Abstract
Aims
To describe early progress of the Healthier You: NHS Diabetes Prevention Programme, a behavioural intervention designed to prevent or delay onset of Type 2 diabetes in people in England already identified to be at high risk, to assess numbers of referrals received by Programme providers and the proportion that attended the initial assessment, and to identify the factors associated with attendance rates.
Methods
These analyses examine the data for referrals received between June 2016 and March 2017.
Results
There were 43 603 referrals received, 16% higher than expected. Of those referred, 49% attended the initial assessment, higher than the 40% modelled uptake. Of those referred, there was no significant difference in uptake by sex (P=0.061); however, attendance per 100 000 population varied significantly by sex, age group, ethnicity and deprivation; it was significantly lower for men (P<0.001), higher as age increased (P<0.001) and higher for individuals from Asian, Afro‐Caribbean, mixed and other ethnic groups compared with individuals from white European groups (P<0.001). There was significant interaction between attendance rates by ethnicity and deprivation (P<0.001) such that attendance rates were significantly higher in the most deprived quintile vs the least deprived quintile for Asian, Afro‐Caribbean, mixed and other ethnic groups but not significantly different for white European ethnic groups.
Conclusion
The analyses show that referral numbers and percentage uptake are in excess of prior modelled values. Characteristics of attendees suggest that the programme is reaching those who are both at greater risk of developing Type 2 diabetes and who typically access healthcare less effectively.
What's new?
The Healthier You: NHS Diabetes Prevention Programme received 43 603 referrals between June 2016 and March 2017.
49% of individuals who were referred attended the first session.
Attendance rates for men, for individuals from Asian, Afro‐Caribbean, mixed and other ethnic groups, and for individuals from areas in the most deprived quintile, suggest that the programme is reaching both those who are at greater risk of developing Type 2 diabetes and those who typically access healthcare less effectively.
What's new?
The Healthier You: NHS Diabetes Prevention Programme received 43 603 referrals between June 2016 and March 2017.
49% of individuals who were referred attended the first session.
Attendance rates for men, for individuals from Asian, Afro‐Caribbean, mixed and other ethnic groups, and for individuals from areas in the most deprived quintile, suggest that the programme is reaching both those who are at greater risk of developing Type 2 diabetes and those who typically access healthcare less effectively.
Introduction
The prevalence of diabetes in England has increased from 2.3 million in 2009/2010 1 to 3.0 million in 2015/2016 2. Over 90% of people with diabetes have Type 2 diabetes 3. The associated complication and premature mortality burden is borne by individuals, their families and carers 4, and by the National Health Service (NHS) 5. Randomized controlled trials in those with impaired glucose tolerance have shown that onset of Type 2 diabetes can be prevented or delayed through behavioural interventions 6, 7.
A strategy for future healthcare in England, published in 2014, suggested a focus on prevention to manage demand, and proposed a national Type 2 diabetes prevention programme 8. The Healthier You: NHS Diabetes Prevention Programme was therefore developed to prevent or delay onset of Type 2 diabetes in adults already identified to be at high risk, defined as having non‐diabetic hyperglycaemia [HbA1c 42–47 mmol/mol (6.0–6.4%) or fasting plasma glucose 5.5–6.9 mmol/l]. Individuals identified after an NHS Health Check 9, through retrospective searches of general practice records for qualifying blood tests, or through routine clinical practice, are offered a place on a behavioural intervention. This approach is outlined in the National Institute for Health and Care Excellence (NICE) Public Health Guideline PH38 10, and will be complemented by the population‐level interventions to tackle obesity, the major modifiable risk factor for Type 2 diabetes, outlined in the UK Government's Childhood Obesity Plan 11.
Following a commissioned evidence review 12, an expert reference group 13 developed a service specification for behavioural interventions and their delivery, which informed a national procurement for intervention providers. Four service providers were appointed, each with the ability to provide the behavioural interventions in localities across England. The behavioural interventions enable weight loss, increased physical activity and improved nutrition through a minimum of 13 face‐to‐face group‐based sessions, over at least 9 months, constituting at least 16 h of contact time. Local health economies, partnerships of Clinical Commissioning Groups and Local Authorities who have responsibility for commissioning healthcare and public health services, choose from the available national service providers. They undertake to identify and refer a target number of eligible individuals into the programme, based on local expected prevalence of those at risk as well as on enabling infrastructure.
