35 (1.36) while patients with normal weight (BMI 18.5 – 24.9) had the lowest annual revision rate (0.28) (Table 2).
Table 2. Revisions per 100 observed years (annual revision rate) in different BMI groups.
| BMI | Mean BMI | Number of UKA | Mean follow-up (months) | Number of Revisions | Total Observed years | Annual Revision Rate |
|---|---|---|---|---|---|---|
| Missing | 0 | 18 | 33.8 | 0 | 50.7 | 0.00 |
| 18.5 – 24.9 | 23.1 | 143 | 29.5 | 1 | 351.3 | 0.28 |
| 25.0 – 29.9 | 27.5 | 401 | 29.5 | 4 | 986.1 | 0.41 |
| 30.0 – 34.9 | 32.2 | 228 | 29.5 | 2 | 561.3 | 0.36 |
| ≥ 35.0 | 38.0 | 119 | 29.6 | 4 | 293.2 | 1.36 |
|
| ||||||
| Total | 29.4 | 909 | 29.6 | 11 | 2242.2 | 0.49 |
UKA indicates unicompartmental knee arthroplasty.
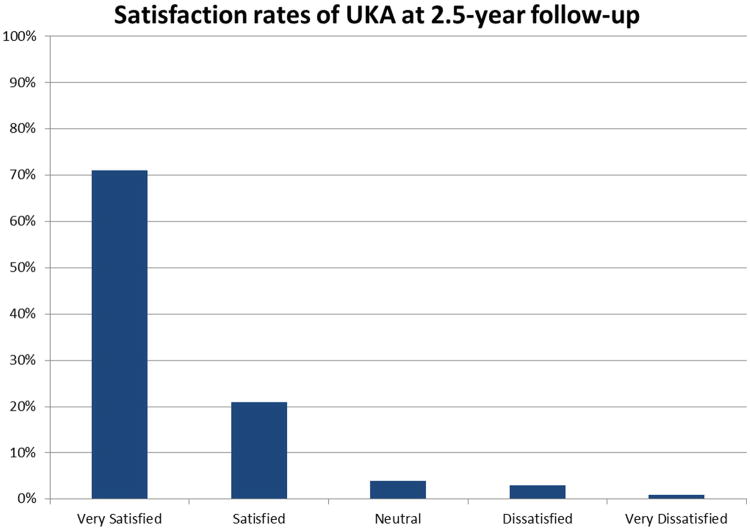
Of all patients without revision, 71% reported feeling very satisfied with their overall operated knee function and 21% of patients were satisfied, while 3% reported feeling dissatisfied and 1% reported feeling very dissatisfied. Four percent of patients were neither satisfied nor dissatisfied (Figure 3).
Fig. 3.
Patient satisfaction results at two-year follow-up are shown with 92% of patients reporting either very satisfied or satisfied regarding the overall function of their operated knee.
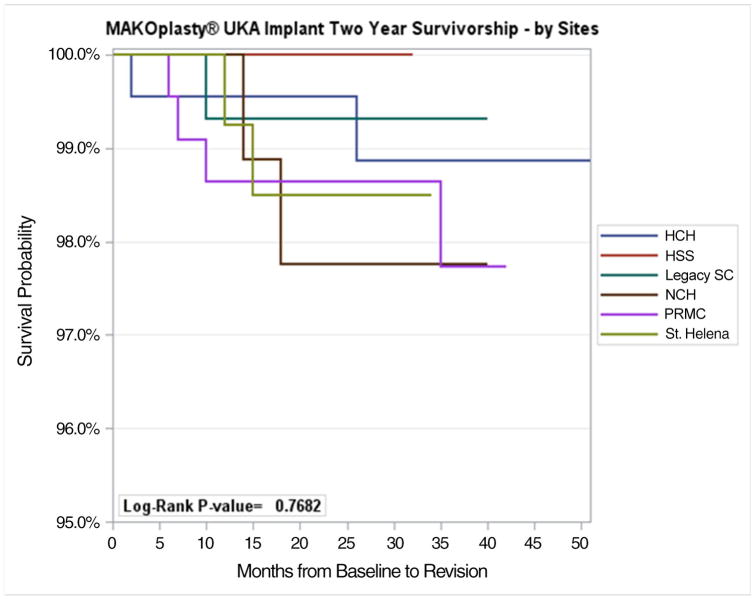
No significant differences were seen between the surgeons concerning revision or reoperation (Figure 4). For all surgeons, no significant learning curve was detected with regards to revision or reoperation (all p > 0.05).
Fig. 4.
Kaplan-Meier curve is shown with the six centers that performed UKA procedures. No significant differences were seen between the centers (p = 0.768).
4. Discussion
This is the first large prospective, multicenter study that has assessed survivorship and satisfaction rate of robotic-assisted UKA. At short-term follow-up, a survivorship of 98.8% in 797 patients (909 knees) was found, while worst-case scenario analysis, with all patients declining participation considered as revised, revealed a survivorship of 96.0%. Furthermore, 92% of the patients were either very satisfied or satisfied with their overall knee function.
When comparing our survivorship with other large cohort studies and registry studies that report two to three year survivorship of UKA over the last decade, we found high survivorship (98.8%) in our large multicenter cohort compared to other cohort studies (average other studies 97.0%, Table 3 [17,18,46–50]). Indeed, to our knowledge, the UKA survivorship rate of 98.8% is the highest reported rate in the literature at this early time point of any large cohort studies (Table 3 [11,12,51,52]). In this study, a patient satisfaction rate of 92% was found at 2.5-year follow-up, which is similar to other cohort studies that reported UKA satisfaction scores of overall knee function at two-year follow-up (91.5%, Table 4 [53–62]) and higher than the satisfaction rates of registry data (85.0%, Table 4 [12,51,63]).