Formative evaluation has already been conducted 14, and a clinical and cost‐effectiveness evaluation of the Programme has been commissioned by the National Institute for Health Research that will report in 2021 15. There are few reports describing the implementation of large‐scale diabetes prevention programmes: the US Diabetes Prevention Programme has reported on 14 747 participants 16, the Australian lifestyle intervention programme ‘Life!’ on 8412 participants 17, and the Finnish National Diabetes Prevention Programme on 2798 participants 18.
The purpose of this paper is to describe early progress of the Healthier You programme. Using referrals from receipt of the first referral in June 2016 to the end of the first financial year of implementation (March 2017), this paper addresses the following questions:
Are the numbers of referrals received by programme providers in line with expectations?
What proportion of those referred, attend the initial assessment?
Do the characteristics of those attending the initial assessment suggest equality of access according to age, sex, ethnicity and deprivation?
Due to the minimum 9‐month intervention duration and time delay from referral to commencing the programme, no one had completed the programme by April 2017, so programme retention and completion rates, and changes in weight and glucose values were not available for this study.
Methods
Providers are contractually required to collect a minimum dataset comprising participant demographic and clinical information, and information about implementation. This study used data submitted by providers in June 2017, covering referrals from the first referral received in June 2016 to referrals made by the end of March 2017, with records of attendance at initial assessment extending to April 2017. Age, sex and general practice of individuals are recorded in the referral. First attendance is for an initial assessment, at which additional data, including ethnicity and postcode, are recorded. Because of the time delay between referral and initial assessment, uptake into the programme was calculated using the number of referrals received by the Providers up to January 2017 as the denominator, with numbers of corresponding attendees at initial assessment by April 2017 as the numerator. A pilot study involving 19 general practices capturing data up to March 2017 suggests that presently, coding at general practices of diagnoses of non‐diabetic hyperglycaemia and of referrals into the Programme was insufficient to use referrals recorded on general practice systems, hence only referrals received by Providers are used in the present study 19.
Recorded ages were grouped into 5‐year age bands and self‐reported ethnicity was grouped as either ‘white European’, or as ‘Asian, Afro‐Caribbean, mixed and other’. Deprivation was derived using Lower Super Output Area (derived from participant postcode), linked to the deprivation quintile from the Index of Multiple Deprivation 20.
The local health economy of each participant is recorded in the minimum dataset. General practice codes were used to assign a Clinical Commissioning Group to each record. The adult population (aged ≥18 years) of each local health economy was calculated using the 2015 mid‐year population estimates produced by the Office for National Statistics of each Clinical Commissioning Group within the local health economy 21. Ethnicity population estimates for each Clinical Commissioning Group were calculated by applying ethnicity proportions from the 2011 census to the adult population 22, and population estimates by deprivation quintile were calculated by applying proportions by deprivation quintile from the Index of Multiple Deprivation to the adult population 20.
Referral and attendance (at initial assessment) rates were calculated using Office for National Statistics adult population estimates as the denominator. Attendance rates for a given subgroup were calculated with respect to the estimated adult population for that subgroup. Uptake was calculated as the proportion of referrals attending initial assessment. All associations were tested using a two‐way chi‐squared test. A logistic regression model was used to investigate the association between the individual ethnicity and deprivation quintile of the participant (independent variables) and attendance (dependant variable). A Wald test was used to test the significance of the interaction between ethnicity and deprivation. Statistical significance was defined as P <0.05. CIs were set at 95%.
Results
There were 43 603 referrals made into the programme during this first financial year, corresponding to a rate of 198 per 100 000 of the adult population. The sum of the referral targets set by local health economies was 37 584, so that referral numbers exceeded targets by 16%. The local health economies included in this first wave of national roll‐out equated to a geographical coverage of 51% of England. By local health economy, the rate of referrals ranged from 70 to 692 per 100 000 (Table 1).
Table 1.