Table 3. Studies and annual registries reporting two to three year UKA survivorship.
| Author/Country | Year Published | Start Cohort | End Cohort | UKA (n) | Survivorship at two to three year follow-up |
|---|---|---|---|---|---|
| Cohort Studies | |||||
| Eickmann et al. [46] | 2006 | 1984 | 1998 | 411 | 96.0 % |
| Hamilton et al. [47] | 2014 | 2001 | 2004 | 517 | 97.0 % |
| Liebs et al. [48] | 2013 | 2002 | 2009 | 401 | 94.7 % |
| Lim et al. [49] | 2012 | 2001 | 2011 | 400 | 97.4 % |
| Pandit et al. [18] | 2011 | 1998 | 2009 | 1000 | 98.0 % |
| Vorlat et al. [50] | 2006 | 1988 | 1996 | 149 | 97.8 % |
| Yoshida et al. [17] | 2013 | 2002 | 2011 | 1279 | 98.3 % |
| Annual Registries | |||||
| Australia [11]* | 2014 | 1999 | 2013 | 41250 | 95.1 % |
| New Zealand [12]* | 2013 | 2000 | 2012 | 7388 | 96.1 % |
| Sweden [13]* | 2013 | 1999 | 2012 | 95.3 % | |
| United Kingdom [51] | 2013 | 2003 | 2010 | 30795 | 95.6 % |
|
| |||||
| Cohort Studies | 97.0 % | ||||
| Annual Registries | 95.5 % | ||||
UKA indicates unicompartmental knee arthroplasty.
These registries reported combined medial and lateral UKA survivorship with predominantly medial UKA
Table 4. Cohort studies and annual registries reporting satisfaction of patients following medial UKA in excellent/good and fair/poor.
| Year | No of UKA | Mean FU (y) | Excellent/good | Fair/poor | |
|---|---|---|---|---|---|
| Cohort Studies | |||||
| Bhattacharya et al. [53] | 2012 | 131 | 4.3 | 93.1 % | 6.9 % |
| Biswal et al. [54] | 2010 | 116 | 5.7 | 91.4 % | 8.4 % |
| Gleeson et al. [55] | 2004 | 101 | 2.0 | 77.5 % | 22.5 % |
| Pietschmann et al. [56] | 2013 | 131 | 4.2 | 93.1 % | 6.9 % |
| Saxler et al. [57] | 2004 | 355 | 5.5 | 92.0 % | 8.0 % |
| Schroer et al. [58] | 2013 | 83 | 3.6 | 87.0 % | 13.0 % |
| Streit et al. [59] | 2015 | 107 | 5.0 | 94.4 % | 5.6 % |
| Von Keudell et al. [60] | 2014 | 141 | 6.1 | 94.3 % | 5.7 % |
| Walker et al. [61] | 2014 | 109 | 4.4 | 94.5 % | 5.5 % |
| Wong et al. [62] | 2014 | 51 | 4.3 | 98.0 % | 2.0 % |
| Annual Registries | |||||
| New Zealand [12] | 2015 | 2034 | 88.0 % | 12.0 % | |
| Sweden [63] | 2000 | 21164 | 83.0 % | 17.0 % | |
| United Kingdom [51] | 2014 | 25982 | 84.1 % | 15.9 % | |
|
| |||||
| Cohort Studies | 91.5 % | 8.5 % | |||
| Annual Registries | 85.0 % | 15.0 % | |||
UKA indicates unicompartmental knee arthroplasty; FU, follow-up.
A possible explanation for the low revision rate of robotic-assisted UKA at short-term follow-up is the ability of robotic-assisted surgery to control surgical variables. Early failures following UKA are associated with technical errors of implant malpositioning and lower limb malalignment [30–34,64]. Previous reports have demonstrated that robotic-assisted UKA can reduce variation in implant positioning in cadaveric studies [26] and improve postoperative implant positioning in patients undergoing UKA compared with conventional manual techniques [27–29]. Additionally, it has been shown that lower limb realignment is reliably controlled by robotic-assisted techniques [20–22,29]. As such, our favorable survivorship data using robotic assistance could be explained by improved control of surgical technique compared with manual approaches, which may decrease the risk of early aseptic loosening due to malpositioning and early disease progress secondary to overcorrection of lower leg alignment (Figure 5). Indeed, a recent systematic review showed that aseptic loosening (36%) and OA progression (20%) are the most common failure modes in medial UKA [35], which were less frequently seen in this study (27% and 9%, respectively, Figure 6). However, as some patients declined participation, a “worst-case” survivorship of 96.0% was calculated which would be consistent with prior cohort studies. In this “worst-case” survivorship scenario, clinical benefit of robotic-assisted UKA versus manual techniques would not be confirmed. Therefore, additional clinical outcomes studies of robotic-assisted UKA are clearly necessary to corroborate our findings.
Fig. 5.
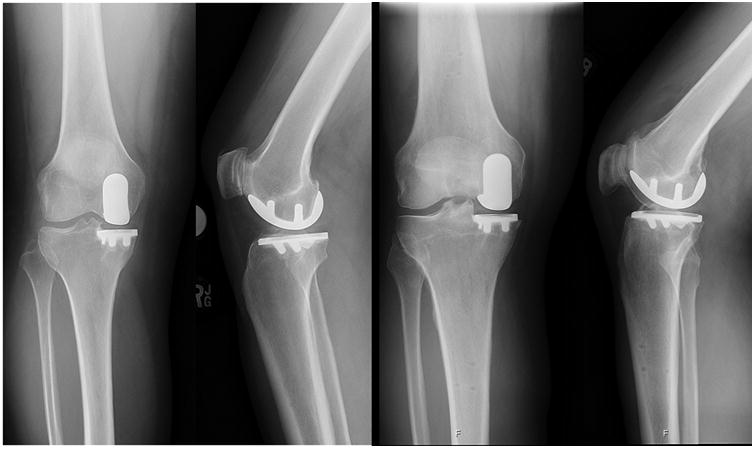
Well-fixed components are shown at two-year follow-up.
Fig. 6.
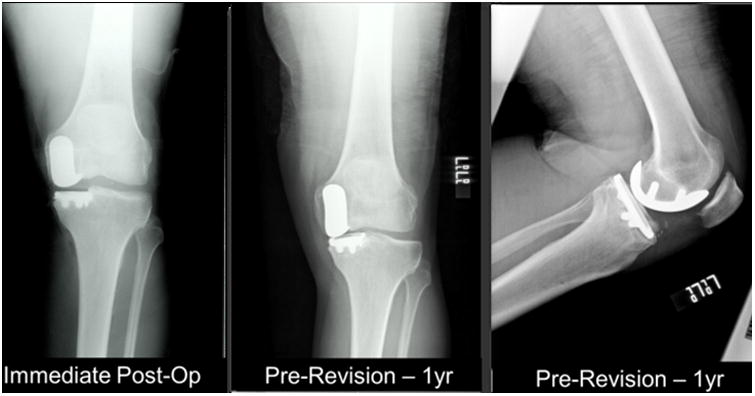
Immediate postoperative and at one-year follow-up radiographs are shown of a patient with a revised UKA. Loosening of the tibial baseplate at the anterior side is evident at one-year follow-up.
In this study cohort, an overall annual revision rate of 0.49 was found and the annual revision rate was higher in patients younger than 60 years (1.07). This finding is similar to several registries that reported higher revision rates in younger patients [41,65–67]. The higher demands and activity level in younger patients could explain the differences in revision when compared to older patients (0.31). Additionally, a higher annual revision rate in patients with obesity was noted. In our study, patients with normal weight had an annual revision rate of 0.28 while patients with class II-III obesity had an annual revision rate of 1.36; these findings are similar to current literature findings. Haughom and colleagues showed in a database analysis of 2316 UKAs that BMI was a significant risk factor for revision [68], while Kandil and colleagues showed in a national database study of 15770 UKAs that obesity and morbid obesity were risk factors for complications and revisions [69]. Interestingly, Bonutti et al. [70] and Berend et al. [71] showed that a higher BMI was associated with higher revision rate at two to three year follow-up, while other studies could not find a correlation between BMI and revision rates at long-term follow-up [72–77]. Our findings of increased annual revision rate in younger and obese patients in spite of the presumed standardization of the surgical technique with the robotic assistance confirm that these modifiable (BMI) and non-modifiable (age) factors influence survivorship in UKA. From our data, it is not possible to assess if robotic UKA surgery increases or decreases revision rates in patients with younger age or higher BMI when compared to conventional UKA, as this can only be assessed in a comparative study of manual and robotic UKA.
Multiple studies have demonstrated that conclusions related to the cost-effectiveness of UKA, TKA and HTO are highly sensitive to annual revision rates [8,78–80]. For example, it has been demonstrated that UKA is cost-effective compared to TKA if the annual revision rate is <4.0 per year in 78 year old patients [78]. In patients between age 50 and 60, UKA becomes the preferred cost-effective treatment for medial compartment OA compared to TKA and HTO when the annual conversion rate drops below 2.0 per year [79]. Our finding of an annual conversion rates of 0.39 per year in the 70 – 79 year old age group and 1.07 per year in the under 60 year old age group fall well below the threshold values to ensure that UKA is the preferred, cost-effective treatment in both these young and old age groups. Furthermore, Moschetti et al. compared cost-effectiveness of robotic-assisted UKA with manual UKA [80]. The authors used a two-year failure rate of 1.2% for robotic-assisted UKA and 3.1% for manual UKA, similar to the findings in this study and pooled manual UKA studies (Table 3), respectively. Taking robotic equipment costs into consideration, these authors found that robotic-assisted UKA is a cost-effective procedure when compared to manual UKA if the case volume exceeds 94 cases per year. These numbers indicate that robotic-assisted UKA is currently cost-effective in high-volume centers. Taken together, these studies suggest that the use of robotic technologies that control UKA surgical technique and improve survivorship may change conclusions regarding the cost-effectiveness of various procedures for treatment of isolated medial compartment degenerative joint disease.
There are several limitations to this study. The most important limitation is that 20% of patients were lost to follow-up. Most of these patients could not be included because they could not be reached by serial phone calls. However, a small percentage of patients declined to participate, which includes a potential bias. Therefore, a worst-case scenario survivorship analysis was performed, which showed comparable survivorship to that reported in registries and most manual cohort studies. A follow-up rate of 80% is not unexpected in a multicenter study of this scale performed in the United States (US) [81–85]. With a follow-up rate of 80%, this study still reports the survivorship and satisfaction rate of 909 robotic-assisted UKA procedures and is, to our knowledge, the largest US multicenter study reporting outcomes following UKA surgery. Findings in this study report that outcomes of robotic-assisted UKA surgery are between superior to similar to conventional UKA and therefore future studies are necessary to further compare outcomes of both procedures. A second limitation was that this study only assessed survivorship and satisfaction rate of robotic-assisted UKA surgery, while functional and radiographic outcomes were not obtained. Several other studies have previously reported radiologic outcomes and accuracy of robotic-assisted UKA surgery [25,26,28,29,37,38]. In addition, several recent studies have reported the short-term functional outcomes of robotic-assisted surgery [86–88]. A third limitation was that due to the nature of a multicenter study and the different surgeon case volumes, standardization of surgical indication was not part of the study design and no distinct exclusion criteria were specified for this study. However, because surgical indications were left to the discretion of the multiple surgeons in the study, these outcomes may be generalizable to the robotic UKA experience in the US. A fourth limitation is that medical notes were not reviewed and that all data is patient-reported, which may contain a potential bias. Lastly, follow-up was relatively short and long-term follow up is needed. This study is ongoing with patient contact planned at five and ten years postoperatively.