Referral numbers and rates per 100 000 during June 2016 to March 2017 and percentage uptake, using referrals received between June 2016 and January 2017 by local health economy
| Local health economy | Number of referrals | Target | Population of each local health economy | Referral rate per 100 000 adult population | 95% CIs | Uptakea, % | 95% CIs for uptake | ||
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | Lower | Upper | ||||||
| Berkshire | 1386 | 1500 | 688 825 | 201 | 191 | 212 | 35 | 32 | 38 |
| Birmingham | 977 | 2092 | 1 233 026 | 79 | 74 | 84 | 52 | 47 | 56 |
| Bury | 232 | 190 | 145,231 | 160 | 140 | 182 | 86 | 79 | 91 |
| Cambridgeshire & Peterborough | 762 | 1333 | 687 857 | 111 | 103 | 119 | 42 | 37 | 47 |
| Camden, Islington & Haringey | 1354 | 1238 | 594 685 | 228 | 216 | 240 | 62 | 59 | 66 |
| Cheshire | 710 | 797 | 821 475 | 86 | 80 | 93 | 46 | 42 | 51 |
| Cumbria | 1190 | 1274 | 410 169 | 290 | 274 | 307 | 32 | 29 | 35 |
| CWHHEa | 6524 | 1560 | 942 193 | 692 | 676 | 709 | 50 | 49 | 52 |
| Derbyshire | 1613 | 587 | 798 109 | 202 | 192 | 212 | 44 | 41 | 47 |
| Dudley | 196 | 350 | 248 478 | 79 | 68 | 91 | 63 | 52 | 72 |
| Durham | 489 | 376 | 419 453 | 117 | 106 | 127 | 55 | 48 | 61 |
| East Midlands CN | 4431 | 5032 | 2 182 542 | 203 | 197 | 209 | 45 | 43 | 47 |
| Essex | 749 | 1169 | 1 064 113 | 70 | 65 | 76 | 31 | 26 | 37 |
| Greater Lincolnshire | 3442 | 2454 | 854 372 | 403 | 390 | 417 | 54 | 52 | 56 |
| Hertfordshire | 2136 | 1002 | 887 082 | 241 | 231 | 251 | 51 | 48 | 53 |
| Inner North East London | 1817 | 2205 | 900 722 | 202 | 193 | 211 | 16 | 14 | 19 |
| Leeds | 1531 | 1943 | 611 462 | 250 | 238 | 263 | 57 | 54 | 60 |
| NHS Herefordshire | 1038 | 1350 | 152 032 | 683 | 642 | 726 | 59 | 55 | 63 |
| Norfolk | 1591 | 1000 | 497 066 | 320 | 305 | 336 | 56 | 53 | 60 |
| Oldham | 258 | 976 | 172 518 | 150 | 132 | 169 | 72 | 65 | 78 |
| Rochdale | 601 | 485 | 163 340 | 368 | 339 | 399 | 56 | 50 | 62 |
| Sefton | 507 | 372 | 220 506 | 230 | 210 | 251 | 86 | 75 | 93 |
| Sheffield | 649 | 850 | 453 896 | 143 | 132 | 154 | 55 | 50 | 60 |
| South East CN | 3455 | 2078 | 3 776 821 | 91 | 88 | 95 | 49 | 47 | 52 |
| South London | 4707 | 4070 | 2 522 861 | 187 | 181 | 192 | 43 | 42 | 45 |
| St. Helens | 339 | 286 | 141 333 | 240 | 215 | 267 | 72 | 66 | 78 |
| Worcestershire | 919 | 1015 | 463 334 | 198 | 186 | 212 | 70 | 67 | 74 |
| Total | 43 603 | 37 584 | 22 053 501 | 198 | 196 | 200 | 49 | 48 | 49 |
CN, clinical network; CWHHE, Central London, West London, Hammersmith & Fulham, Hounslow and Ealing.