5. Conclusion
In this multicenter study, robotic-assisted UKA was found to have high survivorship and high satisfaction rate at short-term follow-up. Since worst-case scenario analysis revealed similar survivorship to manual UKA, prospective comparative studies with longer follow-up and high follow-up rate are necessary in order to further compare survivorship and satisfaction rates of robotic- assisted UKA to conventional UKA and to TKA.
Acknowledgments
We would like to thank Kaitlin Carroll, BS, for her assistance in writing the manuscript and thank Jon Dounchis, MD, and Fredrick Buechel Jr. as surgeons who performed surgery in a subset of patients. Finally, we would like to thank Michael Conditt and Sharon Branch from Stryker (Stryker Corporation, Kalamazoo, MI, USA) for their assistance in performing this study.
Conflict of Interest: The participating institutions received funding from MAKO Surgical Corporation for performing this study. Author ***, ***, *** and *** have received personal funding from MAKO Surgical Corporation over the last three years.
Contributor Information
Andrew D. Pearle, Hospital for Special Surgery, 535 East 70th St, New York, NY 10021, USA.
Jelle P. van der List, Hospital for Special Surgery, 535 East 70th St, New York, NY 10021, USA, Telephone: +1 (646) 238-4326.
Lily Lee, Hospital for Special Surgery, 535 East 70th St, New York, NY 10021, US.
Thomas M. Coon, Coon Joint Replacement Institute, 6 Woodland Road 202, St. Helena, CA 94574, USA.
Todd A. Borus, Legacy Salmon Creek Hospital, 2211 NE 139th Street, Vancouver WA 98686, USA.
Martin W. Roche, Holy Cross Hospital, 103 SE 1st Ave, Fort Lauderdale, FL 33316, USA.
References
- 1.Borus T, Thornhill T. Unicompartmental knee arthroplasty. J Am Acad Orthop Surg. 2008;16:9–18. doi: 10.5435/00124635-200801000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Newman JH, Ackroyd CE, Shah NA. Unicompartmental or total knee replacement? Five-year results of a prospective, randomised trial of 102 osteoarthritic knees with unicompartmental arthritis. J Bone Joint Surg Br. 1998;80:862–5. doi: 10.1302/0301-620x.80b5.8835. [DOI] [PubMed] [Google Scholar]
- 3.Watanabe T, Abbasi AZ, Conditt MA, Christopher J, Kreuzer S, Otto JK, et al. In vivo kinematics of a robot-assisted uni- and multi-compartmental knee arthroplasty. J Orthop Sci. 2014;19:552–7. doi: 10.1007/s00776-014-0578-3. [DOI] [PubMed] [Google Scholar]
- 4.Robertsson O, Borgquist L, Knutson K, Lewold S, Lidgren L. Use of unicompartmental instead of tricompartmental prostheses for unicompartmental arthrosis in the knee is a cost-effective alternative. 15,437 primary tricompartmental prostheses were compared with 10,624 primary medial or lateral unicompartmental prostheses. Acta Orthop Scand. 1999;70:170–5. doi: 10.3109/17453679909011257. [DOI] [PubMed] [Google Scholar]
- 5.Schwab PE, Lavand'homme P, Yombi JC, Thienpont E. Lower blood loss after unicompartmental than total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015;23:3494–500. doi: 10.1007/s00167-014-3188-x. [DOI] [PubMed] [Google Scholar]
- 6.Larsen K, Sørensen OG, Hansen TB, Thomsen PB, Søballe K. Accelerated perioperative care and rehabilitation intervention for hip and knee replacement is effective: a randomized clinical trial involving 87 patients with 3 months of follow-up. Acta Orthop. 2008;79:149–59. doi: 10.1080/17453670710014923. [DOI] [PubMed] [Google Scholar]
- 7.McAllister CM. The role of unicompartmental knee arthroplasty versus total knee arthroplasty in providing maximal performance and satisfaction. J Knee Surg. 2008;21:286–92. doi: 10.1055/s-0030-1247834. [DOI] [PubMed] [Google Scholar]
- 8.Ghomrawi HM, Eggman AA, Pearle AD. Effect of age on cost-effectiveness of unicompartmental knee arthroplasty compared with total knee arthroplasty in the U.S. J Bone Joint Surg Am. 2015;97:396–402. doi: 10.2106/JBJS.N.00169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Riddle DL, Jiranek WA, Neff RS, Whitaker D, Hull JR. Extent of tibiofemoral osteoarthritis before knee arthroplasty: multicenter data from the osteoarthritis initiative. Clin Orthop Relat Res. 2012;470:2836–42. doi: 10.1007/s11999-012-2328-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arno S, Maffei D, Walker PS, Schwarzkopf R, Desai P, Steiner GC. Retrospective analysis of total knee arthroplasty cases for visual, histological, and clinical eligibility of unicompartmental knee arthroplasties. J Arthroplasty. 2011;26:1396–403. doi: 10.1016/j.arth.2010.12.023. [DOI] [PubMed] [Google Scholar]
- 11.Annual Report 2014 Australian Hip and Knee Arthroplasty Register. 2014 [Google Scholar]
- 12.The New Zealand Joint Registry. Fourteen Year Report January 1999 to December 2012. 2013 [Google Scholar]