Uptake calculated using referrals received between June 2016 and January 2017
Of the individuals referred between June 2016 and January 2017, 49% attended the first session by April 2017. This ranged from 16% to 86% by local health economy (Table 1). There was no significant difference in uptake by sex (48% men, 49% women; P=0.061). Uptake was significantly different by age group (P<0.001) and increased as the age range of participants increased: from 34% for individuals aged <40 years to 36% for ages 40–44 years, 39% for ages 45–49 years, 42% for ages 50–54 years, 49% for ages 55–59 years, 51% for ages 60–64 years, 56% for ages 65–69 years and then decreasing to 55% for ages 70–74 and 51% for ages ≥75 years. Ethnicity and deprivation are only recorded at initial assessment; therefore uptake could not be calculated according to these characteristics.
Participant characteristics and subgroup attendance rates are described in Table 2. Attendance rates were significantly lower for men than women [74 (95% CI 72–75) vs 87 (95% CI 86–89) per 100 000; P<0.001] and increased as age group increased up to age 74 years and then decreased for ages ≥75 years (P<0.001). There was a significantly higher attendance rate for Asian, Afro‐Caribbean, mixed and other ethnic group participants compared with white European participants [119 (95% CI 116–123) vs 68 (95% CI 67–69) per 100 000; P<0.001). Attendance rates varied significantly by deprivation with higher rates in the most deprived quintile vs the least deprived quintile [72 (95% CI 69–74) vs 60 (95% CI 57–62) per 100 000; P<0.001]; however, there was a significant interaction between ethnicity and deprivation (Wald=33.3, df=4; P<0.001), so that, while attendance rates were significantly higher in the most deprived quintile vs the least deprived quintile for Asian, Afro‐Caribbean, mixed and other ethnic groups, they were not significantly different for white European groups (Fig. 1).
Table 2.
Participant characteristics and attendance rates by subgroup for individuals who attended initial assessment during June 2016 to April 2017
| Number attended initial assessment | Percentage of attendees | Population of each subgroup | Rate per 100 000 population subgroup | 95% CIs | Chi‐squared P | ||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Total | 17 892 | 22 053 501 | 81 | 80 | 82 | ||
| Sex | |||||||
| Men | 7929 | 44 | 10 763 217 | 74 | 72 | 75 | <0.001 |
| Women | 9866 | 55 | 11 290 284 | 87 | 86 | 89 | |
| unknown | 97 | 1 | n/a | n/a | n/a | n/a | |
| Age group | |||||||
| <40 years | 626 | 3 | 8 403 055 | 7 | 7 | 8 | <0.001 |
| 40–44 years | 624 | 3 | 1 905 971 | 33 | 30 | 35 | |
| 45–49 years | 1019 | 6 | 2 000 593 | 51 | 48 | 54 | |
| 50–54 years | 1520 | 8 | 1 927 497 | 79 | 75 | 83 | |
| 55–59 years | 2020 | 11 | 1 631 036 | 124 | 119 | 129 | |
| 60–64 years | 2,329 | 13 | 1 433 023 | 163 | 156 | 169 | |
| 65–69 years | 3,168 | 18 | 1 475 649 | 215 | 207 | 222 | |
| 70–74 years | 2,903 | 16 | 1 105 270 | 263 | 253 | 272 | |
| ≥75 years | 3,667 | 20 | 2 171 407 | 169 | 163 | 174 | |
| Unknown | 16 | 0 | n/a | n/a | n/a | n/a | |
| Ethnic group | |||||||
| Asian, Afro‐Caribbean, mixed, other | 4,515 | 25 | 3 792 288 | 119 | 116 | 123 | <0.001 |
| White European | 12,397 | 69 | 18 261 213 | 68 | 67 | 69 | |
| Unknown | 980 | 5 | n/a | n/a | n/a | n/a | |
| Deprivation quintile | |||||||
| IMD 1 (most deprived) | 3,073 | 17 | 4 296 577 | 72 | 69 | 74 | <0.001 |
| IMD 2 | 2,972 | 17 | 4 602 993 | 65 | 62 | 67 | |
| IMD 3 | 3,492 | 20 | 4 418 163 | 79 | 76 | 82 | |
| IMD 4 | 2,854 | 16 | 4 294 546 | 66 | 64 | 69 | |
| IMD 5 (least deprived) | 2,651 | 15 | 4 441 222 | 60 | 57 | 62 | |
| Unknown | 2,850 | 16 | n/a | n/a | n/a | n/a | |
IMD, Index of Multiple Deprivation.