- 13.Annual Report 2013 Swedish Knee Arthroplasty Register. 2013 [Google Scholar]
- 14.Baker P, Jameson S, Critchley R, Reed M, Gregg P, Deehan D. Center and surgeon volume influence the revision rate following unicondylar knee replacement: an analysis of 23,400 medial cemented unicondylar knee replacements. J Bone Joint Surg Am. 2013;95:702–9. doi: 10.2106/JBJS.L.00520. [DOI] [PubMed] [Google Scholar]
- 15.Badawy M, Espehaug B, Indrekvam K, Havelin LI, Furnes O. Higher revision risk for unicompartmental knee arthroplasty in low-volume hospitals. Acta Orthop. 2014;85:342–7. doi: 10.3109/17453674.2014.920990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murray DW, Goodfellow JW, O'Connor JJ. The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Jt Surg Br. 1998;80:983–9. doi: 10.1302/0301-620x.80b6.8177. [DOI] [PubMed] [Google Scholar]
- 17.Yoshida K, Tada M, Yoshida H, Takei S, Fukuoka S, Nakamura H. Oxford phase 3 unicompartmental knee arthroplasty in Japan--clinical results in greater than one thousand cases over ten years. J Arthroplasty. 2013;28:168–71. doi: 10.1016/j.arth.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 18.Pandit H, Jenkins C, Gill HS, Barker K, Dodd CA, Murray DW. Minimally invasive Oxford phase 3 unicompartmental knee replacement: results of 1000 cases. J Bone Jt Surg Br. 2011;93:198–204. doi: 10.1302/0301-620X.93B2.25767. [DOI] [PubMed] [Google Scholar]
- 19.van der List JP, McDonald LS, Pearle AD. Systematic review of medial versus lateral survivorship in unicompartmental knee arthroplasty. Knee. 2015;22:454–60. doi: 10.1016/j.knee.2015.09.011. [DOI] [PubMed] [Google Scholar]
- 20.Keene G, Simpson D, Kalairajah Y. Limb alignment in computer-assisted minimally-invasive unicompartmental knee replacement. J Bone Joint Surg Br. 2006;88:44–8. doi: 10.1302/0301-620X.88B1.16266. [DOI] [PubMed] [Google Scholar]
- 21.Jenny JY, Boeri C. Unicompartmental knee prosthesis implantation with a non-image-based navigation system: rationale, technique, case-control comparative study with a conventional instrumented implantation. Knee Surg Sports Traumatol Arthrosc. 2003;11:40–5. doi: 10.1007/s00167-002-0333-8. [DOI] [PubMed] [Google Scholar]
- 22.Jenny JY, Ciobanu E, Boeri C. The rationale for navigated minimally invasive unicompartmental knee replacement. Clin Orthop Relat Res. 2007;463:58–62. doi: 10.1097/BLO.0b013e318126c077. [DOI] [PubMed] [Google Scholar]
- 23.Nam D, Khamaisy S, Gladnick BP, Paul S, Pearle AD. Is tibiofemoral subluxation correctable in unicompartmental knee arthroplasty? J Arthroplasty. 2013;28:1575–9. doi: 10.1016/j.arth.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 24.Khamaisy S, Gladnick BP, Nam D, Reinhardt KR, Heyse TJ, Pearle AD. Lower limb alignment control: is it more challenging in lateral compared to medial unicondylar knee arthroplasty? Knee. 2015;22:347–50. doi: 10.1016/j.knee.2015.02.018. [DOI] [PubMed] [Google Scholar]
- 25.Plate JF, Mofidi A, Mannava S, Smith BP, Lang JE, Poehling GG, et al. Achieving accurate ligament balancing using robotic-assisted unicompartmental knee arthroplasty. Adv Orthop. 2013;2013:837167. doi: 10.1155/2013/837167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Citak M, Suero EM, Citak M, Dunbar NJ, Branch SH, Conditt MA, et al. Unicompartmental knee arthroplasty: is robotic technology more accurate than conventional technique? Knee. 2013;20:268–71. doi: 10.1016/j.knee.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 27.Cobb J, Henckel J, Gomes P, Harris S, Jakopec M, Rodriguez F, et al. Hands-on robotic unicompartmental knee replacement: a prospective, randomised controlled study of the acrobot system. J Bone Joint Surg Br. 2006;88:188–97. doi: 10.1302/0301-620X.88B2.17220. [DOI] [PubMed] [Google Scholar]
- 28.Dunbar NJ, Roche MW, Park BH, Branch SH, Conditt MA, Banks SA. Accuracy of dynamic tactile-guided unicompartmental knee arthroplasty. J Arthroplasty. 2012;27:803–8.e1. doi: 10.1016/j.arth.2011.09.021. [DOI] [PubMed] [Google Scholar]
- 29.Lonner JH, John TK, Conditt MA. Robotic arm-assisted UKA improves tibial component alignment: a pilot study. Clin Orthop Relat Res. 2010;468:141–6. doi: 10.1007/s11999-009-0977-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hernigou P, Deschamps G. Alignment influences wear in the knee after medial unicompartmental arthroplasty. Clin Orthop Relat Res. 2004;(423):161–5. doi: 10.1097/01.blo.0000128285.90459.12. [DOI] [PubMed] [Google Scholar]
- 31.Hamilton WG, Collier MB, Tarabee E, McAuley JP, Engh CA, Engh GA. Incidence and reasons for reoperation after minimally invasive unicompartmental knee arthroplasty. J Arthroplasty. 2006;21:98–107. doi: 10.1016/j.arth.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 32.Engh GA, Dwyer KA, Hanes CK. Polyethylene wear of metal-backed tibial components in total and unicompartmental knee prostheses. J Bone Joint Surg Br. 1992;74:9–17. doi: 10.1302/0301-620X.74B1.1732274. [DOI] [PubMed] [Google Scholar]