Figure 1.
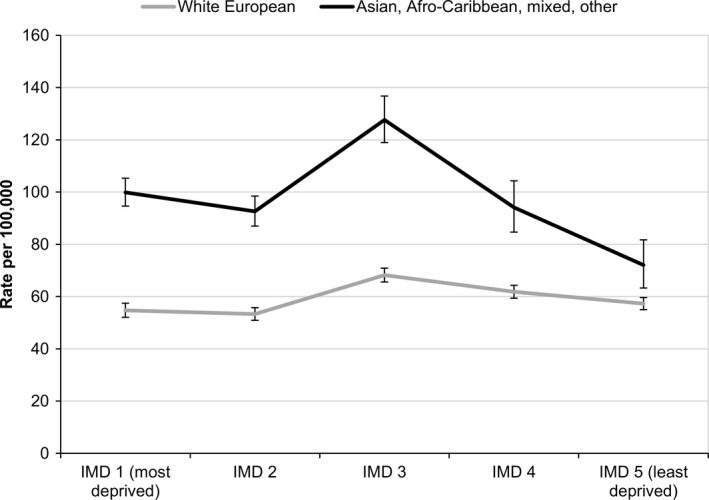
Attendance rates per 100 000 population by ethnic group and deprivation quintile during June 2016 to April 2017.
Discussion
The results of these early analyses show that the Healthier You Programme has achieved higher than anticipated numbers of referrals, 49% uptake and equality of access, reflected by the proportions of men, participants of Asian, Afro‐Caribbean, mixed and other ethnic groups, and participants from the most deprived areas.
There were 43 603 referrals received, exceeding the target by 16%. There was a tenfold variation in referral rates across local health economies. Much of this can be attributed to differences in initial targets set; local health economies that generated higher rates of referrals had typically set a higher target. However, targets were not solely reflective of prevalence of non‐diabetic hyperglycaemia, but also of local health economy infrastructure, and as the Programme progresses, and local infrastructure is developed, it is expected that future referral numbers will better reflect local need.
Uptake into the programme was 49%; the prior modelled estimate was 40%, based on expert knowledge 13. There was also significant variation in uptake across local health economies from 16% to 86%, attributable to factors including staggered roll‐out of programme provision, time lag between referral and initial assessment and differing mechanisms of engagement by referrer of those referred. Indeed, early qualitative evaluation will assess methods of engagement by referrer that are associated with higher uptake 15. There were no significant differences in uptake by sex, and whilst attendance rates for men were lower than for women, attendance for men was higher than observed in implementation of weight management programmes both in England 23, 24 and diabetes prevention programmes internationally 16, 17, 18.
Attendance rates for men, Asian, Afro‐Caribbean, mixed and other ethnic groups and participants from areas in the most deprived quintile further suggest that, in its early stages, the programme is reaching both those who are at greater risk of developing Type 2 diabetes and those who typically access healthcare less effectively, although efforts at engaging those most deprived have not been as successful for white European groups as for Asian, Afro‐Caribbean, mixed and other ethnic groups, something that the Programme will focus on moving forward.
In the US Programme report, 80% of attendees were women and those of non‐Hispanic white ethnicity constituted only 45% of participants 16. In the Australian report, 66% were women, and more participants were not working than were employed 17. In the Finnish report 67% were women, and lower socio‐economic status was associated with higher participation in men 18, 25. The latter two reports did not describe ethnicity.
It is acknowledged that equality extends beyond the four participant characteristics presented here, although those presented are associated with Type 2 diabetes risk. Future analyses will consider equality at a broader level, including geography of implementation and additional individual‐level protected characteristics.
There are some limitations to the analyses. Because of the risk of introducing additional uncertainties through the use of modelled estimates of non‐diabetic hyperglycaemia and the current lack of observational data for non‐diabetic hyperglycaemia prevalence, rates in this study were defined with respect to total populations rather than populations with non‐diabetic hyperglycaemia. Asian, Afro‐Caribbean, mixed and other ethnic groups can be estimated to have 1.2 times greater prevalence of non‐diabetic hyperglycaemia (Barron E, 2017, unpublished data relating to Public Health England 26) so the observed 1.8 times increase in attendance rates of Asian, Afro‐Caribbean, mixed and other ethnic groups compared with white European groups cannot simply be attributed to increased prevalence of non‐diabetic hyperglycaemia.
Some fields in the minimum dataset are better recorded than others. While age and sex have less than or equal to 1% missing values, 5% of ethnicity records and 16% of postcodes (needed to derive deprivation status) are missing, which could affect the deprivation picture presented here. This will be addressed in future through provider contract management and associated data quality assurance. The analysis is further limited by the timing of the data collected; while age and sex of the participant are recorded in the referral received by Providers, ethnicity and deprivation are not recorded until attendance at the initial assessment.
In conclusion, this report contains early analyses of referral and uptake data, focusing on equality of access, and provides a platform for ongoing learning and improvements. As further data become available, it will be possible to examine rates of retention and completion, as well as changes in weight and HbA1c by programme completion. In addition, in 2018/2019 the National Diabetes Audit will extract data from general practices on non‐diabetic hyperglycaemia, allowing the long‐term impact of the programme beyond 2021 to be assessed, although improvements in non‐diabetic hyperglycaemia Read coding, as well as data linkage between Providers and general practices, need to be explored to facilitate this 19.
Funding Sources
None.
Competing interests
All authors are members of the NHS England Diabetes Programme Directors Group. R.H. is Head of Policy, Knowledge and Insight at Diabetes UK; J.S. is the Public Health England Programme Director for the Healthier You programme; J.V. is the Clinical lead for the Healthier You Programme and National Clinical Director for Diabetes and Obesity at NHS England.
Acknowledgements
We thank members of the NHS England Diabetes Programme Directors Group for reviewing the manuscript.
Diabet. Med. 35, 513–518 (2018)
This article is published with the permission of the Controller of HMSO and the Queen's Printer for Scotland.
References
- 1. NHS Digital . Quality and Outcomes Framework (QOF) 2009/10. Available at http://content.digital.nhs.uk/catalogue/PUB04431. Last accessed 10 June 2017.
- 2. NHS Digital . Quality and Outcomes Framework (QOF) 2015/16. Available at http://content.digital.nhs.uk/qof. Last accessed 10 June 2017.
- 3. National Diabetes Audit, Report 1 Care processes and Treatment Targets 2016‐17. Available at https://digital.nhs.uk/catalogue/PUB30142. Last accessed 18 November 2017.
- 4. National Diabetes Audit, 2015‐16 Report 2a: Complications and Mortality. Available at https://digital.nhs.uk/catalogue/PUB30030. Last accessed 3 September 2017.
- 5. Hex N, Bartlett C, Wright D, Taylor M, Varley D. Estimating the current and future costs of Type 1 and Type 2 diabetes in the UK, including direct health costs and indirect societal and productivity costs. Diabet Med 2012; 29: 855–862. [DOI] [PubMed] [Google Scholar]
- 6. Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne‐Parikka P et al Prevention of Type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. NEJM 2001; 344: 1343–1350. [DOI] [PubMed] [Google Scholar]
- 7. Diabetes Prevention Program Research Group . Reduction in the incidence of Type 2 diabetes with lifestyle intervention or metformin. NEJM 2002; 346: 393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. NHS England . Five Year Forward View. 2014. Available at www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf. Last accessed 18 November 2017.
- 9. Public Health England . NHS Health Check Best Practice Guidance. 2017. Available at www.healthcheck.nhs.uk/document.php?o=1308. Last accessed 3 September 2017.
- 10. National Institute for Health and Clinical Excellence . Type 2 diabetes: prevention in people at high risk. 2012. Available at www.nice.org.uk/guidance/ph38/resources/type-2-diabetes-prevention-in-people-at-high-risk-pdf-1996304192197. Last accessed 3 September 2017.
- 11. UK Government . Childhood Obesity: a plan for action. 2016. Available at www.gov.uk/government/publications/childhood-obesity-a-plan-for-action. Last accessed 3 September 2017.