- 33.Kasodekar VB, Yeo SJ, Othman S. Clinical outcome of unicompartmental knee arthroplasty and influence of alignment on prosthesis survival rate. Singapore Med J. 2006;47:796–802. [PubMed] [Google Scholar]
- 34.Swienckowski J, Page BJ. Medial unicompartmental arthroplasty of the knee. Use of the L-cut and comparison with the tibial inset method. Clin Orthop Relat Res. 1989:161–7. [PubMed] [Google Scholar]
- 35.van der List JP, Zuiderbaan HA, Pearle AD. Why Do Medial Unicompartmental Knee Arthroplasties Fail Today? J Arthroplasty. 2016;31:1016–21. doi: 10.1016/j.arth.2015.11.030. [DOI] [PubMed] [Google Scholar]
- 36.van der List JP, Chawla H, Pearle AD. Robotic-Assisted Knee Arthroplasty: An Overview. Am J Orthop (Belle Mead NJ) 2016;45:202–11. [PubMed] [Google Scholar]
- 37.Pearle AD, O'Loughlin PF, Kendoff DO. Robot-assisted unicompartmental knee arthroplasty. J Arthroplasty. 2010;25:230–7. doi: 10.1016/j.arth.2008.09.024. [DOI] [PubMed] [Google Scholar]
- 38.MacCallum KP, Danoff JR, Geller JA. Tibial baseplate positioning in robotic-assisted and conventional unicompartmental knee arthroplasty. Eur J Orthop Surg Traumatol Orthopedie Traumatol. 2016;26:93–8. doi: 10.1007/s00590-015-1708-0. [DOI] [PubMed] [Google Scholar]
- 39.Labek G, Sekyra K, Pawelka W, Janda W, Stöckl B. Outcome and reproducibility of data concerning the Oxford unicompartmental knee arthroplasty: a structured literature review including arthroplasty registry data. Acta Orthop. 2011;82:131–5. doi: 10.3109/17453674.2011.566134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sierra RJ, Kassel CA, Wetters NG, Berend KR, Della Valle CJ, Lombardi AV. Revision of unicompartmental arthroplasty to total knee arthroplasty: not always a slam dunk! J Arthroplasty. 2013;28:128–32. doi: 10.1016/j.arth.2013.02.040. [DOI] [PubMed] [Google Scholar]
- 41.van der List JP, Chawla H, Zuiderbaan HA, Pearle AD. The Role of Preoperative Patient Characteristics on Outcomes of Unicompartmental Knee Arthroplasty: A Meta-Analysis Critique. J Arthroplasty. 2016 doi: 10.1016/j.arth.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 42.Pabinger C, Berghold A, Boehler N, Labek G. Revision rates after knee replacement. Cumulative results from worldwide clinical studies versus joint registers. Osteoarthr Cartil. 2013;21:263–8. doi: 10.1016/j.joca.2012.11.014. [DOI] [PubMed] [Google Scholar]
- 43.Ackroyd CE, Whitehouse SL, Newman JH, Joslin CC. A comparative study of the medial St Georg sled and kinematic total knee arthroplasties. Ten-year survivorship. J Bone Joint Surg Br. 2002;84:667–72. doi: 10.1302/0301-620x.84b5.12404. [DOI] [PubMed] [Google Scholar]
- 44.Kaplan EL, Kaplan EL, Meyer P, Meyer P. Nonparametric estimation from incomplete samples. 1958;73 [Google Scholar]
- 45.van der List JP, Chawla H, Zuiderbaan HA, Pearle AD. Survivorship and functional outcomes of patellofemoral arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015 doi: 10.1007/s00167-015-3878-z. [DOI] [PubMed] [Google Scholar]
- 46.Eickmann THH, Collier MBB, Sukezaki F, McAuley JPP, Engh GaA. Survival of medial unicondylar arthroplasties placed by one surgeon 1984-1998. Clin Orthop Relat Res. 2006;452:143–9. doi: 10.1097/01.blo.0000238793.74843.dc. [DOI] [PubMed] [Google Scholar]
- 47.Hamilton WG, Ammeen DJ, Hopper RH. Mid-term survivorship of minimally invasive unicompartmental arthroplasty with a fixed-bearing implant: revision rate and mechanisms of failure. J Arthroplasty. 2014;29:989–92. doi: 10.1016/j.arth.2013.10.010. [DOI] [PubMed] [Google Scholar]
- 48.Liebs TR, Herzberg W. Better quality of life after medial versus lateral unicondylar knee arthroplasty. Clin Orthop Relat Res. 2013;471:2629–40. doi: 10.1007/s11999-013-2966-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lim HC, Bae JH, Song SH, Kim SJ. Oxford phase 3 unicompartmental knee replacement in Korean patients. J Bone Jt Surg Br. 2012;94:1071–6. doi: 10.1302/0301-620X.94B8.29372. [DOI] [PubMed] [Google Scholar]
- 50.Vorlat P, Putzeys G, Cottenie D, Van Isacker T, Pouliart N, Handelberg F, et al. The Oxford unicompartmental knee prosthesis: an independent 10-year survival analysis. Knee Surg Sports Traumatol Arthrosc. 2006;14:40–5. doi: 10.1007/s00167-005-0621-1. [DOI] [PubMed] [Google Scholar]
- 51.Baker PN, Jameson SS, Deehan DJ, Gregg PJ, Porter M, Tucker K. Mid-term equivalent survival of medial and lateral unicondylar knee replacement: an analysis of data from a National Joint Registry. J Bone Jt Surg Br. 2012;94:1641–8. doi: 10.1302/0301-620X.94B12.29416. [DOI] [PubMed] [Google Scholar]