- 12. Public Health England . A systematic review of the effectiveness of lifestyle interventions for the prevention of type 2 diabetes mellitus (T2DM) in routine practice. 2015. Available at www.gov.uk/government/uploads/system/uploads/attachment_data/file/456147/PHE_Evidence_Review_of_diabetes_prevention_programmes-_FINAL.pdf. Last accessed 18 November 2017.
- 13. NHS England . NHS DPP Expert reference group. Available at www.england.nhs.uk/diabetes/diabetes-prevention/exp-ref-grp/. Last accessed 3 September 2017.
- 14. Penn L, Rodrigues A, Haste A, Marques MM, Budig K, Sainsbury K et al The NHS Diabetes Prevention Programme in England: formative evaluation of the programme in early phase implementation. BMJ Open 2017; in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. NHS National Institute for Health Research . Collaboration for Leadership in Applied Health Research and Care Greater Manchester. DIPLOMA – Evaluation of the national NHS Diabetes Prevention Programme. Available at http://clahrc-gm.nihr.ac.uk/our-work/exploiting-technologies/diploma-evaluation-nation-nhs-dpp/ Last accessed 7 September 2017.
- 16. Ely EK, Gruss SM, Luman ET, Gregg EW, Ali MK, Nhim K et al A national effort to prevent type 2 diabetes: participant‐level evaluation of CDC's national diabetes prevention program. Diabetes Care 2017; 40: 1331–1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dunbar J, Jayawardena A, Johnson G, Roger K, Timoshanko A, Versace VL et al Scaling up diabetes prevention in Victoria, Australia: Policy development, implementation and evaluation. Diabetes Care 2014; 37: 934–942. [DOI] [PubMed] [Google Scholar]
- 18. Saaristo T, Moilanen L, Korpi‐Hyövälti E, Vanhala M, Saltevo J, Niskanen L et al Lifestyle intervention for prevention of type 2 diabetes in primary health care: one‐year follow‐up of the Finnish National Diabetes Prevention Program (FIN‐D2D). Diabetes Care 2010; 33: 2146–2151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. NHS Digital . National Diabetes Prevention Programme: Pilot study for the collection of data from GP practices in England. Available at www.digital.nhs.uk/catalogue/PUB30119. Last accessed 19 November 2017.
- 20. Department for Communities and Local Government . The English indices of deprivation 2015. Available at www.gov.uk/government/uploads/system/uploads/attachment_data/file/465791/English_Indices_of_Deprivation_2015_-_Statistical_Release.pdf Last accessed 23 July 2017.
- 21. Office for National Statistics . Dataset: Clinical commissioning group mid‐year population estimates. Available at www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/clinicalcommissioninggroupmidyearpopulationestimates. Last accessed 23 July 2017.
- 22. NOMIS Official labour market statistics . Ethnic group by sex and age. Available at www.nomisweb.co.uk/census/2011/lc2101ew. Last accessed 3 September 2017.
- 23. Dixon KJ, Shcherba S, Kipping RR. Weight loss from three commercial providers of NHS primary care slimming on referral in North Somerset: service evaluation. J Public Health 2012; 34: 555–561. [DOI] [PubMed] [Google Scholar]
- 24. Ahern AL, Aveyard P, Boyland EJ, Halford JCG, Jebb S. Inequalities in the uptake of weight management interventions in a pragmatic trial: an observational study in primary care. British Journal of General Practice. 2016; 66: e258–e263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rautio N, Jokelainen J, Oksa H, Saaristo T, Peltonen M, Niskanen L et al Participation, socioeconomic status and group or individual counselling intervention in inviduals at high risk for type 2 diabetes: One‐year follow‐up study of the FIN‐D2D‐project. Primary Care Diabetes 2012; 6: 277–283. [DOI] [PubMed] [Google Scholar]
- 26. Public Health England . Research and analysis: Analysis of non‐diabetic hyperglycaemia prevalence in England. Available at www.gov.uk/government/publications/nhs-diabetes-prevention-programme-non-diabetic-hyperglycaemia Last accessed 15 September 2017.