- 52.Swedish Knee Arthroplasty Register: Annual Report. n.d. [Google Scholar]
- 53.Bhattacharya R, Scott CE, Morris HE, Wade F, Nutton RW. Survivorship and patient satisfaction of a fixed bearing unicompartmental knee arthroplasty incorporating an all-polyethylene tibial component. Knee. 2012;19:348–51. doi: 10.1016/j.knee.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 54.Biswal S, Brighton RW. Results of unicompartmental knee arthroplasty with cemented, fixed-bearing prosthesis using minimally invasive surgery. J Arthroplasty. 2010;25:721–7. doi: 10.1016/j.arth.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 55.Gleeson RE, Evans R, Ackroyd CE, Webb J, Newman JH. Fixed or mobile bearing unicompartmental knee replacement? A comparative cohort study. Knee. 2004;11:379–84. doi: 10.1016/j.knee.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 56.Pietschmann MF, Wohlleb L, Weber P, Schmidutz F, Ficklscherer A, Gülecyüz MF, et al. Sports activities after medial unicompartmental knee arthroplasty Oxford III-what can we expect? Int Orthop. 2013;37:31–7. doi: 10.1007/s00264-012-1710-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Saxler G, Temmen D, Bontemps G. Medium-term results of the AMC-unicompartmental knee arthroplasty. Knee. 2004;11:349–55. doi: 10.1016/j.knee.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 58.Schroer WC, Barnes CL, Diesfeld P, LeMarr A, Ingrassia R, Morton DJ, et al. The Oxford unicompartmental knee fails at a high rate in a high-volume knee practice. Clin Orthop Relat Res. 2013;471:3533–9. doi: 10.1007/s11999-013-3174-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Streit MR, Streit J, Walker T, Bruckner T, Philippe Kretzer J, Ewerbeck V, et al. Knee Surg Sports Traumatol Arthrosc. 2015. Minimally invasive Oxford medial unicompartmental knee arthroplasty in young patients. [DOI] [PubMed] [Google Scholar]
- 60.Von Keudell A, Sodha S, Collins J, Minas T, Fitz W, Gomoll AH. Patient satisfaction after primary total and unicompartmental knee arthroplasty: an age-dependent analysis. Knee. 2014;21:180–4. doi: 10.1016/j.knee.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 61.Walker T, Gotterbarm T, Bruckner T, Merle C, Streit MR. Total versus unicompartmental knee replacement for isolated lateral osteoarthritis: a matched-pairs study. Int Orthop. 2014;38:2259–64. doi: 10.1007/s00264-014-2473-0. [DOI] [PubMed] [Google Scholar]
- 62.Wong T, Wang CJ, Wang JW, Ko JY. Functional outcomes of uni-knee arthroplasty for medial compartment knee arthropathy in asian patients. Biomed J. 2014;37:406–10. doi: 10.4103/2319-4170.132877. [DOI] [PubMed] [Google Scholar]
- 63.Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L. Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand. 2000;71:262–7. doi: 10.1080/000164700317411852. [DOI] [PubMed] [Google Scholar]
- 64.Hernigou P, Deschamps G. Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty. J Bone Joint Surg Am. 2004;86–A:506–11. doi: 10.2106/00004623-200403000-00007. [DOI] [PubMed] [Google Scholar]
- 65.Harrysson OLa, Robertsson O, Nayfeh JF. Higher cumulative revision rate of knee arthroplasties in younger patients with osteoarthritis. Clin Orthop Relat Res. 2004:162–8. doi: 10.1097/01.blo.0000127115.05754.ce. [DOI] [PubMed] [Google Scholar]
- 66.Niinimäki T, Eskelinen A, Mäkelä K, Ohtonen P, Puhto AP, Remes V. Unicompartmental knee arthroplasty survivorship is lower than TKA survivorship: a 27-year Finnish registry study. Clin Orthop Relat Res. 2014;472:1496–501. doi: 10.1007/s11999-013-3347-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.W-Dahl A, Robertsson O, Lidgren L, Miller L, Davidson D, Graves S. Unicompartmental knee arthroplasty in patients aged less than 65. Acta Orthop. 2010;81:90–4. doi: 10.3109/17453671003587150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Haughom BD, Schairer WW, Hellman MD, Nwachukwu BU, Levine BR. An Analysis of Risk Factors for Short-Term Complication Rates and Increased Length of Stay Following Unicompartmental Knee Arthroplasty. HSS J. 2015;11:112–6. doi: 10.1007/s11420-014-9422-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kandil A, Werner BC, Gwathmey WF, Browne JA. Obesity, morbid obesity and their related medical comorbidities are associated with increased complications and revision rates after unicompartmental knee arthroplasty. J Arthroplasty. 2015;30:456–60. doi: 10.1016/j.arth.2014.10.016. [DOI] [PubMed] [Google Scholar]
- 70.Bonutti PM, Goddard MS, Zywiel MG, Khanuja HS, Johnson AJ, Mont MA. Outcomes of unicompartmental knee arthroplasty stratified by body mass index. J Arthroplasty. 2011;26:1149–53. doi: 10.1016/j.arth.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 71.Berend KR, Lombardi AV, Mallory TH, Adams JB, Groseth KL. Early failure of minimally invasive unicompartmental knee arthroplasty is associated with obesity. Clin Orthop Relat Res. 2005;440:60–6. doi: 10.1097/01.blo.0000187062.65691.e3. [DOI] [PubMed] [Google Scholar]
- 72.Murray DW, Pandit H, Weston-Simons JS, Jenkins C, Gill HS, Lombardi AV, et al. Does body mass index affect the outcome of unicompartmental knee replacement? Knee. 2013;20:461–5. doi: 10.1016/j.knee.2012.09.017. [DOI] [PubMed] [Google Scholar]
- 73.Bini S, Khatod M, Cafri G, Chen Y, Paxton EW. Surgeon, implant, and patient variables may explain variability in early revision rates reported for unicompartmental arthroplasty. J Bone Joint Surg Am. 2013;95:2195–202. doi: 10.2106/JBJS.L.01006. [DOI] [PubMed] [Google Scholar]
- 74.Bordini B, Stea S, Falcioni S, Ancarani C, Toni A. Unicompartmental knee arthroplasty: 11-year experience from 3929 implants in RIPO register. Knee. 2014;21:1275–9. doi: 10.1016/j.knee.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 75.Cavaignac E, Lafontan V, Reina N, Pailhe R, Wargny M, Laffosse JM, et al. Obesity has no adverse effect on the outcome of unicompartmental knee replacement at a minimum follow-up of seven years. Bone Jt J. 2013;95–B:1064–8. doi: 10.1302/0301-620X.95B8.31370. [DOI] [PubMed] [Google Scholar]
- 76.Plate JFF, Augart MAA, Seyler TMM, Bracey DNN, Hoggard A, Akbar M, et al. Obesity has no effect on outcomes following unicompartmental knee arthroplasty. Knee Surg Sport Traumatol Arthrosc. 2015 doi: 10.1007/s00167-015-3597-5. [DOI] [PubMed] [Google Scholar]
- 77.Tabor OBJB, Tabor OBJB, Bernard M, Wan JYY, Tabor OB, Jr, Tabor OBJB, et al. Unicompartmental knee arthroplasty: long-term success in middle-age and obese patients. J Surg Orthop Adv. 2005;14:59–63. [PubMed] [Google Scholar]
- 78.Slover J, Espehaug B, Havelin LI, Engesaeter LB, Furnes O, Tomek I, et al. Cost-effectiveness of unicompartmental and total knee arthroplasty in elderly low-demand patients. A Markov decision analysis. J Bone Joint Surg Am. 2006;88:2348–55. doi: 10.2106/JBJS.E.01033. [DOI] [PubMed] [Google Scholar]
- 79.Konopka JF, Gomoll AH, Thornhill TS, Katz JN, Losina E. The cost-effectiveness of surgical treatment of medial unicompartmental knee osteoarthritis in younger patients: a computer model-based evaluation. J Bone Joint Surg Am. 2015;97:807–17. doi: 10.2106/JBJS.N.00925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Moschetti WE, Konopka JF, Rubash HE, Genuario JW. Can Robot-Assisted Unicompartmental Knee Arthroplasty Be Cost-Effective? A Markov Decision Analysis. J Arthroplasty. 2016;31:759–65. doi: 10.1016/j.arth.2015.10.018. [DOI] [PubMed] [Google Scholar]
- 81.Bergeson AG, Berend KR, Lombardi AV, Hurst JM, Morris MJ, Sneller Ma. Medial mobile bearing unicompartmental knee arthroplasty: early survivorship and analysis of failures in 1000 consecutive cases. J Arthroplasty. 2013;28:172–5. doi: 10.1016/j.arth.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 82.Kievit AJ, Schafroth MU, Blankevoort L, Sierevelt IN, van Dijk CN, van Geenen RCI. Early experience with the Vanguard complete total knee system: 2-7 years of follow-up and risk factors for revision. J Arthroplasty. 2014;29:348–54. doi: 10.1016/j.arth.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 83.Su EP, Housman LR, Masonis JL, Noble JW, Engh CA. Five year results of the first US FDA-approved hip resurfacing device. J Arthroplasty. 2014;29:1571–5. doi: 10.1016/j.arth.2014.03.021. [DOI] [PubMed] [Google Scholar]
- 84.Meneghini RM, Ireland PH, Bhowmik-Stoker M. Multicenter Study of Highly Cross-linked vs Conventional Polyethylene in Total Knee Arthroplasty. J Arthroplasty. 2016;31:809–14. doi: 10.1016/j.arth.2015.10.034. [DOI] [PubMed] [Google Scholar]
- 85.Wright TW, Flurin PH, Crosby L, Struk AM, Zuckerman JD. Total shoulder arthroplasty outcome for treatment of osteoarthritis: a multicenter study using a contemporary implant. Am J Orthop (Belle Mead NJ) 2015;44:523–6. [PubMed] [Google Scholar]
- 86.Zuiderbaan HA, van der List JP, Chawla H, Khamaisy S, Thein R, Pearle AD. Predictors of Subjective Outcome After Medial Unicompartmental Knee Arthroplasty. J Arthroplasty. 2016;31:1453–8. doi: 10.1016/j.arth.2015.12.038. [DOI] [PubMed] [Google Scholar]
- 87.Zuiderbaan HA, van der List JP, Khamaisy S, Nawabi DH, Thein R, Ishmael C, et al. Unicompartmental knee arthroplasty versus total knee arthroplasty: Which type of artificial joint do patients forget? Knee Surg Sports Traumatol Arthrosc. 2015 doi: 10.1007/s00167-015-3868-1. [DOI] [PubMed] [Google Scholar]
- 88.van der List JP, Chawla H, Villa JC, Zuiderbaan HA, Pearle AD. Early functional outcome after lateral UKA is sensitive to postoperative lower limb alignment. Knee Surgery, Sport Traumatol Arthrosc. 2015 doi: 10.1007/s00167-015-3877-0. [DOI] [PubMed] [Google Scholar]